Abstract
Background
In the general population, job insecurity may be as harmful to health as unemployment. Some evidence suggests that employment is associated with better health outcomes among people with HIV, but it is not known whether job security offers additional quality-of-life benefits beyond the benefits of employment alone.
Methods
We used baseline data for 1660 men and 270 women who participated in the Ontario HIV Treatment Network Cohort Study, an ongoing observational cohort study that collects clinical and socio-behavioural data from people with HIV in the province of Ontario, Canada. We performed multivariable regression analyses to determine the contribution of employment and job security to health-related quality of life after controlling for potential confounders.
Results
Employed men with secure jobs reported significantly higher mental health–related quality of life than those who were non-employed (β = 5.27, 95% confidence interval [CI] 4.07 to 6.48), but insecure employment was not associated with higher mental health scores relative to non-employment (β = 0.18, 95% CI –1.53 to 1.90). Thus, job security was associated with a 5.09-point increase on a 100-point mental health quality-of-life score (95% CI 3.32 to 6.86). Among women, being employed was significantly associated with both physical and mental health quality of life, but job security was not associated with additional health benefits.
Interpretation
Participation in employment was associated with better quality of life for both men and women with HIV. Among men, job security was associated with better mental health, which suggests that employment may offer a mental health benefit only if the job is perceived to be secure. Employment policies that promote job security may offer not only income stability but also mental health benefits, although this additional benefit was observed only for men.
The detrimental effects of job loss on health have been well documented in the general population.1,2 Several longitudinal studies have shown a relationship between unemployment and mortality.3,4 The scientific evidence linking unemployment and poor health is substantial enough to suggest that a portion of the association is causal.5,6 Likewise, the perceived threat of unemployment implies the loss of important financial resources and the potential frustration of some of the needs thought to be associated with the health benefits of employment, including structured time and regular activity, regular contact with people outside the immediate family, connection with goals that transcend one’s own, and identity and position within society.7,8 Some studies have suggested that job insecurity (the perception that one may lose one’s job, as well as negative work-related conditions) may be as detrimental to health as job loss itself.9,10 In this sense, job insecurity, which refers to a subjective experience that includes a threat of involuntary job loss and which involves a degree of uncertainty about the future,8,11,12 represents a classic work stressor and can result in various strains, according to stress process theory.13,14
A meta-analysis of mainly cross-sectional studies in the general population found that job insecurity was associated with poorer health, particularly mental health.15 Subsequent studies have also reported significant associations between job insecurity and a variety of health outcomes, including self-rated health, minor psychiatric disorders and/or depressive symptoms,16-18 increased use of health services and visits to general practitioners,19 high cholesterol levels and high blood pressure,16 and coronary artery disease.20
Published reports of gender differences in the association between job insecurity and health have been inconsistent. Several studies have reported similar effects of job insecurity for men and women in the general population.16,21,22 However, one study found that gender moderated the association between job insecurity and well-being, indicating that job insecurity did not affect psychological well-being in women.8 One longitudinal study found that job insecurity predicted severe depressive symptoms in men but not in women,23 and another study found that job insecurity was associated with poor health for both men and women, but that the effect was stronger for men.24
Although there is substantial evidence linking job insecurity with health in the general population and with health conditions other than HIV/AIDS, there is a lack of evidence for people living with HIV, a group that has a high prevalence of unemployment, ranging from 45% to 62%.25,26 Given the unique nature and episodic course of HIV disease, this issue is particularly salient.
The study of the relationship between work and health has traditionally focused on the negative effects of job loss or unemployment rather than the positive effects of employment and return to work. We have recently shown, in a systematic review of longitudinal studies, that return to work has beneficial effects on health in a variety of populations, time frames and settings.27 In the context of HIV, we have also shown, in a cross-sectional study28 and a longitudinal study,29 that employment is associated with better physical and mental health quality of life. The specific objective of the study reported here was to evaluate whether job security offers additional quality-of-life benefits beyond those provided by employment alone—for both men and women living with HIV—while controlling for clinical and socio-behavioural factors.
Methods
Study population and design
This cross-sectional study presents baseline enrolment data collected between October 2007 and July 2009 from the Ontario HIV Treatment Network Cohort Study. This ongoing longitudinal observational cohort study collects data on the clinical profile and social determinants of health of people living with HIV at 11 clinical sites across the province of Ontario, Canada. There is substantial diversity among the study participants, who broadly represent the population of HIV patients receiving care in Ontario.30 A profile of the cohort and the survey recruitment details are available elsewhere.30,31
Eligible participants in this cohort study are adults (>16 years old) with evidence of HIV infection (positive result on HIV antibody test or laboratory evidence of HIV infection) who are residents of Ontario and are able to provide informed consent. Enrolled patients receive an honorarium for participation. The HIV Research Ethics Board of the University of Toronto approved the study.
Measures
We used a structured interview format to collect socio-demographic data.30 We dichotomized sexual orientation as heterosexual versus gay, lesbian or bisexual; marital status as married or living common-law with a partner versus single, separated, divorced or widowed; ethnicity as white versus non-white; country of birth as Canada versus outside Canada; education as high school diploma or above versus less than high school; and personal income as at least $30 000/year versus less than $30 000/year (based on the median value for this variable). Non-medicinal use of drugs was assessed by a single item asking participants to report whether they had used drugs for non-medicinal purposes in the past 6 months. We used a validated questionnaire to measure alcohol use32 and used the Canadian Community Health Survey definition of heavy alcohol use (i.e., participant reported drinking alcohol in the past 12 months, had 5 or more drinks on a typical day and did this more than once a month).
