Abstract
To develop and refine interventions to prevent youth suicide, knowledge is needed about specific processes that reduce risk at a population level. Using a cross-sectional design, the present study tested hypotheses regarding associations between self-reported suicide attempts, emotion regulation difficulties, and positive youth-adult relationships among 7,978 high-school students (48.6% male, 49.9% female) in 30 high schools from predominantly rural, low-income communities. 683 students (8.6%) reported a past-year suicide attempt. Emotion regulation difficulties and a lack of trusted adults at home and school were associated with increased risk for making a past-year suicide attempt, above and beyond the effects of depressive symptoms and demographic factors. The association between emotion regulation difficulties and suicide attempts was modestly lower among students who perceived themselves as having higher levels of trusted adults in the family, consistent with a protective effect. Having a trusted adult in the community (outside of school and family) was associated with fewer suicide attempts in models that controlled only for demographic covariates, but not when taking symptoms of depression into account. These findings point to adolescent emotion regulation and relationships with trusted adults as complementary targets for suicide prevention that merit further intervention studies. Reaching these targets in a broad population of adolescents will require new delivery systems and “option rich” intervention designs.
Keywords: youth suicide, suicide prevention, emotion regulation, youth-adult relationships, youth-adult communication, underserved populations, suicide attempts
Introduction
Suicide is the third leading cause of death among 10–24 year olds in the US, and 5–8% of adolescents attempt suicide each year (Centers for Disease Control and Prevention, 2012). Rates of suicide and suicide attempts increase dramatically during adolescence. From ages 14 to 20, the suicide rate rises from 2.64 to 12.93 per 100,000 (Centers for Disease Control and Prevention, 2012). Reducing youth suicidal behavior has been named a national priority for over a decade (U.S. Dept. of Health and Human Services, 2001), yet rates of suicide have not declined (Centers for Disease Control and Prevention, 2012; Suicide Prevention Resource Center and Suicide Prevention Action Network USA, 2010). New approaches are needed to complement existing strategies to address the serious problem of youth suicide (Gould, Greenberg, Velting, & Shaffer, 2003; Nock, 2012; U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention, 2012).
Current suicide prevention strategies that rely on identifying youth who are already suicidal or are in high risk groups and referring them for treatment (Gould et al., 2003) are unlikely to be sufficient for lowering suicide rates in the population due to minimal help seeking by adolescents and lack of accessible mental health services (Pisani et al., 2012; Wyman et al., 2008). These barriers are particularly relevant in rural and underserved communities, which have 2–10 times higher youth suicide rates (Brown, Wyman, Brinales, & Gibbons, 2007) and lower utilization of services even where access is available (Bringewatt & Gershoff, 2010; Cohen & Hesselbart, 1993; Simons & Gaher, 2005). One strategy for addressing these limitations involves focusing preventive interventions at a population level and on modifying developmentally-salient risk and protective processes, such as enhancing help-seeking norms, coping skills, and youth-adult communication (Pisani et al., 2012). This approach holds promise for suicide reduction in the adolescent population (Aseltine Jr & DeMartino, 2004; Wyman et al., 2010). To develop and refine interventions for youth suicide, more knowledge is needed about specific processes that reduce risk, especially those that can be applied broadly.
The present study’s aim was to expand knowledge about risk-reduction processes by examining aspects of an emerging model for preventing suicidal behavior, one that centers on strengthening adolescent skills in regulating emotions and social resources for managing emotional distress. While there is no single pathway to suicidal behavior, unmanageable emotional distress may be a common antecedent (Shneidman, 1996; Wyman et al., 2009). Suicidal behavior typically occurs when enduring risk factors and immediate stressors combine, producing intolerable emotional distress from which the adolescent can see no escape (Baumeister, 1990; Goldston, Reboussin, & Daniel, 2006; Williams & Pollock, 2008). Thus, building adolescents’ capacity to identify, manage, and recover from painful emotions, using internal strategies and support from key adults, may be critical in disrupting trajectories toward suicide in the population. The present study lays the groundwork for testing this emerging population-oriented prevention model by examining the associations between difficulties with emotion regulation, having trusted adults to turn to in key social settings, and suicide attempts.
In considering adolescents’ ability to regulate emotions and tolerate distress, it is important to recognize that emotion regulation is a multidimensional construct. It includes awareness, clarity, and acceptance of emotions, as well as having strategies for responding to emotions, and harnessing them toward the accomplishment of a healthy goal, such as getting help or trying to feel better (Cole, Martin, & Dennis, 2004; Gratz & Roemer, 2004; Thompson, 1994). Maladaptive emotion regulation processes have been linked to key risk factors for suicide: depression, (Forbes & Dahl, 2005; Jacobson, Marrocco, Kleinman, & Gould, 2010; Silk, Steinberg, & Morris, 2003), anxiety (Carthy, Horesh, Apter, Edge, & Gross, 2010; Goldin, Manber, Hakimi, Canli, & Gross, 2009), antisocial behavior (Beauchaine, Gatzke-Kopp, & Mead, 2007; Hinshaw, 2002), borderline personality disorder (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006), and drug use (Kuntsche, Knibbe, Engels, & Gmel, 2007). Two dimensions of emotion regulation that are linked to suicide risk are: the ability to identify and understand one’s emotions when upset (emotional clarity), and having the means to respond to and recover from emotional upset (access to effective strategies) (Gratz & Roemer, 2004; Neumann, Van Lier, Gratz, & Koot, 2010). Lack of emotional clarity is associated with increased depression and increased risk for suicide ideation among adolescents (Weinberg & Klonsky, 2009). A related construct, restrictive emotionality (difficulty and fears about expressing feelings), has been associated with elevated depressive symptoms and suicide ideation and found to partially mediate the association between the two (Jacobson et al., 2010). Suicide ideation also has been linked to a lack of strategies to regulate emotions in adolescents (Weinberg & Klonsky, 2009). In a sample of college students, perceived limited access to emotion regulation strategies was associated with suicide ideation, and differentiated among students with a history of single vs. multiple suicide attempts (Rajappa, Gallagher, & Miranda, 2011). In a clinical sample of adolescents, Cha & Nock (Cha & Nock, 2009) showed that the effect of childhood trauma on suicide ideation and suicide attempts was moderated by the ability to perceive, understand, and manage emotions, such that the effect was strongest among adolescents with poor emotional skills and weakest among those with greater emotional skills.
The existing literature examining the role of emotion regulation in depression and suicide risk has generally not taken adolescents’ relationships into account, despite extensive evidence about the importance of family, school, and other adult support in adolescent development. Having help and support from adults in key social settings may be especially important in disadvantaged communities where youth bear an unequal burden of psychosocial risk (Braveman & Barclay, 2009; Marmot et al., 2008), and where access to mental health care may be limited by geographic and financial constraints, as well as by adolescent and family preferences (Bringewatt & Gershoff, 2010; Cohen & Hesselbart, 1993; Simons & Gaher, 2005).
Family relationships are critical for the development and ongoing support of emotion regulation and related skills (Bariola, Hughes, & Gullone, 2011; Hunter et al., 2010). Emotion regulation strategies are learned through intimate bonds between parents and their offspring (Morris, Silk, Steinberg, Myers, & Robinson, 2007), and parents have an enduring and pervasive role in supporting emotional coping throughout adolescence and into young adulthood (Ackard, Neumark-Sztainer, Story, & Perry, 2006; Fingerman, Miller, Birditt, & Zarit, 2009; Mcneely & Barber, 2010). Furthermore, parents and other family members are the primary gatekeepers to mental health services needed (Costello, Pescosolido, Angold, & Burns, 1998; Logan & King, 2001). Adolescents who have supportive relationships with their parents and adult family members are less likely to experience depressive symptoms (Bean & Barber, 2006; Boutelle, Eisenberg, Gregory, & Neumark-Sztainer, 2009; Ge, Natsuaki, Neiderhiser, & Reiss, 2009) and suicide attempts (Kidd et al., 2006). Adolescents who die by suicide have been described as having less frequent and satisfying communication with their mothers and fathers prior to their deaths than matched adolescents in the community (Gould, Fisher, Parides, Flory, & Shaffer, 1996).
