Abstract
Background:
Treatment of proximal humerus fractures is controversial and various operative modalities have been tried in the literature. The aim of the present study was to evaluate functional outcome and complication rate after open reduction and internal fixation of displaced proximal humerus fractures by proximal humerus locking plate.
Materials and Methods:
52 patients with displaced proximal humerus fractures treated with proximal humerus locking plate between May 2008 and October 2010 were included in the study. Fractures were classified according to Neer's classification into displaced 2-part, 3-part, and 4-part fractures. Patients were followed for a minimum period of 1 year. 11 patients had less than 1 year of followup and were not considered in the evaluation of final results. Forty one patients were considered for final evaluation. Functional evaluation was done according to the Constant-Murley scoring system. Constant score was compared between 2-part, 3-part, and 4-part fractures at final up and also between young (≤60 yrs) and old (>60 yrs).
Results:
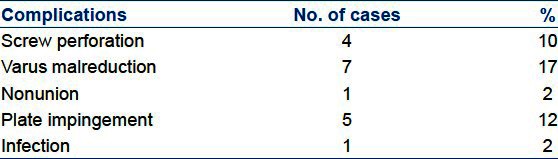
11 patients had 2-part fractures, 22 patients had 3-part fractures, and 19 patients had 4-part fractures. The mean followup period was 15.21 ± 2.59 months. 65.8% (n = 27) patients had good to excellent result, 19.5% (n = 8) had fair, and 14.7% (n = 6) had poor result. Constant scores for 2-part (79.83 ± 6.95) and 3-part fractures (74.22 ± 12.53) were significantly superior to those of 4-part fractures (61.09 ± 14.29) (P value = 0.002 and 0.018, respectively). Difference between 2-part and 3-part fractures was not significant (P value = 0.623). There was no significant difference between younger (≤60) and older patients (>60). Complications encountered in this series were varus malreduction in 17% (n = 7), screw perforation in 10% (n = 4), plate impingement in 12% (n = 5), infection in 2% (n = 1), and nonunion in 2% (n = 1) of cases.
Conclusion:
Proximal humerus locking plate gives reliable fixation for 2-part and 3-part fractures. Its use in more complicated fracture patterns of 4-part fractures is associated with poor clinical outcome.
Keywords: Proximal humerus locking plate, proximal humerus fracture, unstable fracture
INTRODUCTION
The majority of proximal humerus fractures occur in older age groups as a result of trivial trauma where bones are osteoporotic. Because of osteoporosis and comminution both reduction and fixation are difficult. While for undisplaced fractures, literature strongly suggests nonoperative treatment,1–3 the treatment of displaced fractures is still controversial and challenging. A wide variety of treatment modalities have been used in the past which include transosseous suture fixation, tension band wiring, standard plate and screw fixation, hemireplacement arthroplasty, percutaneous wire, and screw fixation.4–6 But consensus is available on the ideal treatment modality especially of 3-part and 4-part fractures.7–9 Precontoured locking plates work on the principle of angular stability, less disruption of vascularity, and less chances of plate failure.10 Improved fixation by locking plates is attributed to the angular stability of the screws locking in the plate and their three-dimensional distribution in the humeral head. But their use for the treatment of proximal humerus fractures demands an accurate surgical technique, long learning curve to avoid plate impingement, and screw perforation of the articular surface.11–13 Also, like with all locking plates, fracture reduction must be achieved prior to plate application which can be challenging. The aim of the present study was to evaluate functional outcome and complication rate after open reduction and internal fixation of displaced proximal humerus fractures by proximal humerus locking plate.
