Abstract
Background:
Dual plate fixation in comminuted bicondylar tibial plateau fractures remains controversial. Open reduction and internal fixation, specifically through compromised soft tissues, has historically been associated with major wound complications. Alternate methods of treatment have been described, each with its own merits and demerits. We performed a retrospective study to evaluate the functional outcome of lateral and medial plate fixation of Schatzker type V and VI fractures through an anterolateral approach, and a medial minimally invasive approach or a posteromedial approach.
Materials and Methods:
We treated 46 tibial plateau fractures Schatzker type V and VI with lateral and medial plates through an anterolateral approach and a medial minimal invasive approach over an 8 years period. Six patients were lost to followup. Radiographs in two planes were taken in all cases. Immediate postoperative radiographs were assessed for quality of reduction and fixation. The functional outcome was evaluated according to the Oxford Knee Score criteria on followup.
Results:
Forty patients (33 men and 7 women) who completed the followup were included in the study. There were 20 Schatzker type V fractures and 20 Schatzker type VI fractures. The mean duration of followup was 4 years (range 1-8 years). All patients had a satisfactory articular reduction defined as ≤2 mm step-off or gap as assessed on followup. All patients had a good coronal and sagittal plane alignment, and articular width as assessed on supine X-rays of the knee in the anteroposterior (AP) and lateral views. The functional outcome, as assessed by the Oxford Knee Score, was excellent in 30 patients and good in 10 patients. All patients returned to their pre-injury level of activity and employment. There were no instances of deep infection.
Conclusions:
Dual plate fixation of severe bicondylar tibial plateau fractures is an excellent treatment option as it provides rigid fixation and allows early knee mobilization. Careful soft tissue handling and employing minimal invasive techniques minimizes soft tissue complications.
Keywords: Dual plating, minimal invasive, bicondylar, tibial plateau
INTRODUCTION
The ideal treatment of high-energy tibial plateau fractures remains controversial. Open reduction and rigid internal fixation achieves the goals of anatomic articular congruity and mechanical alignment restoration, while allowing early knee mobilization.1–8 But open reduction and internal fixation, specifically through compromised soft tissues, has historically been associated with major wound complications.9–11 Alternate methods of treatment have been described, each with its own merits and demerits.1,3,5,7–9,12–14
We evaluated the functional outcome and complications of Schatzker V and VI tibial plateau fractures treated with a lateral plate through an anterolateral approach and a medial plate through a minimally invasive medial approach or an open posteromedial approach.
MATERIALS AND METHODS
We conducted a search of our medical and operation theatre records for patients who had been treated for a tibial plateau fracture. Patients with Schatzker type I, II, III and IV fractures were excluded from the study. Patients whose fractures had been fixed with a single plate or screws were excluded from the study. Forty six patients who presented with Schatzker types V and VI tibial plateau fractures between January 2001 to December 2008 and who had been treated with dual plates were included in the study. Their inpatient records were traced from the medical records department. The patients were called for followup. The preoperative data including demographic data, mode of injury, and fracture classification were collected. Radiographic findings including the fracture pattern, displacement of fragments, and depression of fragments were also noted. Computed tomography (CT) scan findings, intraoperative findings, and data regarding the course in the hospital were collected from the inpatient records. After discharge from the hospital, the patients had been followed up in the outpatient clinic at monthly intervals till fracture union and maximal functional recovery. The followup data were collected from the outpatient records which were retained by the patients and they had brought with them during followup.
Data regarding the age and gender of the patients, mechanism of injury, side, any concomitant injuries and comorbid conditions were collected. The neurovascular status of the fractured leg, presence of compartment syndrome, and the presence of any fracture blisters or open wounds were also noted. In two patients with popliteal artery injury, vascular surgeon's opinion had been sought and Doppler study had been performed. They were taken up for emergency vascular reconstruction by the vascular surgeon, followed by primary internal fixation. The radiographs and CT scan with 3D reconstruction pictures15 were reviewed to note the type of the fracture, the location and extent of articular depression, and fracture extension into the diaphysis, if any.
The fractures were graded preoperatively using the Schatzker's classification of tibial plateau fractures.16 Soft tissue injuries were classified by the Gustilo–Anderson classification of open fractures and Oestern and Tscherne classification of closed fractures.17–19 If there was extensive soft tissue injury, as indicated by soft tissue edema or fracture blisters, surgery was delayed. The limb was elevated and calcaneal pin traction was applied with 3-5 kg of weight. Once the soft tissues recovered, as evidenced by resolution of the edema and the fracture blisters and appearance of skin wrinkles, the patient was taken up for surgery.