Adult relationships outside of the family also can play a protective role, and these associations have been investigated primarily with school staff. Data from the National Longitudinal Study of Adolescent Health suggests that connectedness with teachers is associated with lower levels of suicidal thoughts and behaviors (Borowsky, Ireland, & Resnick, 2001; Resnick et al., 1997), and perceived teacher caring is protective against the initiation of new suicidal thoughts and behavior (McNeely & Falci, 2004). Students with positive attitudes about seeking help from adults at school are less likely to report suicide ideation and suicide attempts (Schmeelk-Cone, Pisani, Petrova, & Wyman, 2012) and more likely to seek help from an adult for suicide ideation (Pisani et al., 2012).
Besides school, adolescents can find “arenas for comfort” (Call & Mortimer, 2001) through interest-based clubs and teams, religious and secular community organizations, and in their neighborhoods. Connections across multiple settings promote healthy adolescent emotional development, including better self-esteem and lower depression (Pedersen et al., 2005). The link between suicidal behavior and having a trusted adult in the community has received limited attention, and the role of positive adults in the community has not been examined together with emotional skills and adult relationships in other key settings. Two studies that did examine suicide ideation and non-parental adults had conflicting results; in a high-risk group, having a non-parental adult mentor during adolescence reduced the likelihood of suicide ideation in adulthood (Ahrens, DuBois, Richardson, Fan, & Lozano, 2008), whereas in a community sample, no association was found (DuBois & Silverthorn, 2005). Thus, examining adult-youth relationships together with emotion regulation is a potentially fruitful direction for discovering processes that could reduce risk of adolescent suicide in the population.
Hypotheses
In the present study, we tested hypotheses regarding associations between self-reported suicide attempts and key dimensions of emotion regulation and youth-adult relationships among high school students from underserved communities. The primary outcome of interest was self-reported suicide attempts. With respect to emotion regulation, we predicted that students with poor emotional clarity and limited access to emotion regulation strategies would be more likely to have had a recent suicide attempt. With respect to youth-adult relationships, we expected that students reporting more supportive, respectful, and trusting relationships with adults in their families, at school, and in the community would be less likely to report a recent suicide attempt. The hypothesis regarding relationships in the community was offered more tentatively because there has been less, and sometime contradictory, research on suicide risk and interaction with adults in the community. Finally, we examined the hypothesis that trusted adult relationships would moderate or “buffer” the adverse effects of emotion regulation problems on suicide attempts. We expected that students with emotion regulation difficulties who had stronger trusted adult relationships would be less likely to engage in suicidal behavior than those lacking trusted adults. The likelihood of suicide attempts should be lessened because adolescents with emotion regulation problems and relationships with trusted adults could turn to these adults, receive help, and avert crises that might otherwise arise from unmitigated emotional distress.
We predicted that these hypothesized relationships would be robust, and persist over and above depressive symptoms. Understanding and controlling for the role of depressive symptoms is essential because depression is a potent risk factor for adolescent suicide attempts (Goldston et al., 2009), and depressive symptoms are linked closely with emotion regulation (Fales et al., 2008; Garnefski & Kraaij, 2006; Hunter et al., 2010; Silk et al., 2003).
Method
Participants
Participants were 7,978 students from thirty high schools (21 in upstate New York and 9 in North Dakota) participating in a randomized trial to evaluate Sources of Strength, a universal school-based suicide-prevention program that was evaluated in a previous randomized trial (LoMurray, 2005; Wyman et al., 2010). The surveys collected for the present study were conducted at baseline only, before any school began suicide-prevention training. Schools enrolled in either the 2010–2011 or 2011–2012 school year. The schools, which were in primarily rural, small town, or micropolitan regions, were selected based on: being underserved, as reported either by county mental health departments or school administrators that described barriers to mental health services among a high proportion of their students, and a self-identified need for suicide prevention intervention. Seven of the nine North Dakota schools and 16 of the 21 New York schools served populations that were classified as rural or small-town according to RUCA scores (WWAMI Rural Health Research Center, 2004). One North Dakota school and six New York schools were classified as micropolitan. One North Dakota and nine New York schools served students in a metropolitan region. School sizes ranged from 72–1563 students. An average of 40.8% of students in the New York schools and 40.1% of students in the North Dakota schools qualified for free or reduced lunches (range 6 – 83%). Of all students invited, 80.4% participated (see Table 1 for sample description). In 28 of the schools, the entire high school population was invited to participate, and 62.8%–98.6% (median = 84.3%) completed surveys. In the two largest schools, a group representative of each school was surveyed using stratified sampling. Specifically, one-half of classrooms were selected randomly within each grade; 63.9% and 75.1% of those invited completed surveys.
Table 1.
Sample characteristics
| Total Students N (%) | % of Total With Suicide Attempt (SI) | |
|---|---|---|
|
|
||
| N | 7,978 | 683 (8.6) |
| Sex | ||
| Male | 3879 (48.6) | 245 (6.2)* |
| Female | 3977 (49.9) | 429 (11.1)* |
| Age | ||
| ≤14 | 1543 (19.3) | 120 (7.8) |
| 15 | 1922 (24.1) | 165 (8.6) |
| 16 | 1988 (24.9) | 181 (9.1) |
| 17 | 1886 (23.6) | 159 (8.4) |
| ≥18 | 592 (7.4) | 55 (9.3) |
| Race | ||
| Asian | 159 (2.0) | 22 (13.8)* |
| Black or African American | 751 (9.4) | 63 (8.4) |
| Native American | 343 (4.3) | 51 (14.9)* |
| White | 6108 (76.6) | 455 (7.5) |
| Other1 | 468 (5.9) | 73 (15.6)* |
| Ethnicity | ||
| Hispanic | 583 (7.3) | 94 (16.1)* |
| Non Hispanic | 7229 (90.6) | 582 (8.1)* |
Other was a response option offered to participants in addition to the others listed.
Differences within age, race, and ethnicity are significant (p < .05). For race, White is used as the statistical reference group.
Procedure
The University of Rochester research staff worked with school administrators to plan and coordinate surveys of each school’s student population, generally during a 1–3 day period at the beginning of the school year. Informational letters were sent to parents in advance, providing them an opportunity to decline their child’s participation (<1% declined). Students completed surveys on computers using a web-based format. Trained research staff conducted student assent/consent, administered surveys, and monitored administration conditions to assure standardization and student privacy. All students were given both oral and written instructions on how to get help with suicide concerns for themselves or for a peer during the consent process, including contact information for an adult in the community. The on-line survey also contained instructions about how to seek help from an adult at school. The survey was only available in English; non-English speaking students, or students unable to complete the survey independently, were excluded and provided an alternative activity. The University of Rochester IRB approved the protocol, which included a wavier of parent permission.
Measures
Suicide attempts
Students with at least one suicide attempt in the past 12 months were identified using an item from the Youth Risk Behavior Survey (YRBS) (Centers for Disease Control and Prevention, 2010): “During the past 12 months, how many times did you actually attempt suicide?” (1 time, 2–3 times, 4–5 times, 6 or more times). Students who reported one or more attempt were coded as having had a suicide attempt (SA) because we were interested in the occurrence of any attempt, rather than in the number of attempts in the past year. Developed for population-based assessments, the YRBS has well-established reliability and validity (Brener et al., 2002; Eaton et al., 2010), and the reliability of individual items, including the suicide attempt item, has been demonstrated for both high school students (Brener, Krug, & Simon, 2000) and middle school students (Zullig, Pun, Patton, & Ubbes, 2006).
Emotion regulation
Problems with emotion regulation were assessed using two subscales of the Difficulties in Emotion Regulation Scale (DERS) (Gratz & Roemer, 2004), a self-report measure that has well-established reliability and validity for population-based studies of adolescents (Neumann et al., 2010; Weinberg & Klonsky, 2009).
The Lack of Emotional Clarity subscale
This subscale (5 items, α = .76 in this sample) measures the adolescent’s difficulty with understanding and making sense out of his or her own emotions (example items: “I have no idea how I am feeling”, “I have difficulty making sense out of my feelings”, “I am clear about my feelings” (reverse-coded)). Items are scored on a 5-point scale ranging from 1 (almost never) to 5 (almost always).