MATERIALS AND METHODS
This was a prospective study conducted in our institute on a consecutive series of patients for the treatment of displaced (angulation of the articular surface of >45 degrees or displacement of more than 1 cm between the major fracture segments)14 2-part, 3-part, and 4-part proximal humerus fractures from May 2008 to October 2010. After obtaining institutional ethical committee clearance, 57 consecutive patients of displaced proximal humerus fractures (as defined by Neer's criteria) were enrolled in the study. Written informed consent was obtained from all the patients. Open fractures, stable 2-part fractures, isolated tuberosity fractures, bilateral fractures, fractures with ipsilateral significant injuries which could prevent early rehabilitation, head splitting fractures, fracture dislocations, and fractures occurring in children less than 18 years old were excluded from the study. Anteroposterior and axillary views of shoulder were obtained in all patients [Figure 1a and b]. 3-D CT reconstruction was used only in those patients in whom head splitting fracture was suspected. Fractures were classified according to Neer's classification15 into 2-part, 3-part, and 4-part. There were eleven 2-part, twenty two 3-part, and nineteen 4-part fractures. To precisely classify the fractures independent opinion of two orthopaedic surgeons were taken. We used proximal humerus locking plate (Uma surgical, Mumbai) in all patients which is a precontoured plate according to the anatomy of proximal part of humerus. There are five locking screw holes for the head fragment in which the direction of screws are nonparallel. The screw holes in the shaft portion are combi holes and the plate is available in different sizes.
Figure 1.
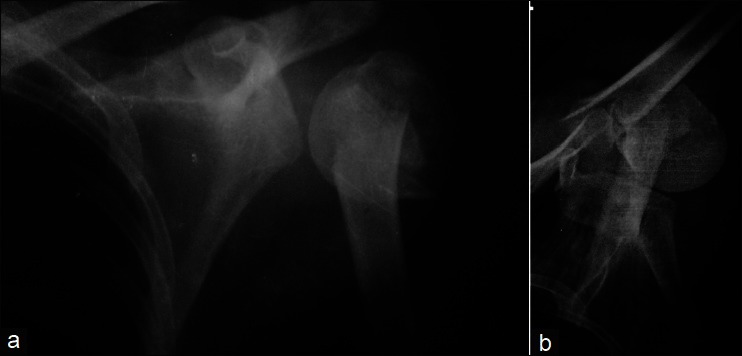
(a) and (b) Preoperative X-ray (anteroposterior and axillary view) of a 3-part proximal humerus fracture
All the fractures were operated by senior orthopaedic surgeon (AKG) using a standard deltopectoral approach with the patient in the supine position on a radiolucent table with access for image intensifier to obtain intraoperative anteroposterior and axillary views. Fractures were reduced by manual traction and abduction to neutralize pull of the deltoid muscle. After provisional stabilization of fractures by k-wires, definitive fixation with proximal humerus locking plate was done. Tuberosity fractures were reduced by means of nonabsorbable Ethibond sutures whenever required. If the fracture was reduced plate was applied over lateral aspect of proximal humerus and locking screws were inserted first in the head fragment. Care was taken in placing the plate lateral to the biceps tendon and 5-8 mm distal to upper end of greater tuberosity. In case the shaft was medially displaced first cortical screw (3.5 mm) was inserted in the shaft portion to neutralize pull of pectoralis major muscle. After that, locking screws in the head were inserted. Postoperative x-ray was obtained in all patients [Figure 2]. On immediate postoperative evalutation of X-rays varus malreduction of more than 20 degrees was present in 7 patients and screw perforation was identified in 3 patients.
Figure 2.
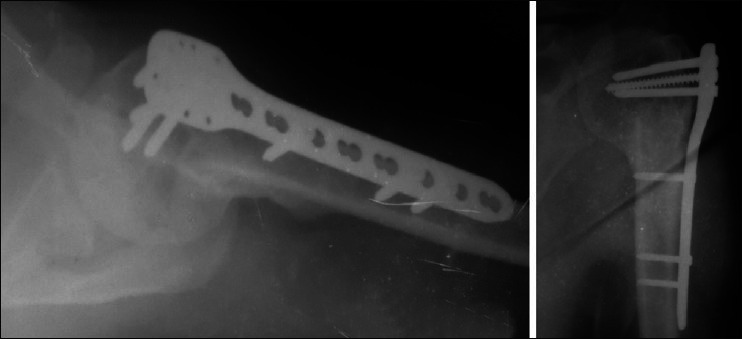
Postoperative X-rays showing anatomical reduction
Postoperatively arm sling was applied and continued till fracture union. Passive-guarded physiotherapy was started in the first postoperative week and continued till fracture union. Active range of motion exercises and passive stretching exercises were started after fracture union. Patients were followed up at 6 weeks, 3 months, 6 months, 1 year, 1.5 years, and 2 years [Figure 3a and b]. At each visit, functional evaluation was done according to Constant-Murley scoring system [Figure 4a-c].16 The Constant score was graded as poor (0-55 points), fair (56-70), good (71-85), or excellent (86-100). Constant score and its various subcomponents were compared between 2-part, 3-part, and 4-part fractures at the last available followup after 1 year. Scores were also compared between young (≤60 years) and old (>60 years) patients.
