Abstract
Background:
Thromboprophylaxis in arthroscopy is controversial. Recent literature has shown variable rates of deep vein thrombosis following routine arthroscopic knee surgery; however, it is unknown if current practice reflects the literature. We have conducted a cross sectional survey to provide insight into the practice patterns perceived risks, benefits and barrier in the use of thromboprophylaxis.
Materials and Methods:
A 19 item survey was created regarding surgeons' use of thromboprophylaxis in their patients undergoing routine knee arthroscopy. E-mail surveys were sent out to members of the Canadian Orthopaedic Association.
Results:
Seventy-seven responses were obtained; of which 58.2% (n=45) of surgeons stated that they had a clinical interest in sports medicine, and 37.3% (n=29) had completed a fellowship in sports medicine or arthroscopy. Fifty five surgeons (71.6%) performed more than 40 arthroscopies per year. Prolonged surgical time was the only risk factor that would significantly increase their use of prophylaxis. Practice patterns surrounding the use of thromboprophylaxis were otherwise quite variable.
Conclusions:
Our survey reveals that opinions and practice patterns surrounding the use of thromboprophylaxis following routine knee arthroscopy are diverse. This survey points out the need for larger well designed studies for concise guidelines.
Keywords: Knee arthroscopy, deep vein thrombosis, thromboprophylaxis
INTRODUCTION
Arthroscopic knee surgery is usually shown to be associated with a low rate of thromboembolic complications.1–3 Previous studies were often performed retrospectively, poor diagnostic tests were used, and studies were often biased.4 As a result, controversy has surrounded the use of thromboprophylaxis in routine arthroscopy of the knee. Current literature, however, reports an incidence of deep vein thrombosis (DVT) of 9.9% overall and 2.1% for proximal DVTs,5 and a pulmonary embolism (PE) rate of 0.028%6 in patients undergoing routine knee arthroscopy.
The objective of this study was to provide insight into the practice patterns, perceived risks, benefits, and barriers to the use of thromboprophylaxis. We hypothesized that the majority of surgeons do not use any form of thromboprophylaxis in routine knee arthroscopy unless significant risk factors are present. Additionally, we hypothesized that those who perform more than 40 arthroscopies a year and those who are fellowship trained in arthroscopy will be more likely to use prophylaxis since the prevalence of DVTs in their practice is likely to be higher.
MATERIALS AND METHODS
This is a cross sectional survey. The survey consisted of a 9 item English language questionnaire. The 5-point Likert Scale (Strongly agree, Agree, Neutral, Disagree, Strongly Disagree) was used for most questions, and a nominal scale (yes-no) was used for the remainder. In addition, ten questions were asked regarding surgeon demographics [Appendix 1]. The questions were phrased as “close-ended” to reduce any vagueness or confusion. The survey was designed to be completed within ten minutes to encourage participation. Prior to sending out the surveys, a pre-test questionnaire was given to three orthopedic surgeons who were fellowship trained in Sports Medicine to ensure face validity. The surgeons further commented on the clarity and comprehensiveness of the questionnaire.
Questionnaire administration
An online survey was sent to all practicing orthopedic surgeons in early 2011 regarding the use of thromboprophylaxis in their patients undergoing routine knee arthroscopy. A total of 691 practicing orthopedic surgeons were identified. Surveys were then emailed and administered via Lime Survey (www.limesurvey.com) along with a cover letter disclosing the intent of survey. Each surgeon received a unique identification token, and responses remained anonymous. Those wishing not to participate were able to request to be removed from the email list. After 4 and 8 weeks, invitations were reissued to all nonresponders with a gift certificate incentive to increase our response rate. Approval was obtained from our local ethics board.
Statistical analysis
Categorical variables were reported as count and percentages, and compared using Chi-square test. Ordinal variables were summarized as median, minimum, and maximum. Between group comparison of Likert scale questions were performed using Mann-Whitney U test. A P value of 0.05 was considered for statistical significance and was adjusted for multiple between group comparisons if applicable. SPSS 19.0 (SPSS, Chicago, IL) statistical software was used for statistical analysis.