The Limited Access to Strategies for Emotion Regulation subscale
This subscale (8 items, α = .90 in this sample) measures the degree to which an individual feels powerless to manage his or her own emotional reactions and recover from feeling upset (example items: When I am upset… “I believe I’ll remain that way for a long time”, “I know I can find a way to feel better”(reverse-coded), “I believe there is nothing I can do to feel better”, “My emotions feel overwhelming”). Items are scored on a 5-point scale ranging from 1 (almost never) to 5 (almost always).
Trusted adults in key settings
We measured adolescents’ perception of having an adult to turn to for open, honest, and safe communication across three domains of adolescent life: parents and family, school, and community. Where available, we adapted existing measures of youth-parent communication (Barnes & Olson, 1982) and of relying on trusted others (Kessler & Merikangas, 2004) to capture this relational dimension in a way that would be congruent with roles in each setting.
Trusted adult in the family
To measure adolescents’ perceptions of having a trusted adult in the family, we drew a subset of 6 items from the Open Family Communication subscale of the Parent-Adolescent Communication Scale (Barnes & Olson, 1982). The original scale, which has been used in numerous studies, had 10 items that asked separately about communication with mothers and fathers. We trimmed and adapted these items to accommodate the time constraints of a population-based survey and the expectation that many students participating in this study would be raised by a single parent or other family member. We selected six items that focused on comfort and safety with personal disclosure and used the stem, “There is a parent or other adult in my family…” (items: “I can discuss hard issues with”, “I am very satisfied with how I can communicate with”, “I can tell if I were in trouble”, “I don’t have to worry what I say to them”, “I get honest answers from”, “I can discuss problems with”). Participants responded on a four-point Likert scale that ranged from “strongly disagree” to “strongly agree”. The 6-item scale had high internal reliability (α = .94) comparable to that reported for the 10-item scale (α = .87; 4-week test-retest reliability r=.78). The six items loaded as a single factor in CFA with highly acceptable item loadings (.79–.92).
Trusted adult at school
We could find no existing scales that measured students’ perceptions of having a caring, attentive adult at school with whom to communicate about problems. Thus, to assess adolescents’ perceptions of having a trusted adult at school, we created a four-item scale (α = .90) that mirrored some of the constructs from the Trusted Adult in the Family scale, but with more emphasis on caring and trust and less on concerns about negative consequences of disclosure to a parental authority. Each of the four items began with the stem, “At school there is in adult who…” (items: “Listens to what I have to say”, “I trust”, “Cares about me”, “I can talk to about a problem”). Participants responded on a four-point Likert scale that ranged from “strongly disagree“ to “strongly agree”. The four items loaded as a single factor in CFA with highly acceptable item loadings (.79–.85).
Trusted adult in the community
To measure adolescents’ perceptions of having a trusted adult outside of school, we adapted items from the National Comorbidity Study (Kessler & Merikangas, 2004; Merikangas, Avenevoli, Costello, Koretz, & Kessler, 2009) regarding bonding with non-parental adults to form a three-item scale (α = .95). These items began with the stem, “I know an adult outside of my family and school who…” (items: “I can open up to if I need to talk about my worries”, “I can rely on if I have a serious problem”, “I feel comfortable talking with”). Participants responded on a four-point Likert scale that ranged from “strongly disagree“ to “strongly agree”. The four items loaded as a single factor in CFA with highly acceptable item loadings (.90–.93).
Depressive Symptoms
We measured core symptoms of depression in adolescence using the Short Mood and Feelings Questionnaire (SMFQ) (Angold et al., 1996; Messer et al., 1995). The SMFQ (13 items, α = .93 in this sample) has well-established content and criterion-related validity, with significant and high correlations between the SMFQ and the longer version (MFQ), the Children’s Depression Inventory, and the Diagnostic Interview Schedule for Children. Scores ranged from 0–26, with higher scores indicating more depressive symptoms.
Statistical Analyses
As a preliminary step toward testing our main hypotheses about suicide attempts, we first examined associations between emotion regulation, youth-adult relationships, and depressive symptoms. We conducted mixed-effect multiple regression tests using the XTMIXED procedure in STATA 12 (StataCorp, 2011) with school treated as a random effect to account for the nesting of participants.
To identify the contributions of emotion regulation and youth-adult relationships in predicting suicide attempts above and beyond the well-established effects of depression, the “step up” approach was used in this study. We conducted univariate, followed by multivariate, mixed-effect logistic regression tests using the XTMELOGISTIC procedure in STATA 12 to test the primary hypothesis that difficulties with emotion regulation (lack of emotional clarity and limited access to emotion-regulation strategies) and lacking trusted adults in the family, school, and community would be positively associated with suicide attempts. We first conducted univariate analyses, controlling only for sex, age, race, and Hispanic ethnicity. Second, we conducted univariate analyses that also included depressive symptoms. Third, we conducted multivariate regressions of suicide attempts on all predictors that had an association with suicide attempts when controlling for depressive symptoms. Finally, for measures of trusted adult relationships and emotion regulation difficulties that were significant in the final models, we tested trusted adult relationships as moderators between the association between emotion regulation difficulties and suicide attempts using XTMELOGISTIC procedure. For any significant interaction effects, we determined the direction the interaction effects using the MARGINS procedure in STATA 12 to examine and plot the marginal effects of the emotion regulation variable on suicide attempts in a multivariate model (Cameron & Trivedi, 2009) at different levels of trusted adult (at the mean and at +/− 1 standard deviations from the mean). The marginal effect is a measure of the strength of association between two variables. In logistic regression models, the marginal effect is the slope of the probability curve relating the independent variable (emotion regulation) to dependent variable (suicide attempts). Because this slope is not intuitive to interpret on its own, changes in marginal effect on a dichotomous dependent variable are best seen by plotting it at different fixed levels in relation to a covariate (trusted adult).
To assess the between-school-level effects of the predictors on outcomes, we calculated intra-class correlation coefficients (ICCs) for linear models predicting depressive symptoms and for logistic models predicting suicide attempts, including the same covariates as above. The ICCs in all models were ≤.06, indicating negligible school-level effects. Nevertheless, school was retained as a random effect variable in all reported models.
Results
Of 7,978 students, 683 (8.6%) reported that they had attempted suicide in the past 12 months (see Table 1). Of those who attempted suicide, 341 (50%) reported one attempt, 198 (29%) reported 2–3 attempts, and 55 (8%) reported 4–5 attempts, and 89 (13%) reported 6 or more attempts. Suicide attempts (SA) were reported more frequently by females (11.1%) than by males (6.2%) (F (1,7665)= 57.46, p<.001). The proportion of attempts differed significantly by race/ethnicity (F (4,7634)=15.95, p<.001). Compared to White students, higher rates of SA were reported by Asians (p=.023) and Native Americans (p<.001). Whites and Blacks did not differ significantly. Hispanic students reported more attempts than non-Hispanics (F (1,7626)= 43.76, p<.001). There were no significant differences in SA among the age groups.
The two scales measuring difficulties with emotion regulation were correlated highly (r =.60); the three measures of relationships with trusted adults were correlated moderately with one another (r=.34 to .48), as shown in Table 2. Difficulties with emotion regulation scales were correlated moderately to strongly with depressive symptoms, suicide attempts, and relationship variables in the expected directions. Youth-adult relationship variables showed low to moderate negative correlations with depressive symptoms and with suicide attempts. Mean scores (standard deviations) for students with vs. without SA, respectively, were as follows: trusted parent or family member, 2.61 (.89) vs. 3.15 (.74); trusted adult at school, 2.82 (.82) vs. 3.12 (.63); trusted adult in the community, 2.68 (.97) vs. 2.92 (.85); lack of emotional clarity, 2.93 (.91) vs. 2.15 (.79); and limited access to emotion regulation strategies, 2.85 (1.06) vs. 1.74 (.75).
Table 2.
Bivariate Pearson product-moment correlations among independent variables, suicide attempt, age, sex, depression.
| Trusted Adult in Family | Trusted Adult at School | Trusted Adult in Community | Lack of Emotional Clarity | Limited ER Strategies | Depression | Suicide Attempt | Age | |
|---|---|---|---|---|---|---|---|---|
| Trusted Adult at School | .34 | |||||||
| Trusted Adult in Community | .48 | .38 | ||||||
| Lack of Emotional Clarity | −.34 | −.21 | −.21 | |||||
| Limited ER Strategies | −.33 | −.17 | −.17 | .60 | ||||
| Depression | −.32 | −.18 | −.17 | .56 | .70 | |||
| Suicide Attempt | −.20 | −.13 | −.08 | .26 | .37 | .41 | ||
| Age1 | −.01 | .08 | .04 | .01 | .03 | .05 | .01 | |
| Sex2 | −.00 | −.07 | −.07 | −.12 | −.12 | −.19 | −.08 | .02 |
Grouped age categories are 1=less than or equal to 14, 2=15, 3=16, 4=17, 5= greater than or equal to 18
Gender is coded 0=female, 1=male.
