Abstract
Background
The prevalence of diabetes mellitus and its complications is higher among First Nations people and people with low socio-economic status (SES). Previous studies in Alberta have shown that provision of care through Primary Care Networks (PCNs) is associated with better quality of care and better outcomes for people with diabetes, possibly because of greater utilization of chronic disease management programs. However, it is unknown whether First Nations individuals and those in lower SES groups experience these benefits.
Methods
We used administrative and laboratory data for a population-based cohort analysis of Alberta residents under 65 years of age with diabetes. The primary outcome, assessed over a 1-year period, was admission to hospital or emergency department visit for a diabetes-specific ambulatory care sensitive condition (ACSC). Secondary outcomes were 2 quality-of-care indicators (likelihood of measurement of glycated hemoglobin [HbA1c] and or retinal screening) and 2 measures of health care utilization (visits to specialist and primary care physicians). We used negative binomial regression to determine the association between care within a PCN and hospital admission or emergency department visit for diabetes-specific ACSCs. We also assessed outcomes in 3 populations of interest (individuals receiving a health care subsidy [household income less than $39 250 and not eligible for Income Support], those receiving Income Support, and First Nations individuals) relative to the remainder of the population, controlling for whether care was provided in a PCN and adjusting for several baseline characteristics.
Results
We identified a total of 106 653 patients with diabetes eligible for our study, of whom 43 327 (41%) received care in a PCN. Receiving care through a PCN was associated with lower rates of ACSC-related hospital admission or emergency department visits for all groups of interest, which suggests that PCNs had similar effects across each group. However, regardless of where care was provided, First Nations and low-SES patients had more than twice the adjusted rates of hospital admission or emergency department visits for diabetes-specific ACSCs than the general population and were less likely to receive guideline-recommended care, including measurement of HbA1c and retinal screening.
Interpretation
Care in a PCN was associated with lower risks of hospital admission or emergency department visits for diabetes-specific ACSCs, even within vulnerable groups such as First Nations people and those of low SES. However, differences in outcomes and quality-of-care indicators persisted for First Nations individuals and those of low SES, relative to the general population, irrespective of where care was provided.
One in 10 Canadian adults has diabetes mellitus,1 a condition that is associated with high health care costs and is frequently complicated by blindness, premature cardiovascular disease, and kidney failure.2-4 The prevalence of diabetes is higher in certain subsets of the Canadian population, including First Nations people and those experiencing poverty. Up to 15% of the on-reserve Canadian First Nations population may have diabetes,5 and people with low income have a 20% to 26% higher risk of this condition.6-8 Furthermore, both low-income individuals and First Nations people are less likely to access care, including specialist care, for problems such as diabetes,9,10 which may contribute to their worse health outcomes.4,10,11
The care of patients with diabetes is complex, often requiring a multidisciplinary approach and extensive patient education.12 Providing such care is challenging because primary care practices typically do not have the additional resources required to do so. Many Canadian jurisdictions are undergoing “primary care reform,” which includes establishing models of care for chronic diseases.13,14 In part, these reforms are meant to address concerns about access and equity, both important tenets of the Canadian health care system. Unfortunately, health care resources in Canada are delivered inequitably, especially in secondary and tertiary care.15 Improving primary care has been proposed as a means to improve equity within the health care system.16,17
Primary care reform in Alberta has taken the form of establishing Primary Care Networks (PCNs) in both rural and urban parts of the province. A PCN consists of primary care physicians and allied health care professionals working together to provide care to patients with and without chronic diseases. Funding to PCNs is provided on a capitated basis to support activities that fall outside the fee-for-service model, and these funds may be used to hire the allied health care professionals or for other initiatives, such as developing quality improvement programs for people with chronic diseases, including diabetes. Individual PCNs may take different approaches to chronic disease management, but most use multidisciplinary teams and enhanced patient education.18
PCNs are postulated to be an effective means of implementing models of chronic disease management.19 In a recent study evaluating the care and outcomes of patients with diabetes, our group documented that care within a PCN was associated with a slightly lower rate of admission to hospital or visits to the emergency department for diabetes-specific ambulatory care sensitive conditions (ACSCs) and a slightly lower mean glycated hemoglobin (HbA1c) level,20 relative to patients outside PCNs, possibly because of the implementation of quality improvement programs within the PCNs.18
Although our previous study suggested that care within PCNs was associated with small improvements in diabetes care for the overall Alberta population, it is not known whether PCNs help to achieve equity of care and outcomes across patient groups, especially those who might traditionally experience difficulties with accessing health care and for whom adverse outcomes are more common.4,10,11 Our objectives for the current study were to determine whether the apparent benefit of PCNs observed in the general population, measured in terms of admissions to hospital and emergency department visits for ACSCs, was also evident for First Nations people and those in lower SES groups and to determine the association between population type and outcomes after adjustment for PCN exposure. We hypothesized that the team-based approach of PCNs might have a more significant impact on care and outcomes for these vulnerable groups than for the general population.
