Abstract
Desmoplastic fibroma is a rare, well differentiated, locally aggressive fibrous tumor usually arising from soft tissues, and rarely from bones. Involvement of forearm bones is extremely unusual. We present a large desmoplastic fibroma of right ulna in a 15-year-old male. The tumor was excised with a wide margin, and the bony defect was reconstructed with nonvascular autologous fibular graft. Reconstruction of the olecranon process was attempted using the fibular head and the remaining olecranon. At 2-years followup, there was no recurrence, flexion extension arc of the elbow joint was 40°–130° and there was no restriction of activities of daily living.
Keywords: Autologous fibular graft, desmoplastic fibroma, tumor reconstruction
INTRODUCTION
Desmoplastic fibroma of bone is a well differentiated, locally aggressive fibrous tumor that histologically resembles the extra abdominal desmoid tumor of soft tissues. It is extremely rare, and less than 200 cases have been reported so far.1,2 The most common site of affection is the jaw, followed by pelvis and long bones.3,4 Forearm bones are rarely involved.5–8 The mainstay of treatment is surgical excision. Wide excision followed by reconstruction of the bony defect using fibular graft has been widely described in tumor surgery. Fibular graft functions well as an intercalary graft; even, there are reports of reconstruction of the distal radius (after excision of giant cell tumor) using fibular graft where the fibular head functions as an articular part of the wrist joint. However, there are no reports of the use of fibular graft in reconstruction of the elbow joint.
We report a case of giant desmoplastic fibroma of ulna that has involved the proximal two thirds. It was excised and reconstructed with nonvascularized fibular graft. The unique technique of reconstruction of the olecranon process with the articular surface of the fibular head has been described.
CASE REPORT
A 15-year-old child presented with a 3-year history of progressively increasing swelling in the right forearm. There was no significant pain or constitutional symptoms. Local examination revealed a diffuse swelling over dorsomedial and medial aspects of the forearm, extending from just below the elbow joint to about 8 cm above the wrist. Overlying skin was normal and there was no local tenderness. Swelling was firm in consistency, with a bosselated surface and was arising from ulna. There was full range of motion of the elbow and wrist joints.
Plain radiograph showed an expansile osteolytic growth involving the proximal ulnar metaphysis and two-third of the diaphysis [Figure 1a]. There was honeycomb pattern with coarse ridge like trabeculae, and matrix was purely lytic. Overlying cortex appeared intact. Magnetic resonance imaging showed a large circumferential growth arising from the central medullary canal, expanding the bone [Figure 1b]. Surrounding cortex was intact and there was no soft tissue component. Elbow and wrist joints were free of tumor. The tumor appeared iso- to hypointense to muscle on T1-weighted images and the majority of the tumor areas were isointense to surrounding muscle on T2-weighted images. Core biopsy of the lesion was suggestive of a desmoplastic fibroma.
Figure 1.
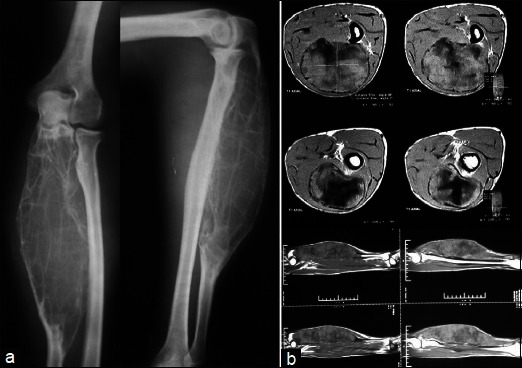
(a) Preoperative anteroposterior and lateral radiographs showing a well demarcated expansile osteolytic growth involving about two-thirds of ulna. (b) magnetic resonance imaging showing a large circumferential growth from the central medullary canal, expanding the bone. Surrounding cortex is intact and there is no soft tissue component
The tumor was excised including half of the olecranon process and distally up to about 9 cm from the wrist joint. Intraoperative frozen section revealed a negative tumor margin. On gross examination, the tumor measured 18 cm × 10 cm. Cut surface showed a homogenous grayish white appearance destroying the entire bone with intermittent ballooning of the cortex. Reconstruction of the bony defect was performed using autologous nonvascularized fibular graft. Fibular head and diaphyses measuring 18 cm were harvested from ipsilateral leg. The head of fibula was cut transversely to match the remaining half of the olecranon process to recreate the elbow joint. This was fixed with the remainder of the olecranon process with tension band wires and a square nail. The head of the fibula was cut transversely, and the distal part of the head and shaft was used for reconstruction. The transverse cut in the head of fibula was aligned at the articular surface with the remaining proximal olecranon. This was fixed with tension band wires and a square nail. Distally fibular diaphysis was fixed with ulnar shaft with a dynamic compression plate [Figures 2, 3]. The functional attachment of the triceps was that which remained attached to the proximal olecranon. Some part of the triceps attachment was also freed from the resected part of the ulna. This was sutured back to the tension band wiring construct and surrounding soft tissues.