Data on CD4 cell count (i.e., immune cell count) were collected through electronic medical records and chart abstractions. Information about viral load was obtained through a data linkage with Public Health Ontario Laboratories, an agency that conducts serological, viral and bacteriological test results for the province.30 We categorized recent CD4 counts as at least 500 cells/μL versus less than 500 cells/μL and recent viral load as detectable (≥ 50 copies/mL) versus undetectable (< 50 copies/mL).
We dichotomized employment status as employed (i.e., working for pay) versus non-employed (i.e., unemployed, volunteering, student, retired or on disability) and job security as secure, if participants reported feeling “secure or very secure,” versus insecure, if they reported feeling “very insecure, insecure or neutral” on the job security item (“How secure do you feel in your current job?”). We then created a 3-level employment/job security variable that combined these 2 dichotomous variables as securely employed, insecurely employed and non-employed.
We administered the SF-12 Health Survey33 to those participants who completed the core questionnaire for the cohort study (at 7 sites across the province of Ontario) and the SF-36 Health Survey34 to those participants who completed an extended version of the questionnaire (at 4 sites in Toronto). We followed the developers’ instructions to compute the Physical Component Summary (PCS) and the Mental Component Summary (MCS) scores using the SF-12 for all participants, because the 12 items of the SF-12 are also included within the SF-36 and form the same 8 health domains in both versions of the instrument (i.e., general health perception, physical functioning, role functioning, body pain, vitality, social functioning, role emotional and mental health).33
Statistical analysis
To determine whether individuals excluded from analysis (as described below) were significantly different from those included in the analyses, we compared the sample characteristics for the 2 groups using t tests for continuous variables and Pearson’s χ2 tests for categorical variables.
We performed bivariable regression analyses between the SF-12 PCS and MCS scores and each of the predictor variables to determine which variables were most strongly associated with each outcome. We selected for inclusion in the regression models the covariates that showed the strongest relationship with the particular outcome of interest (p < 0.10). When 2 covariates were highly correlated (e.g., CD4 counts and viral load), we selected the variable that showed the strongest association with the outcome of interest. We fitted 2 separate models, including the PCS and the MCS scores as the health-related quality-of-life outcomes, and we included the employment/job security variable in all multivariable regression models. The final models included only those predictors with significant associations with the outcomes (p < 0.05), and we ensured that potential effect modifiers did not affect the coefficient of employment/job security. Post hoc multiple comparisons (i.e., least significant difference tests) were conducted to compare PCS and MCS scores among participants who were employed with a secure job, those who were employed with an insecure job and non-employed participants. All analyses were performed using SPSS 16.0 (SPSS Inc., Chicago, Illinois).
Results
Participants
We collected baseline data from 2127 participants in the Ontario HIV Treatment Network Cohort Study. For multivariable analyses, we excluded 197 participants (173 because of missing data on key variables of interest and 24 who identified as transgender, inter-sexed or 2-spirited [see below]). The remaining 1930 participants who were included in the final analyses were not significantly different from the 197 people who were excluded in terms of age, education, recent CD4 counts, job security, non-medicinal use of drugs, alcohol use, and physical and mental health–related quality of life. However, a higher proportion of included participants were male (86% v. 79%, p = 0.006), gay, lesbian or bisexual (71% v. 61%, p = 0.003), white (74% v. 64%, p = 0.004), born in Canada (71% v. 64%, p = 0.035), married or living in a common-law relationship (39% v. 31%, p = 0.019) and employed (47% v. 34%, p = 0.001), and a higher proportion had an annual income of at least $30 000 (45% v. 30%, p = 0.001). Participants included in our final analyses were also more likely to have undetectable viral load (75% v. 65%, p = 0.002) and longer duration since HIV diagnosis (11.4 v. 9.6 years, p = 0.001). We conducted the same regression analyses using mean substitution on the missing variables, and the results were similar to the models reported in this paper. Thus, we report the regression models using the participants with complete data.
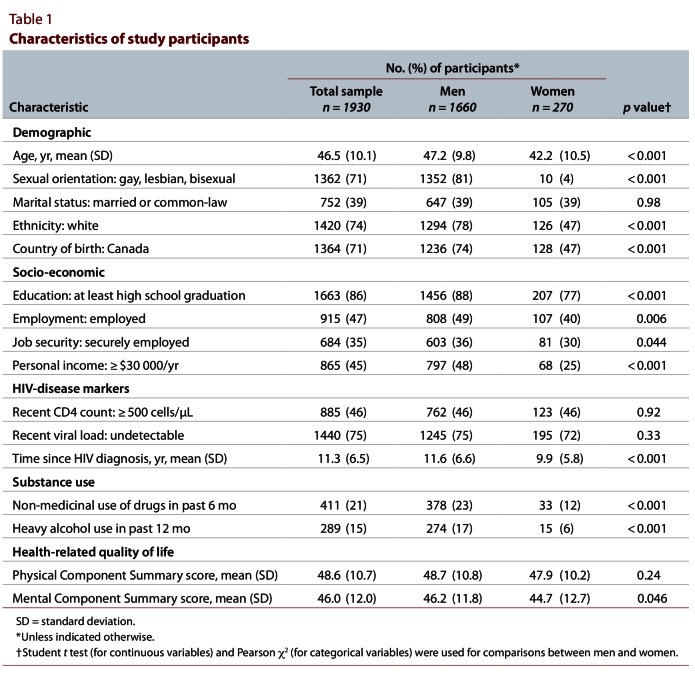
Men and women were significantly different in terms of several key variables, including both the main predictors (employment status and job security) and one of the outcomes (mental health–related quality of life). Thus, we decided to stratify by gender instead of adjusting for its effects. Men were significantly more likely to be older, gay or bisexual, white, Canadian-born and employed (Table 1). Men were also more likely to have a higher level of education and higher income and to report having a secure job. In addition, men were more likely to have lived for longer since their HIV diagnosis and to report non-medicinal use of drugs, heavy alcohol use and better mental health–related quality of life. As noted above, we excluded 24 participants who identified as transgender, inter-sex or 2-spirited because these people did not identify themselves as men or women, and their data could therefore not be stratified by gender.