Methods
Data sources and study population
The data sources have been described previously.20 Briefly, for the overall period 1994 Apr. 1 to 2009 Apr. 1, we extracted data on hospital admissions, physician visits, and emergency department visits from Alberta Health and Wellness administrative data files. We also obtained laboratory data from a province-wide repository that captures data for all Albertans who undergo inpatient or outpatient laboratory testing.21
Within these data sources, we used a validated algorithm to define a cohort of adult patients with a diagnosis of diabetes as of 2008 Apr. 1.22 A patient was considered to have prevalent diabetes if there were 2 or more physician claims for diabetes (International Statistical Classification of Diseases and Related Health Problems, 9th revision, Clinical Modification [ICD-9-CM] code 250) within a period of 2 years, or at least one hospital admission with an ICD-9-CM code of 250, selected from all available diagnostic codes on the patient’s hospital discharge abstract, between 1994 Apr. 1 and 2002 Mar. 31, or the equivalent ICD 10th revision (ICD-10) codes (E10–E14) from 2002 Apr. 1 to 2008 Apr. 1. The date of the first claim or hospital admission for diabetes (whichever came earlier) was defined as the date of diagnosis.
We were interested in assessing the effect of low SES or First Nations status on the care and outcomes of patients with diabetes. Because the Alberta Health and Wellness registry file classifies patients 65 years and older into a single population category (“pensioners”), with no further information on income, we excluded patients in this age group.
Study variables
PCN status
We used provincial administrative data and a defined protocol based on physician claims data to determine whether a patient had received care through a PCN.23
Population type
Patients were categorized as being in the general population, as having First Nations status, as receiving a health care subsidy, or as receiving Income Support, as specified in the Alberta Health and Wellness registry file. More specifically, First Nations status was defined as the presence of a First Nations status indicator at any time between 1994 Apr. 1 and 2009 Mar. 31, signalling that the person was registered under the federal Indian Act. All other patients in the study were categorized into 1 of 3 categories: general population (annual adjusted taxable family income at least $39 250), those receiving the Alberta Health Care Insurance Plan subsidy (family income less than $39 250 but not receiving Income Support),24 and those receiving Alberta Income Support (a heterogeneous group of individuals, including those not expected to work [because of chronic mental or physical ailments] and those expected to work [looking for or unable to find work]).25
Covariates and other variables of interest
We obtained demographic data, including age and sex, from the Alberta Health and Wellness registry file. We used data from the physician claims and hospital admission databases and validated algorithms to identify patients with hypertension.26 Other comorbid conditions and the Charlson comorbidity index were identified using validated ICD-9-CM and ICD-10 coding algorithms.27 We obtained estimated glomerular filtration rate (eGFR) and HbA1c from the provincial laboratory repository and defined the most recent outpatient eGFR and HbA1C values in the year before 2008 Apr. 1 as the “baseline” values for the purpose of our analysis.21
Outcome variables
Our primary outcome was hospital admission or emergency department visit for a diabetes-specific ACSC from 2008 Apr. 1 to 2009 Mar. 31. In general, the primary outcome corresponded to hospital admission or emergency department visit for hypoglycemia, diabetic ketoacidosis or hyperosmolar non-ketotic state, as determined by ICD codes in the Alberta Health and Wellness data set.28 These outcomes have been identified as a reasonable proxy for the quality of primary diabetes care (since appropriate outpatient management can help to reduce the burden of complications and the need for hospital admission29,30) and were adopted as such in the Canadian Consensus for the Standardized Evaluation of Quality Improvement Interventions in Type 2 Diabetes.31
The secondary outcomes of interest included 2 quality-of-care indicators: the proportion of people with at least one measurement of HbA1c and the proportion who underwent retinal screening by an ophthalmologist or optometrist during the 1-year observation period. The Canadian Diabetes Association (CDA) guidelines32 state that all patients with diabetes should have HbA1c levels checked every 3 to 6 months. These guidelines also state that patients with type 2 diabetes and a history of normal results on funduscopic examination require only biannual retinal screening. As such, not all of the patients in our sample would have required screening during the 1-year assessment period; nonetheless, differences in screening rates across groups would still be meaningful.
Finally, since access to health care is the first step in quality outpatient care, we assessed measures of health care utilization, including outpatient visits to internal medicine or endocrinology specialists and to primary care physicians.
Statistical analysis
Initially, we used a Poisson log–linear regression model to determine the rate of hospital admission or emergency department visits for diabetes-specific ACSC, by PCN status and population type. To test for overdispersion, we performed the deviance goodness-of-fit test. Given the presence of overdispersion, we used negative binomial regression models to calculate rate ratios (RRs) and to determine the association between care within a PCN and admission to hospital or visit to an emergency department for a diabetes-specific ACSC. Relevant covariates were identified using backward selection techniques. Final models were adjusted for age, sex, duration of diabetes, presence of hypertension, baseline HbA1c, baseline kidney function (in terms of eGFR), and Charlson comorbidity score. Age, baseline HbA1c, baseline kidney function, and Charlson score were modelled as categorical variables (see Table 1). We used an interaction term (PCN × population type) to determine whether this association varied by population type.
