Abstract
Objectives
To examine the prevalence of obesity and its relationship with pressure ulcers among nursing home (NH) populations, and whether such relationship varies with certified nursing assistant (CNA) level in NHs.
Data and study population
The 1999–2009 nationwide Minimum Data Sets were linked with Online Survey of Certification and Reporting records. We identified newly admitted NH residents who became long-stayers and followed them up to 1 year.
Analyses
The outcome variable was presence of pressure ulcers during the 1-year follow-up period. Residents were categorized as normal (18.5<=BMI<30 kg/m2), mild obesity (30 <=BMI <35 kg/m2) and moderate or severe obesity (BMI>=35 kg/m2). Pooled and stratified analyses were performed to examine the relationship between obesity and pressure ulcers, and how it varied by facility CNA level.
Results
The prevalence of obesity increased from 16.9% to 25.8% among newly admitted NH residents over the last decade. Obesity was associated with higher risks of pressure ulcers among long-stay residents. The relationship between obesity and pressure ulcers persisted after accounting for individual health conditions at the baseline and facility-level variations. Further, the within-facility relationship between obesity and pressure ulcers varied by facility CNA levels. The odds of pressure ulcers were 18.9% higher for residents with moderate or severe obesity than for non-obese residents within NHs with low CNA levels. The percents for medium and high CNA level facilities were 14.0% and 12.8%, respectively.
Conclusion
To prepare for the growing obesity epidemic in NHs, policies should focus on strategies to improve care provided for obese residents.
Keywords: obesity, nursing home, pressure ulcers
INTRODUCTION
Over the past thirty years the rate of obesity in the U.S. population has increased from 14.1% to 30.5%.(1, 2) The escalating rates of obesity impacts on many health care providers including the nursing home (NH) setting. A study of obesity prevalence in NHs in five states found that the prevalence of obesity in NHs rose from 15% in 1992 to 25% in 2002 (3)
Obesity leads to multiple complications and co-morbidities. Obese people usually have increased difficulties in mobility, such as rising from a chair or bed.(4, 5) Due to their heavy body weight and immobility, obese persons may be prone to pressure ulcers, (6) which usually develop when body weight presses skins and tissues on to surfaces such as beds or wheel chairs for long periods. However, the empirical evidence of the relationship between obesity and pressure ulcers among the elderly is not clear. While some studies indicate obesity is a risk factor for pressure ulcers, (7, 8) others find that obesity is not related or may even reduce the risk of pressure ulcers among some elderly populations (9–11).
NH populations are particularly susceptible to pressure ulcers because they are generally old, frail and have multiple co-morbidities, and often have limitations in mobility.(12) Obese NH residents may have an added risk of acquiring pressure ulcers due to their heavy body weight and immobility. NH attributes may further affect the risk of pressure ulcers for obese residents. For example, NH certified nursing assistant (CNA) level may have been an important role in preventing pressure ulcers. CNAs are the frontline workers who are responsible for repositioning residents or helping them move around to prevent the occurrence of pressure ulcers.(13, 14) Obese residents may require more CNA time to help them with daily activities as well as pressure ulcer prevention due to their heavy body weights. (15)(16) Therefore, facilities with insufficient CNA staffing may not be able to provide sufficient care such as repositioning obese residents often, and the differences in presence of pressure ulcers between obese and non-obese residents might be exacerbated in such facilities. However, to date, most of the published studies have not examined the role of obesity when evaluating pressure ulcer rates in a NH (17–22), and none has examined whether and how CNA staffing level impact pressure ulcer rates among obese residents.
Pressure ulcers are closely related to quality of life, mortality, and mobility among NH residents. (23, 24) Therefore it is necessary to understand the relationship between obesity and pressure ulcers so that efforts can be made to prevent the occurrence of pressure ulcers among obese residents. This study aims to examine the role of obesity in the development of pressure ulcers, and whether facility characteristics, specifically CNA level, is associated with the relationship between obesity and pressure ulcers.
METHODS
Data and study population
This study used the Minimum Data Set (MDS) data for all NH residents in Medicare or Medicaid certified U.S. NHs from 1999 to 2009. Resident assessments are required at admission and at least quarterly thereafter, as long as the resident remains in the NH. The MDS contains residents’ socio-demographic characteristics and detailed information about their health conditions. The Online Survey, Certification and Reporting (OSCAR) data containing information from annual Medicare/Medicaid certification surveys of NHs were matched with the MDS assessments by facility identifiers and by year. The OSCAR contains facility level characteristics, such as information about staffing levels in NHs.
We identified all residents who were newly admitted to NHs between 2000 and 2008. Newly admitted residents were defined as those who did not have any NH stay in the prior year (i.e. no MDS records in the prior year). The new admission cohort allowed us to control for individuals’ health conditions that were beyond NHs’ control (i.e. health conditions at admission), and thus protected the analyses against over-adjustment of the NH’s quality of care. The few residents who had multiple “new” admissions during the study period were represented once by randomly selecting one admission. We followed the new admission cohort for up to one year. Thus study accrual was between 2000 and 2008 with 1999 data used to identify new NH admissions in 2000 and 2009 records used to obtain one year follow up information for 2008 cohort. We further identified residents whose NH stay lasted over 90 days (as evidenced by a quarterly or annual MDS assessment), and they were considered “long-stayers”. We selected this cohort because as compared with short-term residents, the presence of pressure ulcers among long-stay residents was more likely to be a reflection of the quality of care in the NH.(25)
We identified 10,663,317 new admissions between the years 2000 to 2008. As we were interested in the effects of obesity, we excluded residents who were underweight ( BMI <18.5 kg/m2). (26) Our final sample included 2,217,961 newly admitted residents who became long-stayers.
