Abstract
Background
Among people living with HIV infection in the era of combination antiretroviral therapy (cART), admission to hospital may indicate inadequate community-based care. As such, population-based assessments of the utilization of inpatient services represent a necessary component of evaluating the quality of HIV-related care.
Methods
We used a validated algorithm to search Ontario’s administrative health care databases for all persons living with HIV infection aged 18 years or older between 1992/93 and 2008/09. We then conducted a population-based study using time-series and longitudinal analyses to first quantify the immediate effect of cART on hospital admission rates and then analyze recent trends (for 2002/03 to 2008/09) in rates of total and HIV-related admissions.
Results
The introduction of cART in 1996/97 was associated with more pronounced reductions in the rate of hospital admissions among men than among women (for total admissions, –89.9 v. –60.5 per 1000 persons living with HIV infection, p = 0.003; for HIV-related admissions, –56.9 v. –36.3 per 1000 persons living with HIV infection, p < 0.001). Between 2002/03 and 2008/09, higher rates of total hospital admissions were associated with female sex (adjusted relative rate [RR] 1.15, 95% confidence interval [CI] 1.05–1.27) and low socio-economic status (adjusted RR 1.21, 95% CI 1.14–1.29). Higher rates of HIV-related hospital admission were associated with low socio-economic status (adjusted RR 1.30, 95% CI 1.17–1.45). Recent immigrants had lower rates of both total admissions (adjusted RR 0.70, 95% CI 0.61–0.80) and HIV-related admissions (adjusted RR 0.77, 95% CI 0.61–0.96).
Interpretation
We observed important socio-economic- and sex-related disparities in rates of hospital admission among people with HIV living in Ontario, Canada.
Patterns of health services utilization among patients infected with HIV have been demonstrably altered by the introduction and widespread adoption of combination antiretroviral therapy (cART) during the latter half of the 1990s.1-6 Most notably, large declines in rates of hospital admission for HIV-associated opportunistic infections were observed in the years immediately following adoption of cART as the standard of care for HIV infection. However, more recent studies examining the utilization of inpatient services by people living with HIV have described stabilizing or increasing rates of hospital admission, particularly among patients for whom the effects of HIV infection intersect with socially and structurally mediated barriers to care, such as women and people from ethnic minority groups.7-11 These data are especially salient for the evaluation of trends in hospital admission among people living with HIV who reside in Ontario, where important changes in the demographic composition of this population have been observed over the past decade. Specifically, the proportion of diagnosed cases of HIV infection represented by women has increased substantially, from less than 3% in the early years of the epidemic to 25% in 2008.12 Similarly, the prevalence of HIV among persons immigrating to Ontario from HIV-endemic countries increased 62% from 2003 to 2008.12 In this context of pronounced change in both the treatment and demography of HIV infection, accurate population-based estimates of health services utilization are required by clinicians, researchers and policy-makers involved in the provision, evaluation and funding of HIV-related care. However, these data are currently lacking for Ontario, home to over 40% of Canada’s population of people living with HIV and destination for about half of all immigrants to Canada on an annual basis.13
Admission to hospital for HIV-related illness in the era of cART may be an indicator of inadequate community-based care. As such, ongoing assessment of trends in inpatient service utilization is a necessary component of the evaluation of quality of care for people living with HIV. We therefore conducted a population-based study of temporal trends in hospital admission rates among people with HIV in the province of Ontario. We hypothesized that, because of socially and structurally rooted challenges in accessing care among marginalized people living with HIV, rates of hospital admission in the modern era of cART (2002/03 to 2008/09) would be disproportionately higher among women, recent immigrants and people with HIV living in low-income neighbourhoods.
Methods
Study design
We used a validated case-finding algorithm derived from administrative data to identify all people with HIV infection aged 18 years and older who were receiving care in Ontario between 1992 Apr. 1 and 2009 Mar. 31. The development and test characteristics of the algorithm have been described in detail elsewhere.14 Briefly, the algorithm, based on identification, within a 3-year period, of at least 3 physician claims with an International Classification of Diseases, Ninth Revision (ICD-9) code for HIV infection (i.e., 042, 043 or 044), had a sensitivity of 96.2% (95% confidence interval [CI] 95.2%–97.9%) and specificity of 99.6% (95% CI 99.1%–99.8%). When assembling our cohort, we chose 2009 Mar. 31 (the end of the 2008/09 fiscal year) for our analyses to meet the 3-year “look forward” criterion of the algorithm. We then conducted a retrospective, population-based study to examine temporal trends in rates of hospital admission within the cohort. Specifically, we used interrupted time-series analysis to isolate and quantify the effect of the introduction of cART on hospital admission rates among people living with HIV in Ontario and methods of longitudinal data analysis to examine trends and predictors of hospital admission during the modern era of cART, defined as the period spanning 2002 Apr. 1 to 2009 Mar. 31. We selected this period for the longitudinal analyses because it corresponds to important changes in the demographic composition of the population of people living with HIV in Ontario and to the availability of antiretrovirals with enhanced potency and ease of administration relative to earlier formulations of these drugs.12,15
Data sources and outcomes
We used the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD) to determine the annual number of hospital admissions for each individual in our population-based cohort of people with HIV. The CIHI-DAD contains information from all acute care hospital separations (i.e., discharge, sign-out, transfer to a different facility) in Ontario, abstracted by trained health information professionals using standard diagnosis and procedure codes, including dates of admission to and discharge from the hospital, the diagnosis representing the condition accountable for the greatest portion of the length of stay or greatest use of resources during the hospital stay (i.e., most responsible diagnosis), and secondary diagnoses or complications contributing to the admission. We calculated annual crude rates of total and HIV-related hospital admissions per 1000 population of people with HIV aged 18 and over. HIV-related hospital admissions were defined as those admissions in which the most responsible diagnosis was coded as being attributable to HIV infection or an associated opportunistic infection according to the relevant ICD-9 and ICD-10 (10th revision) codes. We excluded obstetric admissions and admissions for elective surgery from our calculation of hospital admission rates.