RESULTS
Respondent demographics
Of 691 surgeons, five surgeons declined to complete the questionnaire because they did not perform routine knee arthroscopy. Seventy-seven completed the online survey questionnaire, a response rate of 11.2%. The majority of surgeons who responded were in community practice (n=47, 61.2%) and the remainders were in academic practice (n=30, 38.8%). Most had practiced for more than 20 years (40.3%), and were located in Ontario (43.3%)or British Columbia (22.4%). Surgeons' clinical areas of interest or expertise were in arthroplasty (67.2%), sports medicine (58.2%), and general orthopedics (31.3%).37.3% of respondents had completed a fellowship in sports medicine or arthroscopy. The majority of all surgeons were performing more that 40 knee arthroscopies a year (71.6%).
Use of thromboprophylaxis
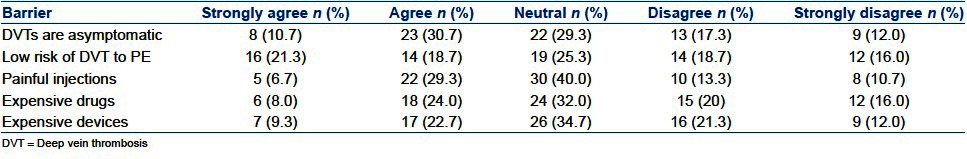
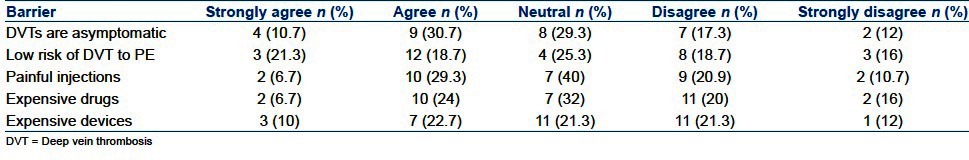
The majority of surgeons do not routinely use pharmaceutical or mechanical thromboprophylaxis in arthroscopic knee debridements (100%; 95.7%), ACL reconstructions (90.9%; 89.1%), or meniscal repairs (95.3%; 93.7%) [Table 1]. Risk factors that most surgeons felt would increase their use of thromboprophylaxis were patient history of a previous DVT (91.7.6%), postoperative immobility of the patient (80.3%), and use of oral contraceptive pills (50.7%). Risk factors that most surgeons did not believe would change their use of thromboprophylaxis were patient age greater than 50 or less than 18 years, use of a tourniquet, and patient history of smoking. Roughly half of all surgeons responded that prolonged surgical time greater than two hours did not affect their use of thromboprophylaxis (49.3%) [Table 2]. Factors that surgeons agreed were barriers to their use of thromboprophylaxis were that most DVTs are felt to be asymptomatic (41.3%), the risk of a DVT becoming a PE is too low (40.0%), and that patients did not like giving self injections (35.0%). The cost of pharmaceutical or mechanical prophylaxis did notstrongly affect surgeons' choices [Table 3].
Table 1.
Routine use of thromboprophylaxis
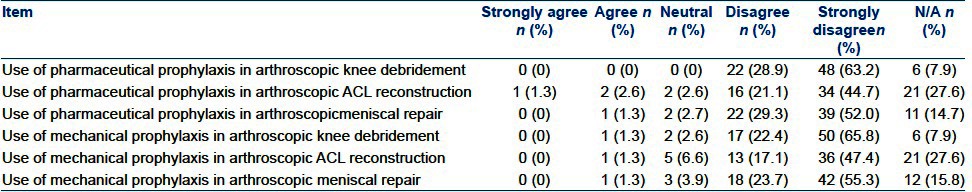
Table 2.
Patient risk factors and effect on use of thromboprophylaxis
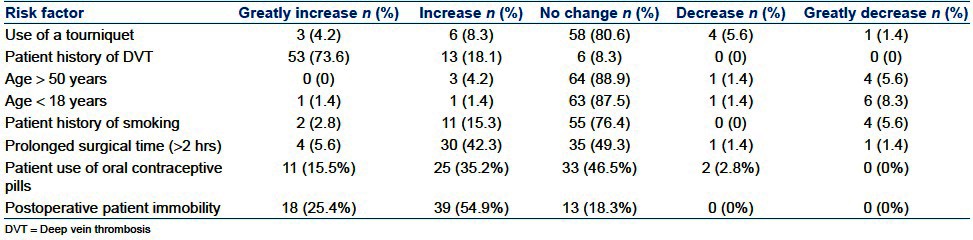
Table 3.