Variables
Outcome variable
The outcome variable was dichotomous, defined as the presence of any pressure ulcers (at any stage) on quarterly or annual assessments during a one-year follow-up period. MDS assessments record the pressure ulcer conditions within 7 days prior to the assessment date. We used the prevalence of pressure ulcers because pressure ulcers are potentially treatable and the prevalence is commonly used as a quality indicator.(25)
Independent variables of interest
We obtained residents’ height and weight from the MDS admission assessments and calculated their BMI index, defined as kg/m2. We excluded residents who were underweight (BMI<18.5 kg/m2). Based on their BMI index, we classified residents into three groups: mild obesity (30 <= BMI <35 kg/m2), moderate to severe obesity (BMI>=35 kg/m2) and not obese ( 18.5 <= BMI <30 kg/m2 ). (26)
Control variables
We controlled for residents’ pressure ulcer status at admission, as well as other health conditions at admission that could be associated with the occurrence of pressure ulcers, including bed mobility (whether a resident needs extensive help or totally dependent), activities of daily living (ADL) scale (ranging from 0 to 28 with 0 indicating total independence and 28 indicating total dependence), severe cognitive impairment (cognitive performance scale [CPS]>=4), bowel or bladder incontinence, use of psychotic medications, terminal disease conditions, use of physical restraints, and co-morbidities (diabetes, stroke, dementia, cancer, heart disease, asthma or chronic obstructive pulmonary disease). We further controlled for individual socio-demographic characteristics (age, gender, and race coded as black, white, and other races). Finally, we controlled for secular time trend by including annual indicators based on year of admission.
Facility certified nurse assistant (CNA) staffing level, measured by CNA hours per resident per day, was obtained from OSCAR and was used to stratify our analysis, as will be discussed below.
Statistical Analysis
Descriptive analysis
We first examined the prevalence of obesity at admission among all newly admitted NH residents over a 9-year period (2000–2008). We then examined individual characteristics among the newly admitted residents who became long-stayers. We obtained individual socio-demographic characteristics and health status at the time of their initial admission and compared these measures among non-obese, mildly obese and moderately or severely obese residents.
The relationship between obesity and pressure ulcers
Two types of analyses – pooled and stratified analyses – were performed to examine the relationship between obesity and pressure ulcers among long-stay residents, and whether such relationship varied by NH characteristics. All analyses used individual as the unit of analysis and adjusted for individual conditions measured at admission. The pooled analyses fit regression models by using all eligible residents across all NHs. We first used a logit model to examine the overall relationship between obesity and pressure ulcers among all residents, regardless of the facility in which they resided. We then fit a conditional fixed-effects logit model to account for NH effects and examine the difference in the odds of pressure ulcers between obese and non-obese residents within facilities. The conditional fixed-effects logit model accounts for the heterogeneity of facilities (27, 28) – that is, the difference in facilities’ overall quality of care and pressure ulcer rates. The advantage of this model is that it accounts for unobserved facility effects and provides consistent estimates without requiring assumptions of the distribution of unobserved facility effects or the correlation between unobserved facility effects and other covariates. In contrast, a random-effects model requires unobserved facility effects to be independent of other covariates, and the violation of this assumption may result in inconsistent estimates.(28)
Secondly, we performed a stratified analysis to examine whether the within-facility difference in pressure ulcers between obese and non-obese residents varied across facilities with different CNA staffing levels. The within-facility differences in pressure ulcers between obese and non-obese residents could be caused by two possible reasons. First, it may be caused by the underlying physiologic relationship between pressure ulcers and obesity – that is, obese residents are more likely to develop pressure ulcers than non-obese residents because of inherent obesity related health conditions. Secondly, it may arise from the different levels of care received by obese and non-obese residents within a facility. While we were not able to directly differentiate these two reasons, we tested the hypothesis that the relationship between obesity and pressure ulcers was exclusively caused by physiologic mechanism – that is, the within-facility difference between obese and non-obese residents should not vary across NHs. The rejection of this hypothesis implies the role of NH in the relationship between obesity and pressure ulcers. To test this hypothesis, we stratified NHs into three strata according to their CNA staffing level. The stratification was based on the distribution of CNA hours per resident per day in each facility (top 25 percentile [>=2.52 hours per resident per day], bottom 25 percentile [<=1.76 hours per resident per day], versus all others). We chose to use CNA staffing level to stratify the analysis because most pressure ulcer care relied primarily on CNAs. Therefore, NHs with a lower level of CNA staffing may not be able to provide good care in preventing pressure ulcer as well as NHs with higher CNA staffing levels. We repeated the conditional fixed-effects logit model in each stratum and tested whether the estimates of obesity varied across the subgroups. If the within-facility difference in the odds of having pressure ulcers between obese and non-obese residents varies by facility CNA level, it implies that the relationship between obesity and pressure ulcers is not exclusively caused by physiologic mechanism and NH attributes also matters.
Finally, in order to check the robustness of our findings, we performed the same set of analyses on the incidence of new pressure ulcers using a subset of the sample who did not have pressure ulcers at admission, and examining whether they developed any pressure ulcers in the follow-up period.
All these analyses were performed by STATA 11. The conditional fixed-effects models were performed by XTLOGIT procedure, and test of coefficients across models was performed by SUEST procedure.
RESULTS
Descriptive analysis
The prevalence of obesity in NHs increased substantially among newly admitted NH residents over the 9-year period. Specifically, the proportion of newly admitted NH residents with mild obesity (35>BMI>=30 kg/m2) increased from 10.2 % in the year 2000 to 13.9 % in the year 2008, and the proportion of newly admitted NH residents with moderate or severe obesity (BMI >=35 kg/m2) increased from 6.7 % to 11.9 % during the same time period (Figure 1).
Figure 1.