Associations Between Emotion Regulation, Trusted Adults, Depressive Symptoms, and Suicide Attempts
Emotion regulation difficulties, including both lack of emotional clarity and limited access to emotion regulation strategies, and stronger adolescent perceptions of having trusted adults at home and at school were found to be related to depressive symptoms and the likelihood of suicide attempts (see Table 3). After controlling for the severity of depressive symptoms and the strength of relationships with adults, students who had limited access to effective strategies for responding to, and recovering from, emotional distress had an increased likelihood of reporting a suicide attempt across all models (see Table 3). The odds of a suicide attempt were 1.6 times greater for every one point increase in a student’s difficulties in finding effective emotion regulation strategies (OR=1.59, CI: 1.39, 1.81). Lacking emotional clarity was associated with an adolescent’s suicide attempts in univariate models, including those that controlled for depressive symptoms (OR=1.38, CI: 1.22, 1.56); however, when examined together with the other dimension of emotion regulation (with which it is strongly correlated), lacking emotional clarity was not associated independently with attempts.
Table 3.
Emotion regulation difficulties and youth-adult relationships predicting depressive symptoms and suicide attempt vs. no suicide attempt.
| Predictor | Depressive Symptoms Mixed-Effect Linear Regression |
Suicide Attempt vs. No Suicide Attempt (Mixed-Effect Logistic Regression)
|
||||||
|---|---|---|---|---|---|---|---|---|
| Multivariate | Univariate | Univariate (with Depression) | Multivariate | |||||
| β | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Emotion Regulation Difficulties | ||||||||
| Lack of Emotional Clarity | 1.28*** | (1.14, 1.42) | 2.76*** | (2.50, 3.05) | 1.38*** | (1.22, 1.56) | 1.13 | (.99, 1.29) |
| Limited ER Strategies | 3.78*** | (3.64, 3.92) | 3.17*** | (2.90, 3.45) | 1.72*** | (1.52, 1.95) | 1.59*** | (1.39, 1.81) |
| Positive Relationships with Adults | ||||||||
| Communication with parents and family | −.48*** | (−.63, −.34) | .46*** | (.41, .50) | .69*** | (.62, .78) | .76*** | (.67, .87) |
| Trusted adults at school | −.29*** | (−.45, −.13) | .53*** | (.47, .60) | .75*** | (.66, .85) | .85* | (.74, .98) |
| Trusted adults in community | −0.01 | (−.13, .12) | .74*** | (.67, .81) | .99 | (.89, 1.09) | ||
| Depression (SFMQ) | -- | -- | 1.22*** | (1.20, 1.24) | -- | -- | 1.14*** | (1.11, 1.16) |
Note: All models include gender, age, race, and hispanic ethnicity. School is entered as a random effects variable in all models to account for nesting.
p < .05.
p < .01.
p < .001.
Of the domains of youth-adult relationships, positive relationships with parents were associated most highly with reduced suicide attempts. After accounting for depressive symptoms, emotion regulation, and demographic factors, students with stronger connections to parents or other adults in their family that they saw as trustworthy, safe, and supportive were less likely (OR=0.76, CI: 0.67, 0. 87) to have had a suicide attempt within the past year. Having caring and trustworthy adults at school also significantly reduced the likelihood of a suicide attempt (OR=0.85, CI: 0.74, .98), above and beyond depressive symptoms, emotion regulation, and the youth-family communication. Having a trusted adult in the community was associated with fewer suicide attempts in models that controlled only for demographic covariates, but not in models where symptoms of depression were taken into account. This variable was therefore removed from subsequent models.
Consistent with our hypothesis that stronger trusted adult relationships would serve a protective function, having a trusting relationship with one or more family adults moderated the association between emotion regulation problems and suicide attempts. Specifically, the association between limited strategies for emotion regulation and higher rates of suicide attempts was attenuated for students who more strongly endorsed having a trusted parents or other family member (p < 0.05). This interaction effect was modest, but consistent across low and high levels of trusting relationships with parents and family members. Figure 1 illustrates this moderation effect. The plot shows the decreasing association between the marginal effect of emotion regulation difficulties on suicide attempts (shown on the Y axis) as a function of increasing perceptions of oneself as having a trusted adult in the family (shown on the X axis). Lacking strategies for emotion regulation has a weaker, though still significant, association with suicide attempts as the perceived relationship with a trusted adult in the family increases. Trusted adult relationships at school did not moderate the association between emotion regulation difficulties and suicide attempts.
Figure 1.
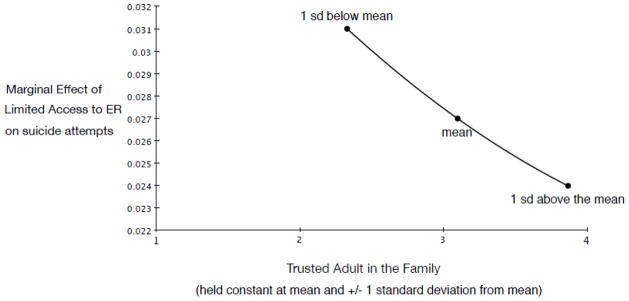
The strength of association between Limited Access to ER Strategies and suicide attempts as perception of having a trusted adult in the family increases.
Discussion
One promising strategy for reducing youth suicide is to focus preventive interventions on modifying developmentally salient risk and protective processes at a population level (Pisani et al., 2012; Wyman et al., 2010). The present study’s aim was to expand existing knowledge about the role of emotion regulation and youth-adult relationships as a key risk factor for suicide mortality–a suicide attempt–in order to lay the empirical groundwork for a population-oriented model for preventing suicide. Previous research has established links with aspects of emotion regulation and youth-adult relationships and youth suicide risk, but no study had examined these together in relationship to recent suicide attempts in a large population of high school students from underserved communities. Using a cross-sectional design, the present study examined associations between self-reported suicide attempts, emotion regulation difficulties, and trusted adult relationships in the family, school, and community. Among 7,978 high school students in 30 predominantly rural schools underserved by mental health resources, 683 (8.6%) reported a suicide attempt in the past year (11.1% of girls; 6.2% of boys). We found strong, consistent associations between lower likelihood of a suicide attempt and more frequently being able to respond and recover from emotional distress and having trusted adults in the family and at school. Although the effect of depressive symptoms on suicide attempts was strong and persistent, these preceding associations were found above and beyond the effects of depressive symptoms. Strong youth-parent communication partially buffered the association between limited emotion regulation strategies and suicide attempts. For youth who reported strong communication with a parent, the association between low emotion regulation resources and elevated suicide attempts was modestly lower than for youth with weaker communication with a parent. Having a trusted adult in the community (outside of school and family) was associated with fewer suicide attempts in models that included only this measure and demographic covariates, but not when taking depressive symptoms into account.
Our findings substantially extend previous research studies on associations between emotion regulation problems and suicide risk in adolescents (e.g., Cha & Nock, 2009; Dour, Cha, & Nock, 2011; Jacobson et al., 2010; Weinberg & Klonsky, 2009), which have examined aspects of emotion regulation without accounting for adult relationships that could aid in emotion regulation. In the present study, lacking strategies for effective emotional regulation emerged as the most potent correlate to suicide attempts. For every one point increase on a scale indicating that students perceived themselves as lacking the means to respond to and recover from emotional upset, students were 1.6 times more likely to have had a suicide attempt in the past year (OR 95% CI: 1.39 – 1.81). Adolescents who reported more frequently experiencing emotions as overwhelming and unmanageable, but who strongly perceived themselves as having an adult in the family whom they could trust and talk to, were less likely to have had a suicide attempt than those lacked such an adult. These findings are congruent with previous research pointing to the potency of having or lacking emotion regulation strategies in the emotional health of adolescents (Neumann et al., 2010; Weinberg & Klonsky, 2009), and with research with younger children showing that teaching them emotion regulation strategies improves mental health and risk behavior outcomes (Greenberg et al., 2003). Together, findings from this and other research provide a compelling rationale for testing the efficacy of enhancing adolescents’ awareness and use of external resources and self-directed skills for managing emotions as a suicide prevention measure in the population. Suggested steps for developing such interventions are discussed below.