Table 1.
Characteristics of study participants
Associations between sample characteristics and health-related quality of life for men
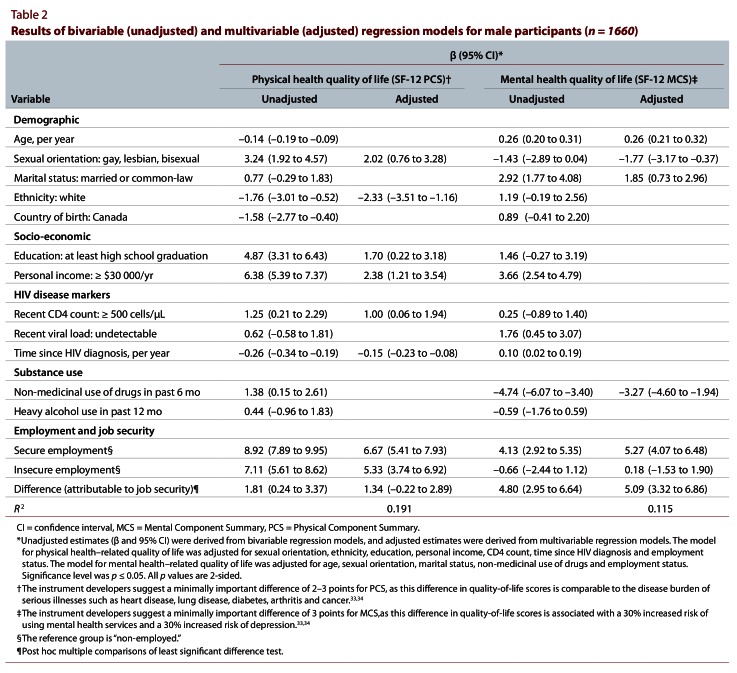
Multivariable analyses showed that, among men, being employed (regardless of job security level) was associated with physical health–related quality of life after controlling for being gay or bisexual, being non-white, having a higher level of education, having more income, having higher CD4 counts and having been diagnosed with HIV for a shorter period of time (Table 2). After adjustment for potential confounders, secure employment was associated with a 6.67-point increase on a 100-point physical health score (95% confidence interval [CI] 5.41 to 7.93) and insecure employment was associated with a 5.33-point increase (95% CI 3.74 to 6.92) in physical health relative to non-employment. With a suggested minimally important difference of 2–3 points for the physical health–related quality-of-life scores, the associations for both secure and insecure employment were both statistically and clinically significant. Thus, job security was not significantly associated with physical health–related quality of life (β = 1.34, 95% CI –0.22 to 2.89).
Table 2.
Results of bivariable (unadjusted) and multivariable (adjusted) regression models for male participants
Multivariable analyses also showed that job security was associated with mental health–related quality of life among men, which suggests that employment may offer a mental health benefit only if the job is perceived to be secure (Table 2). Employed men with secure jobs reported significantly higher mental health–related quality of life than those who were non-employed (β = 5.27, 95% CI 4.07 to 6.48), but insecure employment was not associated with a significant increase in mental health relative to non-employment (β = 0.18, 95% CI –1.53 to 1.90). Thus, after adjustment for potential confounders, job security was associated with an average increase of 5.09 points in mental health (95% CI 3.32 to 6.86). With a suggested minimally important difference of 3 points for the mental health–related quality-of-life scores, this association was statistically and clinically significant. Being older, heterosexual, married or living in a common-law relationship and not participating in non-medicinal drug use were also associated with higher mental health scores.