The operation notes were reviewed to note the time since injury to the surgery, the duration of the surgery, the type of anesthesia, and the extent of blood loss. Details of the operative technique such as the position of the patient, surgical incisions employed, reduction techniques, use of bone grafts, implants used for fixation, and techniques for assessment of reduction were also recorded.
Antibiotic prophylaxis (intravenous Cefazolin 2 g) was administered at the time of induction of anesthesia in the patients with closed fractures and it was continued for 24 h. In one patient with grade IIIc Gustilo–Anderson open fracture, 2 g of Cefazolin and an aminoglycoside were administered in the emergency room. Prophylaxis was continued for 72 h.
All the patients had undergone open reduction through an anterolateral approach, and a minimally invasive medial or an open posteromedial approach, and internal fixation with a lateral plate, and a medial or posteromedial plate. Surgeries were performed under fluoroscopic control to aid and assess the reduction. All the surgeries were performed by the senior surgeon, (NKS).
Operative procedure
Patients were operated under regional or general anesthesia. They were placed in the supine position on the radiolucent table with a sand bag under the ipsilateral gluteal region for the anterolateral approach, which was removed while starting the minimal invasive medial approach. The sand bag was placed under the contralateral hip if a posteromedial approach was used. Tourniquet was used for all the surgeries except in the two patients with vascular injury and in one patient with impending compartment syndrome.
As the first step, indirect fracture reduction, under image intensifier guidance, was achieved by longitudinal traction provided by the assistant. Percutaneously drilled Kirschner wires were then used as joysticks to fine-tune the reduction of individual fragments or to correct the tilt of articular fragments. The reduced fragments were then provisionally fixed with Kirschner wires. The Kirschner wires were later replaced with interfragmentary screws, either separately or through the plate. The articular reduction was further verified during open reduction by direct visualization through submeniscal arthrotomy. Articular surface depressions were also elevated under direct visualization through the submeniscal arthrotomy, supplemented by the image intensifier. We prefer to elevate the depressed fragment through a separate cortical window on the medial tibial wall using a bone punch. The depressed fragment was elevated with compacted cancellous bone beneath it and the resultant metaphyseal void was filled with autogenous cancellous or synthetic bone graft.
After provisional reduction and fixation with Kirschner wires, the tourniquet was inflated and open reduction was done. We typically fix the medial column first. If the medial condyle was severely comminuted, then we approached and fixed the lateral column first to maintain the length.
The minimally invasive posteromedial approach utilized a 1-inch longitudinal skin incision. The medial or the posteromedial fragment was exposed subperiosteally by elevating the pes anserinus with a periosteal elevator. After reducing the fragment, a small T buttress plate was slid beneath the pes anserinus. Image intensifier was utilized to position the plate below the level of the joint line and the plate was then fixed to the bone with screws inserted through stab incisions [Figure 1].
Figure 1.

(a) Plain radiograph of right tibia anteroposterior view (b) lateral view showing tibial plateau fracture in a postrenal transplant patient. (c) postoperative plain radiograph of right tibia both anteroposterior and lateral views showing dual plate fixation. 2 years followup showing good range of movements (d) extension. (e) flexion. (f) clinical photograph showing anterolateral approach and minimally invasive medial approach
If the medial fragment was more posterior, the open posteromedial approach is used. The skin was incised 1 cm posterior to the posteromedial border of the proximal tibia, curving proximally along the line of the pes anserinus tendons, as was required in four patients. The saphenous vein and nerve were identified and retracted anteriorly. The deep fascia is incised to expose the pes anserinus tendons and the medial head of the gastrocnemius. The pes anserinus tendons are retracted anteriorly and the medial head of the gastrocnemius was gently retracted laterally to expose the posteromedial aspect of the proximal tibia. The fracture edges were exposed to aid in visualizing reduction. Dissection over the subcutaneous anteromedial surface of the proximal tibia was avoided. The posteromedial fragment was reduced and fixed provisionally with Kirschner wires under the guidance of the image intensifier. The fragment was then stabilized with a posteromedial plate. We regularly use the T buttress plate or a 3.5-mm locking proximal medial tibia plate. For anterolateral approach, a curvilinear longitudinal incision was made starting from the lateral femoral epicondyle and passing over the Gerdy's tubercle and running parallel to the shin and 1 cm lateral to it. The iliotibial band was elevated from the Gerdy's tubercle and the underlying capsule. The tibialis anterior was elevated subperiosteally to expose the lateral surface of the lateral tibial condyle and shaft. An “L” buttress plate or a lateral tibial head plate or an anatomical lateral tibial locking plate was used to fix the lateral column. Tibial tuberosity avulsion fractures in two patients were fixed with tension band wiring using two Kirschner wires and a stainless steel wire.