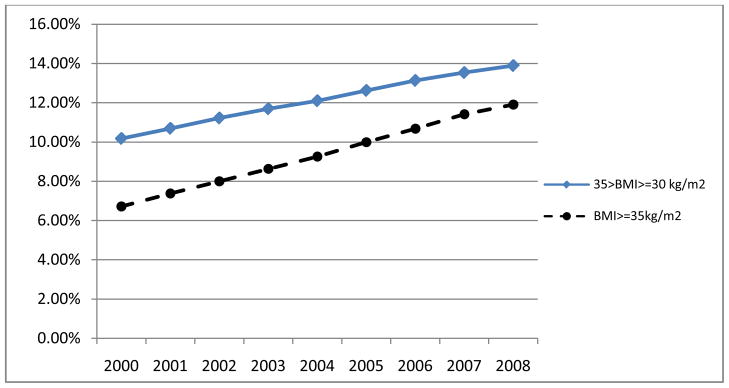
Prevalence of obesity among newly admitted NH residents, 2000–2008 (N=10,663,317 )
Among the newly admitted residents, 24.8% of non-obese residents (N=1,789,655), 19.9% of mildly obese residents (N=257,368), and 17.1% of moderately or severely obese residents became long-stayers (N=170,938). Table 1 presents individual characteristics (i.e. control variables for regression models) among residents who became long-stayers, stratified by their obesity status. Compared with non-obese residents, obese residents were younger, more likely to be female and black. As expected, residents with moderate or severe obesity were more likely to have bed mobility problems as compared with non-obese residents. However, they were less likely to have cognitive impairment, less likely to have incontinence and less likely to use physical restraints than non-obese residents. The distributions of co-morbidities were also different between obese and non-obese residents. Residents with moderate or severe obesity were more likely to have diabetes, heart and lung problems, but less likely to have cancer or dementia, as compared with non-obese residents.
Table 1.
Individual characteristics among non-obese, mildly obese and moderately or severely obese residents who became long-stayers based on measures at time of admission 2000–2008 (N=2,217,961)
| Non-obese residents (18.5 <= BMI <30kg/m2) | Residents with mild obesity (30<=BMI<35 kg/m2) | Residents with moderate or severe obesity (BMI>=35 kg/m2) | |
|---|---|---|---|
| No. of observations | 1,789,655 | 257,368 | 170,938 |
| Age | 79.98(12.60) | 76.10 (13.18) | 70.27(14.00) |
| Male | 35.82% | 32.33% | 24.97% |
| Black | 11.41% | 12.65% | 15.45% |
| Other race | 5.70% | 4.89% | 4.34% |
| Need extensive help with bed mobility or totally dependent | 40.79% | 43.70% | 50.80% |
| ADL (on 28 scale) | 14.80(7.73) | 14.43(7.74) | 14.98(7.61) |
| Severe cognitive impairment (CPS>=4) | 19.51% | 13.30% | 8.30% |
| Bowel Incontinence | 36.17% | 31.73% | 29.23% |
| Bladder Incontinence | 44.65% | 41.74% | 36.23% |
| Any use of antipsychotic medication | 22.49% | 22.96% | 21.12% |
| Terminal disease | 1.24% | 0.95% | 0.89% |
| Any use of restraints | 41.12% | 38.29% | 38.78% |
| Diabetes | 23.55% | 40.18% | 53.35% |
| Cancer | 7.57% | 6.70% | 5.66% |
| Stroke | 18.84% | 20.13% | 17.09% |
| Dementia | 41.04% | 31.41% | 17.88% |
| Heart disease | 34.09% | 38.41% | 41.57% |
| COPD/asthma | 14.85% | 16.91% | 23.27% |
| Having pressure ulcers at the admission time | 19.25% | 18.70% | 24.03% |
The numbers in the cell indicate percentage for categorical variables, and mean (SD) for continuous variables.
Obesity and pressure ulcers
Table 2 presents the results relating obesity status and pressure ulcers, controlling for individual health conditions at admission (all variables listed in Table 1 were controlled but were not presented in Table 2. See Appendix 1 for details). Obese residents, especially those who were moderately or severely obese, were more likely to have pressure ulcers than non-obese residents after adjusting for their health conditions at admission. This effect persisted even after accounting for overall quality of care in NHs (i.e. facility fixed-effects). As indicated by the pooled analysis in Table 2, residents with moderate or severe obesity had 15.8% higher odds of having pressure ulcers than non-obese residents if not accounting for facility effects. After accounting for facility effects, residents with moderate or severe obesity had, on average, 15.0% higher odds of having pressure ulcers as compared with non-obese residents in the same facility.
Table 2.
Association between obesity and pressure ulcers among newly admitted NH residents who became long-stayers
| Mild obesity (30<=BMI<35 kg/m2 ) | Moderate or severe obesity (BMI>= 35 kg/m2 ) | ||
|---|---|---|---|
| Pooled analysis | Overall difference (logit model) | 1.032 *** [1.020–1.045] | 1.158*** [1.142–1.174] |
| Within-facility difference (conditional fixed-effects logit model) | 1.029 *** [1.017–1.041] | 1.150*** [1.134–1.166] | |
| Stratified analysis | CNA level <=1.76 hours per resident per day (conditional fixed-effects logit model) | 1.045*** [1.019–1.072] | 1. 189*** [1.155–1.225] |
| 1.76< CNA level <2.52 hours per resident per day (conditional fixed-effects logit model) | 1.023*** [1.006–1.039] | 1.140*** [1.119–1.162] | |
| CNA level >=2.52 hours per resident per day (conditional fixed-effects logit model) | 1.033** [1.006–1.060] | 1.128*** [1.092–1.165] | |
All the variables listed in Table 1 as well as secular time trends were included in the analyses as control variables but results not shown in this table ( details are available in Appendix-1).
The numbers in the cells indicate odds ratios of having pressure ulcers among obese residents relative to non-obese residents (i.e. non-obese residents serve as the reference group). The numbers in the parentheses represent 95% confidence intervals.
The effects of moderate or severe obesity on pressure ulcers are statistically significant across the three strata (i.e. odds ratio of 1.189, 1.140 and 1.128) with P value < 0.05.
P<0.05
P<0.01
Table 2 also presents the findings from the stratified analyses (by conditional fixed-effects logit model). While the within-facility difference in the odds of having pressure ulcers between obese and non-obese residents persisted in each stratum, the magnitude of such difference varied across strata. Specifically, the adjusted odds ratio of pressure ulcers for residents with moderate or severe obesity relative to non-obese residents was 1.189 within NHs with low CNA levels, 1.140 within NHs with medium CNA levels, and 1.128 within NHs with high CNA levels. These odds ratios were statistically different (P<0.05), suggesting there were variations of within-facility relationships between pressure ulcers and moderate or severe obesity across NHs with different CNA levels.