Associations between sample characteristics and health-related quality of life for women
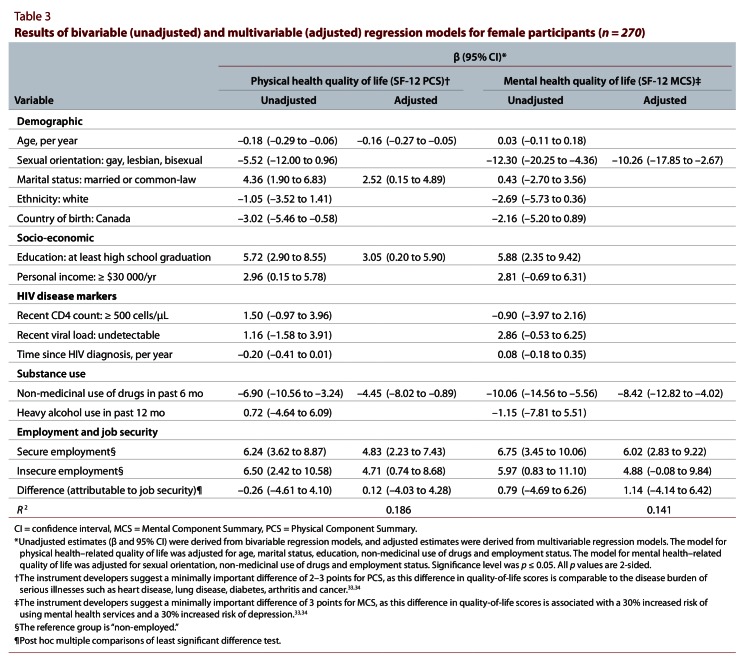
Multivariable analyses showed that, among women, being employed (regardless of job security level) was significantly associated with both physical and mental health–related quality of life (Table 3). After adjustment for potential confounders, secure employment was associated with an average increase of 4.83 points (95% CI 2.23 to 7.43) and insecure employment with an increase of 4.71 points (95% CI 0.74 to 8.68) in physical health compared with non-employment. Thus, the additional physical health benefit attributed to job security was minimal and non-significant (β = 0.12, 95% CI –4.03 to 4.28). Younger age, being married, having a higher level of education and not participating in non-medicinal drug use were also associated with better physical health. For mental health, having a secure job was associated with an average increase of 6.02 points (95% CI 2.83 to 9.22) relative to non-employment, after adjustment for potential confounders. Being lesbian or bisexual and participating in non-medicinal drug use were also independently associated with lower mental health–related quality of life. With a suggested minimally important difference of 3 points, the association between secure employment and mental health–related quality of life was both statistically and clinically significant, whereas the association between insecure employment and mental health was not statistically significant but may be of clinical importance.
Table 3.
Results of bivariable (unadjusted) and multivariable (adjusted) regression models for male participants
Interpretation
This paper conceptually expands on previous studies that have evaluated the health effects of the availability of work (i.e., employment versus non-employment)28,29,35 by examining the association between health and one aspect of the nature or quality of work (i.e., job security). We found that for men living with HIV, having a job was associated with better mental health only if the job was perceived as being secure, which suggests that the level of job security makes a difference to mental health. However, we also found that job security was not associated with additional physical health benefits beyond those provided by employment alone, which suggests that work is associated with better physical health regardless of the level of job security. For women living with HIV, however, although employment was associated with both better physical and mental health, job security did not provide additional health benefits, which suggests that having a job is more important than the level of security that the job is perceived to offer. We also found that the additional effect sizes associated with job security for both men and women were higher for mental health than for physical health quality of life.
Our finding of a stronger relationship between job security and health among men with HIV than among women with this condition is consistent with some studies conducted in non-HIV populations,8,23,24 but not all.16,21,22 This finding can be explained in part by role theory, which suggests that having a secure job is central to men’s traditional role of being the primary source of family support; hence, losing a job or having an insecure job is more stressful for them.8 This could be true of both gay and straight men, as both groups would typically have no expectation of financial dependence on partners or spouses. Conversely, it is also plausible that the women in this study represented a more vulnerable group, who face more fundamental challenges derived from the combination of other hardships. For example, the women in this study were more likely than the men to be foreign-born, non-white and non-employed. They also had less education, generated less income and were more likely to be working in insecure jobs. It might be that the cumulative effect of these factors placed more pressure on the importance of having a job, any job, regardless of the level of security that the job could offer. It is also possible that for this particularly vulnerable group, the instability of the job did not constitute a sufficiently salient threat relative to the other social challenges they were facing. In addition, given that women are more likely than men to be over-represented in precarious employment,36 they would generally have lower expectations related to job security and stability. This suggests that gender differences may be explained—at least in part—by the differences in the structure of occupations and the characteristics of jobs available to men and women.
Our finding of a stronger association between job security and mental health than between job security and physical health is consistent with studies that have evaluated the contribution of job insecurity to poor health in the general population. One meta-analysis reported that the average size of the associations between job insecurity and mental health was greater in magnitude than the average size of such associations for physical health.15 A potential explanation for this finding is that the stress associated with the threat of job loss may have a more proximal, earlier and/or more direct effect on mental health, which can then be translated through neuroimmunological and other pathways into worse physical health at a later time.16,20 It could be argued that experiencing uncertainty for an extended period of time (the classic emotional exhaustion or burnout that is a defining feature of job insecurity) is in some ways worse than actual job loss, which at least allows the person to face the outcome and take steps to regain control and cope with the loss.
On the other hand, in our previous studies of people with HIV, in which we have examined the health differences associated with the availability of work (the simpler comparison between employed and non-employed participants), we have found that the strength of the relationship between employment and health was greater for physical than for mental health.28,29 In those previous studies, we suggested that the relationship between employment and health might be more pronounced for physical health because of a process of adaptation to the experience of unemployment that is more salient to the mental health component of quality of life.28,29 This finding would be consistent with set-point theories suggesting that people’s mental health tends to return to baseline levels over time after reacting negatively to job loss,37 although some studies have found that unemployment can have long-term effects on well-being.38,39 It might be that factors related to the nature or quality of work—in addition to the availability of work—may have a differential effect on different health attributes.