We used Ontario’s Registered Persons Database, a registry of all residents eligible for coverage under the Ontario Health Insurance Plan (OHIP), to identify individual demographic information such as age, sex, date of OHIP eligibility and postal code. We determined patients’ socio-economic status at the neighbourhood level for each year of follow-up using postal code information and Statistics Canada census data. We defined a recent immigrant as any adult for whom an OHIP card was first issued within 3 years of becoming a member of our cohort. The date of issuance of an OHIP card has been used in other studies as a proxy for the date of arrival in Ontario.16
Statistical analyses
To examine the effect of cART on hospital admission rates during the period spanning 1992/93 to 2008/09, we conducted an interrupted time-series analysis using autoregressive integrated moving-average models with an indicator variable for the fiscal year 1996/97, corresponding to the first full year that cART was widely available in Ontario.17,18 We performed subgroup analyses to determine if the effect of cART on total and HIV-related hospital admission rates varied according to sex and socio-economic status and used the Ljung-Box χ2 statistic to examine autocorrelation of the model residuals.19
For the longitudinal analyses, we evaluated temporal trends in the rates of hospital admission during the years 2002/03 to 2008/09 using multivariable generalized estimating equation (GEE) models with a log link function and autoregressive correlation structure.20 Because the GEE method is not a likelihood-based method, we used the quasi-likelihood under the independence model criterion both to ascertain the appropriateness of the autoregressive correlation structure relative to other working correlation matrices and to assess the fit of our regression models.21 We also evaluated the data for overdispersion by comparing the Poisson and negative binomial distributions.
We conducted separate analyses for total hospital admission rates and rates of HIV-related hospital admission. All multivariable analyses included fiscal year as the main predictor, along with variables for sex, income quintile group (2 lowest quintiles v. 2 highest quintiles) and immigration status, because of our a priori hypotheses that differences in access to care may have contributed to differences in rates of admission according to these factors. We estimated adjusted relative rates (RRs) from the model using fiscal year as both a continuous variable and a categorical variable. In the former case, trends are reported as percentages per year, whereas in the latter case, adjusted RRs were used to compare annual changes in the rate of hospital admission relative to the reference fiscal year of 2002/03. We considered additional variables as confounders if there was a plausible association with our outcomes of interest and if the variables changed the estimate for fiscal year by at least 10%.22 Variables meeting these criteria were patient age, annual number of physician visits, geographic residence (urban v. rural), years in the cohort and level of comorbidity. We used the Johns Hopkins Adjusted Clinical Groups case-mix assignment software (Sun Microsystems Inc., Santa Clara, Calif.) to determine the level of comorbidity for each patient, on the basis of diagnostic codes listed in hospital admission records and physicians’ services claims from each year during the study period. This methodology is described in detail elsewhere.23 We assessed the potential for collinearity between covariates using a threshold tolerance of > 0.4 and a variance inflation of < 2.5. We also examined interactions of sex, socio-economic status and immigration status with year in separate models. We included interaction terms in the final model if they were statistically significant and if their inclusion improved the goodness of fit of the model by at least 10%.
All statistical analyses were conducted using SAS statistical software, version 9.2 (SAS Institute Inc., Cary, N.C.).
Ethics approval
We obtained ethics approval for this study from the Research Ethics Board of Sunnybrook Health Sciences Centre and the HIV Research Ethics Board of the University of Toronto.