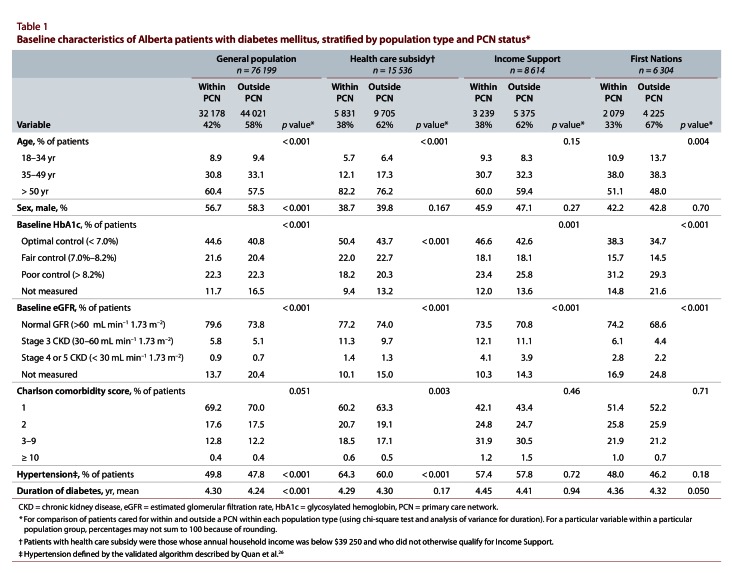
Table 1.
Baseline characteristics of Alberta patients with diabetes mellitus, stratified by population type and PCN status
Given that we also aimed to explore the association between population type and outcomes, we subsequently developed multivariate adjusted models, with population type as the primary exposure, using the general population as the reference group and adjusting for care within a PCN. We used logistic regression to determine the association between population type and dichotomous secondary outcomes (likelihood of HbA1C measurement, retinal screening, and specialist visits), with adjustment as described for our primary analysis. We used negative binomial regression and RRs for the outcome of primary care physician visits. All analyses were performed using STATA 11.0 (Statacorp, College Station, Tex.). This study was approved by the Conjoint Health Research Ethics Board of the University of Calgary.
Results
As of 2008 Apr. 1, we identified 183 654 persons with diabetes. After exclusion of patients 65 years of age and older (n = 77 001), 106 653 patients remained for analysis. Within each population type, those cared for within PCNs were older than those cared for outside of PCNs (Table 1). Baseline glycemic control (as indicated by HbA1c) and renal function (as indicated by eGFR) were generally slightly worse in the non-PCN group across population types. For most population types, the burden of comorbidities was similar for PCN and non-PCN groups, the exception being the health care subsidy group, for which the PCN group was more likely to have hypertension and higher Charlson comorbidity scores. Notably, only 33% of First Nations patients and 38% of patients receiving Income Support received care through a PCN, compared to 42% of the general population (p < 0.001).
Association between PCN status and primary outcome (admission to hospital or visit to emergency department for diabetes-specific ACSC)
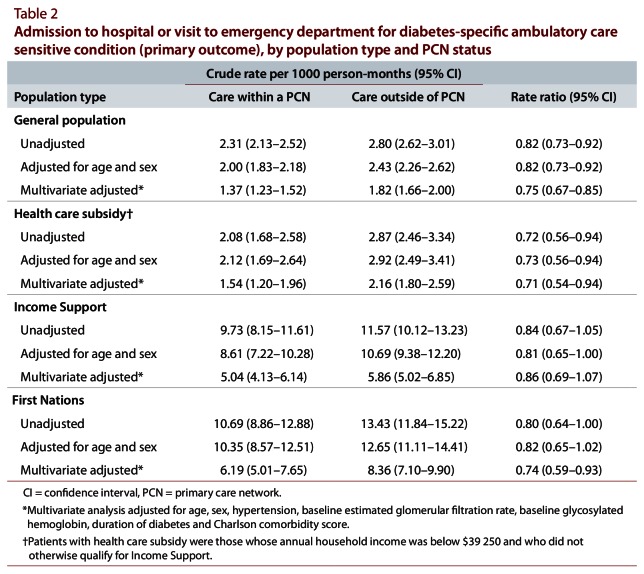
Receiving care in a PCN was associated with significantly lower rates of hospital admission or emergency department visits for diabetes-specific ACSCs for both the health care subsidy and First Nation groups, but no statistically significant association was noted for the Income Support group (Table 2). These results did not vary by population type (i.e., the interaction term was non-significant [p > 0.10]), which suggests that PCN care had similar effects across each of the groups.
Table 2.
Admission to hospital or visit to emergency department for diabetes-specific ambulatory care sensitive condition (primary outcome), by population type and PCN status
Although our primary analysis suggested that the association between PCNs and outcomes did not vary by population type, we did note important differences in quality of care and outcomes across population types, which are highlighted below.