The strengths of this study include the examination of a broad set of socio-demographic data for a relatively heterogeneous sample of people with HIV, with comprehensive adjustment for a range of potential confounders. However, our study did have some limitations. The cross-sectional nature of the data did not allow us to establish the direction of the association between job security and health. Although our conceptual framework assumed that job insecurity precedes poor health, it is also plausible that people suffering from poor health are more likely to experience job insecurity and to be more strongly affected by it. Future research using longitudinal data would provide an opportunity to examine the relative contributions of these reinforcing mechanisms. Gender differences should also be interpreted with caution, because the men and women in our study had different demographic and clinical characteristics. It is also possible that the small sample size for the women participants may have increased the probability of type 2 error (i.e., failing to detect a difference when there is one), particularly in the multivariable analyses.
Another potential limitation of this study is the use of a single-item measure of job security. It has been argued that the definition of job insecurity as the threat of job loss exclusively is too narrow,11 as there are other important factors that should be taken into account, such as threats to career opportunities or to valued job features, employment conditions (e.g., demotions), relations with co-workers and a person’s powerlessness to deal with these threats.8,11,12,15,40,41 Despite the narrow focus of a single-item measure, studies that have used multi-item measures of job insecurity have revealed stronger associations between job insecurity and various outcomes than studies using single-item measures.15 As such, our use of a single-item measure of job security may have neglected important components of the experience of working in an insecure job, but it is also plausible that our findings underestimated the health effects of job insecurity.
To our knowledge, this is the first study that has examined the association between job security and health among people with HIV. We focused on the availability of work (employment status) and only one of many aspects related to the nature or quality of work (job security). The increasing body of research on the availability and quality of work suggests that policies that focus on improving employment opportunities may offer not only income stability but also health benefits to people with HIV. These preliminary findings indicate the need for thorough discussions between health care providers and people living with HIV regarding disability, employment stability, and access to employment supports and benefits. Insecure jobs are more likely to have limited benefits, even in countries with universal health care, where access to drug coverage, dental and other health services, and disability insurance is mostly sponsored by employers. AIDS service organizations generally offer limited return-to-work programs or retention supports for those who are currently working and may be struggling to keep their jobs, but these organizations may work in partnerships with health care providers to assist people with HIV navigate the systems for medication coverage and health care benefits.
Acknowledgments
The OHTN [Ontario HIV Treatment Network] Cohort Study (OCS) Team consists of OCS site investigators and scientists. Members include Dr. Sean B. Rourke (Principal Investigator, University of Toronto and OHTN), Dr. Ann Burchell (Co-Principal Investigator, OHTN), Dr. Sandra Gardner (OHTN), Dr. Sergio Rueda (OHTN), Dr. Ahmed Bayoumi and Dr. Kevin Gough (St. Michael’s Hospital, Toronto), Dr. Jeffrey Cohen (Windsor Regional Hospital, Windsor), Dr. Curtis Cooper (The Ottawa Hospital–General Campus, Ottawa), Dr. Don Kilby (University of Ottawa Health Services, Ottawa), Dr. Mona Loutfy and Dr. Fred Crouzat (Maple Leaf Medical Clinic, Toronto), Dr. Anita Rachlis and Dr. Nicole Mittmann (Sunnybrook Health Sciences Centre, Toronto), Dr. Janet Raboud and Dr. Irving Salit (Toronto General Hospital, Toronto), Dr. Edward Ralph (St. Joseph’s Health Care, London), Dr. Roger Sandre (Health Sciences North, Sudbury), Dr. Marek Smieja (Hamilton Health Sciences, McMaster University Medical Centre, Hamilton), and Dr. Wendy Wobeser (Hotel Dieu Hospital, Kingston).
We gratefully acknowledge all of the people living with HIV who volunteered to participate in the OCS and the work and support of the past and present members of the OCS Governance Committee: Darien Taylor, Dr. Evan Collins, Dr. Greg Robinson, Shari Margolese, Patrick Cupido, Tony Di Pede, Rick Kennedy, Michael Hamilton, Ken King, Brian Finch, Lori Stoltz, Adrian Betts, Colleen Price, Tracey Conway, John MacTavish, Claire Kendall, Anita Benoit, Rosie Thein, Brian Huskins, Les Bowman, Dr. Ahmed Bayoumi, Dr. Clemon George and Dr. Curtis Cooper. We thank all the interviewers, data collectors, research associates and coordinators, nurses and physicians who provide support for data collection and extraction. The authors wish to thank the OHTN staff and their teams for data management and IT support (Mark Fisher, Director, IT) and for OCS project coordination (Samantha Robinson, OCS Project Coordinator). The OCS is supported by the Ontario Ministry of Health and Long-Term Care.
Biographies
Sergio Rueda, PhD, is Scientist and Director of Population Health Research at the Ontario HIV Treatment Network, Assistant Professor with the Department of Psychiatry, University of Toronto, and Adjunct Scientist with the Institute for Work and Health, Toronto, Ontario.
Janet Raboud, PhD, is Associate Professor at the Dalla Lana School of Public Health, University of Toronto, and Scientist with the Division of Infectious Disease, University Health Network, Toronto, Ontario.