Figure 3.

(a) and (b) Followup X-ray at 18 months showing union
Figure 4.
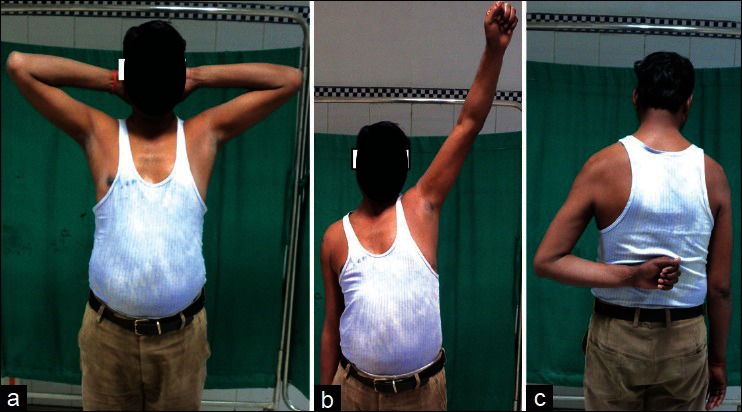
(a-c) Clinical photographs at 18 month followup showing range of motion
The Student t test was used for comparison of scores between young and old patients, while for comparison between three fracture types ANOVA was used. All the statistical calculations were done using SPSS 16 software and the level of significance was set at ≤0.05.
RESULTS
A total of 57 patients of proximal humerus fractures were treated during the above-mentioned period of study. Five patients were excluded from the study by above-mentioned exclusion criteria (two patients had proximal humerus fracture dislocation, two patients had displaced greater tuberosity fracture, and one patient had head splitting fracture). Eleven patients had less than 1 year of followup and were not included in the evaluation of final result. Forty one patients were considered for final evaluation. Patient characteristics are represented in Table 1. 54% patients (n = 22) were less than or equal to 60 years of age and 46% (n = 19) were more than 60 years of age. Patients were operated after an average period of 6.2 days. The average union time was 3 months (range 2-5 months). Clinical evaluation was done according to Constant-Murley score. The overall mean score was 72.34 ± 13.57. 66% (n = 27) patients had good to excellent result, 20% (n = 8) had fair, and 15% (n = 6) had poor result. The mean Constant score for 2-part fractures was 79.83 ± 6.95, of 3-part fractures was 74.22 ± 12.53, and of 4-part fractures was 61.09 ± 14.29. Constant scores for 2-part and 3-part fractures were significantly superior to those of 4-part fractures (P value = 0.002 and 0.018, respectively). Difference between 2-part and 3-part fractures was not significant (P value 0.623). Mean score of patients with age less than or equal to 60 years of age was 73.61 ± 13.51 and in patients with more than 60 years was 70.31 ± 14.26. The difference was not significant (P value 0.564). Differences between pain, activities of daily living, range of motion and strength subcomponents of the Constant-Murley score between 2-part, 3-part and 4-part fractures were also significant [Table 2]. Overall 18 complications occurred in 10 patients [Table 3].
Table 1.
Patient demography

Table 2.
Comparison of subscores of Constant. Murley score between three fracture types
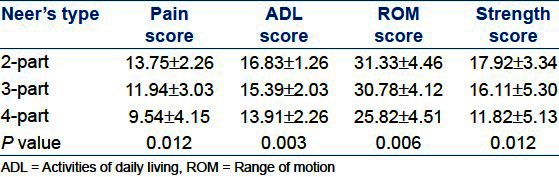
Table 3.