Association between population type and primary outcome (admission to hospital or visit to emergency department for diabetes-specific ACSC)
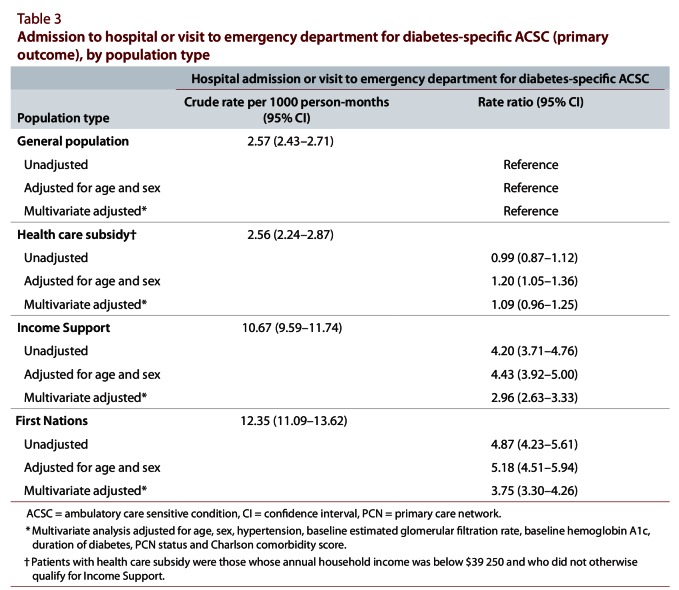
There were significant differences across groups in terms of crude rates of hospital admission or emergency department visits for a diabetes-specific ACSC, with significantly higher rates in the Income Support and First Nations groups (Table 3). Although these differences were attenuated after adjustment for confounders, including PCN status, there remained a marked difference in the adjusted rates of the primary outcome for people in the Income Support group and the First Nations group. Compared with the general population, both of these groups experienced an increased risk of admission to hospital or emergency department visit for diabetes-specific ACSC (for Income Support group, adjusted RR 2.96, 95% confidence interval [CI] 2.63–3.33; for First Nations group, adjusted RR 3.75, 95% CI 3.30–4.26).
Table 3.
Admission to hospital or visit to emergency department for diabetes-specific ACSC (primary outcome), by population type
Secondary outcomes: quality-of-care indicators
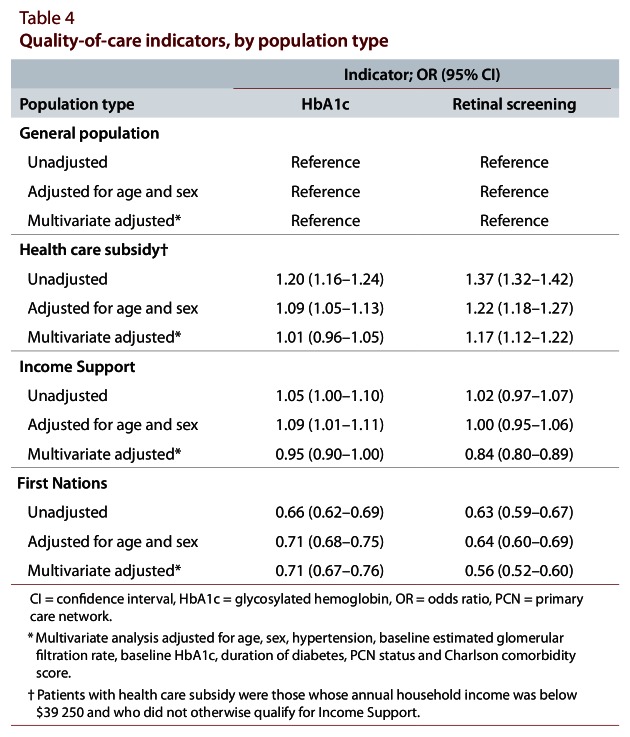
The likelihood that HbA1c would be measured at least once over the 1-year follow-up period varied by population type (Table 4), with patients receiving Income Support (adjusted odds ratio [OR] 0.95, 95% CI 0.90–1.00) and First Nations patients (adjusted OR 0.71, 95% CI 0.67–0.76) being significantly less likely to undergo HbA1c measurement relative to the general population.
Table 4.
Quality-of-care indicators, by population type
The odds of having retinal screening performed by an ophthalmologist or optometrist over the 1-year follow-up period were also lower for people in the Income Support and First Nations groups than in the general population (Table 4). Those receiving the health care subsidy were slightly more likely to undergo retinal screening than those in the general population (adjusted OR 1.17, 95% CI 1.12–1.22). The association between population type and these outcomes did not vary by PCN status, with the interaction term being non-significant (p > 0.10).
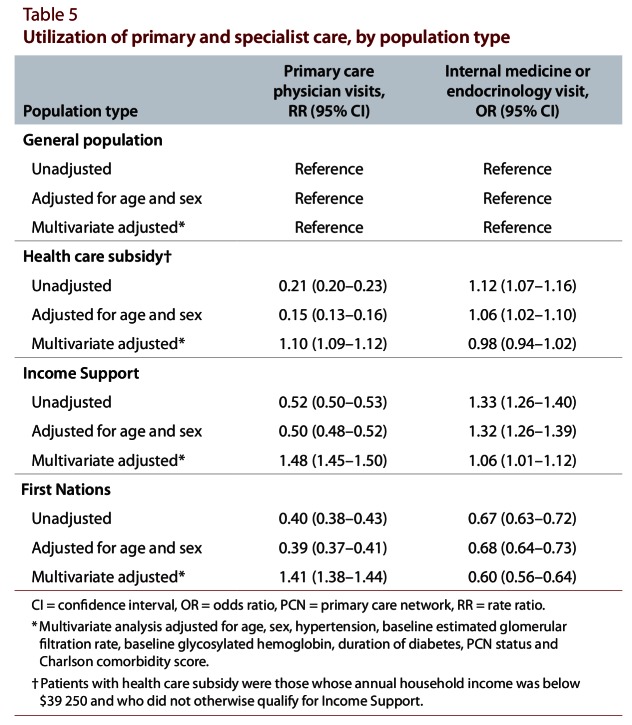
Secondary outcomes: health care resource utilization
Outpatient visits to primary care physicians were higher for the 3 groups of interest than for the general population (Table 5): for those receiving the health care subsidy, adjusted RR 1.10 (95% CI 1.09–1.12); for those receiving Income Support, adjusted RR 1.48 (95% CI 1.45–1.50); and for First Nations patients, adjusted RR 1.41 (95% CI 1.38–1.44). The First Nations group was significantly less likely to access specialist care over the course of the observation period (adjusted OR 0.60, 95% CI 0.56–0.64). As for the previous comparisons, we noted a non-significant interaction term in this analysis.