After fixation, the tourniquet was released and hemostasis was achieved. The surgical incisions were closed over a suction drain. Postoperatively, the knee is not immobilized. A light compression dressing was applied.
The data regarding the postoperative rehabilitation, antibiotic prophylaxis, and development of any complications were noted. Postoperative radiographs were reviewed to assess the adequacy of articular reduction, metaphyseo-diaphyseal reduction, and alignment.
No form of knee immobilization was used in any of the patients postoperatively. Non weight-bearing mobilization and quadriceps exercises, were started on the 1st postoperative day (POD) itself. In the two patients with tibial tuberosity avulsions, the rehabilitation protocol was not altered. Patients were mobilized with the aid of axillary crutches or a walking frame, non-weight-bearing on the operated leg. After removal of compression dressings on the 2nd POD, patients were encouraged to do active assisted knee bending exercises and quadriceps exercises. Patients were called for review at 2 weeks, 4 weeks, 8 weeks, 12 weeks, and at monthly intervals thereafter till bony union and maximal functional recovery, to assess the fracture healing and knee joint movements. Weight bearing ambulation was commenced after 12 weeks.
The outpatient records were reviewed to obtain data regarding pain, disability, wound healing, and range of movements of the knee. Followup radiographs were reviewed to note the time to union, any loss of articular reduction, fixation failure, or deformity. After clinical and radiological union, data regarding the functional recovery, such as walking ability, ability to climb and descend stairs, and activities of daily living were recorded. Return to pre-injury employment and ability to participate in sporting activities was also noted.
All the patients who satisfied the selection criteria were called for followup at the end of the study period. Radiographs of the knee and leg in supine position were obtained in the anteroposterior (AP) and lateral planes to assess the articular congruity, the metaphyseo-diaphyseal alignment, and any evidence of new arthritic changes. The patients were also questioned regarding functional recovery and their responses noted. The results were analyzed according to the Oxford knee score criteria. The patients were questioned regarding the degree of pain in the knee during the past week, distance that they are able to walk, any difficulty in toilet activities, any difficulty in getting in and out of a car or bus, getting up from the floor or chair, any limp, ability to kneel and get up, any night pains, ability to do household chores or activities of daily living, climbing on coming down stairs, and household shopping. They were also questioned regarding any giving way of the knee. The scores were graded as poor (0-19), moderate (20-29), good (30-39), and excellent (40-48).
RESULTS
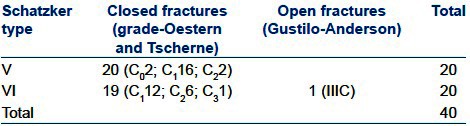
Forty six patients with tibial plateau fractures of Schatzker type V and VI had been treated in our institution between January 2001 and December 2008. Six patients had been lost to followup. The remaining 40 patients with Schatzker type V/VI fractures (n = 20 in each type) were included in this retrospective analysis. Thirty three patients were men and seven patients were women. All the injuries were a result of vehicular accidents, (two-wheeler versus pedestrian in 23 cases, fall from two wheeler in 8 cases, and car versus two wheeler in 9 cases). The age of the patients varied from 22 to 61 years (mean 40 years). Hospital stay varied from 5 to 14 days (mean 6 days). The mean duration of followup was 4 years (range 1-8 years). One patient had an open fracture [Table 1].
Table 1.