Results
Effect of cART on hospital admissions
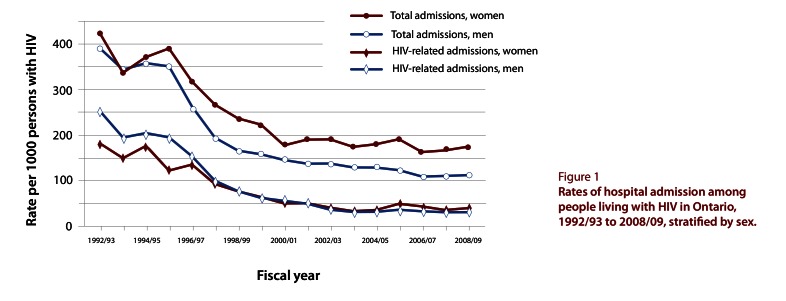
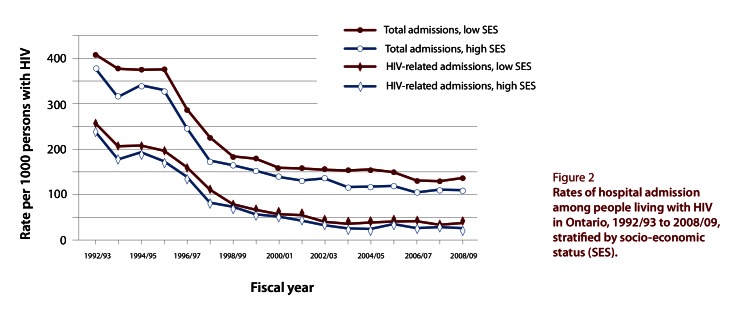
Over the 17-year study period, crude annual rates of total hospital admissions decreased from 392.4 to 123.9 per 1000 persons with HIV, and crude annual rates of HIV-related hospital admissions declined from 247.6 to 32.2 per 1000 persons with HIV. As expected, rates of both total hospital admissions (–86.1 per 1000 persons with HIV, 95% CI –77.1 to –95.; p < 0.001) and HIV-related hospital admissions (–54.1 per 1000 persons with HIV, 95% CI –48.4 to –59.8; p < 0.001) declined immediately following the introduction of cART in 1996/97. In subgroup analyses, significant reductions in hospital admission rates were associated with the introduction of cART for both men and women, as well as those living in both high- and low-income neighbourhoods. However, the effect of cART was more pronounced among men than among women for both total hospital admissions (–89.9 v. –60.5 per 1000 persons with HIV, p = 0.003) and HIV-related hospital admissions (–56.9 v. –36.3 per 1000 persons with HIV, p < 0.001) (Figure 1). In contrast, no differences were observed between patients with low and high socio-economic status in terms of the immediate effects of cART on total admissions (–91.3 v. –83.5 per 1000 persons with HIV, p = 0.36) or HIV-related admissions (–57.4 v. –53.7 per 1000 persons with HIV, p = 0.25) (Figure 2).
Figure 1.
Rates of hospital admission among people living with HIV in Ontario, 1992/93 to 2008/09, stratified by sex.
Figure 2.
Rates of hospital admission among people living with HIV in Ontario, 1992/93 to 2008/09, stratified by socio-economic status (SES)
Multivariable analysis of trends in hospital admissions
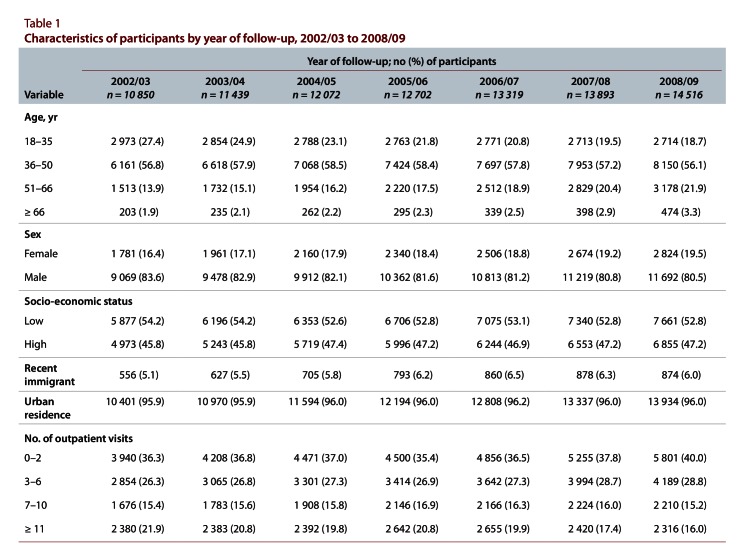
For each year in the modern era of cART, most patients were male, lived in Ontario’s large urban centres and were between the ages of 36 and 50 years (Table 1). The proportion of people living with HIV who were women increased from 16.4% in 2002/03 to 19.5% in 2008/09. Similarly, the number of individuals aged 51 years and older increased longitudinally, accounting for 15.8% of people with HIV in 2002/03 and 25.2% in 2008/09.
Table 1.
Characteristics of participants by year of follow-up, 2002/03 to 2008/09
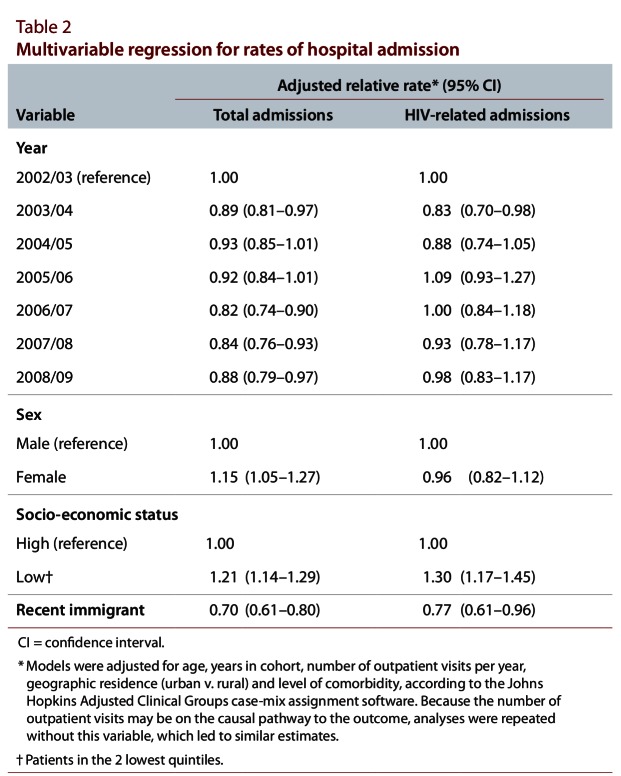
Adjusted rates of total hospital admissions among Ontario residents with HIV decreased by 2.3% (95% CI 0.8%–3.8%) per annum between the years 2002/03 and 2008/09. Over the 7-year study period, adjusted rates of total hospital admissions were higher among women relative to men (adjusted RR 1.15, 95% CI 1.05–1.27) and among people living in low- versus high-income neighbourhoods (adjusted RR 1.21, 95% CI 1.14–1.29). In contrast, recent immigration was associated with lower rates of total hospital admissions (adjusted RR 0.70, 95% CI 0.61–0.80) (Table 2).