Sean B. Rourke, PhD, is the Scientific and Executive Director of the Ontario HIV Treatment Network, Professor with the Department of Psychiatry, University of Toronto, and Scientist at the Centre for Research on Inner City Health and the Keenan Research Centre in the Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Ontario.
Tsegaye Bekele, MSA, is Research Analyst at the Ontario HIV Treatment Network.
Ahmed Bayoumi, MD, MSc, is the Director of the Clinical Epidemiology and Health Care Research Program in the Department of Health Policy, Management and Evaluation, University of Toronto, and Research Scientist with the Centre for Research on Inner City Health and the Keenan Research Centre in the Li Ka Shing Knowledge Institute, St. Michael’s Hospital.
John Lavis, PhD, is Professor with the Department of Clinical Epidemiology and Biostatistics, McMaster University, Hamilton, Ontario.
John Cairney, PhD, is Associate Professor with the Departments of Family Medicine and of Psychiatry and Behavioural Neurosciences, McMaster University.
Cameron Mustard, PhD, is President and Senior Scientist at the Institute for Work and Health and Professor at the Dalla Lana School of Public Health, University of Toronto.
Footnotes
Competing interests: None declared.
Funding source: The Ontario HIV Treatment Network Cohort Study is supported by the AIDS Bureau of the Ontario Ministry of Health and Long-Term Care.
Sergio Rueda conceived the project, oversaw the analysis, acted as the principal writer and is the guarantor for the manuscript. Janet Raboud and Cameron Mustard made substantial contributions to the conception and design of the analysis and the interpretation of the results, and revised the manuscript. Sean B. Rourke provided the data, contributed to the interpretation of the results and revised the manuscript. Tsegaye Bekele conducted the data analyses, contributed to the interpretation of the results and revised the manuscript. Ahmed Bayoumi, John Lavis and John Cairney contributed to the study design and interpretation of the results and revised the manuscript. All of the authors approved the final version of the manuscript.
References
- 1.Strully K. Job loss and health in the US labor market. Demography. 2009;46(2):221–246. doi: 10.1353/dem.0.0050. http://muse.jhu.edu/content/crossref/journals/demography/v046/46.2.strully.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kasl S V, Rodriguez E, Lasch K E. The impact of unemployment on health and well-being. In: Dohrenwend B P E, editor. Adversity, stress, and psychopathology. New York: Oxford University Press; 1998. pp. 111–131. [Google Scholar]
- 3.Sullivan D, von Wachter T. Job displacement and mortality: an analysis using administrative data. Q J Econ. 2009;124(3):1265–1306. doi: 10.1162/qjec.2009.124.3.1265. http://qje.oxfordjournals.org/lookup/doi/10.1162/qjec.2009.124.3.1265. [DOI] [Google Scholar]
- 4.Martikainen Pekka T, Valkonen Tapani. Excess mortality of unemployed men and women during a period of rapidly increasing unemployment. Lancet. 1996;348(9032):909–912. doi: 10.1016/S0140-6736(96)03291-6. http://linkinghub.elsevier.com/retrieve/pii/S0140673696032916. [DOI] [PubMed] [Google Scholar]
- 5.Jin R L, Shah C P, Svoboda T J. The impact of unemployment on health: a review of the evidence. J Public Health Policy. 1997;18(3):275–301. doi: 10.2307/3343311. http://www.jstor.org/stable/3343311?origin=crossref. [DOI] [Google Scholar]
- 6.Hill A B. The environment and disease: Association or causation? Proc R Soc Med. 1965;58(5):295–300. [PMC free article] [PubMed] [Google Scholar]
- 7.Jahoda Marie. Work, employment, and unemployment: Values, theories, and approaches in social research. Am Psychol. 1981;36(2):184–191. doi: 10.1037/0003-066X.36.2.184. http://content.apa.org/journals/amp/36/2/184. [DOI] [Google Scholar]
- 8.De Witte H. Job insecurity and psychological well-being: review of the literature and exploration of some unresolved issues. Eur J Work Organ Psychol. 1999;8(2):155–177. doi: 10.1080/135943299398302. http://www.tandfonline.com/doi/abs/10.1080/135943299398302. [DOI] [Google Scholar]
- 9.Dekker S W A, Schaufeli W B. The effects of job insecurity on psychological health and withdrawal: a longitudinal study. Aust Psychol. 1995;30(1):57–63. doi: 10.1080/00050069508259607. http://doi.wiley.com/10.1080/00050069508259607. [DOI] [Google Scholar]
- 10.Broom D H, D’Souza R M, Strazdins L, Butterworth P, Parslow R, Rodgers B. The lesser evil: bad jobs or unemployment? A survey of mid-aged Australians. Soc Sci Med. 2006;63(3):575–586. doi: 10.1016/j.socscimed.2006.02.003. http://linkinghub.elsevier.com/retrieve/pii/S0277953606000840. [DOI] [PubMed] [Google Scholar]