The results from the sensitivity analyses on the cohort of residents who did not have pressure ulcers at admission were consistent with the results from our main analyses, and the relationship between obesity and pressure ulcers was even stronger. As presented in Table 3, the adjusted odds ratio of pressure ulcers for residents with moderate or severe obesity relative to non-obese residents was 1.241 within NHs with low CNA levels, 1.187 within NHs with medium CNA levels, and 1.146 within NHs with high CNA levels, respectively (the detailed results of covariates are available in Appendix-2). Consistently with the main analyses, the within-facility differences in the odds of pressure ulcers between non-obese and moderately or severely obese residents were statistically different across the strata (P<0.05).
Table 3.
Sensitivity analysis – the association of obesity and pressure ulcers among newly admitted NH residents who became long-stayers and who did not have pressure ulcers at admission
| Mild obesity (30<=BMI<35 kg/m2) | Moderate or severe obesity (BMI>= 35 kg/m2) | ||
|---|---|---|---|
| Pooled analysis | Overall difference (logit model) | 1.032 *** [1.017–1.047] | 1.192*** [1.171–1.214] |
| Within-facility difference (conditional fixed-effects logit model) | 1.031 *** [1.016–1.046] | 1.190*** [1.168–1.212] | |
| Stratified analysis | CNA level <=1.76 hours per resident per day (conditional fixed-effects logit model) | 1.055*** [1.023–1.088] | 1.241*** [1.195–1.288] |
| 1.76< CNA level <2.52 hours per resident per day (conditional fixed-effects logit model) | 1.023** [1.003–1.044] | 1.187*** [1.158–1.217] | |
| CNA level >=2.52 hours per resident per day (conditional fixed-effects logit model) | 1.028 [0.994–1.062] | 1.146*** [1.099–1.195] | |
All the variables listed in Table 1 as well as secular time trends were included in the analyses as control variables but results not shown in this table ( details are available in Appendix-2).
The numbers in the cells indicate odds ratios of having pressure ulcers among obese residents relative to non-obese residents (i.e. non-obese residents serve as the reference group). The numbers in the parentheses represent 95% confidence intervals.
The effects of moderate or severe obesity on pressure ulcers are statistically significant across the three strata (i.e. odds ratio of 1.241, 1.187 and 1.146) with P value < 0.05.
P<0.05
P<0.01
DISCUSSION
To the best of our knowledge, this is the first study to use a recent longitudinal nationwide dataset to examine the prevalence of obesity and the prospective relationship between obesity and pressure ulcers among NH residents. We found that the prevalence of obesity increased significantly among newly admitted NH residents in the last decade. Moreover, we found that obesity, especially moderate or severe obesity, was associated with higher odds of having pressure ulcers among long-stay NH residents. Such relationship was quite robust, even after controlling for other individual characteristics and overall facility quality of care. These findings suggest that there may be a physiologic relationship between moderate or severe obesity and pressure ulcers among NH residents. Therefore it may be necessary to consider obesity as a risk adjustor when evaluating the quality of care in NHs by using pressure ulcer rates. In other words, if the rate of moderate or severe obesity in a NH is not controlled, NHs with a higher proportion of moderately or severely obese residents may be penalized because they are inherently more likely to have a high prevalence of pressure ulcers.
In addition to the possible physiologic relationship between obesity and pressure ulcers, our findings also suggest the impact of NH’s characteristics on the relationship between obesity and pressure ulcers. Specifically, the within-facility difference in the odds of having pressure ulcers between moderately or severely obese and non-obese residents was smaller in NHs with a higher level of CNA staffing as compared with that in NHs with a lower level of CNA staffing. Due to their excessive body weight, moderately or severely obese residents usually require more staff hours to fulfill even a simple task such as moving around, as compared to non-obese residents.(16) Hence, the level of care required by obese residents could be higher than that required by non-obese residents to achieve the same level of pressure ulcer prevention. Facilities with lower CNA staffing levels may be even less likely to be able to provide the optimal care to their obese residents, and therefore the difference in pressure ulcer prevention between obese and non-obese residents may be even larger in such facilities.
To prevent pressure ulcers among obese residents and reduce the related complications, efforts should be focused on developing options to improve the quality of care of obese residents. However, caring for obese residents is challenging for NHs. Obese residents, especially those with moderate or severe obesity, often require personal care assistance from more than one provider to perform activities of daily living because of their heavy body weight and immobility.(3)(16) The need for care by more than a single provider increases the need for coordination of care among several caregivers, making the scheduling of care even more complicated. In addition to the staffing burden, NHs need special equipment and space to accommodate obese residents. (29, 30) Equipment, such as for lifting, is not only important for providing accommodation to obese residents, but also important to prevent injuries of staff caring for obese residents.(31) Staff injuries are not only costly but also affect staff satisfaction, which consequently influence the quality of care delivered to residents. Thus, caring for obese residents incur higher costs to NHs due to the additional needs in staff time, space, and supplies.
One strategy that may help improve the care of obese residents is to incorporate obesity as an adjuster in case-mix reimbursement. In this way, facilities with a higher proportion of obese residents will be more likely to receive reimbursement for care commensurate with the needs of their obese residents. Better reimbursement can potentially help NHs invest in the resources needed to care for their obese residents. However, a change in reimbursement strategy should be combined with quality monitoring efforts. Previous studies have demonstrated that case-mix reimbursement creates a financial incentive to “cherry picking”, and does not necessarily translates into better quality of care. (32, 33)
It has also been suggested that special care units with specialized equipment and specially trained staff for obese residents may be an alternative to ensure optimal care for these residents.(16) However, the economic consequence of providing special care, and in particular to obese residents is unclear. While one study found that within a given facility, specialty care unit was not related to a higher level of resource use (except for the initial investment in developing the special care unit), (34) another study indicated that the use of special care units was significantly related to the use of more direct care resources.(35)
Several limitations need to be noted. First, our analysis focused only on residents who become long-stayers. These residents may be quite different from other residents admitted to NHs for short-stays. Hence, our study may not represent the general obese NH populations, especially those who are discharged from NH in a short time period. However, we consider NH attributes more relevant to the prevention and treatment of pressure ulcers among long-stayers while the prevalence of pressure ulcers among short-stayers could be a result of care provided outside of the NH, such as the discharging hospitals.(25) Moreover, the relationship between pressure ulcers and obesity among long-stayers may have the same implication for short-stayers. Secondly, this study did not examine the reoccurrence of pressure ulcers for obese and non-obese NH residents, which may provide additional information about the relationship between NH staffing and pressure ulcer risks among obese NH residents. Thirdly, although we found CNA staffing levels can modify the relationship between obesity and the occurrence of pressure ulcers, we were not able to draw the causal relationship between CNA staffing level and the risk of pressure ulcers experienced by obese residents. Some other facility characteristics, such as ownership, may affect the CNA staffing levels as well as the prevalence of pressure ulcers in NHs. Therefore, at this stage, it may not be appropriate to simply recommend NHs to invest in CNAs. However, based on the literature which shows the important role of CNA in providing care to obese residents and pressure ulcer prevention, we believe our study implies the potential important role of CNA staffing level in pressure ulcer prevention among obese NH residents. Future studies are warranted to differentiate the impact of different facility factors on pressure ulcer risks among obese residents. Fourthly, we did not examine the effects of time-varying covariates on the development of pressure ulcers since we were not able to differentiate whether time-varying covariates were the consequence of facility effects or underlying disease conditions. Lastly, as the quality of care in NHs is multi-dimensional, and association between quality performance in different areas is not always clear(36). Therefore, future research should extend this research to other quality indicators (e.g. falls).