Table 2.
Multivariate regression for rates of hospital admission
Adjusted rates of HIV-related hospital admissions remained relatively stable among Ontario residents with HIV between 2002/03 and 2008/09, increasing by 0.9% (95% CI –1.6% to 3.4%) per annum. In contrast to total hospital admissions, no association with sex was evident for this outcome. However, significant associations were observed with both low socio-economic status and recent immigration (Table 2).
Interpretation
In this population-based study, we observed a striking reduction in the rates of total and HIV-related hospital admissions associated with availability of cART between the years 1992/93 and 2008/09. Although these benefits were observed for all subgroups examined, the effect of cART was attenuated among women relative to men. In the modern era of cART, sustained reductions in the rates of total hospital admissions among people with HIV were observed, whereas the rates of HIV-related hospital admissions remained relatively unchanged during the 7-year follow-up period. However, because the numbers of HIV-related hospital admissions were relatively low, we cannot discount the possibility of a type II error when analyzing temporal trends in this outcome. We also identified several disparities in the risk of hospital admission among Ontario residents with HIV following multivariable adjustment for socio-demographic variables, level of comorbidity and annual number of outpatient physician visits. Specifically, female sex and low socio-economic status were significantly associated with higher rates of total hospital admissions, with the latter variable also being associated with a heightened risk of HIV-related hospital admission. In contrast to our initial hypothesis, recent immigrants were less likely to be admitted to hospital in the modern era of cART relative to the reference population of people with HIV in Ontario.
Our findings of decreasing rates of hospital admission among people with HIV in the modern era of cART are similar to those of previous studies analyzing these trends in other regions.11 In addition, our work corroborates previous investigations highlighting inequity in hospital admission rates among certain groups, most notably, women relative to men.9,11 However, unlike the settings of other analyses, our study was conducted within a context of universal coverage for all medically necessary physician, laboratory and inpatient services. Consequently, differences in rates of hospital admission according to sex, socio-economic status or immigration status should not be confounded by health insurance status, which thus implies a role for other biological, social or structural factors in these disparities, including stigma, non-disclosure of HIV status, drug addiction and coexisting mental health disease.24-30
Although the underlying basis of observed differences cannot be readily discerned from our administrative databases, several explanations are possible. With respect to women living with HIV, a comprehensive body of literature has described various barriers impeding access to regular HIV-related care, including lack of transportation, depression, and history of physical or sexual abuse.31-33 In addition, compared with men, women living with HIV are more likely to delay initiating cART and less likely to begin treatment.34,35 Several reasons have been postulated to account for these sex-based discrepancies in treatment uptake, including concern about disclosure of HIV status to children, socio-economic circumstances and family commitments, which often include assuming the role of primary caregiver to other family members living with HIV.35-37 Furthermore, several toxic effects of antiretroviral drugs are noted to occur at greater frequency among women relative to men, including severe hypersensitivity reactions and lipodystrophy.38-40 As a result, women may be more likely than men to discontinue cART. Although individuals living in low-income neighbourhoods undoubtedly share some of the obstacles to care faced by women, other structurally mediated inequities are important determinants of health among these patients. Specifically, instability with respect to housing status and food security have both been documented to undermine adherence with antiretroviral therapy and to contribute to poor outcomes among people with HIV.41-44 Furthermore, despite the availability of various programs intended to mitigate the expense of cART for Ontario residents with HIV who lack alternative sources of drug coverage, individuals who do not qualify for provincially funded social assistance must assume a share of the cost of their treatment, in the form of a copayment, which may be prohibitive when evaluated against competing demands for food and housing. Finally, reduced rates of hospital admission among recent immigrants may be attributable to a “healthy immigrant” effect, whereby these patients adopt specific behaviours and practices that translate into better clinical outcomes relative to the reference population of people with HIV in Ontario.45 For example, in a single-centre retrospective cohort study, recent immigrants with HIV were more likely to remain in care within 3 years of their first clinic visit than either Canadian-born people with HIV or patients who had immigrated to Canada more than 10 years before their index clinic visit.46 This finding may have accounted for the significantly lower risk of death among recent immigrants with HIV relative to the 2 referent groups.46 Further research is required to delineate the processes through which recent immigrants with HIV may attain better outcomes than other groups of people with HIV. Such research will be helpful in enacting policies and programs that support the healthier practices of recent immigrants living with HIV and that can be applied toward improving the health of other Canadians with HIV.