Fracture distribution according to type
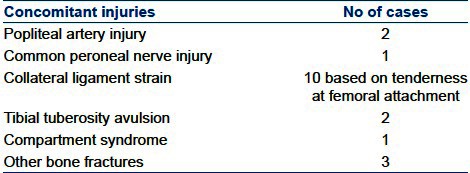
There were 19 concomitant injuries in 18 patients [Table 2]. Two patients had popliteal artery injury (one of whom was the patient with the open fracture who also had a tibial tuberosity avulsion). Common peroneal nerve palsy was seen in one patient, impending compartment syndrome in one patient. Avulsion fracture of the ipsilateral tibial tuberosity was seen in two patients (one of whom was the patient with the open fracture and vascular injury). Three patients had fractures of other bones as well. One patient had fracture of both bones of the ipsilateral forearm, one had an ipsilateral Colles' fracture, and one patient had an ipsilateral fracture shaft of humerus.
Table 2.
Concomitant injuries
All patients underwent surgery at a mean interval of 41 h (range 6-96 h) depending upon severity of the injury and fitness. Emergency surgeries were done in three patients of whom one had an open fracture with a vascular injury, one had a closed fracture with vascular injury, and one had impending compartment syndrome. The two patients with vascular injury underwent vascular reconstruction with reversed saphenous vein graft and primary internal fixation. The patient with impending compartment syndrome underwent fasciotomy, primary internal fixation, primary closure of the operative wound, and split skin grafting of the fasciotomy wound. Tourniquet was not used in these three patients.
Surgeries were performed under fluoroscopic control in all patients to aid and assess the reduction. The open posteromedial approach was used in 4 patients and in the rest 36 cases medial minimal invasive plating was employed. A transverse submeniscal arthrotomy was performed to assess the articular reduction in all the patients.20 Also, radiographs in the AP and lateral planes were performed in the immediate postoperative period to verify articular reduction and meta-diaphyseal alignment restoration in all the cases. The mean duration of the surgery was 1 h 52 min (range: 56 min to 2 hrs 16 min). The average blood loss was 250 ml (range: 200 ml to 350 ml).
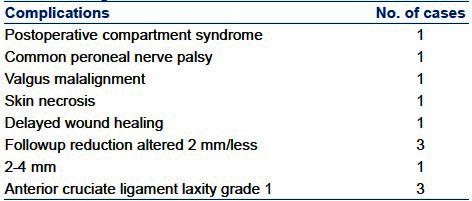
All our patients had union in 8-22 weeks (average 14 weeks). All our patients had 120° and above knee flexion. Four patients had extension lag of less than 5°. None of our patients had deep infection. One patient had valgus malalignment. Articular reduction obtained intraoperatively was lost during the followup period in four patients, ranging from 2 to 4 mm (average 2.7 mm). The alignment of the knee was not affected in these patients. One patient developed increased compartment pressure after skin closure that required fasciotomy and later underwent secondary suturing. Skin necrosis occurred in one patient due to oblique placement of plate which caused persisting pressure on the distal end of suture line and required secondary suturing. Delayed wound healing was present in one patient who had renal transplant which required stopping of immunosuppressant till wound healing. One patient developed common peroneal nerve palsy postoperatively which recovered completely in 6 weeks. The patient with preoperative common peroneal nerve palsy also recovered completely in 6 weeks. Persistent grade 1 ligament laxity of the anterior cruciate ligament was seen in three patients, but no intervention was required [Table 3]. There was no complication in the patients with vascular injury.
Table 3.
Complications
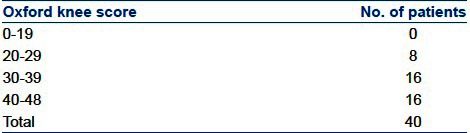
Functional outcome of our patients was graded by the Oxford Knee Score criteria. Sixteen patients had scores between 40 and 48. Sixteen patients had scores between 30 and 39 and 8 patients between 20 and 29 [Table 4]. Sixteen patients had no pain from their operated knee, 14 had very mild pain, while 10 had mild pain. The mean extension was −1.75° (range: −2° to 4°) and the mean flexion was 128.5° (range: 120°-135°).
Table 4.