Table 5.
Utilization of primary and specialist care, by population type
Interpretation
In this study of administrative data from Alberta, we assessed the association between care in a PCN and outcomes for patients with diabetes and explored whether outcomes differed by population type. In general, care in PCNs was associated with better outcomes for people with diabetes across all population types, specifically lower rates of admission to hospital or emergency department visits for diabetes-specific ACSCs. This result is consistent with previous work showing that receipt of care in an Alberta PCN was associated with better diabetes-related outcomes and quality-of-care measures.20
Despite our hypothesis that PCNs would be associated with better care for high-risk groups (i.e., First Nations and those with lower SES), we found that PCNs were associated with similar improvements in outcomes for all groups (as indicated by non-significant interaction terms). However, the well-described disparities in quality of care and outcomes persisted for both the Income Support and First Nations cohorts, relative to the general population, even when these patients received care within PCNs.
PCNs represent Alberta’s version of primary care reform, but such reform has also occurred in other Canadian jurisdictions. Ontario has developed several new primary care models to enhance quality and access to care.14 These models have focused on changing physician payment from fee-for-service to capitation and providing incentives for provision of multidisciplinary care.33 Alberta’s PCNs are most closely aligned with Ontario’s Family Health Groups, in that both maintain a fee-for-service model with additional payments per patient enrolled. Both the Alberta PCNs and the Ontario Family Health Groups provide care to a representative sample of the population and are associated with decreased need for hospital care.14,34 It is unclear from our analysis which types of chronic disease management programs offered by PCNs in Alberta are associated with improvements in outcomes; however, in Ontario, the involvement of a nurse practitioner has been associated with improvements in chronic disease management, while changes to the funding model do not appear to have been associated with improvements in quality-of-care markers.35,36
We are unaware of other studies comparing the effect of primary care reform on care and outcomes of people with diabetes who are members of a First Nations or lower-SES group. Given that First Nations and low-income patients are at higher risk of diabetes-related complications,37,38 the impact of PCNs in these higher-risk groups is of significant interest. Despite better baseline health in terms of certain measures, First Nations persons had worse glycemic control and significantly higher crude rates of hospital admission or emergency department visits for diabetes-specific ACSCs than any of the other groups in the study, consistent with the literature on health care utilization among First Nations populations.39-41 There are likely many issues contributing to higher ACSCs in this population, including genetic, social, cultural, environmental and health system–related factors.42
Our study involved 2 low-SES groups: people receiving the health care subsidy (employed with family income less than $39 250 and not eligible for Income Support) and those receiving Income Support (unable to work or not having found work). These groups generally had worse baseline health status than the general population. Furthermore, their health status generally followed a gradient, with patients receiving the subsidy having worse health than the general population, and those receiving Income Support having worse health than those receiving the subsidy. Consistent with other studies, we found that individuals in the Income Support group had worse glycemic control and higher rates of diabetes-related hospital admission or emergency department visits.29,43,44
Both of the low-SES groups and the First Nations group had lower enrolment in PCNs (Table 1), possibly because they face greater barriers to regular primary care and are more likely to access care in a walk-in clinic setting. For First Nations people, this approach to seeking care may be related to the fact that many live on reserve, where (as noted below) some health care services may be provided through federal programs rather than provincial programs (such as PCNs).
Our study should be interpreted in light of its limitations. First, SES was not available for persons 65 years of age or older, as they are all classified as “pensioners” in the Alberta Health and Wellness registry file; as such, people in this age group were excluded from our analysis. Another limitation with this classification system is the lack of income data for the First Nations cohort; as such, we could not determine how their SES compared with that of the non–First Nations group. We were also unable to include rurality as a variable within our models, although it may be a relevant covariate for our outcomes of interest. Analyses based on administrative data have well known limitations, including inconsistency or potential unreliability of information available in the hospital discharge abstracts and physician claims data used to estimate the prevalence of comorbid conditions. However, it is unlikely that systematic differences existed in terms of completeness of coding for patients cared for within or outside of a PCN or for patients with different SES levels. Finally, we were unable to identify whether First Nations people were living on or off reserve, a factor that could potentially mask some differences within the First Nations group. This distinction is also important because of its implications for the care people received: on many reserves, diabetes care is supplemented by the Aboriginal Diabetes Initiative (ADI) of Health Canada’s First Nations and Inuit Health Branch,45 care that is not recorded in the Alberta Health and Wellness database. However, although the ADI administers the retinal screening program, all images are read through tele-ophthalmology consultations in which the ophthalmologist is paid on a fee-for-service basis through Alberta Health and Wellness, which would be captured in our data. In contrast, point-of-care measurement of HbA1c administered by the ADI was not captured in the administrative databases that we used; therefore, our results may underestimate HbA1c measurement performed for First Nations individuals living on reserve.