Figure 2.

Postoperative radiograph anteroposterior and lateral views of the same patient showing restoration of the proximal ulnar anatomy with fixation hardware in situ
Figure 3.
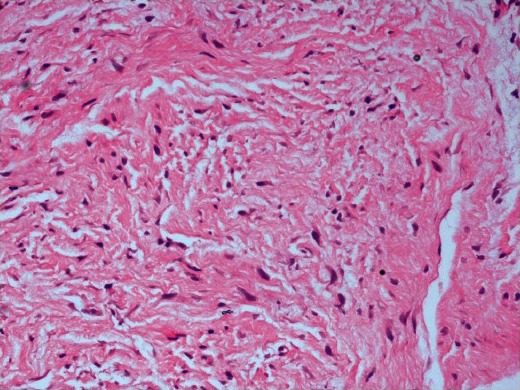
20× microscopic field of the tumor section showing monomorphic cells without any anaplastic changes, interspersed between the strands of collagen, arranged in a parallel fashion
Histopathology of the tumor revealed a moderately cellular lesion on low-power microscopy, with spindle-shaped cells interspersed between the strands of collagen, arranged in a parallel fashion. On high-power microscopic field, there was clustering of monomorphic cells without any anaplastic changes or mitosis [Figure 3]. Periphery of the lesion showed no invasion of the surrounding tissues.
Patient was followed up for 2 years with no evidence of recurrence. The fibular graft united with the olecranon proximally and distally with remaining part of ulna. Elbow range of motion was 40°–130° and was pain free [Figure 4]. There was 70° arc of supination and pronation. No donor site morbidity was seen in the leg from where fibula was harvested.
Figure 4.

Followup radiographs at 2 years showing union of the fibular graft with proximal ulna and some restoration of the elbow joint (a,b). clinical photographs showing the range of elbow motion at followup (c,d)
DISCUSSION
Desmoplastic fibroma of bones is considered to be locally aggressive with a high recurrence rate. Radiological differential diagnosis include other lytic lesions such as aneurysmal bone cyst, giant cell tumour, chondromyxoid fibroma, and low-grade fibrosarcoma. Treatment of choice is wide local excision through the normal soft tissue.7,8 Recurrence rate is 17% following resection and as high as 55% following curettage.2
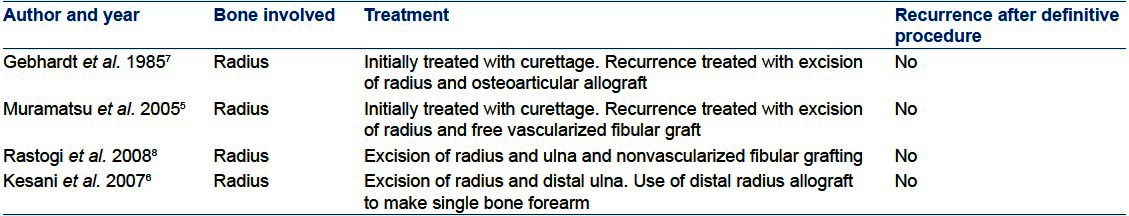
Various options have been used in literature [Table 1] for the reconstruction of bone defects in forearm following tumor resections, such as creation of single bone forearm from radius and ulna and centralizing the carpus over the single bone, free fibular graft, fibular head graft for distal radius, and microvascular fibular graft and allografts. Free fibular graft has proved to a good option for reconstruction of bony defects and has been extensively used in tumor surgery. The technique we have used to create the articular surface of the olecranon using the fibular head articular surface has not been previously described. Though a normal joint surface cannot be expected, this reconstruction is an acceptable option considering the morbidity of the tumor resection for elbow function. Elbow is not a weight-bearing joint and some degree of degenerative changes can be tolerated. This will provide a more stable and mobile elbow joint compared to the single bone forearm.