The “buffering” effect of having a trusted adult in the family parallels findings reported by Dour et al. (2011) showing a stronger association between emotional reactivity and suicide attempts among those with poorer cognitive problem-solving skills, defined as performance on a neuropsychological executive function test. Whereas Dour et al.’s (2011) findings provided evidence of an emotion-cognition interaction leading to suicidal behavior, our present findings add evidence of an emotion- adult relationship interaction. Overall, these studies highlight the interdependence among emotional, cognitive, and relational resources during the adolescent developmental period. Taken together with other evidence that adolescents’ emotional skills could be protective against the long-term effects of major life stressors on suicidal behavior (Cha & Nock, 2009), these results suggest that promoting emotional skills together with strengthening youth-adult communication and relationships could be a fruitful direction for youth suicide prevention, as discussed below. The relative importance of parents and family is highly congruent with a previous study that compared family, school, and peer connectedness (Kaminski et al., 2009), and extends that work by comparing the effects of having trusted adults in the community, as well as in the family and at school, and by examining these relationships together with emotion regulation.
Having a trusted adult at school was associated with lower risk for suicide attempts. This finding is congruent with previous work showing that perceived teacher caring is associated with lower risk of new suicidal behavior (McNeely & Falci, 2004), and enriches the concept of “caring” by highlighting a dimension of youth-adult relationships in the school that has not previously been measured: the sense of being able to rely on and talk honestly to an adult about problems. The schools that participated this study were located in mostly rural and low-income communities. Having trusted adults at home and school is especially relevant in these communities, where families have less access to mental health services and typically are less willing to participate in services that are offered. In rural communities, the public schools play an especially important role in the social fabric (Lyson, 2002). The association between having trusted adults at school and fewer suicide attempts suggests that youth-adult relationships are an important element of the schools’ contribution to well-being in rural communities, and could be a potent target for suicide prevention (Wyman et al., 2010).
Students who had relationships with trusted adults in the community were less likely to report a suicide attempt, but this association was not statistically significant after controlling for symptoms of depression. The hypotheses regarding trusted adults in the community were offered more tentatively because, in contrast to literature relating to relationships with family and at school, there was limited evidence from the literature linking connections with adults in the community to suicide risk. Nevertheless, we expected to find a more robust association with reduced suicide attempts than what was found. One possible explanation is that some of the trusted adult relationships which adolescents reported were those that youth pursued, or were referred to, in response to inadequate support at home or school, or when other risk factors in the home or school were present. This interpretation would be congruent with previous work suggesting that the salutary effect of non-parental mentors occurs mostly among those who have the most significant risk (Zimmerman, Bingenheimer, & Notaro, 2002). Because a diversity of possible relationships and motivations may be at play, more research is needed to understand the possible protective role of trusted adults in the community.
Our findings suggest several future directions for research and prevention. This study was motivated by an emerging model for preventing suicidal behavior that centers on enhancing adolescents’ skills and resources to reduce emotional distress that is a proximate risk factor for suicidal behavior. This model posits that promoting emotion regulation skills and bolstering communication with adults in key settings, both separately and together, could prevent distress from leading to suicide attempts, especially in communities where mental health care is less accessible or acceptable. A logical next step in developing this model will be to measure immediate and accumulated stressors as well as acute emotional distress (Bagge, Glenn, & Lee, 2012) in order to test the hypothesis that emotion regulation skills and youth-adult relationships protect adolescents against suicidal behavior by helping them modulate their emotional responses to stressors known to trigger suicidal crises, such as relationship break-ups, peer and family conflicts, and victimization through violence. The potential for this future direction is further supported by a recent longitudinal study showing that reductions in perceived stress mediated the effect of emotional control strategies on reduced suicide ideation at 1 year follow-up (Khurana & Romer, 2012).
In terms of prevention, it may be helpful for intervention developers and stakeholders to consider strategies for promoting youth-parent communication and supportive parenting, which generally have not received direct focus from school and community-based suicide prevention programs (see Thompson, Eggert, Randell, & Pike, 2001 for a notable exception). Because these relationships are measured from the perspective of the adolescent, it is not known what behaviors the parents of adolescents in this study exhibited to elicit their adolescent children’s feelings of trust and security, and whether low levels of reliable, open communication reflect long-term disruptions in the parent-child relationships or reflect short-term problems; however, it is well known that effective parenting during adolescence includes encouraging autonomy, providing safe and open channels of communication, and conveying a strong sense of care and respect (Biglan, Flay, Embry, & Sandler, 2012). These parenting skills could be targeted in interventions. Furthermore, since positive early parent-child relationships promote both emotion regulation and open communication, suicide prevention could look further “upstream” to encourage and strengthen parent-child relationships at earlier developmental stages. For example, the New Beginnings Program has demonstrated remarkable long-term results in reducing many of the common risk factors for suicide (mental disorders, conduct problems, substance abuse) among children who have experienced divorce (Barber, Stoltz, & Olsen, 2005). Other programs, such as the Mother Plus Child Program, have demonstrated the potential for improving mental health outcomes through strengthening parent-child relationships (Wolchik et al., 2002), yet these models have rarely been considered under the rubric of suicide prevention.
Another important step toward developing interventions to reduce suicide will be to identify specific emotion regulation strategies that could be targeted at a population level to enhance students’ repertoire for responding to and recovering from painful emotions. Ideally, this could be done in concert with interventions that strengthen the student’s ties and foster open communication with adults at home and at school, and provide adults with complementary strategies for promoting open communication and for coaching adolescents in handling severe emotional distress. Examples from the clinical literature can be helpful in this regard. For example, dialectical behavioral therapy (DBT) (Linehan, 1993), which focuses heavily on teaching strategies for regulating emotion, has been adapted for suicidal adolescents (Miller, Rathus, & Linehan, 2007; Rathus & Miller, 2002). This adaptation includes a family skills component that teaches family members core emotion regulation skills, both to enhance generalization of adolescents’ skills through coaching at home and to improve parents’ own self-regulation skills, thereby improving the emotional environment for these suicidal youth.
To prevent new suicidal behavior, interventions with similar components to those tested in clinical interventions are needed to reach adolescents earlier and more broadly, including in geographically isolated communities. Doing so will require new intervention delivery systems and designs. With respect to delivery, helping teenagers discover and practice new emotional skills on a broad scale could be accomplished by delivering interventions via information-communication devices, such as mobile phones. A number of health-promotion interventions have harnessed mobile technology to change adolescent risk behavior (e.g., Daniels et al., 2012; Levine, McCright, Dobkin, Woodruff, & Klausner, 2008). With respect to design, interventions that target emotion regulation and youth-adult communication on a large scale will need to be exceedingly flexible. Adolescents have varying opportunities for forming relationships with adults, and available adults would have a range of capabilities. Each adolescent has and needs a different repertoire of emotion regulation strategies in order to feel that his or her emotions are manageable. Thus, prevention programs targeting emotion regulation and youth-adult relationships need to pursue empirically identified targets using option-rich interventions (OR) that can accommodate individual needs, preferences, and circumstances. This means developing interventions that offer participants ongoing options for how they will participate, in terms of content, structure, breadth and depth. Although challenging to develop, OR interventions could be especially engaging to teenagers, who prize their freedom and individuality.
Several limitations of this study should be noted. As mentioned above, this study relied on cross-sectional data gathered through self-reporting. Findings reflect correlational associations rather than causal relationships. It is possible that other unmeasured factors are responsible for the associations discovered here. Although the large sample size and rigorous survey methods bolster confidence in the findings, multi-method longitudinal and experimental work is needed to test whether enhancing adolescents’ emotion regulation skills and strengthening relationships and open communication with adults in key settings reduces rates of attempted suicide in a population. Although generally pointing to trusted adult relationships as a potential prevention target, these results need to be applied cautiously toward the goal of developing preventive interventions. One well-designed intervention that aimed to increase support for youth-adult contacts for psychiatrically hospitalized adolescents did not achieve the desired long-term results for this high-risk population (King et al., 2009)—highlighting the complexity of translating basic research to interventions and the challenges of reducing suicidal behavior.