The use of population-based administrative data is a major strength of this study, because it allowed us to undertake a population-based study of persons with diabetes who were receiving care in Alberta. Furthermore, the ability to combine province-wide laboratory data with information on health care utilization enabled us to assess process-based markers of care, as well as clinically relevant outcomes.
Care in PCNs was associated with better outcomes for First Nations individuals and those requiring social assistance, but the current model of care does not appear to fully address existing disparities, possibly because chronic disease management programs designed for the general population are less effective in reaching people with lower SES.46,47 Patients in the lowest SES group may have other priorities that take precedence over improving how they manage their diabetes.48 Previous studies have suggested that chronic disease management programs for people with low SES may be more effective when specifically tailored to the needs of those populations,49 and certain features of such programs are recommended, including high intensity, long duration, and the incorporation of community outreach and diligent follow-up.47,50
Consistent with prior work, we noted that care in PCNs was associated with better outcomes (in terms of hospital admission or emergency department visits for diabetes-specific ACSCs) for people with diabetes. Although this difference occurred across all population groups, important disparities in quality of care and outcomes persisted for the highest-risk groups (those receiving Income Support and First Nations individuals, compared with the general population), which suggests that additional programming and different models of care are required for these groups. Future research should focus on implementing and evaluating strategies aimed at improving processes of care and outcomes in these high-risk groups.
Biographies
David J. T. Campbell, MD, MSc, is a graduate student in the Department of Community Health Sciences, University of Calgary, Calgary, Alberta.
Paul E. Ronksley, MSc, is a PhD candidate in the Department of Community Health Sciences, University of Calgary, Calgary, Alberta.
Brenda R. Hemmelgarn, MD, PhD, is an Associate Professor in the Departments of Medicine and of Community Health Sciences, University of Calgary, Calgary, Alberta.
Jianguo Zhang, MSc, is a Senior Research Assistant with the Alberta Kidney Disease Network, University of Calgary, Calgary, Alberta.
Cheryl Barnabe, MD, MSc, is an Assistant Professor in the Departments of Medicine and of Community Health Sciences, University of Calgary, Calgary, Alberta.
Marcello Tonelli, MD, SM, is a Professor in the Department of Medicine, University of Alberta, Edmonton, Alberta.
Braden Manns, MD, MSc, is an Associate Professor in the Departments of Medicine and of Community Health Sciences, University of Calgary, Calgary, Alberta.
Footnotes
Competing interests: None declared.
Funding source: This research was supported by an interdisciplinary team grant from Alberta Innovates – Health Solutions, the Interdisciplinary Chronic Disease Collaboration, and the Canadian Institutes of Health Research (application no. 238543).The funding organizations had no role in the conception, design, conduct, analysis, interpretation, or reporting of the study and had no access to the data.
David Campbell, Paul Ronksley, Brenda Hemmelgarn, Marcello Tonelli, and Braden Manns designed the study protocol. David Campbell, Paul Ronksley, Jianguo Zhang, and Cheryl Barnabe were involved with the analysis and interpretation of the data. David Campbell wrote the first draft of the manuscript. All authors contributed to drafting and critically revising the manuscript. Braden Manns is guarantor for the manuscript and takes responsibility for the contents and appropriateness of the reference list.
References
- 1.The prevalence and costs of diabetes: facts. Toronto (ON): Canadian Diabetes Association; 2009. [accessed 2011 Sept.]. http://www.diabetes.ca/documents/about-diabetes/PrevalanceandCost_09.pdf. [Google Scholar]
- 2.Herman William H. The economics of diabetes prevention. Med Clin North Am. 2011;95(2):373–384. doi: 10.1016/j.mcna.2010.11.010. http://pubmedcentralcanada.ca/pmcc/articles/pmid/21281839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simpson Scot H, Corabian Paula, Jacobs Philip, Johnson Jeffrey A. The cost of major comorbidity in people with diabetes mellitus. CMAJ. 2003 Jun 24;168(13):1661–1667. http://pubmedcentralcanada.ca/pmcc/articles/pmid/12821619. [PMC free article] [PubMed] [Google Scholar]
- 4.Diabetes in Canada: national statistics and opportunities for improved surveillance, prevention and control. Ottawa (ON): Health Canada; 2011. [accessed 2012 Nov.]. http://www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/index-eng.php. [Google Scholar]