- 11.Hellgren J, Sverke M, Isaksson K. A two-dimensional approach to job insecurity: consequences for employee attitudes and well-being. Eur J Work Organ Psychol. 1999;8(2):179–195. doi: 10.1080/135943299398311. http://www.tandfonline.com/doi/abs/10.1080/135943299398311. [DOI] [Google Scholar]
- 12.Sverke M, Hellgren J. The nature of job insecurity: understanding employment uncertainty on the brink of a new millennium. Appl Psychol. 2002;51(1):23–42. doi: 10.1111/1464-0597.0077z. http://doi.wiley.com/10.1111/1464-0597.0077z. [DOI] [Google Scholar]
- 13.Karasek R, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. New York (NY): Basic Books; 1992. [Google Scholar]
- 14.Siegrist J. Adverse health effects of effort–reward imbalance at work: theory, empirical support, and implications for prevention. In: Cooper CL, editor. Theories of organizational stress. New York (NY): Oxford University Press; 2000. pp. 190–204. [Google Scholar]
- 15.Sverke Magnus, Hellgren Johnny, Näswall Katharina. No security: a meta-analysis and review of job insecurity and its consequences. J Occup Health Psychol. 2002;7(3):242–264. doi: 10.1037/1076-8998.7.3.242. http://www.scholaruniverse.com/ncbi-linkout?id=12148956. [DOI] [PubMed] [Google Scholar]
- 16.Ferrie J E, Shipley M J, Stansfeld S A, Marmot M G. Effects of chronic job insecurity and change in job security on self reported health, minor psychiatric morbidity, physiological measures, and health related behaviours in British civil servants: the Whitehall II study. J Epidemiol Community Health. 2002;56(6):450–454. doi: 10.1136/jech.56.6.450. http://pubmedcentralcanada.ca/pmcc/articles/pmid/12011203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burgard Sarah A, Brand Jennie E, House James S. Perceived job insecurity and worker health in the United States. Soc Sci Med. 2009;69(5):777–785. doi: 10.1016/j.socscimed.2009.06.029. http://linkinghub.elsevier.com/retrieve/pii/S0277953609003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rugulies R, Aust B, Burr H, Bultmann U. Job insecurity, chances on the labour market and decline in self-rated health in a representative sample of the Danish workforce. J Epidemiol Community Health. 2008 Mar 1;62(3):245–250. doi: 10.1136/jech.2006.059113. http://jech.bmj.com/cgi/doi/10.1136/jech.2006.059113. [DOI] [PubMed] [Google Scholar]
- 19.D'Souza Rennie M, Strazdins Lyndall, Clements Mark S, Broom Dorothy H, Parslow Ruth, Rodgers Bryan. The health effects of jobs: status, working conditions, or both? Aust N Z J Public Health. 2005;29(3):222–228. doi: 10.1111/j.1467-842X.2005.tb00759.x. http://doi.wiley.com/10.1111/j.1467-842X.2005.tb00759.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee Sunmin, Colditz Graham A, Berkman Lisa F, Kawachi Ichiro. Prospective study of job insecurity and coronary heart disease in US women. Ann Epidemiol. 2004;14(1):24–30. doi: 10.1016/S1047-2797(03)00074-7. http://www.scholaruniverse.com/ncbi-linkout?id=14664776. [DOI] [PubMed] [Google Scholar]
- 21.Ferrie Jane E, Shipley Martin J, Newman Katherine, Stansfeld Stephen A, Marmot Michael. Self-reported job insecurity and health in the Whitehall II study: potential explanations of the relationship. Soc Sci Med. 2005;60(7):1593–1602. doi: 10.1016/j.socscimed.2004.08.006. http://linkinghub.elsevier.com/retrieve/pii/S0277953604003892. [DOI] [PubMed] [Google Scholar]
- 22.Virtanen P, Vahtera J, Kivimäki M, Pentti J, Ferrie J. Employment security and health. J Epidemiol Community Health. 2002;56(8):569–574. doi: 10.1136/jech.56.8.569. http://pubmedcentralcanada.ca/pmcc/articles/pmid/12118045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rugulies Reiner, Bültmann Ute, Aust Birgit, Burr Hermann. Psychosocial work environment and incidence of severe depressive symptoms: prospective findings from a 5-year follow-up of the Danish work environment cohort study. Am J Epidemiol. 2006 Mar 29;163(10):877–887. doi: 10.1093/aje/kwj119. http://aje.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16571741. [DOI] [PubMed] [Google Scholar]
- 24.Cheng Y, Chen C W, Chen C J, Chiang T L. Job insecurity and its association with health among employees in the Taiwanese general population. Soc Sci Med. 2005;61(1):41–52. doi: 10.1016/j.socscimed.2004.11.039. http://linkinghub.elsevier.com/retrieve/pii/S0277953604005970. [DOI] [PubMed] [Google Scholar]
- 25.Dray-Spira Rosemary, Gueguen Alice, Ravaud Jean-François, Lert France. Socioeconomic differences in the impact of HIV infection on workforce participation in France in the era of highly active antiretroviral therapy. Am J Public Health. 2007;97(3):552–558. doi: 10.2105/AJPH.2005.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burgoyne R W, Saunders D S. Quality of life among urban Canadian HIV/AIDS clinic outpatients. Int J STD AIDS. 2001 Aug 1;12(8):505–512. doi: 10.1258/0956462011923598. http://ijsa.rsmjournals.com/cgi/doi/10.1258/0956462011923598. [DOI] [PubMed] [Google Scholar]