Table 1.
Review of literature on desmoplastic fibroma arising from bone in forearm
Proximal half of the olecranon has been preserved during excision based on intraoperative frozen section. Thus, the fibular graft functioned as an intercalary graft between the olecranon proximally and distal third ulna distally. This was very important in two ways. Firstly, it helped to maintain some integrity of the extensor apparatus of the elbow to have some useful elbow function also to and counterbalance the elbow flexors. Secondly, it provided a surface to articulate with the trochlea to provide some stability and mobility of the elbow joint. Most of the elbow articulation was made from this segment of the olecranon that was preserved. Following principles of olecranon reconstruction from trauma surgery, elbow joint can be reasonably restored even if a large part of olecranon is sacrificed, provided the triceps mechanism is restored.9,10 This explains the reasonable range of motion achieved in elbow in this case.
Thus, desmoplastic fibroma is a rare tumor of bone with a benign but locally aggressive behavior. Diagnosis is based on clinic-radio-pathological correlation. Treatment of choice is wide local excision. Free fibular graft is an excellent option for reconstruction for defects in upper limb.10
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Nag HL, Kumar R, Bhan S, Awasthy BS, Julka PK, Ray RR. Radiotherapy for desmoplastic fibroma of bone: A case report. J Orthop Surg (Hong Kong) 2003;11:90–3. doi: 10.1177/230949900301100117. [DOI] [PubMed] [Google Scholar]
- 2.Böhm P, Kröber S, Greschniok A, Laniado M, Kaiserling E. Desmoplastic fibroma of the bone: A report of two patients, review of the literature, and therapeutic implications. Cancer. 1996;78:1011–23. doi: 10.1002/(SICI)1097-0142(19960901)78:5<1011::AID-CNCR11>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 3.Bertoni F, Calderoni P, Bacchini P, Campanacci M. Desmoplastic fibroma of bone. A report of six cases. J Bone Joint Surg Br. 1984;66:265–8. doi: 10.1302/0301-620X.66B2.6707066. [DOI] [PubMed] [Google Scholar]
- 4.Taconis WK, Schütte HE, van der Heul RO. Desmoplastic fibroma of bone: A report of 18 cases. Skeletal Radiol. 1994;23:283–8. doi: 10.1007/BF02412362. [DOI] [PubMed] [Google Scholar]
- 5.Muramatsu K, Ihara K, Azuma E, Orui R, Goto Y, Shigetomi M, et al. Free vascularized fibula grafting for reconstruction of the wrist following wide tumor excision. Microsurgery. 2005;25:101–6. doi: 10.1002/micr.20088. [DOI] [PubMed] [Google Scholar]
- 6.Kesani AK, Tuy B, Beebe K, Patterson F, Benevenia J. Single-bone forearm reconstruction for malignant and aggressive tumors. Clin Orthop Relat Res. 2007;464:210–6. doi: 10.1097/BLO.0b013e318156fb30. [DOI] [PubMed] [Google Scholar]
- 7.Gebhardt MC, Campbell CJ, Schiller AL, Mankin HJ. Desmoplastic fibroma of bone. A report of eight cases and review of the literature. J Bone Joint Surg Am. 1985;67:732–47. [PubMed] [Google Scholar]
- 8.Rastogi S, Varshney MK, Trikha V, Khan SA, Mittal R. Desmoplastic fibroma: A report of three cases at unusual locations. Joint Bone Spine. 2008;75:222–5. doi: 10.1016/j.jbspin.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Sanfilippo NJ, Wang GJ, Larner JM. Desmoplastic fibroma: A role for radiotherapy? South Med J. 1995;88:1267–9. doi: 10.1097/00007611-199512000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Colton CL. Fractures of the olecranon in adults: Classification and management. Injury. 1973;5:121–9. doi: 10.1016/s0020-1383(73)80088-9. [DOI] [PubMed] [Google Scholar]