Barriers that prevent use of thromboprophylaxis
When pharmaceutical prophylaxis was required, the most frequently used agent was low-molecular-weight heparin (59.4%) followed by Rivaroxaban (24.3%), and the duration of treatment was most commonly between 10 to 30 days (68.4%). Most surgeons would prefer to use an oral agent compared to injections (84.9%) assuming risks and efficacy were the same. 57.3% of surgeons have not increased their use of anticoagulation over the past five years, and 71.2% feel that the quality of evidence supporting use of thromboprophylaxis is not high. Approximately half of respondents have seen a major complication from a DVT in their practice, and only one respondent said that their hospital had a protocol for anticoagulation following knee arthroscopy.
Subgroup analysis
Surgeons performing more than 40 arthroscopies a year, they most often described their clinical interest in general orthopedics (P = 0.003), sports medicine (P = 0.026), or had fellowship training in sports medicine or arthroscopy (P = 0.019). Prolonged surgical time was the only factor that significantly increased use of thromboprophylaxis for surgeons who performed more than 40 arthroscopies per year compared to those who performed less than 40 arthroscopies each year (P = 0.028).
There was no significant difference between surgeons with a clinical interest in sports medicine and surgeons with clinical interest in other areas for any of the questions [Tables 4 and 5]. Surgeons who practiced in an academic setting use mechanical prophylaxis less frequently following arthroscopic knee debridement compared to surgeons who practiced in community setting (P = 0.022). Surgeons who completed a sports medicine fellowship training more frequently responded that most DVTs are asymptomatic and did not warrant thromboprophylaxis [Table 6], compared with surgeons without a sport medicine fellowship (P = 0.037).
Table 4.
Routine use of thromboprophylaxis - sports surgeons
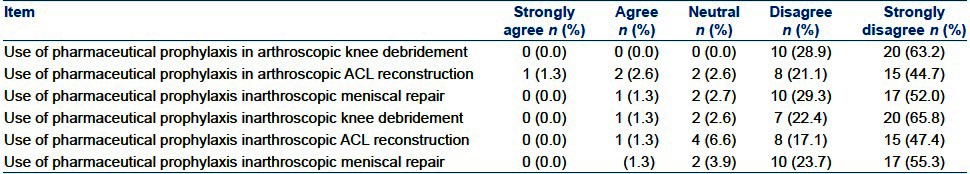
Table 5.
Patient risk factors and effect on use of thromboprophylaxis - sports surgeons
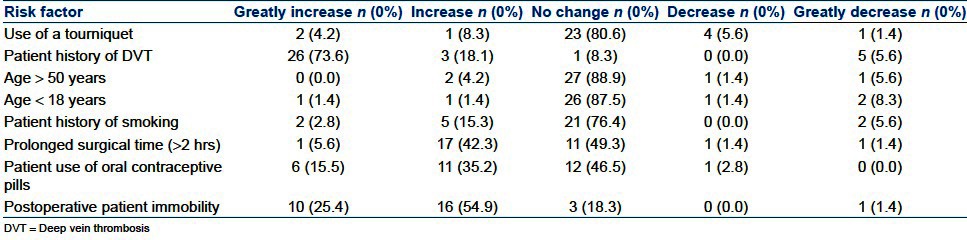
Table 6.
Barriers that prevent use of thromboprophylaxis-sports surgeons
DISCUSSION
As thromboembolic disease forms only a small part of orthopedic practice, it can be difficult to stay abreast with advances that are important for optimal clinical care. Our survey of Canadian orthopedic surgeons reveals that opinions and practice patterns surrounding the use of thromboprophylaxis following routine knee arthroscopy are diverse. The varying opinions about the use of thromboprophylaxis in our survey may be explained by several reasons. First, different perceptions about the underlying risks of DVT may be associated with the varying quality and reporting of the current literature. Second, there are no definitive guidelines (or nonambiguous) by associations or hospitals that aid the surgeon in patients that do possess certain risk factors. Our varying responses are consistent with other surveys regarding practice patterns in routine knee arthroscopy.7–9 This highlights a glaring deficit in which there is no standardized patient care surrounding the most frequently performed surgery.