There are other limitations of this study. A second arises because this study examined the association between retrospective reports of suicide attempts and contemporaneous reports of depressive symptoms, emotion regulation, and youth-adult relationships. It is possible that perceptions of emotion regulation and relationships were colored by past attempts or that significant emotional changes might have occurred for other reasons, including normal growth and maturation during adolescence. We also cannot be certain that the youth-adult relationships measured here preceded the suicide attempts. Third, although the YRBS suicide attempt item has well-established validity, participants could have misinterpreted the question, “how many times did you actually attempt suicide” as referring to non-suicidal self-harm in addition to suicide attempts. Fourth, while having a large sample is strength of the study, the sample size powered the study to detect small differences as significant; thus, significance levels should be interpreted cautiously and in light of effect sizes. Finally, this study was conducted in high schools in predominantly rural, low-income communities serving mostly white students. Our sample did not include non-English-speaking students and students who could not complete the survey independently--for example, those with severe cognitive disabilities. Thus, findings may not generalize to these populations and to populations with greater racial diversity.
This study lays the initial groundwork for further developing and testing population-oriented suicide prevention strategies that center on building adolescents’ capacity to manage and recover from painful emotions using self-regulation strategies and support from key adults. Results pointed to two targets that merit further examination through longitudinal research and intervention studies: access to strategies for recovering from painful emotions, and communication with trusted adults in the family and at school. Longitudinal research, new intervention delivery systems and designs, and intervention studies are needed to discover how best to reach these targets in a broad population of adolescents and whether doing so results in reduced rates of suicide among youth.
Acknowledgments
The authors wish to thank Caitlin Eberle and Jane Fitzgerald for their help collecting data and preparing tables for this manuscript.
Funding for this work: We gratefully acknowledge support from the National Institute of Mental Health (R01MH091452, K24MH066252); the University of Rochester CTSA award number KL2 RR024136 from the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health; New York State-Office of Mental Health; and the Locker Family Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or any of our other funders.
Biographies
Anthony R. Pisani is an Associate Professor of Psychiatry (Psychology) and Pediatrics at the University of Rochester Center for the Study and Prevention of Suicide, and the Wynne Center for Family Research. Dr. Pisani earned his Ph.D. in Clinical Psychology from the University of Virginia in 2001. Dr. Pisani pursues a program of research aimed at developing and testing population-oriented interventions to reduce youth suicide.
Peter A. Wyman is a Professor in the Department of Psychiatry at the University of Rochester School of Medicine and Dentistry. Dr. Wyman received his Ph.D. in Clinical Psychology from the University of Rochester in 1988. His research focuses on developing and evaluating community-based interventions that are designed to promote positive life-course trajectories in youth, prevent suicide, and reduce problems with school socialization and emotion self-regulation.
Mariya Petrova is a Health Project Coordinator in the University of Rochester (UR) Department of Psychiatry. She earned her M.S. in Mental Health Counseling from the University of Rochester. She has coordinated research activities in the UR School and Community-Based Prevention Laboratory since 2008. Her research interests include understanding how different types of pubic messaging influence adolescents’ health behavior and attitudes.
Karen Schmeelk-Cone is an Information Analyst in the Psychiatry Department at the University of Rochester Medical Center. Dr. Schmeelk-Cone received her Ph.D. in Biobehavioral Health from the Pennsylvania State University in 1999. Dr. Schmeelk-Cone has been a data analyst since 2004, working on suicide prevention studies and the Rochester Resilience Project, with a special focus on adolescent depression and suicide.
David Goldston is a clinical psychologist and Associate Professor in the Division of Medical Psychology, and Division of Child and Adolescent Psychiatry in the Department of Psychiatry and Behavioral Sciences at Duke University School of Medicine. Dr. Goldston’s research focuses on the longitudinal course, risk, assessment, prevention, and treatment of suicidal and related behaviors, and the impact of adolescent suicidal behaviors on parents.
Yinglin Xia is a Research Assistant Professor of Biostatistics in the Department of Biostatistics and Computational Biology. Dr. Xia’s areas of research interest include structural equation modeling (SEM), multi-level modeling, latent growth curve modeling (LGM), growth mixture modeling (GMM), longitudinal data analysis, mediation analysis, missing data, and mental health statistics.
Madelyn S. Gould is a Professor in Child Psychiatry and Epidemiology at Columbia University and a Research Scientist at the New York State Psychiatric Institute. She received her Ph.D. in Epidemiology from Columbia University in 1980. Her research focuses on the epidemiology of youth suicide, as well as the evaluation of youth suicide prevention interventions. Specific projects examine risk factors for teenage suicide; various aspects of cluster suicides; suicide crisis intervention programs in schools; and the effect of youth suicide screening programs.
Footnotes
AP conceived of the study, conducted most analyses, and drafted the manuscript. PW led the trial from which data are generated and participated at all stages of study design, analysis, interpretation, and manuscript preparation. MP helped to recruit schools, coordinated the study, and supervised data collection, entry, and cleaning. KS-C managed data, conducted preliminary analysis, and assisted with analytic interpretation. DG assisted interpretation of findings and helped to draft the manuscript. YX reviewed analyses and assisted in interpretation. MG contributed to the study design and manuscript preparation. All authors read and approved the final manuscript.
References
- Ackard D, Neumark-Sztainer D, Story M, Perry C. Parent-child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine. 2006;30(1):59–66. doi: 10.1016/j.amepre.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Ahrens KR, DuBois DL, Richardson LP, Fan MY, Lozano P. Youth in foster care with adult mentors during adolescence have improved adult outcomes. Pediatrics. 2008;121(2):e246–e252. doi: 10.1542/peds.2007-0508. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer S, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1996;5:237–249. [Google Scholar]
- Aseltine R, Jr, DeMartino R. An outcome evaluation of the sos suicide prevention program. American Journal of Public Health. 2004;94(3):446. doi: 10.2105/ajph.94.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagge CL, Glenn CR, Lee H-J. Quantifying the impact of recent negative life events on suicide attempts. Journal of Abnormal Psychology. 2012 doi: 10.1037/a0030371. ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- Barber BK, Stoltz HE, Olsen JA. Parental support, psychological control, and behavioral control: Assessing relevance across time, culture, and method. Monographs of the Society for Research in Child Development. 2005;70(4) doi: 10.1111/j.1540-5834.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- Bariola E, Hughes EK, Gullone E. Relationships between parent and child emotion regulation strategy use: A brief report. Journal of Child and Family Studies. 2011;21(3):443–448. doi: 10.1007/s10826-011-9497-5. [DOI] [Google Scholar]
- Barnes H, Olson D. Parent adolescent communication scale. In: Olson D, McCubbin H, Barnes H, Larsen M, Muxen M, Wilson M, editors. Family inventories: Inventories used in a national survey of families across the family life cycle. St. Paul: Family Social Science, University of Minnesota; 1982. pp. 33–48. [Google Scholar]
- Baumeister R. Suicide as escape from self. Psychological Review. 1990;97(1):90–113. doi: 10.1037/0033-295X.97.1.90. [DOI] [PubMed] [Google Scholar]
- Bean R, Barber B. Parental support, behavioral control, and psychological control among african american youth. Journal of Family Issues 2006 [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74(2):174–184. doi: 10.1016/j.biopsycho.2005.08.008. http://dx.doi.org/10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biglan A, Flay BR, Embry DD, Sandler IN. The critical role of nurturing environments for promoting human well-being. American Psychologist. 2012;67(4):257–271. doi: 10.1037/a0026796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borowsky IW, Ireland M, Resnick MD. Adolescent suicide attempts: Risks and protectors. Pediatrics. 2001;107(3):485–493. doi: 10.1542/peds.107.3.485. [DOI] [PubMed] [Google Scholar]
- Boutelle K, Eisenberg ME, Gregory ML, Neumark-Sztainer D. The reciprocal relationship between parent–child connectedness and adolescent emotional functioning over 5 years. Journal of Psychosomatic Research. 2009;66(4):309–316. doi: 10.1016/j.jpsychores.2008.10.019. [DOI] [PubMed] [Google Scholar]
- Braveman P, Barclay C. Health disparities beginning in childhood: A life-course perspective. 2009;124(Suppl 3):S163–175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2002;31(4):336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- Brener ND, Krug EG, Simon TR. Trends in suicide ideation and suicidal behavior among high school students in the united states, 1991–1997. Suicide and Life-Threatening Behavior. 2000;30(4):304–312. [PubMed] [Google Scholar]
- Bringewatt EH, Gershoff ET. Falling through the cracks: Gaps and barriers in the mental health system for america’s disadvantaged children. Children and Youth Services Review. 2010;32(10):1291–1299. doi: 10.1016/j.childyouth.2010.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CH, Wyman PA, Brinales JM, Gibbons RD. The role of randomized trials in testing interventions for the prevention of youth suicide. International Review of Psychiatry. 2007;19(6):617–631. doi: 10.1080/09540260701797779. [DOI] [PubMed] [Google Scholar]
- Call KT, Mortimer J. Arenas for comfort in adolescence: A study of adjustment in context. Mahwah, NJ: Lawrence Erlbaum; 2001. [Google Scholar]
- Cameron A, Trivedi P. Microeconomics using stata. College Station, TX: Stata Press; 2009. [Google Scholar]
- Carthy T, Horesh N, Apter A, Edge MD, Gross JJ. Emotional reactivity and cognitive regulation in anxious children. Behaviour Research and Therapy. 2010;48(5):384–393. doi: 10.1016/j.brat.2009.12.013. http://dx.doi.org/10.1016/j.brat.2009.12.013. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth risk behavior surveillance--united states, 2009. Morbidity and Mortality Weekly Report. 2010;59(SS-5):1–142. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Trends in suicide rates among persons ages 10 years and older, by sex, united states, 1991–2009. Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury Reports. 2012 Retrieved March 9, 2012, from http://www.cdc.gov/injury/wisqars/index.html.