Several strengths and limitations of our work merit emphasis. First, our study was population-based and therefore representative of all HIV-infected patients receiving care in the province of Ontario over the 17-year study period. In addition, because we used administrative data, we were able to evaluate temporal trends and disparities in hospital admission rates among people with HIV while considering variation in place of residence, utilization of outpatient health care and extent of comorbidity, important covariates that have not traditionally been considered in the study of this phenomenon. Nonetheless, the administrative databases that we used were limited by their lack of clinical information, which prevented us from examining the role of variables such as stage of illness and adherence to cART in accounting for the observed disparities. However, this limitation is common among studies using administrative data for the conduct of health services research.47 Furthermore, because the administrative databases lacked individual-level measures of income, we used neighbourhood income as a proxy for patients’ socio-economic status. However, this approach has been previously validated as a measure of household income and social deprivation.48 In addition, residential neighbourhood may exert effects on health and outcomes independent of those ascribed to individual income.49 Finally, the potential for misclassification is always a consideration when using administrative data for health services research. To address this concern, we used a validated algorithm with excellent test characteristics for discriminating between HIV-infected and non-infected individuals to assemble our cohort of people with HIV.14 Although use of the date of OHIP enrolment as a surrogate for recency of immigration has not been validated and may be biased by interprovincial migration of Canadian citizens, any misclassification of immigration status would likely have attenuated our findings. To our knowledge, this is the first population-based study using a validated case-finding algorithm to examine trends in hospital admission among people with HIV.
In summary, we observed significant disparities in the rates of hospital admission for certain groups of people with HIV living in Ontario. Our findings have important implications for researchers, clinicians and policy-makers involved in the provision of HIV-related care. Because receipt of cART is associated with a reduced risk of hospital admission for HIV-attributable illness, the occurrence of such admissions may represent inadequate access to outpatient medical care or challenges in initiating or maintaining long-term antiretroviral therapy.1-6 In addition, persistent differences in rates of total hospital admission for specific groups of people with HIV imply that gaps may exist in the current complement of community-based health and social services, which may render the most marginalized HIV-infected patients vulnerable to poor health outcomes. Continued collaborations among the community of people living with HIV, researchers, clinicians and policy-makers will be essential to generate the qualitative and quantitative data required to elicit and address the social and structural factors modifying access to care among people living with HIV. Addressing these factors may ultimately lead to greater parity in the quality of care received by all HIV-infected individuals.
Acknowledgments
We thank Dr. Rahim Moineddin for his advice regarding the statistical analysis.
Biographies
Tony Antoniou, BScPhm, PharmD, PhD, is a Clinical Pharmacy Specialist and Research Scholar in the Department of Family and Community Medicine at St. Michael’s Hospital and an Assistant Professor in the Leslie Dan Faculty of Pharmacy, University of Toronto, Toronto, Ontario.
Brandon Zagorski, MSc, is an Analyst with the Institute for Clinical Evaluative Sciences and an Adjunct Professor in the Faculty of Medicine, University of Toronto, Toronto, Ontario.
Mona R. Loutfy, MD, MPH, is an Associate Professor in the Department of Medicine, University of Toronto, and a Scientist at the Women’s College Hospital Research Institute, Toronto, Ontario.
Carol Strike, PhD, is an Associate Professor in the Dalla Lana School of Public Health at the University of Toronto, Toronto, Ontario.
Richard H. Glazier, MD, MPH, is a Senior Scientist at the Institute for Clinical Evaluative Sciences; a Scientist with the Centre for Research on Inner City Health and a Research Scholar in the Department of Family and Community Medicine, St. Michael’s Hospital; and Professor in the Department of Family and Community Medicine, University of Toronto, Toronto, Ontario.
Footnotes
Competing interests: During the past 3 years, Tony Antoniou has received unrestricted research grants from Merck and Pfizer for various studies, and Mona Loutfy has received unrestricted research grants from, and has acted as a speaker and advisor for, Abbott Laboratories, Merck Frosst Canada Ltd., Pfizer and ViiV Healthcare. None declared for all other authors.
Funding source: This project was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The sponsors had no role in the design or conduct of the study; in the collection, analysis or interpretation of the data; or in the preparation, review or approval of the manuscript. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding source. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
At the time of this study, Tony Antoniou was supported by a fellowship from the Primary Health Care System Program. He is currently supported by a postdoctoral fellowship from the Ontario HIV Treatment Network. Mona Loutfy receives salary support from the Canadian Institutes of Health Research.
Contributors: All authors contributed to the concept and design of the study. Tony Antoniou and Brandon Zagorski acquired the data, and all authors were involved in the analysis and interpretation of the data. Tony Antoniou drafted the manuscript, and all authors were involved in critical revision of the manuscript. All authors approved the manuscript submitted for publication. Tony Antoniou and Brandon Zagorski provided administrative, technical or material support. Tony Antoniou, Mona Loutfy, Carol Strike and Richard Glazier supervised the study, and Tony Antoniou is the guarantor for the manuscript.