In conclusion, the increasing prevalence of obesity affects multiple health care settings, including NHs. To prepare for the rising rate of obesity in health care settings, policies and practice strategies should be developed in order to improve the quality of care of obese residents. Methods to evaluate the costs and benefits of the potential approaches should also be examined.
Acknowledgments
We gratefully acknowledge funding from the National Institute on Aging Grant P01AG027296.
Appendix 1. Association between obesity and pressure ulcers among newly admitted NH residents who became long-stayers
| Pooled analysis | Stratified analysis | ||||
|---|---|---|---|---|---|
| Overall difference (Logit model) | Within-facility difference (conditional fixed- effects Logit model) | CNA level <=1.76 hours per resident per day (conditional fixed- effects Logit model) | 1.76< CNA level <2.52 hours per resident per day (conditional fixed- effects Logit model) | CNA level >=2.52 hours per resident per day (conditional fixed- effects Logit model) | |
| Residents with mild obesity (30<=BMI<35 kg/m2) | 1.032*** (1.020 – 1.045) | 1.029*** (1.017 – 1.041) | 1.045*** (1.019–1.072) | 1.023*** (1.006–1.039) | 1.033** (1.006–1.060) |
| Residents with moderate or severe obesity(BMI>=35 kg/m2) | 1.158*** (1.142 – 1.174) | 1.150*** (1.134–1.166) | 1.189*** (1.155–1.225) | 1.140*** (1.119–1.162) | 1.128*** (1.092–1.165 ) |
| Age | 0.996*** (0.994 – 0.998) | 0.991*** (0.989–0.993) | 0.993*** (0.989–0.998) | 0.990*** (0.987–0.994) | 0.988*** (0.983–0.992) |
| Age (squared term) | 1.000*** (1.000 - 1.000) | 1.000*** (1.000-1.000) | 1.000*** (1.000-1.000) | 1.000*** (1.000-1.000) | 1.000*** (1.000-1.000) |
| Male | 1.252*** (1.242 – 1.262) | 1.259*** (1.249–1.270) | 1.249*** (1.228–1.271) | 1.259*** (1.245–1.273) | 1.275*** (1.252–1.297) |
| Black | 1.117*** (1.105 – 1.130) | 1.115*** (1.099–1.131) | 1.097*** (1.065–1.130) | 1.119*** (1.098–1.141) | 1.119*** (1.084–1.156) |
| Other race | 0.790*** (0.777 – 0.804) | 0.858*** (0.841–0.876) | 0.887*** (0.849–0.926) | 0.851*** (0.827–0.876) | 0.842*** (0.807–0.879) |
| Need extensive help with bed mobility or totally dependent | 1.102*** (1.090 – 1.114) | 1.101*** (1.089–1.114) | 1.082*** (1.056–1.109) | 1.115*** (1.097–1.132) | 1.108*** (1.081–1.137) |
| ADL (on 28 scale) | 1.053*** (1.053 – 1.054) | 1.054*** (1.053–1.055) | 1.058*** (1.056–1.060) | 1.054*** (1.053–1.056) | 1.049*** (1.047–1.051) |
| Severe cognitive impairment (CPS>=4) | 0.977*** (0.967 – 0.987) | 0.989* (0.979–1.000) | 1.001 (0.978–1.025) | 0.991 (0.976–1.005) | 0.975** (0.953–0.998) |
| Bowel Incontinence | 1.236*** (1.224 – 1.248) | 1.242*** (1.230–1.255) | 1.245*** (1.217–1.273) | 1.243*** (1.226–1.261) | 1.228*** (1.201–1.255) |
| Bladder Incontinence | 0.834*** (0.827 – 0.842) | 0.834*** (0.827–0.842) | 0.848*** (0.832–0.865) | 0.830*** (0.820–0.840) | 0.832*** (0.817–0.849) |
| Any use of antipsychotic medication | 0.965*** (0.955 – 0.974) | 0.988** (0.978–0.998) | 0.972** (0.952–0.994) | 0.985** (0.972–0.998) | 1.007 (0.985–1.029) |
| Terminal disease | 1.162*** (1.125 – 1.199) | 1.176*** (1.138–1.214) | 1.231*** (1.147–1.320) | 1.165*** (1.114–1.219) | 1.143*** (1.071–1.220) |
| Any use of restraints | 1.044*** (1.035 – 1.052) | 1.052*** (1.042–1.063) | 1.078*** (1.055–1.101) | 1.050*** (1.036–1.064) | 1.021* (0.999–1.044) |
| Diabetes | 1.461*** (1.449 – 1.473) | 1.457*** (1.445–1.470) | 1.454*** (1.428–1.480) | 1.463*** (1.446–1.480) | 1.449*** (1.422–1.476) |
| Cancer | 1.033*** (1.018 – 1.047) | 1.016** (1.001–1.030) | 1.030* (0.999–1.063) | 1.002 (0.983–1.022) | 1.042*** (1.010–1.075) |