- Cha CB, Nock MK. Emotional intelligence is a protective factor for suicidal behavior. JAAC. 2009;48(4):422–430. doi: 10.1097/CHI.0b013e3181984f44. [DOI] [PubMed] [Google Scholar]
- Cohen P, Hesselbart CS. Demographic factors in the use of children’s mental health services. American Journal of Public Health. 1993;83(1):49. doi: 10.2105/ajph.83.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole P, Martin S, Dennis T. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75(2):317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Pescosolido B, Angold A, Burns BJ. A family network-based model of access to child mental health services. In: Morrissey JP, editor. Research in community and mental health: Social networks and mental illness. Vol. 9. Stamford, CT: JAI Press; 1998. pp. 165–190. [Google Scholar]
- Daniels A, Taylor SC, Post S, Pilsner AM, Hunt YM, Auguston E. Tech to treat: The smokefree teen approach to cessation. Paper presented at the National Conference on Health Communication Marketing and Media; Atlanta, GA. 2012. [Google Scholar]
- Dour HJ, Cha CB, Nock MK. Evidence for an emotion-cognition interaction in the statistical prediction of suicide attempts. Behaviour Research and Therapy. 2011;49(4):294–298. doi: 10.1016/j.brat.2011.01.010. [DOI] [PubMed] [Google Scholar]
- DuBois DL, Silverthorn N. Natural mentoring relationships and adolescent health: Evidence from a national study. American Journal of Public Health. 2005;95(3):518. doi: 10.2105/AJPH.2003.031476). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton D, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Wechsler H. Youth risk behavior surveillance---united states, 2009. MMWR. Surveillance summaries: Morbidity and mortality weekly report Surveillance summaries/CDC. 2010;59(5):1. [PubMed] [Google Scholar]
- Fales CL, Barch DM, Rundle MM, Mintun MA, Snyder AZ, Cohen JD, Sheline YI. Altered emotional interference processing in affective and cognitive-control brain circuitry in major depression. Biological Psychiatry. 2008;63(4):377–384. doi: 10.1016/j.biopsych.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingerman K, Miller L, Birditt K, Zarit S. Giving to the good and the needy: Parental support of grown children. Journal of Marriage and the Family. 2009;71(5):1220–1233. doi: 10.1111/j.1741-3737.2009.00665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Dahl RE. Neural systems of positive affect: Relevance to understanding child and adolescent depression? Develop Psychopathol. 2005;17(3):827–850. doi: 10.1017/S095457940505039X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences. 2006;40(8):1659–1669. [Google Scholar]
- Ge X, Natsuaki MN, Neiderhiser JM, Reiss D. The longitudinal effects of stressful life events on adolescent depression are buffered by parent–child closeness. Development and Psychopathology. 2009;21(02):621. doi: 10.1017/S0954579409000339. [DOI] [PubMed] [Google Scholar]
- Goldin PR, Manber T, Hakimi S, Canli T, Gross JJ. Neural bases of social anxiety disorder: Emotional reactivity and cognitive regulation during social and physical threat. Archives of General Psychiatry. 2009;66(2):170–180. doi: 10.1001/archgenpsychiatry.2008.525. http://dx.doi.org/10.1001/archgenpsychiatry.2008.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston D, Reboussin B, Daniel S. Predictors of suicide attempts: State and trait components. Journal of Abnormal Psychology. 2006;115(4):842. doi: 10.1037/0021-843X.115.4.842. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Erkanli A, Reboussin BA, Mayfield A, Frazier PH, Treadway SL. Psychiatric diagnoses as contemporaneous risk factors for suicide attempts among adolescents and young adults: Developmental changes. J Consult Clin Psychol. 2009;77(2):281–290. doi: 10.1037/a0014732. 2009-03774-008 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould MS, Fisher P, Parides M, Flory M, Shaffer D. Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry. 1996;53(12):1155–1162. doi: 10.1001/archpsyc.1996.01830120095016. [DOI] [PubMed] [Google Scholar]
- Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(4):386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. http://dx.doi.org/10.1023/B:JOBA.0000007455.08539.94. [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. J Abnorm Psychol. 2006;115(4):850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Greenberg MT, Weissberg RP, O’Brien MU, Zins JE, Fredericks L, Resnik H, Elias MJ. Enhancing school-based prevention and youth development through coordinated social, emotional, and academic learning. American Psychologist. 2003;58(6–7):466–474. doi: 10.1037/0003-066X.58.6-7.466. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Process, mechanism, and explanation related to externalizing behavior in developmental psychopathology. Journal of Abnormal Child Psychology: An official publication of the International Society for Research in Child and Adolescent Psychopathology. 2002;30(5):431–446. doi: 10.1023/a:1019808712868. http://dx.doi.org/10.1023/A:1019808712868. [DOI] [PubMed] [Google Scholar]
- Hunter EC, Katz LF, Shortt JW, Davis B, Leve C, Allen NB, Sheeber LB. How do i feel about feelings? Emotion socialization in families of depressed and healthy adolescents. Journal of Youth and Adolescence. 2010;40(4):428–441. doi: 10.1007/s10964-010-9545-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson CM, Marrocco F, Kleinman M, Gould MS. Restrictive emotionality, depressive symptoms, and suicidal thoughts and behaviors among high school students. J Youth Adolescence. 2010:1–10. doi: 10.1007/s10964-010-9573-y. [DOI] [PubMed] [Google Scholar]
- Kaminski JW, Puddy RW, Hall DM, Cashman SY, Crosby AE, Ortega LAG. The relative influence of different domains of social connectedness on self-directed violence in adolescence. Journal of Youth and Adolescence. 2009;39(5):460–473. doi: 10.1007/s10964-009-9472-2. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The national comorbidity survey replication (ncs-r): Background and aims. International Journal of Methods in Psychiatric Research. 2004;13(2):60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana A, Romer D. Modeling the distinct pathways of influence of coping strategies on youth suicidal ideation: A national longitudinal study. Prevention Science. 2012:1–11. doi: 10.1007/s11121-012-0292-3. [DOI] [PubMed] [Google Scholar]
- Kidd S, Henrich CC, Brookmeyer KA, Davidson L, King RA, Shahar G. The social context of adolescent suicide attempts: Interactive effects of parent, peer, and school social relations. Suicide and Life Threatening Behavior. 2006;36(4):386–395. doi: 10.1521/suli.2006.36.4.386. [DOI] [PubMed] [Google Scholar]
- King CA, Klaus N, Kramer A, Venkataraman S, Quinlan P, Gillespie B. The youth-nominated support team–version ii for suicidal adolescents: A randomized controlled intervention trial. J Consult Clin Psychol. 2009;77(5):880–893. doi: 10.1037/a0016552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, Gmel G. Drinking motives as mediators of the link between alcohol expectancies and alcohol use among adolescents. Journal of Studies on Alcohol and Drugs. 2007;68(1):76–85. doi: 10.15288/jsad.2007.68.76. [DOI] [PubMed] [Google Scholar]
- Levine D, McCright J, Dobkin L, Woodruff A, Klausner J. Sexinfo: A sexual health text messaging service for san francisco youth. American Journal of Public Health. 2008;98(3):393–395. doi: 10.2105/AJPH.2007.110767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Logan DE, King CA. Parental facilitation of adolescent mental health services utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2001;8(3):319–333. http://dx.doi.org/10.1093/clipsy/8.3.319. [Google Scholar]