References
- 1.Mocroft A, d'Arminio Monforte A, Kirk O, Johnson M A, Friis-Moller N, Banhegyi D, Blaxhult A, Mulcahy F, Gatell J M, Lundgren J D, Group EuroSIDA Study. Changes in hospital admissions across Europe: 1995–2003. Results from the EuroSIDA study. HIV Med. 2004;5(6):437–447. doi: 10.1111/j.1468-1293.2004.00250.x. http://doi.wiley.com/10.1111/j.1468-1293.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- 2.Buchacz Kate, Baker Rose K, Moorman Anne C, Richardson James T, Wood Kathleen C, Holmberg Scott D, Brooks John T HIV Outpatient Study (HOPS) Investigators. Rates of hospitalizations and associated diagnoses in a large multisite cohort of HIV patients in the United States, 1994–2005. AIDS. 2008;22(11):1345–1354. doi: 10.1097/QAD.0b013e328304b38b. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002030-200807110-00012. [DOI] [PubMed] [Google Scholar]
- 3.Fleishman J A, Hellinger F J. Trends in HIV-related inpatient admissions from 1993 to 1997: a seven-state study. J Acquir Immune Defic Syndr. 2001 Sep 1;28(1):73–80. doi: 10.1097/00042560-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Krentz H B, Dean S, Gill M J. Longitudinal assessment (1995–2003) of hospitalizations of HIV-infected patients within a geographical population in Canada. HIV Med. 2006;7(7):457–466. doi: 10.1111/j.1468-1293.2006.00408.x. http://www.scholaruniverse.com/ncbi-linkout?id=16925732. [DOI] [PubMed] [Google Scholar]
- 5.Altés Jordi, Guadarrama Manuel, Force Lluís, Tapiz Alfons, Vilaró Josep, García Isabel. The impact of highly active antiretroviral therapy on HIV-related hospitalizations in 17 county hospitals in Catalonia, Spain. Catalonian County Hospitals HIV Infection Study Group. AIDS. 1999;13(11):1418–1419. doi: 10.1097/00002030-199907300-00025. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002030-199907300-00025. [DOI] [PubMed] [Google Scholar]
- 6.Gebo K A, Diener-West M, Moore R D. Hospitalization rates in an urban cohort after the introduction of highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2001 Jun 1;27(2):143–152. doi: 10.1097/00126334-200106010-00009. http://www.scholaruniverse.com/ncbi-linkout?id=11404536. [DOI] [PubMed] [Google Scholar]
- 7.Dávalos Diana M, Hlaing WayWay M, Kim Sunny, de la Rosa Mario. Recent trends in hospital utilization and mortality for HIV infection: 2000-2005. J Natl Med Assoc. 2010;102(12):1131–1138. doi: 10.1016/s0027-9684(15)30767-7. [DOI] [PubMed] [Google Scholar]
- 8.Fleishman John A, Gebo Kelly A, Reilly Erin D, Conviser Richard, Christopher Mathews W, Todd Korthuis P, Hellinger James, Rutstein Richard, Keiser Philip, Rubin Haya, Moore Richard D. Hospital and outpatient health services utilization among HIV-infected adults in care 2000–2002. Med Care. 2005;43(9 Suppl) doi: 10.1097/01.mlr.0000175621.65005.c6. http://www.scholaruniverse.com/ncbi-linkout?id=16116308. [DOI] [PubMed] [Google Scholar]
- 9.Crum-Cianflone Nancy F, Grandits Greg, Echols Sara, Ganesan Anuradha, Landrum Michael, Weintrob Amy, Barthel Robert, Agan Brian. Infectious Disease Clinical Research Program. Trends and causes of hospitalizations among HIV-infected persons during the late HAART era: What is the impact of CD4 counts and HAART use? J Acquir Immune Defic Syndr. 2010;54(3):248–257. doi: 10.1097/QAI.0b013e3181c8ef22. http://pubmedcentralcanada.ca/pmcc/articles/pmid/20658748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falster Kathleen, Wand Handan, Donovan Basil, Anderson Jonathan, Nolan David, Watson Kerrie, Watson Jo, Law Matthew G. Australian HIV Observational Database. Hospitalizations in a cohort of HIV patients in Australia, 1999–2007. AIDS. 2010;24(9):1329–1339. doi: 10.1097/QAD.0b013e328339e245. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002030-201006010-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yehia Baligh R, Fleishman John A, Hicks Perrin L, Ridore Michelande, Moore Richard D, Gebo Kelly A. HIV Research Network. Inpatient health services utilization among HIV-infected adult patients in care 2002–2007. J Acquir Immune Defic Syndr. 2010;53(3):397–404. doi: 10.1097/QAI.0b013e3181bcdc16. http://pubmedcentralcanada.ca/pmcc/articles/pmid/19841589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Remis R S, Swantee C, Liu J. Report on HIV/AIDS in Ontario 2008. Toronto (ON): Ontario Ministry of Health and Long-Term Care; 2010. [accessed 2012 Jan. 23]. http://www.ohemu.utoronto.ca/doc/PHERO2008_report_final.pdf. [Google Scholar]
- 13.HIV and AIDS in Canada. Surveillance report to December 31, 2008. Ottawa (ON): Minister of Health, Public Health Agency of Canada; 2009. [accessed 2012 Jan. 23]. http://www.phac-aspc.gc.ca/aids-sida/publication/survreport/2008/dec/index-eng.php. [Google Scholar]