- 5.First Nations regional longitudinal health survey (RHS) 2002/03 survey results for adults, youth and children living in First Nations communities. Ottawa (ON): First Nations Centre; 2005. [accessed 2011 Oct.]. http://www.rhs-ers.ca/sites/default/files/ENpdf/RHS_2002/rhs2002-03-technical_report.pdf. [Google Scholar]
- 6.Choi B C K, Shi F. Risk factors for diabetes mellitus by age and sex: results of the National Population Health Survey. Diabetologia. 2001;44(10):1221–1231. doi: 10.1007/s001250100648. http://www.springerlink.com/openurl.asp?genre=article&id=doi:10.1007/s001250100648. [DOI] [PubMed] [Google Scholar]
- 7.Smith Brendan T, Lynch John W, Fox Caroline S, Harper Sam, Abrahamowicz Michal, Almeida Nisha D, Loucks Eric B. Life-course socioeconomic position and type 2 diabetes mellitus: the Framingham Offspring Study. Am J Epidemiol. 2011;173(4):438–447. doi: 10.1093/aje/kwq379. http://pubmedcentralcanada.ca/pmcc/articles/pmid/21242301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yu Vanessa L, Raphael Dennis. Identifying and addressing the social determinants of the incidence and successful management of type 2 diabetes mellitus in Canada. Can J Public Health. 2004;95(5):366–368. doi: 10.1007/BF03405148. http://www.scholaruniverse.com/ncbi-linkout?id=15490927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunlop S, Coyte P C, McIsaac W. Socio-economic status and the utilisation of physicians’ services: results from the Canadian National Population Health Survey. Soc Sci Med. 2000;51(1):123–133. doi: 10.1016/S0277-9536(99)00424-4. http://linkinghub.elsevier.com/retrieve/pii/S0277953699004244. [DOI] [PubMed] [Google Scholar]
- 10.Gao Song, Manns Braden J, Culleton Bruce F, Tonelli Marcello, Quan Hude, Crowshoe Lynden, Ghali William A, Svenson Lawrence W, Ahmed Sofia, Hemmelgarn Brenda R. Access to health care among status Aboriginal people with chronic kidney disease. CMAJ. 2008 Nov 4;179(10):1007–1012. doi: 10.1503/cmaj.080063. http://www.cmaj.ca/cgi/doi/10.1503/cmaj.080063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raphael D. Poverty, income inequality, and health in Canada. Toronto (ON): CSJ Foundation for Research and Education; 2002. [accessed 2011 May]. http://www.povertyandhumanrights.org/docs/incomeHealth.pdf. [Google Scholar]
- 12.Rubin R J, Dietrich K A, Hawk A D. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab. 1998;83(8):2635–2642. doi: 10.1210/jc.83.8.2635. http://jcem.endojournals.org/cgi/doi/10.1210/jc.83.8.2635. [DOI] [PubMed] [Google Scholar]
- 13.Shortt S. CMA leadership series: primary care reform. Ottawa (ON): Canadian Medical Assocation; [accessed 2011 Oct.]. Primary care reform: change in search of evidence? http://www.cma.ca/multimedia/CMA/Content_Images/Inside_cma/WhatWePublish/LeadershipSeries/English/in_search_of_evidence.pdf. [Google Scholar]
- 14.Glazier R, Zagorski B M, Rayner J. Comparison of primary care models in Ontario by demographics, case mix and emergency department use, 2008/09 to 2009/10. Toronto (ON): Institute for Clinical Evaluative Sciences; 2012. [accessed 2012 July]. http://www.ices.on.ca/file/ICES_Primary%20Care%20Models%20English.pdf. [Google Scholar]
- 15.Murphy K, Glazier R, Wang X, Holton E, Fazli G, Ho M. Hospital care for all: an equity report on differences in household income among patients at Toronto Central Local Health Integration Network (TC LHIN) hospitals, 2008–2010. Toronto (ON): Institute for Clinical Evaluative Sciences; 2012. [accessed 2011 Oct.]. http://www.stmichaelshospital.com/crich/projects/hospital-care-for-all.php. [Google Scholar]
- 16.Starfield Barbara, Shi Leiyu. The medical home, access to care, and insurance: a review of evidence. Pediatrics. 2004;113(5 Suppl):1493–1498. http://www.scholaruniverse.com/ncbi-linkout?id=15121917. [PubMed] [Google Scholar]
- 17.Glazier Richard H. Balancing equity issues in health systems: perspectives of primary healthcare. Healthc Pap. 2007;8 Spec No:35–45. doi: 10.12927/hcpap.2007.19218. [DOI] [PubMed] [Google Scholar]
- 18.Campbell D, Sargious P, Lewanczuk R, McBrien K, Tonelli M, Hemmelgarn B, et al The use of chronic disease management programs for diabetes by Alberta’s Primary Care Networks. Can Fam Physician. In press [PMC free article] [PubMed] [Google Scholar]
- 19.Every Barbara. Better for ourselves and better for our patients: chronic disease management in primary care networks. Healthc Q. 2007;10(3):70–74. doi: 10.12927/hcq..18927. http://www.longwoods.com/product.php?productid=18927. [DOI] [PubMed] [Google Scholar]