| Stroke | 0.848*** (0.840 – 0.856) | 0.841*** (0.832–0.849) | 0.849*** (0.831–0.867) | 0.841*** (0.830–0.852) | 0.827*** (0.810–0.845) |
| Dementia | 0.876*** (0.869 – 0.884) | 0.872*** (0.865–0.880) | 0.885*** (0.868–0.902) | 0.874*** (0.864–0.885) | 0.861*** (0.845–0.878) |
| Heart disease | 1.106*** (1.098 – 1.115) | 1.098*** (1.089–1.107) | 1.101*** (1.082–1.120) | 1.093*** (1.081–1.105) | 1.106*** (1.087–1.126) |
| COPD/asthma | 0.919*** (0.910 – 0.929) | 0.911*** (0.902–0.921) | 0.916*** (0.895–0.937) | 0.902*** (0.889–0.915) | 0.934*** (0.913–0.956) |
| Having pressure ulcers at the admission time | 4.393*** (4.358 – 4.428) | 4.310*** ( 4.275 – 4.346) | 4.585*** (4.503 – 4.669) | 4.236*** (4.189–4.284) | 4.202*** (4.127–4.277) |
| Year (2001) | 1.040*** (1.024 – 1.057) | 1.039*** (1.022–1.056) | 1.018 (0.983–1.054) | 1.040*** (1.017–1.064) | 1.052** (1.005–1.101) |
| Year (2002) | 1.161*** (1.143 – 1.179) | 1.161*** (1.142–1.179) | 1.099*** (1.059–1.141) | 1.173*** (1.147–1.199) | 1.206*** (1.154–1.260) |
| Year (2003) | 1.135*** (1.117 – 1.153) | 1.131*** (1.113–1.150) | 1.146*** (1.103–1.191) | 1.136*** (1.111–1.163) | 1.129*** (1.080–1.179) |
| Year (2004) | 1.057*** (1.040 – 1.074) | 1.054*** (1.037–1.071) | 1.016 (0.975–1.058) | 1.066*** (1.042–1.091) | 1.052** (1.006–1.100) |
| Year (2005) | 1.003 (0.987 – 1.019) | 0.999 (0.983–1.016) | 0.967 (0.928–1.008) | 1.008 (0.985–1.032) | 1.003 (0.959–1.050) |
| Year (2006) | 0.964*** (0.948 – 0.980) | 0.962*** (0.946–0.978) | 0.975 (0.935–1.016) | 0.959*** (0.936–0.982) | 0.965*** (0.922–1.010) |
| Year (2007) | 0.913*** (0.898 – 0.929) | 0.912*** (0.896–0.927) | 0.911*** (0.875–0.948) | 0.918*** (0.896–0.941) | 0.902*** (0.861–0.945 ) |
| Year (2008) | 0.890*** (0.875 – 0.905) | 0.890*** (0.875–0.906) | 0.875*** (0.842–0.908) | 0.886*** (0.862 – 0.911) | 0.898*** (0.855–0.944) |
The numbers in the cells indicate odds ratios. The numbers in the parentheses indicate 95% confidence interval. Non-obese residents serve as the reference group.
P<0.05,
P<0.01
Appendix 2. Sensitivity analysis: the association of obesity and pressure ulcers among newly admitted NH residents who became long-stayers and who did not have pressure ulcers at admission
| Pooled analysis | Stratified analysis | ||||
|---|---|---|---|---|---|
| Overall difference (Logit model) | Within-facility difference (conditional fixed- effects Logit model) | CNA level <=1.76 hours per residents per day (conditional fixed- effects Logit model) | 1.76< CNA level <2.52 hours per resident per day (conditional fixed- effects Logit model) | CNA level >=2.52 hours per resident per day (conditional fixed- effects Logit model) | |
| Residents with mild obesity (30<=BMI<35 kg/m2) | 1.032*** (1.017–1.047) | 1.031*** (1.016–1.046) | 1.055*** (1.023–1.088) | 1.023** (1.003–1.044) | 1.028 (0.994–1.062) |
| Residents with moderate or severe obesity (BMI>=35 kg/m2) | 1.192*** (1.171–1.214) | 1.190*** (1.168–1.212) | 1.241*** (1.195 – 1.288) | 1.187*** (1.158–1.217) | 1.146*** (1.099–1.195) |
| Age | 1.013*** (1.010–1.016) | 1.007*** (1.003–1.010) | 1.010*** (1.003–1.016) | 1.007*** (1.003–1.012) | 0.999 (0.992–1.006) |
| Age (squared term) | 1.000 (1.000–1.000) | 1.000*** (1.000–1.000) | 1.000 (1.000–1.000) | 1.000* (1.000–1.000) | 1.000*** (1.000–1.000) |
| Male | 1.232*** (1.220–1.245) | 1.245*** (1.233–1.258) | 1.236*** (1.210–1.263) | 1.241*** (1.224–1.258) | 1.276*** (1.247–1.306) |
| Black | 1.030*** (1.015–1.045) | 1.044*** (1.025–1.063) | 1.046** (1.007 – 1.087) | 1.043*** (1.018–1.069) | 1.036 (0.993–1.081) |
| Other race | 0.749*** (0.732–0.766) | 0.825*** (0.803–0.848) | 0.868*** (0.820–0.918) | 0.812*** (0.782–0.844) | 0.799*** (0.754–0.846) |