- 14.Antoniou Tony, Zagorski Brandon, Loutfy Mona R, Strike Carol, Glazier Richard H. Validation of case-finding algorithms derived from administrative data for identifying adults living with human immunodeficiency virus infection. PLoS One. 2011 Jun 30;6(6):21748. doi: 10.1371/journal.pone.0021748. http://pubmedcentralcanada.ca/pmcc/articles/pmid/21738786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bangsberg David R, Ragland Kathleen, Monk Alex, Deeks Steven G. A single tablet regimen is associated with higher adherence and viral suppression than multiple tablet regimens in HIV+ homeless and marginally housed people. AIDS. 2010;24(18):2835–2840. doi: 10.1097/QAD.0b013e328340a209. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002030-201011270-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ray Joel G, Vermeulen Marian J, Schull Michael J, Singh Gita, Shah Rajiv, Redelmeier Donald A. Results of the Recent Immigrant Pregnancy and Perinatal Long-term Evaluation Study (RIPPLES) CMAJ. 2007 May 8;176(10):1419–1426. doi: 10.1503/cmaj.061680. http://pubmedcentralcanada.ca/pmcc/articles/pmid/17485694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Helfenstein Ulrich. The use of transfer function models, intervention analysis and related time series methods in epidemiology. Int J Epidemiol. 1991;20(3):808–815. doi: 10.1093/ije/20.3.808. http://ije.oxfordjournals.org/cgi/doi/10.1093/ije/20.3.808. [DOI] [PubMed] [Google Scholar]
- 18.Yaffee R. Introduction to time series analysis and forecasting with applications of SAS and SPSS. San Diego (CA): Acadmic Press; 2000. [Google Scholar]
- 19.Ljung G M, Box G E P. On a measure of lack of fit in time series models. Biometrika. 1978 Aug 1;65(2):297–303. doi: 10.1093/biomet/65.2.297. http://biomet.oxfordjournals.org/cgi/doi/10.1093/biomet/65.2.297. [DOI] [Google Scholar]
- 20.Fitzmaurice G M, Laird N M, Ware J H. Applied longitudinal analysis. Hoboken (NJ): John Wiley & Sons; 2004. Applied longitudinal analysis. [Google Scholar]
- 21.Pan Wei. Akaike’s information criterion in generalized estimating equations. Biometrics. 2001;57(1):120–125. doi: 10.1111/j.0006-341X.2001.00120.x. http://www.scholaruniverse.com/ncbi-linkout?id=11252586. [DOI] [PubMed] [Google Scholar]
- 22.Greenland S. Modeling and variable selection in epidemiologic analysis. Am J Public Health. 1989;79(3):340–349. doi: 10.2105/AJPH.79.3.340. http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.John Hopkins adjusted clinical groups (ACG) system. Baltimore (MD): John Hopkins University; [2012-01]. http://www.acg.jhsph.edu. [Google Scholar]
- 24.Kinsler Janni J, Wong Mitchell D, Sayles Jennifer N, Davis Cynthia, Cunningham William E. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS. 2007;21(8):584–592. doi: 10.1089/apc.2006.0202. http://www.scholaruniverse.com/ncbi-linkout?id=17711383. [DOI] [PubMed] [Google Scholar]
- 25.Sayles Jennifer N, Wong Mitchell D, Kinsler Janni J, Martins David, Cunningham William E. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009 Aug 4;24(10):1101–1108. doi: 10.1007/s11606-009-1068-8. http://pubmedcentralcanada.ca/pmcc/articles/pmid/19653047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schuster Mark A, Collins Rebecca, Cunningham William E, Morton Sally C, Zierler Sally, Wong Myra, Tu Wenli, Kanouse David E. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. 2005;20(9):807–813. doi: 10.1111/j.1525-1497.2005.05049.x. http://www.springerlink.com/index/10.1111/j.1525-1497.2005.05049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vlassoff Carol, Ali Firdaus. HIV-related stigma among South Asians in Toronto. Ethn Health. 2011;16(1):25–42. doi: 10.1080/13557858.2010.523456. http://www.tandfonline.com/doi/abs/10.1080/13557858.2010.523456. [DOI] [PubMed] [Google Scholar]
- 28.Weiser Sheri D, Wolfe William R, Bangsberg David R. The HIV epidemic among individuals with mental illness in the United States. Curr Infect Dis Rep. 2004;6(5):404–410. doi: 10.1007/s11908-004-0041-2. http://www.springerlink.com/index/10.1007/s11908-004-0041-2. [DOI] [PubMed] [Google Scholar]
- 29.Tobias Carol R, Cunningham William, Cabral Howard D, Cunningham Chinazo O, Eldred Lois, Naar-King Sylvie, Bradford Judith, Sohler Nancy L, Wong Mitchell D, Drainoni Mari-Lynn. Living with HIV but without medical care: barriers to engagement. AIDS Patient Care STDS. 2007;21(6):426–434. doi: 10.1089/apc.2006.0138. http://www.scholaruniverse.com/ncbi-linkout?id=17594252. [DOI] [PubMed] [Google Scholar]
- 30.Lucas Gregory M, Gebo Kelly A, Chaisson Richard E, Moore Richard D. Longitudinal assessment of the effects of drug and alcohol abuse on HIV-1 treatment outcomes in an urban clinic. AIDS. 2002;16(5):767–774. doi: 10.1097/00002030-200203290-00012. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00002030-200203290-00012. [DOI] [PubMed] [Google Scholar]
- 31.Cohen Mardge H, Cook Judith A, Grey Dennis, Young Mary, Hanau Lawrence H, Tien Phyllis, Levine Alexandra M, Wilson Tracey E. Medically eligible women who do not use HAART: the importance of abuse, drug use, and race. Am J Public Health. 2004;94(7):1147–1151. doi: 10.2105/AJPH.94.7.1147. http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.94.7.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stein M D, Crystal S, Cunningham W E, Ananthanarayanan A, Andersen R M, Turner B J, Zierler S, Morton S, Katz M H, Bozzette S A, Shapiro M F, Schuster M A. Delays in seeking HIV care due to competing caregiver responsibilities. Am J Public Health. 2000;90(7):1138–1140. doi: 10.2105/AJPH.90.7.1138. http://www.scholaruniverse.com/ncbi-linkout?id=10897195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook Judith A, Cohen Mardge H, Burke Jane, Grey Dennis, Anastos Kathryn, Kirstein Lynn, Palacio Herminia, Richardson Jean, Wilson Tracey, Young Mary. Effects of depressive symptoms and mental health quality of life on use of highly active antiretroviral therapy among HIV-seropositive women. J Acquir Immune Defic Syndr. 2002;30(4):401–409. doi: 10.1097/00042560-200208010-00005. http://www.scholaruniverse.com/ncbi-linkout?id=12138346. [DOI] [PubMed] [Google Scholar]