Complications associated with management of proximal humerus fractures with proximal humerus locking plate
DISCUSSION
Treatment of proximal humerus fractures has been controversial. For displaced fractures, traditional treatment with conventional plates and screws has been associated with high rates of unsatisfactory results and complications.17 Locking plates are angular stable plates which has advantage of secure fixation in metaphyseal and osteoporotic bones. There are biomechanical studies which suggest that locking plates resist physiological loads more effectively.18,19 There are many clinical studies which indicate that proximal humerus locking plates have good result in proximal humerus fractures.20,21,22
In our study, 66% (n = 27) of the patients had excellent to good outcome. The overall mean Constant score was 72.34 ± 13.57. Aggarwal et al.23 in their study found moderate to excellent outcome in 90% of patients. They also found significantly higher Constant score for younger patients (P value = 0.12). The mean age of the patients in this series was 58.51 years (range 23-81 years) and fracture types were Neer 2-part, 3-part, and 4-part fractures and fracture dislocations. Thyagarajan et al.10 in their study on 30 patients showed an overall average Constant score of 57.5. The mean age in this series was 58 years (range 19-92 years) and fractures were Neer's 2-part, 3-part, and 4-part fractures.
Parmaksizoglu et al.24 in their study showed 68.7% excellent to good results. Mean age was 63 years (range 29-82 years) and fractures were Neers, 3-part, and 4-part 31.8% (n=10). Patients have not achieved optimal results.
Solberget al.25 in their retrospective study of Neer, 3 and 4-part fractures showed mean Constant score of 64.7 in 4-part fractures. The mean age of the patients in locked plate group was 66.5 ± 8.6 years.
In the study of Aggarwal et al.23 the mean Constant score for 4-part fractures was 66 ± 12.61 and was significantly inferior to other types.
In our study also the mean Constant score for 4-part fractures was 61.09 ± 14.29 which was significantly inferior compared to 2-part and 3-part fractures (P value = 0.001 and = 0.018, respectively). This result is comparable to the above mentioned studies.
In our study, the comparison of subcomponents of Constant score shows a significant difference between 4-part fracture and other two fracture types. Similar findings were reported by Aggarwal et al.23
Varus malreduction has been correlated with poor outcome in many studies. In our study varus malreduction of >20 degrees occurred in 17% of cases (n = 7) [Table 3]. All the patients with varus malreduction had Constant score <70. All but one of the fractures with varus malreduction of >20 degrees united. Four of these cases also had plate impingement in the subacromial area. This implicates varus malreduction as a principal cause of plate impingement in the subacromial area and this error is more common than placing the plate too far superiorly.
Screw perforation [Figure 5] occurred in our study in 4 cases. Three out of four screw perforations occurred because of intraoperative errors of screw placement. Similar incidence of screw perforation has been reported in other studies.
Figure 5.

Axillary view of shoulder following proximal humeral locking plate fixation showing screw perforation of humeral head
We found no significant difference in outcome between patients of age group less than or more than 60 years of age. Similar findings have been reported by Koukakis et al.20 who reported no significant difference between younger (<65) and older (>65) patients. Moonot et al.22 also reported similar findings.
No osteonecrosis occurred in our series. This may be because of smaller number of patients in 4-part fracture group (n = 11). Also, a majority of fractures in 4-part group were in the surgical neck region and hence had low risk of osteonecrosis.
The limitation of this study is lack of a control group. A randomized study comparing the result of other treatment modalities will probably serve as a better guideline for treatment of these fractures.
We conclude that proximal humerus locking plate fixation for 2-part and 3-part fractures has good functional outcome but its use in 4-part fractures is associated with high complication rate. Use of this implant needs technical expertise and most of the complications occur because of intraoperative technical errors.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Koval KJ, Gallagher MA, Marsicano JG, Cuomo F, McShinawy A, Zuckerman JD. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79:203–7. doi: 10.2106/00004623-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Tejwani NC, Liporace F, Walsh M, France MA, Zuckerman JD, Egol KA. Functional outcome following one-part proximal humeral fractures: A prospective study. J Shoulder Elbow Surg. 2008;17:216–9. doi: 10.1016/j.jse.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Gaebler C, McQueen MM, Court-Brown CM. Minimally displaced proximal humeral fractures: Epidemiology and outcome in 507 cases. Acta Orthop Scand. 2003;74:580–5. doi: 10.1080/00016470310017992. [DOI] [PubMed] [Google Scholar]