Oxford knee score
Additional procedures were required in four patients. Wound debridement and secondary suturing was done in one patient who had skin necrosis at the distal end of the anterolateral skin incision due to pressure from the implant. The skin went on to heal uneventfully. One patient, who had undergone fasciotomy for compartment syndrome, required skin grafting of the fasciotomy wounds. One patient [Figure 2], who had an open wound with vascular injury and an avulsion fracture of the tibial tuberosity, required skin grafting for the area of skin loss. The fracture united well and the soft tissues healed uneventfully, but after 4 years, he developed delayed skin necrosis and persistent discharge from the wound overlying the tension band wires. The watery discharge did not grow any organism on culture despite the patient not being on any antibiotic. This required removal of the implants, wound debridement, and a soft tissue flap cover 4 years after the index surgery. None of our patients had new osteoarthrosis changes compared with the contralateral knee at the final followup. At the final followup, the mean medial proximal tibial angle was 84.05° (range: 83°-92°), the mean proximal posterior tibial angle was 8.25° (range: 3°-14°), and the mean condylar width was 2.3 mm (range: 0-5 mm). Three patients had articular step-off of more than 2 mm, 2 patients had a step-off of 2 mm, and 32 patients had a step-off of less than 2 mm. There was no varus–valgus instability at the final followup.
Figure 2.
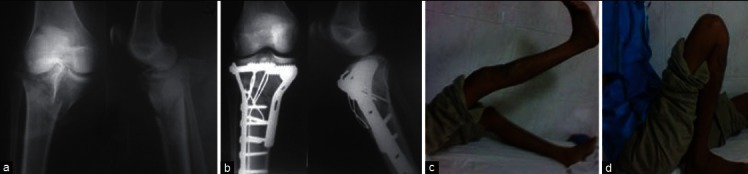
(a) Plain radiograph of right tibia anteroposterior and lateral views showing bicondylar fracture Schatzker type VI (Gustilo–Anderson type IIIc). (b) postoperative plain radiograph of right tibia both AP and lateral views showing dual plate fixation and tension band fixation of tibial tuberosity. clinical 4 years followup showing good range of movements (c) extension (d) flexion
DISCUSSION
High-energy tibial plateau fractures remain a challenge to the orthopedic surgeon. The use of open reduction and internal fixation techniques has historically been associated with wound complications, especially when a single midline incision or a Mercedes-Benz incision is employed. This has led to the emergence of alternate methods of fixation such as Ilizarov ring fixation, external fixation with limited internal fixation, hybrid external fixation, etc., Achieving good reduction and stable fixation sparing knee joint is a challenging task in external fixation.9 Rigid fixation with good articular reduction is an important goal of surgery to get good knee function.20 Open reduction and internal fixation achieves this goal. Most of the open reduction techniques were associated with high wound complication rates due to midline anterior approach or Mercedes-Benz incision. Reaching the posteromedial fragment through a single incision causes wide periosteal stripping and extensive muscle dissection and may hamper reduction as well.10,21,22 Dual incisions are better than single incision.23
Using the image intensifier to aid in indirect reduction techniques and using k wires as joysticks, we were able to obtain reduction of the articular and metaphyseal fragments without damaging the soft tissues. Using minimally invasive techniques on the medial side to place and fix the plates with screws has helped mitigate soft tissue complications. As we were able to obtain rigid fixation with lateral and medial plates, we could dispense with any external knee immobilization and start knee movements in the immediate postoperative period. Also, when the tibial tuberosity was avulsed, we fixed it with two Kirschner wires and tension band wire in order to allow early knee mobilization. This ability to start early aggressive knee rehabilitation has helped us achieve excellent functional outcome in our series, as functional outcome of knee surgeries is so intricately related to knee range of movements in our patient population.
Loss of articular reduction of less than 2 mm was encountered in three patients and of 2-4 mm in one patient due to loosening of screws in the osteoporotic metaphyseal bone, but it did not affect the functional recovery. Minimal articular cartilage incongruity was well tolerated in the knee joint, possibly due to the presence of menisci.24–26 Commonly used techniques to assess articular reduction are fluoroscopy, arthrotomy, and arthroscopy.7,11,27,28 We have no experience in using arthroscopy to assess or assist reduction.29,30 We have relied entirely on fluoroscopy and submeniscal arthrotomy in all cases to assess articular reduction intraoperatively.