- LoMurray M. Sources of strength facilitators guide: Suicide prevention peer gatekeeper training. The North Dakota Suicide Prevention Project; Bismarck, ND: 2005. [Google Scholar]
- Lyson TA. What does a school mean to a community? Assessing the social and economic benefits of schools to rural villages in new york. Journal of Research in Rural Education. 2002;17(3):131–137. [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S Health obotCoSDo. Closing the gap in a generation: Health equity through action on the social determinants of health. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- McNeely C, Falci C. School connectedness and the transition into and out of health-risk behavior among adolescents: A comparison of social belonging and teacher support. The Journal of school health. 2004;74(7):284–292. doi: 10.1111/j.1746-1561.2004.tb08285.x. [DOI] [PubMed] [Google Scholar]
- Mcneely CA, Barber BK. How do parents make adolescents feel loved? Perspectives on supportive parenting from adolescents in 12 cultures. Journal of Adolescent Research. 2010;25(4):601–631. doi: 10.1177/0743558409357235. [DOI] [Google Scholar]
- Merikangas KR, Avenevoli S, Costello EJ, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (ncs-a): I. Background and measures. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(4):367–379. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer S, Angold A, Costello E, Loeber R, Van Kammen W, Stouthamer-Loeber M. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: Factor composition and structure across development. International Journal of Methods in Psychiatric Research. 1995;5:251–262. [Google Scholar]
- Miller AL, Rathus JH, Linehan MM. Dialectical behavior therapy with suicidal adolescents. New York, NY: Guilford Press; US; 2007. [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social development (Oxford, England) 2007;16(2):361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann A, Van Lier PAC, Gratz KL, Koot HM. Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. Assessment. 2010;17(1):138–149. doi: 10.1177/1073191109349579. [DOI] [PubMed] [Google Scholar]
- Nock MK. Future directions for the study of suicide and self-injury. Journal of Clinical Child & Adolescent Psychology. 2012;41(2):255–259. doi: 10.1080/15374416.2012.652001. [DOI] [PubMed] [Google Scholar]
- Pedersen S, Seidman E, Yoshikawa H, Rivera AC, Allen L, Aber JL. Contextual competence: Multiple manifestations among urban adolescents. American Journal of Community Psychology. 2005;35(1–2):65–82. doi: 10.1007/s10464-005-1890-z. [DOI] [PubMed] [Google Scholar]
- Pisani AR, Schmeelk-Cone K, Gunzler D, Petrova M, Goldston DB, Tu X, Wyman PA. Associations between suicidal high school students’ help-seeking and their attitudes and perceptions of social environment. Journal of Youth and Adolescence. 2012;41(10):1312–1324. doi: 10.1007/s10964-012-9766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajappa K, Gallagher M, Miranda R. Emotion dysregulation and vulnerability to suicidal ideation and attempts. Cognitive Therapy and Research. 2011 doi: 10.1007/s10608-011-9419-2. [DOI] [Google Scholar]
- Rathus JH, Miller AL. Dialectical behavior therapy adapted for suicidal adolescents. Suicide and Life Threatening Behavior. 2002;32(2):146–157. doi: 10.1521/suli.32.2.146.24399. http://dx.doi.org/10.1521/suli.32.2.146.24399. [DOI] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, Udry JR. Protecting adolescents from harm. Findings from the national longitudinal study on adolescent health. JAMA: the journal of the American Medical Association. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Schmeelk-Cone K, Pisani AR, Petrova M, Wyman PA. Three scales assessing high school students’ attitudes and perceived norms about seeking adult help for distress and suicide concerns. Suicide and Life Threatening Behavior. 2012;42(2):157–172. doi: 10.1111/j.1943-278X.2011.00079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shneidman ES. The suicidal mind. New York, NY: Oxford University Press; 1996. [Google Scholar]
- Silk J, Steinberg L, Morris A. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development. 2003;74(6):1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. doi: 10.1007/s11031-005-7955-3. [DOI] [Google Scholar]
- StataCorp. Stata statistical software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Litts D, editor. Suicide Prevention Resource Center and Suicide Prevention Action Network USA. Charting the future of suicide prevention: A 2010 progress review of the national strategy and recommendations for the decade ahead. Newton, MA: 2010. [Google Scholar]
- Thompson E, Eggert L, Randell B, Pike K. Evaluation of indicated suicide risk prevention approaches for potential high school dropouts. American Journal of Public Health. 2001;91(5):742. doi: 10.2105/ajph.91.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R. Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development. 1994;59(2):25–52. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 national strategy for suicide prevention: Goals and objectives for action. Washington, DC: HSS; 2012. [PubMed] [Google Scholar]
- U.S. Dept. of Health and Human Services. National strategy for suicide prevention: Goals and objectives for action. 2001 Retrieved 02/10/2009, from http://mentalhealth.samhsa.gov/publications/allpubs/SMA01-3517/ [PubMed]
- Weinberg A, Klonsky ED. Measurement of emotion dysregulation in adolescents. Psychological Assessment. 2009;21(4):616–621. doi: 10.1037/a0016669. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Pollock LR. The international handbook of suicide and attempted suicide. John Wiley & Sons, Ltd; 2008. The pschology of suicidal behaviour; pp. 79–93. [Google Scholar]
- Wolchik SA, Sandler IN, Millsap RE, Plummer BA, Greene SM, Anderson ER, Haine RA. Six-year follow-up of preventive interventions for children of divorce. JAMA: the journal of the American Medical Association. 2002;288(15):1874–1881. doi: 10.1001/jama.288.15.1874. [DOI] [PubMed] [Google Scholar]
- WWAMI Rural Health Research Center. 2004 zip ruca code files. 2004 Retrieved March 13, 2012, from http://depts.washington.edu/uwruca/ruca-download.php.
- Wyman PA, Brown CH, Inman J, Cross W, Schmeelk-Cone K, Guo J, Pena JB. Randomized trial of a gatekeeper program for suicide prevention: 1-year impact on secondary school staff. Journal of Consulting and Clinical Psychology. 2008;76(1):104–115. doi: 10.1037/0022-006X.76.1.104. 2008-00950-013 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA, Brown CH, LoMurray M, Schmeelk-Cone K, Petrova M, Yu Q, Wang W. An outcome evaluation of the sources of strength suicide prevention program delivered by adolescent peer leaders in high schools. American Journal of Public Health. 2010;100(9):1653–1661. doi: 10.2105/AJPH.2009.190025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA, Gaudieri PA, Schmeelk-Cone K, Cross W, Brown CH, Sworts L, Nathan J. Emotional triggers and psychopathology associated with suicidal ideation in urban children with elevated aggressive-disruptive behavior. J Abnorm Child Psychol. 2009;37(7):917–928. doi: 10.1007/s10802-009-9330-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman MA, Bingenheimer JB, Notaro PC. Natural mentors and adolescent resiliency: A study with urban youth. American Journal of Community Psychology. 2002;30(2):221–243. doi: 10.1023/A:1014632911622. [DOI] [PubMed] [Google Scholar]
- Zullig KJ, Pun S, Patton JM, Ubbes VA. Reliability of the 2005 middle school youth risk behavior survey. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2006;39(6):856–860. doi: 10.1016/j.jadohealth.2006.07.008. [DOI] [PubMed] [Google Scholar]