- 4.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93:121–31. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park MC, Murthi AM, Roth NS, Blaine TA, Levine WN, Bigliani LU. Two-part and three-part fractures of the proximal humerus treated with suture fixation. J Orthop Trauma. 2003;17:319–25. doi: 10.1097/00005131-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Resch H, Povacz P, Fröhlich R, Wambacher M. Percutaneous fixation of three- and four-part fractures of the proximal humerus. J Bone Joint Surg Br. 1997;79:295–300. doi: 10.1302/0301-620x.79b2.6958. [DOI] [PubMed] [Google Scholar]
- 7.Antuña SA, Sperling JW, Cofield RH. Shoulder hemiarthroplasty for acute fractures of the proximal humerus: A minimum five-year followup. J Shoulder Elbow Surg. 2008;17:202–9. doi: 10.1016/j.jse.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 8.Goldman RT, Koval KJ, Cuomo F, Gallagher MA, Zuckerman JD. Functional outcome after humeral head replacement for acute three- and four-part proximal humeral fractures. J Shoulder Elbow Surg. 1995;4:81–6. doi: 10.1016/s1058-2746(05)80059-x. [DOI] [PubMed] [Google Scholar]
- 9.Green A, Barnard WL, Limbird RS. Humeral head replacement for acute fourpart proximal humerus fractures. J Shoulder Elbow Surg. 1993;2:249–54. doi: 10.1016/S1058-2746(09)80084-0. [DOI] [PubMed] [Google Scholar]
- 10.Thyagarajan DS, Haridas SJ, Jones D, Dent C, Evans R, Williams R. Functional outcome following proximal humeral interlocking system plating for displaced proximal humeral fractures. Int J Shoulder Surg. 2009;3:57–62. doi: 10.4103/0973-6042.59971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Owsley K, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures. J Bone Joint Surg Am. 2008;90:233–40. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 12.Egol KA, Ong CC, Walsh M, Jazrawi LM, Tejwani NC, Zuckerman JD. Early complications in proximal humerus fractures (OTA Types 11) treated with locked plates. J Orthop Trauma. 2008;22:159–64. doi: 10.1097/BOT.0b013e318169ef2a. [DOI] [PubMed] [Google Scholar]
- 13.Agudelo J, Schürmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21:676–81. doi: 10.1097/BOT.0b013e31815bb09d. [DOI] [PubMed] [Google Scholar]
- 14.Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–8. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 15.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–89. [PubMed] [Google Scholar]
- 16.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 17.Kristiansen B, Christensen SW. Plate fixation of proximal humeral fractures. Acta Orthop Scand. 1986;57:320–3. doi: 10.3109/17453678608994401. [DOI] [PubMed] [Google Scholar]
- 18.Lever JP, Aksenov SA, Zdero R, Ahn H, McKee MD, Schemitsch EH. Biomechanical analysis of plate osteosynthesis systems for proximal humerus fractures. J Orthop Trauma. 2008;22:23–9. doi: 10.1097/BOT.0b013e31815c89ce. [DOI] [PubMed] [Google Scholar]
- 19.Seide K, Triebe J, Faschingbauer M, Schulz AP, Püschel K, Mehrtens G, et al. Locked vs. unlocked plate osteosynthesis of the proximal humerus-A biomechanical study. Clin Biomech (Bristol, Avon) 2007;22:176–82. doi: 10.1016/j.clinbiomech.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Koukakis A, Apostolou CD, Taneja T, Korres DS, Amini A. Fixation of proximal humerus fractures using the PHILOS plate: Early experience. Clin Orthop Relat Res. 2006;442:115–20. doi: 10.1097/01.blo.0000194678.87258.6e. [DOI] [PubMed] [Google Scholar]
- 21.Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R. A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res. 2005;430:176–81. doi: 10.1097/01.blo.0000137554.91189.a9. [DOI] [PubMed] [Google Scholar]
- 22.Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89:1206–9. doi: 10.1302/0301-620X.89B9.18528. [DOI] [PubMed] [Google Scholar]
- 23.Aggarwal S, Bali K, Dhillon MS, Kumar V, Mootha AK. Displaced proximal humeral fractures: An Indian experience with locking plates. J Orthop Surg Res. 2010;5:60. doi: 10.1186/1749-799X-5-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parmaksizoğlu AS, Sökücü S, Ozkaya U, Kabukçuoğlu Y, Gül M. Locking plate fixation of three- and four-part proximal humeral fractures. Acta Orthop Traumatol Turc. 2010;44:97–104. doi: 10.3944/AOTT.2010.2275. [DOI] [PubMed] [Google Scholar]
- 25.Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009;91:1689–97. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]