| Need extensive help with bed mobility or totally dependent | 1.102*** (1.087–1.118) | 1.092*** (1.077–1.108) | 1.073*** (1.041–1.106) | 1.106*** (1.085–1.128) | 1.097*** (1.063–1.133) |
| ADL (on 28 scale) | 1.060*** (1.059–1.061) | 1.061*** (1.060–1.062) | 1.065*** (1.063–1.068) | 1.061*** (1.059–1.063) | 1.056*** (1.054–1.059) |
| Severe cognitive impairment (CPS>=4) | 0.994 (0.981–1.007) | 1.010 (0.997–1.024) | 1.027* (0.997–1.057) | 1.011 (0.993–1.029) | 1.006 (0.976–1.035) |
| Bowel Incontinence | 1.218*** (1.203–1.234) | 1.218*** (1.202–1.234) | 1.234*** (1.199–1.269) | 1.213*** (1.192–1.235) | 1.203*** (1.169–1.238) |
| Bladder Incontinence | 0.923*** (0.913–0.934) | 0.925*** (0.914–0.936) | 0.939*** (0.916–0.963) | 0.925*** (0.910–0.939) | 0.915*** (0.892–0.939) |
| Any use of antipsychotic medication | 1.014** (1.002–1.027) | 1.034*** (1.022–1.047) | 1.016 (0.990–1.043) | 1.032*** (1.015–1.049) | 1.055*** (1.027–1.084) |
| Terminal disease | 1.175*** (1.128–1.224) | 1.192*** (1.143–1.242 ) | 1.265*** (1.159–1.382) | 1.175*** (1.108–1.245) | 1.138*** (1.045–1.239) |
| Any use of restraints | 1.069*** (1.059–1.080) | 1.070*** (1.057–1.083) | 1.098*** (1.070–1.128) | 1.066*** (1.049–1.084) | 1.042*** (1.013–1.071) |
| Diabetes | 1.468*** (1.453–1.484) | 1.462*** (1.447–1.478) | 1.476*** (1.443–1.509) | 1.465*** (1.444–1.486) | 1.451*** (1.417–1.486) |
| Cancer | 1.068*** (1.050–1.087) | 1.051*** (1.033–1.070) | 1.063*** (1.023–1.105) | 1.039*** (1.014–1.065) | 1.076*** (1.035–1.120) |
| Stroke | 0.887*** (0.876–0.898) | 0.876*** (0.865–0.887) | 0.877*** (0.855–0.900) | 0.881*** (0.867–0.896) | 0.857*** (0.834–0.880) |
| Dementia | 0.875*** (0.866–0.884) | 0.870*** (0.861–0.880) | 0.890*** (0.870–0.911) | 0.875*** (0.863–0.889) | 0.844*** (0.824–0.865) |
| Heart disease | 1.119*** (1.108–1.130) | 1.111*** (1.099–1.122) | 1.107*** (1.084–1.131) | 1.108*** (1.093–1.123) | 1.120*** (1.095–1.145) |
| COPD/asthma | 0.945*** (0.932–0.957) | 0.935*** (0.923–0.948) | 0.940*** (0.914–0.967) | 0.927*** (0.911–0.944) | 0.955*** (0.927–0.984) |
| Year (2001) | 1.034*** (1.013–1.054) | 1.034*** (1.013–1.055) | 1.031 (0.988-) 1.075 | 1.028* (1.000–1.058) | 1.033 (0.976–1.094) |
| Year (2002) | 1.202*** (1.179–1.225) | 1.203*** (1.179–1.227) | 1.145*** (1.094–1.198) | 1.218*** (1.185–1.253) | 1.223*** (1.158–1.292) |
| Year (2003) | 1.171*** (1.148–1.194) | 1.176*** (1.152–1.200) | 1.216*** (1.160–1.275) | 1.168*** (1.136–1.202) | 1.165*** (1.103–1.231) |
| Year (2004) | 1.068*** (1.047–1.090) | 1.071*** (1.049–1.093) | 1.042 (0.992–1.095) | 1.078*** (1.047–1.109) | 1.054* (0.997–1.115) |
| Year (2005) | 1.009 (0.989–1.030) | 1.007 (0.987–1.029) | 0.985 (0.936–1.036) | 1.011 (0.982–1.041) | 0.994 (0.939–1.052) |
| Year (2006) | 0.964*** (0.944–0.984) | 0.963*** (0.943–0.983) | 0.977 (0.929–1.028) | 0.961*** (0.932–0.990) | 0.955 (0.901–1.011) |
| Year (2007) | 0.906*** (0.887 – 0.925) | 0.902*** (0.883–0.922) | 0.890*** (0.848–0.935) | 0.906*** (0.878–0.935) | 0.881*** (0.831–0.935) |
| Year (2008) | 0.869*** (0.851–0.888) | 0.865*** (0.847–0.885) | 0.859*** (0.820–0.899) | 0.854*** (0.825–0.885) | 0.865*** (0.813–0.920) |
The numbers in the cells indicate odds ratios. The numbers in the parentheses indicate 95% confidence interval. Non-obese residents serve as the reference group.
P<0.05,
P<0.01
Footnotes
This study does not have any potential conflicts of interest in the past three years.
This study was presented at AcademyHealth Annual Meeting 2012, Orlando
Contributor Information
Shubing Cai, Email: Shubing_Cai@brown.edu.
Momotazur Rahman, Email: momotazur_rahman@brown.edu.
Orna Intrator, Email: orna_intrator@brown.edu.