Surgeons performing more than 40 arthroscopies a year were more likely to use thromboprophylaxis following prolonged surgery (>2 hours). This may be explained by the increased prevalence of complications in their practice following more involved surgeries. This may also be a reflection of staying current with the literature through various venues (academic and society meetings), or through discussion with other colleagues in sports medicine who may have experienced complications in their practice.
Risk factors that increased surgeons' use of anticoagulation included a patient history of previous DVT, use of oral contraceptive pills, and postoperative immobility. Reasons for not routinely prescribing anticoagulation were that surgeons felt most DVTs are asymptomatic, the risk of a DVT becoming a PE is too low, and that patients did not like to give self-injections. Overall, our survey has shown that most surgeons have not increased their use of thromboprophylaxis over the past 5 years, and that they feel that the quality of evidence is not high enough to change their practice. The notion that most DVTs are asymptomatic and thus do not warrant use of routine thromboprophylaxis was shared by most surgeons.
It is currently felt by many physicians that the risk of DVT in routine arthroscopy is too low to warrant routine use of thromboprophylaxis.9,10 Furthermore, the 2008 guidelines put out by the American College of Chest Physicians (ACCP) do not advocate the use of routine anticoagulation other than early mobilization unless additional risk factors exist. Currently, no guidelines have been put forth by the American Academy of Orthopaedic Surgeons specific to thromboprophylaxis after knee arthroscopy.11 Known independent risk factors for the development of DVTs after knee arthroscopy are tourniquet time greater than one hour and a previous DVT.2,12 Delis et al. have shown an increased risk of DVT following knee arthroscopy if two or more of the following six factors were present: Age greater than 65 years, obesity, smoking, female hormone intake, venous insufficiency, and previous VTE.12 Hetsroni et al. found that the risk of developing a PE increased to more than six fold for patients over 40 years compared to less than 20 years, and that procedures taking longer than 90 minutes increased the risk of PE by a factor of three compared to surgeries taking less than 30 minutes.6 Prevention of DVTs following this commonly performed surgery can not only lead to postoperative morbidity and mortality, but also reduced hospital stays and healthcare costs.13–18
Strengths and limitations
This survey was designed and conducted following best practice guidelines.19 Reponses were obtained from all provinces and territories, from a variety of academic and community surgeons, and across all orthopedic subspecialties.
The response rate for this survey was lower compared to the response rate reported in a systematic review of postal surveys.20 Possible explanations include the dissemination of the survey via e-mail rather than by fax, and several e-mail accounts may have been out-of-date or not regularly checked. Additionally, there were demographic variations between surgeons in our survey. Data have been summarized collectively, however, should be interpreted with caution due to different surgeon experiences, practices, and exposure to arthroscopy.
CONCLUSIONS
Varying perceptions of DVT prophylaxis exists among orthopedic surgeons, and there lacks consensus on indications, methods, and dosages surrounding its use. However, among high-volume arthroscopists, use of thromboprophylaxis following surgery lasting more than two hours was significantly higher compared to low-volume surgeons. This survey points out the need for larger, well-designed randomized controlled trials that focus on both pharmaceutical and mechanical prophylaxis, patient risk factors, cost-benefit analysis, and the need for more concise guidelines.