Most of the degenerative changes occur in the first 6-8 years of the initial injury.24,31–33 The probability of degenerative changes increased significantly with higher age at the time of injury. The main factors in preventing early degenerative changes after intraarticular fractures appear to be the early restoration of joint congruity, realignment to the normal anatomical axis, joint stability, and early movement.32 Our study population was mainly in third or fourth decade, and that may be the reason for no new osteoarthrosis changes in the series.24,31–33 We found that ligament laxity has a greater impact on the functional outcome than minor irregularity in articular cartilage.24,26,32,33
Other authors have reported similar good results with dual plating in this difficult subset of fractures. Chang-Wug Oh et al.34 reported the outcome of double plating in a series of 23 unstable proximal tibial fractures in 23 patients with a mean age of 54 years. All fractures healed at an average of 19 weeks. Twenty one patients had excellent or good clinical and radiographic results. There was one case of shortening (1 cm), two cases of mild varus malalignment (less than 10°), and one case of superficial infection which healed after hardware removal. No deep infections occurred.
In our series, we had one case of postoperative common peroneal nerve palsy, possibly due to intraoperative stretching while achieving reduction. It recovered completely in 6 weeks. One patient had delayed wound gaping due to pressure from the implant. He required wound debridement and secondary suturing and had an uneventful course thereon. One patient had a valgus angulation due to premature weight-bearing.
We conclude that open reduction and internal fixation of high-energy tibial plateau fractures with dual plates gives excellent to good functional outcome with minimal soft tissue complications. The minimally invasive approach should be utilized wherever possible, preventing soft tissue problems, and thus avoiding wound healing issues. Rigid fixation obtained with dual plating is essential to start early aggressive rehabilitation. Regaining full range of movements depends on early and aggressive knee mobilization, and this goes a long way in ensuring optimal functional recovery and patient satisfaction.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Dendrinos GK, Kontos S, Katsenis D, Dalas A. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996;78:710–7. [PubMed] [Google Scholar]
- 2.Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation of comminuted tibial plateau fractures. Clin Orthop Relat Res. 1996;328:203–10. doi: 10.1097/00003086-199607000-00032. [DOI] [PubMed] [Google Scholar]
- 3.Marsh JL, Smith ST, Do TT. External fixation and limited internal fixation for complex fractures of the tibial plateau. J Bone Joint Surg Am. 1995;77:661–73. doi: 10.2106/00004623-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Ries MD, Meinhard BP. Medial external fixation with lateral plate internal fixation in metaphyseal tibia fractures. A report of eight cases associated with severe soft-tissue injury. Clin Orthop Relat Res. 1990;256:215–23. [PubMed] [Google Scholar]
- 5.Stamer DT, Schenk R, Staggers B, Aurori K, Aurori B, Behrens FF. Bicondylar tibial plateau fractures treated with a hybrid ring external fixator: A preliminary study. J Orthop Trauma. 1994;8:455–61. [PubMed] [Google Scholar]
- 6.Waddell JP, Johnston DW, Neidre A. Fractures of the tibial plateau: A review of ninety-five patients and comparison of treatment methods. J Trauma. 1981;21:376–81. doi: 10.1097/00005373-198105000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Watson JT. High-energy fractures of the tibial plateau. Orthop Clin North Am. 1994;25:723–52. [PubMed] [Google Scholar]
- 8.Weiner LS, Kelley M, Yang E, Steuer J, Watnick N, Evans M, et al. The use of combination internal fixation and hybrid external fixation in severe proximal tibia fractures. J Orthop Trauma. 1995;9:244–50. doi: 10.1097/00005131-199506000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Mallik AR, Covall DJ, Whitelaw GP. Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev. 1992;21:1433–6. [PubMed] [Google Scholar]
- 10.Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: Definition, demographics, treatment rationale, and long term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1:97–119. [PubMed] [Google Scholar]
- 11.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994;23:149–54. [PubMed] [Google Scholar]