References
- 1.Flegal KM, Carroll MD, Kuczmarski RJ, et al. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord. 1998;22:39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, et al. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 3.Lapane KL, Resnik L. Obesity in nursing homes: an escalating problem. J Am Geriatr Soc. 2005;53:1386–1391. doi: 10.1111/j.1532-5415.2005.53420.x. [DOI] [PubMed] [Google Scholar]
- 4.Hills AP, Hennig EM, Byrne NM, et al. The biomechanics of adiposity--structural and functional limitations of obesity and implications for movement. Obes Rev. 2002;3:35–43. doi: 10.1046/j.1467-789x.2002.00054.x. [DOI] [PubMed] [Google Scholar]
- 5.Evers Larsson U, Mattsson E. Functional limitations linked to high body mass index, age and current pain in obese women. Int J Obes Relat Metab Disord. 2001;25:893–899. doi: 10.1038/sj.ijo.0801553. [DOI] [PubMed] [Google Scholar]
- 6.Allman RM, Goode PS, Patrick MM, et al. Pressure ulcer risk factors among hospitalized patients with activity limitation. JAMA. 1995;273:865–870. [PubMed] [Google Scholar]
- 7.Gallagher S. The challenges of obesity and skin integrity. Nurs Clin North Am. 2005;40:325–335. doi: 10.1016/j.cnur.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Gallagher SM. Morbid obesity: a chronic disease with an impact on wounds and related problems. Ostomy Wound Manage. 1997;43:18–24. 26-17. [PubMed] [Google Scholar]
- 9.Compher C, Kinosian BP, Ratcliffe SJ, et al. Obesity reduces the risk of pressure ulcers in elderly hospitalized patients. J Gerontol A Biol Sci Med Sci. 2007;62:1310–1312. doi: 10.1093/gerona/62.11.1310. [DOI] [PubMed] [Google Scholar]
- 10.Casimiro C, Garcia-de-Lorenzo A, Usan L. Prevalence of decubitus ulcer and associated risk factors in an institutionalized Spanish elderly population. Nutrition. 2002;18:408–414. doi: 10.1016/s0899-9007(01)00805-x. [DOI] [PubMed] [Google Scholar]
- 11.Baumgarten M, Margolis DJ, Localio AR, et al. Pressure ulcers among elderly patients early in the hospital stay. J Gerontol A Biol Sci Med Sci. 2006;61:749–754. doi: 10.1093/gerona/61.7.749. [DOI] [PubMed] [Google Scholar]
- 12.Smith DM. Pressure ulcers in the nursing home. Ann Intern Med. 1995;123:433–442. doi: 10.7326/0003-4819-123-6-199509150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Horn SD, Sharkey SS, Hudak S, et al. Pressure ulcer prevention in long-term-care facilities: a pilot study implementing standardized nurse aide documentation and feedback reports. Adv Skin Wound Care. 2010;23:120–131. doi: 10.1097/01.ASW.0000363516.47512.67. [DOI] [PubMed] [Google Scholar]
- 14.Barry TT, Brannon D, Mor V. Nurse aide empowerment strategies and staff stability: effects on nursing home resident outcomes. Gerontologist. 2005;45:309–317. doi: 10.1093/geront/45.3.309. [DOI] [PubMed] [Google Scholar]
- 15.Felix HC, Bradway C, Miller E, et al. Obese nursing home residents: a call to research action. J Am Geriatr Soc. 2010;58:1196–1197. doi: 10.1111/j.1532-5415.2010.02879.x. [DOI] [PubMed] [Google Scholar]
- 16.Felix HC. Personal care assistance needs of obese elders entering nursing homes. J Am Med Dir Assoc. 2008;9:319–326. doi: 10.1016/j.jamda.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Yin J, Cai X, et al. Association of race and sites of care with pressure ulcers in high-risk nursing home residents. JAMA. 2011;306:179–186. doi: 10.1001/jama.2011.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cai S, Mukamel DB, Temkin-Greener H. Pressure ulcer prevalence among black and white nursing home residents in New York state: evidence of racial disparity. Med Care. 2010;48:233–239. doi: 10.1097/MLR.0b013e3181ca2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mor V, Gruneir A, Feng Z, et al. The effect of state policies on nursing home resident outcomes. J Am Geriatr Soc. 2011;59:3–9. doi: 10.1111/j.1532-5415.2010.03230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapoor A, Kader B, Cabral H, et al. Using the case mix of pressure ulcer healing to evaluate nursing home performance. Am J Med Qual. 2008;23:342–349. doi: 10.1177/1062860608316109. [DOI] [PubMed] [Google Scholar]
- 21.Abt Associates Inc. [Accessed on Jun 6, 2012];National nursing home quality measures. 2004 https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/downloads/NHQIQMUsersManual.pdf.
- 22.Grabowski DC, Angelelli JJ. The relationship of Medicaid payment rates, bed constraint policies, and risk-adjusted pressure ulcers. Health Serv Res. 2004;39:793–812. doi: 10.1111/j.1475-6773.2004.00258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gruneir A, Mor V. Nursing home safety: current issues and barriers to improvement. Annu Rev Public Health. 2008;29:369–382. doi: 10.1146/annurev.publhealth.29.020907.090912. [DOI] [PubMed] [Google Scholar]
- 24.Allman RM. Pressure ulcer prevalence, incidence, risk factors, and impact. Clin Geriatr Med. 1997;13:421–436. [PubMed] [Google Scholar]
- 25.Agency for Healthcare Research and Quality. [Accessed on June 6,2012];National Healthcare Quality Report. 2010 http://www.ahrq.gov/qual/nhqr10/nhqr10.pdf.
- 26.National Heart; Lung; and Blood Institute Obesity Education Intiative. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Bethesda, MD: National Institutes of Health; 1998. [PubMed] [Google Scholar]
- 27.Chamberlain G. Analysis of covariance with qualitative data. Review of Economic Studies. 1980;47:13. [Google Scholar]
- 28.Greene WH. Econometric Analysis. (5) 2002;21 [Google Scholar]
- 29.Pemberton V, Turner V, VanGilder C. The effect of using a low-air-loss surface on the skin integrity of obese patients: results of a pilot study. Ostomy Wound Manage. 2009;55:44–48. [PubMed] [Google Scholar]
- 30.Green SM, Gillett A. Caring for patients with morbid obesity in hospital. Br J Nurs. 1998;7:785–792. doi: 10.12968/bjon.1998.7.13.5650. [DOI] [PubMed] [Google Scholar]
- 31.Lapane KL, Resnik L. Weighing the relevant issues: obesity in nursing homes. J Aging Soc Policy. 2006;18:1–9. doi: 10.1300/J031v18n02_01. [DOI] [PubMed] [Google Scholar]
- 32.Feng Z, Grabowski DC, Intrator O, et al. Medicaid payment rates, case-mix reimbursement, and nursing home staffing--1996–2004. Med Care. 2008;46:33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- 33.Feng Z, Grabowski DC, Intrator O, et al. The effect of state medicaid case-mix payment on nursing home resident acuity. Health Serv Res. 2006;41:1317–1336. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mehr DR, Fries BE. Resource use on Alzheimer s special care units. Gerontologist. 1995;35:179–184. doi: 10.1093/geront/35.2.179. [DOI] [PubMed] [Google Scholar]
- 35.Arling G, Williams AR. Cognitive impairment and resource use of nursing home residents: a structural equation model. Med Care. 2003;41:802–812. doi: 10.1097/00005650-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Mukamel DB. Risk-adjusted outcome measures and quality of care in nursing homes. Med Care. 1997;35:367–385. doi: 10.1097/00005650-199704000-00007. [DOI] [PubMed] [Google Scholar]