- 27.Rueda Sergio, Chambers Lori, Wilson Mike, Mustard Cameron, Rourke Sean B, Bayoumi Ahmed, Raboud Janet, Lavis John. Association of returning to work with better health in working-aged adults: a systematic review. Am J Public Health. 2012;102(3):541–556. doi: 10.2105/AJPH.2011.300401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rueda Sergio, Raboud Janet, Mustard Cameron, Bayoumi Ahmed, Lavis John N, Rourke Sean B. Employment status is associated with both physical and mental health quality of life in people living with HIV. AIDS Care. 2011;23(4):435–443. doi: 10.1080/09540121.2010.507952. http://www.tandfonline.com/doi/abs/10.1080/09540121.2010.507952. [DOI] [PubMed] [Google Scholar]
- 29.Rueda Sergio, Raboud Janet, Plankey Michael, Ostrow David, Mustard Cameron, Rourke Sean B, Jacobson Lisa P, Bekele Tsegaye, Bayoumi Ahmed, Lavis John, Detels Roger, Silvestre Anthony J. Labor Force Participation and Health-Related Quality of Life in HIV-Positive Men Who Have Sex with Men: The Multicenter AIDS Cohort Study. AIDS Behav. 2012 doi: 10.1007/s10461-012-0257-3. http://www.springerlink.com/index/10.1007/s10461-012-0257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rourke Sean B, Gardner Sandra, Burchell Ann N, Raboud Janet, Rueda Sergio, Bayoumi Ahmed M, Loutfy Mona, Cooper Curtis, Smieja Marek, Taylor Darien, Dipede Tony, Wobeser Wendy, Major Carol, Waring Virginia, Fisher Mark, Cairney John, Mittmann Nicole, Salit Irving E, Crouzat Fred, Gough Kevin, Ralph Edward, Sandre Roger, Kilby Don, Rachlis Anita. Cohort Profile: The Ontario HIV Treatment Network Cohort Study (OCS) Int J Epidemiol. 2012 Feb 16; doi: 10.1093/ije/dyr230. [DOI] [PubMed] [Google Scholar]
- 31.The OHTN Cohort Study. Toronto (ON): Ontario HIV Treatment Network; 2011. http://www.ohtncohortstudy.ca. [updated 2012; cited 2012 May 12] [Google Scholar]
- 32.Saunders J B, Aasland O G, Babor T F, de la Fuente J R, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. http://ClinicalTrials.gov/search/term=8329970%20%5BPUBMED-IDS%5D. [DOI] [PubMed] [Google Scholar]
- 33.Ware J E, Jr, Kosinski M, Turner-Bowker D M, Gandeck B. User’s manual for the SF-12v2 health survey (with a supplement documenting SF-12 Health Survey) Lincoln (RI): QualityMetric Incorporated; 2007. [Google Scholar]
- 34.Ware J E, Jr, Kosinski M, Bjoner J, Turner-Bowker D, Gandeck B, Maruish M. User’s manual for the SF-36v2 health survey. 2nd ed. Lincoln (RI): QualityMetric Incorporated; 2007. [Google Scholar]
- 35.Worthington C, Krentz H B. Socio-economic factors and health-related quality of life in adults living with HIV. Int J STD AIDS. 2005;16(9):608–614. doi: 10.1258/0956462054944408. http://www.scholaruniverse.com/ncbi-linkout?id=16176627. [DOI] [PubMed] [Google Scholar]
- 36.Kivimäki Mika, Vahtera Jussi, Virtanen Marianna, Elovainio Marko, Pentti Jaana, Ferrie Jane E. Temporary employment and risk of overall and cause-specific mortality. Am J Epidemiol. 2003 Oct 1;158(7):663–668. doi: 10.1093/aje/kwg185. http://www.scholaruniverse.com/ncbi-linkout?id=14507602. [DOI] [PubMed] [Google Scholar]
- 37.Warr P, Jackson P. Adapting to the unemployed role: a longitudinal investigation. Soc Sci Med. 1987;25(11):1219–1224. doi: 10.1016/0277-9536(87)90369-8. http://linkinghub.elsevier.com/retrieve/pii/0277953687903698. [DOI] [PubMed] [Google Scholar]
- 38.Lucas Richard E, Clark Andrew E, Georgellis Yannis, Diener Ed. Unemployment alters the set point for life satisfaction. Psychol Sci. 2004;15(1):8–13. doi: 10.1111/j.0963-7214.2004.01501002.x. http://www.scholaruniverse.com/ncbi-linkout?id=14717825. [DOI] [PubMed] [Google Scholar]
- 39.Morrell S, Taylor R, Quine S, Kerr C, Western J. A cohort study of unemployment as a cause of psychological disturbance in Australian youth. Soc Sci Med. 1994;38(11):1553–1564. doi: 10.1016/0277-9536(94)90117-1. http://linkinghub.elsevier.com/retrieve/pii/0277953694901171. [DOI] [PubMed] [Google Scholar]
- 40.Blau Gary, Tatum Donna S, McCoy Keith, Dobria Lidia, Ward-Cook Kory. Job loss, human capital job feature, and work condition job feature as distinct job insecurity constructs. J Allied Health. 2004;33(1):31–41. http://www.scholaruniverse.com/ncbi-linkout?id=15053218. [PubMed] [Google Scholar]
- 41.Reisel William D, Banai Moshe. Comparison of a multidimensional and a global measure of job insecurity: predicting job attitudes and work behaviors. Psychol Rep. 2002;90(3 Pt 1):913–922. doi: 10.2466/pr0.2002.90.3.913. http://www.scholaruniverse.com/ncbi-linkout?id=12090528. [DOI] [PubMed] [Google Scholar]