- 12.Mikulak SA, Gold SM, Zinar DM. Small wire external fixation of high energy tibial plateau fractures. Clin Orthop Relat Res. 1998;356:230–8. doi: 10.1097/00003086-199811000-00031. [DOI] [PubMed] [Google Scholar]
- 13.Murphy CP, D'Ambrosia R, Dabezies EJ. The small pin circular fixator for proximal tibial fractures with soft tissue compromise. Orthopedics. 1991;14:273–80. [PubMed] [Google Scholar]
- 14.Watson JT, Coufal C. Treatment of complex lateral plateau fractures using Ilizarov techniques. Clin Orthop Relat Res. 1998;353:97–106. doi: 10.1097/00003086-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Dias JJ, Stirling AJ, Finlay DB, Gregg PJ. Computerised axial tomography for tibial plateau fractures. J Bone Joint Surg Br. 1987;69:84–8. doi: 10.1302/0301-620X.69B1.3818741. [DOI] [PubMed] [Google Scholar]
- 16.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The toronto experience 1968-1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 17.Dirschl DR, Dawson PA. Injury severity assessment in tibial plateau fractures. Clin Orthop Relat Res. 2004;423:85–92. doi: 10.1097/01.blo.0000132626.13539.4b. [DOI] [PubMed] [Google Scholar]
- 18.Gustilo RB, Merkow RL. Templeman D: The management of open fractures. J Bone Joint Surg Am. 1990;72:299–304. [PubMed] [Google Scholar]
- 19.Oestern HJ, Tscherne H. Pathophysiology and classification of soft tissue injuries associated with fractures. In: Tscherne H, editor. Fractures with soft tissue injuries. New York: Springer-Verlag; 1984. pp. 1–9. [Google Scholar]
- 20.Su EP, Westrich GH, Rana AJ, Kapoor K, Helfet DL. Operative treatment of tibial plateau fractures in patients older than 55 years. Clin Orthop Relat Res. 2004;421:240–8. doi: 10.1097/01.blo.0000119247.60317.bc. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez DL. Anterior approach to the knee with osteotomy of the tibial tubercle for bicondylar tibial fractures. J Bone Joint Surg Am. 1988;70:208–19. [PubMed] [Google Scholar]
- 22.Moore TM. Fracture-dislocation of the knee. Clin Orthop Relat Res. 1981;156:128–40. [PubMed] [Google Scholar]
- 23.Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke SK. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am. 2006;88:1713–21. doi: 10.2106/JBJS.E.00907. [DOI] [PubMed] [Google Scholar]
- 24.Buckwalter JA, Brown TD. Joint injury, repair, and remodeling: roles in posttraumatic osteoarthritis. Clin Orthop. 2004;423:7–16. [PubMed] [Google Scholar]
- 25.Lundy DW, Albert MJ. Pearls and pitfalls in the treatment of tibial plateau fractures. AAOS Now. 2007 Sep;1:21. [Google Scholar]
- 26.Honkonen SE. Degenerative arthritis after tibial plateau fractures. J Orthop Trauma. 1995;9:273–7. doi: 10.1097/00005131-199509040-00001. [DOI] [PubMed] [Google Scholar]
- 27.Buchko GM, Johnson DH. Arthroscopy assisted operative management of tibial plateau fractures. Clin Orthop Relat Res. 1996;332:29–36. doi: 10.1097/00003086-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Caspari RB, Hutton PM, Whipple TL, Meyers JF. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy. 1985;1:76–82. doi: 10.1016/s0749-8063(85)80035-9. [DOI] [PubMed] [Google Scholar]
- 29.Holzach P, Matter P, Minter J. Arthroscopically assisted treatment of lateral tibial plateau fractures in skiers: Use of a cannulated reduction system. J Orthop Trauma. 1994;8:273–81. doi: 10.1097/00005131-199408000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Jennings JE. Arthroscopic management of tibial plateau fractures. Arthroscopy. 1985;1:160–8. doi: 10.1016/s0749-8063(85)80003-7. [DOI] [PubMed] [Google Scholar]
- 31.Volpin G, Dowd GS, Stein H, Bentley G. Degenerative arthritis after intraarticular fractures of the knee, long term results. J Bone Joint Surg Br. 1990;72:634–8. doi: 10.1302/0301-620X.72B4.2380219. [DOI] [PubMed] [Google Scholar]
- 32.McKinley TO, Rudert MJ, Koos DC, Brown TD. Incongruity versus instability in the etiology of posttraumatic arthritis. Clin Orthop Relat Res. 2004;423:44–51. doi: 10.1097/01.blo.0000131639.89143.26. [DOI] [PubMed] [Google Scholar]
- 33.Wang S, Gao Y, Wang J, Zhang C, Mei J, Rao Z. Surgical approach for high-energy posterior tibial plateau fractures. Indian J Orthop. 2011;45:125–31. doi: 10.4103/0019-5413.77131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oh CW, Oh JK, Kyung HS, Jeon IH, Park BC, Min WK, et al. Double plating of unstable proximal tibial fracturesusing minimally invasive percutaneous osteosynthesis technique. Acta Orthop. 2006;77:524–30. doi: 10.1080/17453670610012548. [DOI] [PubMed] [Google Scholar]