APPENDIX 1: TRAK SURVEY

Footnotes
Source of Support: A McMaster Univeristy Residents Research
Conflict of Interest: None
REFERENCES
- 1.Jaureguito JW, Greenwald AE, Wilcox JF, Paulos LE, Rosenberg TD. The incidence of deep venous thrombosis after arthroscopic knee surgery. Am J Sports Med. 1999;27:707–10. doi: 10.1177/03635465990270060401. [DOI] [PubMed] [Google Scholar]
- 2.Demers C, Marcoux S, Ginsberg JS, Laroche F, Cloutier R, Poulin J. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med. 1998;158:47–50. doi: 10.1001/archinte.158.1.47. [DOI] [PubMed] [Google Scholar]
- 3.Williams JS, Hulstyn MJ, Fadale PD, Lindy PB, Ehrlich MG, Cronan J, et al. Incidence of deep vein thrombosis after arthroscopic knee surgery: A prospective study. Arthroscopy. 1995;11:701–5. doi: 10.1016/0749-8063(95)90113-2. [DOI] [PubMed] [Google Scholar]
- 4.Michot M, Conen D, Holtz D, Erni D, Zumstein M, Ruflin G, et al. Prevention of deep-vein thrombosis in ambulatory arthroscopic knee surgery: A randomized trial of prophylaxiswith low– molecular weight heparin. Arthroscopy. 2002;18:257–63. doi: 10.1053/jars.2002.30013. [DOI] [PubMed] [Google Scholar]
- 5.Ilahi O, Reddy J, Ahmad I. Deep venous thrombosis after knee arthroscopy: A meta-analysis. Arthroscopy. 2005:21727–30. doi: 10.1016/j.arthro.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Hetsroni I, Lyman S, Do H, Mann G, Marx RG. Symptomatic pulmonary embolism after outpatient arthroscopic procedures of the knee: The incidence and risk factors in 418323 arthroscopies. J Bone Joint Surg Br. 2011;93:47–5. doi: 10.1302/0301-620X.93B1.25498. [DOI] [PubMed] [Google Scholar]
- 7.Brattwall M, Jacobson E, Forssblad M, Jakobsoon J. Knee arthroscopy routines and practice. Knee Surg Sports Traumatol Arthrosc. 2010;18:1656–60. doi: 10.1007/s00167-010-1266-2. [DOI] [PubMed] [Google Scholar]
- 8.Muller-Rath R, Ingenhoven E, Mumme T, Schumacher M, Miltner O. Perioperative management in outpatient arthroscopy of the knee joint. Z Orthop Unfall. 2010;148:282–7. doi: 10.1055/s-0029-1240784. [DOI] [PubMed] [Google Scholar]
- 9.Redfern J, Burks R. 2009 survey results: Surgeon practice patterns regarding arthroscopic surgery. Arthroscopy. 2009;25:1447–52. doi: 10.1016/j.arthro.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Tucker J, Doulens K. Pulmonary embolism after knee arthroscopy. Am J Orthop. 2010;39:E7–10. [PubMed] [Google Scholar]
- 11.Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition) Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 12.Delis KT, Hunt N, Strachan RK, Nicolaides AN. Incidence, natural history and risk factors of deep vein thrombosis in elective knee arthroscopy. Thromb Haemost. 2001;86:817–21. [PubMed] [Google Scholar]
- 13.Eynon AM, James S, Leach P. Thromboembolic events after arthroscopic knee surgery. Arthroscopy. 2004;20:23–4. doi: 10.1016/j.arthro.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 14.Janssen RP, Sala HA. Fatal pulmonary embolism after anterior cruciateligament reconstruction. Am J Sports Med. 2007;35:1000–2. doi: 10.1177/0363546506298581. [DOI] [PubMed] [Google Scholar]
- 15.Navarro-Sanz A, Férnandex-Ortega JF. Fatal pulmonary embolism after knee arthroscopy. Am J Sports Med. 2004;32:525–8. doi: 10.1177/0363546503258876. [DOI] [PubMed] [Google Scholar]
- 16.Rozencwaig R, Shilt JS, Ochsner JL., Jr Fatal pulmonary embolus after knee arthroscopy. Arthroscopy. 1996;12:240–1. doi: 10.1016/s0749-8063(96)90020-1. [DOI] [PubMed] [Google Scholar]
- 17.Camporese G, Bernardi E, Prandoni P, Noventa F, Verlato F, Simioni P, et al. Low-molecular-weight heparin versus compression stockings for thromboprophylaxis after knee arthroscopy: A randomized trial. Ann Intern Med. 2008;149:73–82. doi: 10.7326/0003-4819-149-2-200807150-00003. [DOI] [PubMed] [Google Scholar]
- 18.Hirsh J, Hoak J. Management of deep vein thrombosis and pulmonary embolism. A statement for healthcare professionals. Council on thrombosis (in consultation with the council on cardiovascular radiology), American Heart Association. Circulation. 1996;93:2212–45. doi: 10.1161/01.cir.93.12.2212. [DOI] [PubMed] [Google Scholar]
- 19.Sprague S, Quigley L, Bhandari M. Survey design in orthopaedic surgery: Getting surgeons to respond. J Bone Joint Surg Am. 2009;91:27–34. doi: 10.2106/JBJS.H.01574. [DOI] [PubMed] [Google Scholar]
- 20.Asch DA, Jedrzwieski MK, Christakis NA. Response rates to mail surveys published in medical journals. J ClinEpidemiol. 1997;50:1129–36. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]