- 34.Shapiro M F, Morton S C, McCaffrey D F, Senterfitt J W, Fleishman J A, Perlman J F, Athey L A, Keesey J W, Goldman D P, Berry S H, Bozzette S A. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA. 1999;281(24):2305–2315. doi: 10.1001/jama.281.24.2305. http://www.scholaruniverse.com/ncbi-linkout?id=10386555. [DOI] [PubMed] [Google Scholar]
- 35.Mocroft A, Gill M J, Davidson W, Phillips A N. Are there gender differences in starting protease inhibitors, HAART, and disease progression despite equal access to care? J Acquir Immune Defic Syndr. 2000 Aug 15;24(5):475–482. doi: 10.1097/00126334-200008150-00013. http://www.scholaruniverse.com/ncbi-linkout?id=11035619. [DOI] [PubMed] [Google Scholar]
- 36.Ingram D, Hutchinson S A. HIV-positive mothers and stigma. Health Care Women Int. 1999;20(1):93–103. doi: 10.1080/073993399245999. [DOI] [PubMed] [Google Scholar]
- 37.Murphy Debra A, Roberts Kathleen J, Hoffman Dannie. Stigma and ostracism associated with HIV/AIDS: children carrying the secret of their mothers’ HIV+ serostatus. J Child Fam Stud. 2002;11(2):191–202. [Google Scholar]
- 38.Lucas G M, Chaisson R E, Moore R D. Highly active antiretroviral therapy in a large urban clinic: risk factors for virologic failure and adverse drug reactions. Ann Intern Med. 1999;131(2):81–87. doi: 10.7326/0003-4819-131-2-199907200-00002. [DOI] [PubMed] [Google Scholar]
- 39.Bersoff-Matcha S J, Miller W C, Aberg J A, van Der Horst C, Hamrick H J, Jr, Powderly W G, Mundy L M. Sex differences in nevirapine rash. Clin Infect Dis. 2000 Dec 13;32(1):124–129. doi: 10.1086/317536. http://www.scholaruniverse.com/ncbi-linkout?id=11118391. [DOI] [PubMed] [Google Scholar]
- 40.Galli Massimo, Veglia Fabrizio, Angarano Gioacchino, Santambrogio Sara, Meneghini Elena, Gritti Francesco, Cargnel Antonietta, Mazzotta Francesco, Lazzarin Adriano. Gender differences in antiretroviral drug-related adipose tissue alterations. Women are at higher risk than men and develop particular lipodystrophy patterns. J Acquir Immune Defic Syndr. 2003;34(1):58–61. doi: 10.1097/00126334-200309010-00008. http://www.scholaruniverse.com/ncbi-linkout?id=14501794. [DOI] [PubMed] [Google Scholar]
- 41.Weiser Sheri D, Fernandes Kimberly A, Brandson Eirikka K, Lima Viviane D, Anema Aranka, Bangsberg David R, Montaner Julio S, Hogg Robert S. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–349. doi: 10.1097/QAI.0b013e3181b627c2. http://www.scholaruniverse.com/ncbi-linkout?id=19675463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weiser Sheri D, Frongillo Edward A, Ragland Kathleen, Hogg Robert S, Riley Elise D, Bangsberg David R. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francsico. J Gen Intern Med. 2009;24(1):14–20. doi: 10.1007/s11606-008-0824-5. http://www.springerlink.com/index/10.1007/s11606-008-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aidala Angela A, Lee Gunjeong, Abramson David M, Messeri Peter, Siegler Anne. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav. 2007 Sep 3;11(6 Suppl):101–115. doi: 10.1007/s10461-007-9276-x. http://www.scholaruniverse.com/ncbi-linkout?id=17768674. [DOI] [PubMed] [Google Scholar]
- 44.Leaver Chad A, Bargh Gordon, Dunn James R, Hwang Stephen W. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007 Aug 8;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. http://www.scholaruniverse.com/ncbi-linkout?id=17682940. [DOI] [PubMed] [Google Scholar]
- 45.Beiser M. The health of immigrants and refugees in Canada. Can J Public Health. 2005;96 Suppl 2:2–30. doi: 10.1007/BF03403701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raboud J, Blitz S, Antoniou T, Loutfy M, Walmsley S. Recent immigrants show improved clinical outcomes at a tertiary care HIV Clinic. Can J Infect Dis Med Microbiol. 2012;23(1):9–14. doi: 10.1155/2012/963474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Virnig B A, McBean M. Administrative data for public health surveillance and planning. Annu Rev Public Health. 2001;22:213–230. doi: 10.1146/annurev.publhealth.22.1.213. http://www.scholaruniverse.com/ncbi-linkout?id=11274519. [DOI] [PubMed] [Google Scholar]
- 48.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710. doi: 10.2105/AJPH.82.5.703. http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith, G. D,, Hart C, Watt G, Hole D, Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley Study. J Epidemiol Community Health. 1998 Jun 1;52(6):399–405. doi: 10.1136/jech.52.6.399. http://jech.bmj.com/cgi/doi/10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]