- 20.Manns Braden J, Tonelli Marcello, Zhang Jianguo, Campbell David J T, Sargious Peter, Ayyalasomayajula Bharati, Clement Fiona, Johnson Jeffrey A, Laupacis Andreas, Lewanczuk Richard, McBrien Kerry, Hemmelgarn Brenda R. Enrolment in primary care networks: impact on outcomes and processes of care in patients with diabetes. CMAJ. 2012;184(2):144–152. doi: 10.1503/cmaj.110755. http://pubmedcentralcanada.ca/pmcc/articles/pmid/22143232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hemmelgarn Brenda R, Clement Fiona, Manns Braden J, Klarenbach Scott, James Matthew T, Ravani Pietro, Pannu Neesh, Ahmed Sofia B, MacRae Jennifer, Scott-Douglas Nairne, Jindal Kailash, Quinn Robert, Culleton Bruce F, Wiebe Natasha, Krause Richard, Thorlacius Laurel, Tonelli Marcello. Overview of the Alberta Kidney Disease Network. BMC Nephrol. 2009;10(1):30. doi: 10.1186/1471-2369-10-30. http://www.biomedcentral.com/1471-2369/10/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hux Janet E, Ivis Frank, Flintoft Virginia, Bica Adina. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25(3):512–516. doi: 10.2337/diacare.25.3.512. http://www.scholaruniverse.com/ncbi-linkout?id=11874939. [DOI] [PubMed] [Google Scholar]
- 23.Funding a primary care network: four cut funding methodology. Edmonton (AB): Government of Alberta, Primary Care Initiative; 2007. [accessed 2011 Apr.]. http://www.albertapci.ca/DevelopingPCN/PCNFunding/Documents/Fact%20Sheet%20-%20Four%20Cut%20Funding%20Methodology_Nov24FINAL.pdf. [Google Scholar]
- 24.Premium assistance program—premium subsidy. Edmonton (AB): Government of Alberta, Health and Wellness; 2011. [accessed 2011 Apr.]. http://www.health.alberta.ca/AHCIP/premium-subsidy.html. [Google Scholar]
- 25.Income support. Edmonton (AB): Government of Alberta, Employment and Immigration; 2006. [accessed 2012 Apr.]. http://employment.alberta.ca/FCH/689.html. [modified 2010] [Google Scholar]
- 26.Quan H, Khan N, Hemmelgarn B. R., Tu K, Chen G, Campbell N, Hill M. D., Ghali W. A., McAlister F. A. Hypertension Outcome and Surveillance Team of the Canadian Hypertension Education Programs. Validation of a case definition to define hypertension using administrative data. Hypertension. 2009;54(6):1423–1428. doi: 10.1161/HYPERTENSIONAHA.109.139279. http://hyper.ahajournals.org/cgi/doi/10.1161/HYPERTENSIONAHA.109.139279. [DOI] [PubMed] [Google Scholar]
- 27.Quan Hude, Sundararajan Vijaya, Halfon Patricia, Fong Andrew, Burnand Bernard, Luthi Jean-Christophe, Saunders L D, Beck Cynthia A, Feasby Thomas E, Ghali William A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. http://www.scholaruniverse.com/ncbi-linkout?id=16224307. [DOI] [PubMed] [Google Scholar]
- 28.Technical note: ambulatory care sensitive conditions (ACSC) Ottawa (ON): Canadian Institute for Health Information; 2010. [accessed 2011 Apr.]. http://www.cihi.ca/CIHI-ext-portal/internet/en/document/health+system+performance/indicators/health/tech_acsc_2010. [Google Scholar]
- 29.Booth Gillian L, Hux Janet E. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med. 2003 Jan 13;163(1):101–106. doi: 10.1001/archinte.163.1.101. http://www.scholaruniverse.com/ncbi-linkout?id=12523923. [DOI] [PubMed] [Google Scholar]
- 30.Stratton I M, Adler A I, Neil H A, Matthews D R, Manley S E, Cull C A, Hadden D, Turner R C, Holman R R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. http://pubmedcentralcanada.ca/pmcc/articles/pmid/10938048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Majumdar S R, Johnson J A, Bowker S L, Booth G L, Dolovich L, Ghali W, Harris S B, Hux, J. E, Holbrook A, Lee H N, Toth E L, Yale J. A Canadian consensus for the standardized evaluation of quality improvement interventions in type 2 diabetes. Can J Diabetes. 2005;29(3):220–229. http://www.diabetes.ca/files/Johnson_Canadian_Conensus-pages%20220-229.pdf. [Google Scholar]
- 32.Canadian Diabetes Association. Canadian Diabetes Association 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32(Suppl 1) [Google Scholar]
- 33.Kralj B, Katarevic J, OMA Department of Economics Primary care in Ontario: reforms, investments and achievements. [accessed 2011 Aug.];Ont Med Rev. 2012 Feb;:18–24. https://www.oma.org/Resources/Documents/PrimaryCareFeature.pdf. [Google Scholar]
- 34.Liddy Clare, Singh Jatinderpreet, Hogg William, Dahrouge Simone, Taljaard Monica. Comparison of primary care models in the prevention of cardiovascular disease—a cross sectional study. BMC Fam Pract. 2011;12(1):114. doi: 10.1186/1471-2296-12-114. http://www.biomedcentral.com/1471-2296/12/114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russell Grant M, Dahrouge Simone, Hogg William, Geneau Robert, Muldoon Laura, Tuna Meltem. Managing chronic disease in Ontario primary care: the impact of organizational factors. Ann Fam Med. 2009;7(4):309–318. doi: 10.1370/afm.982. http://www.scholaruniverse.com/ncbi-linkout?id=19597168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dahrouge Simone, Hogg William E, Russell Grant, Tuna Meltem, Geneau Robert, Muldoon Laura K, Kristjansson Elizabeth, Fletcher John. Impact of remuneration and organizational factors on completing preventive manoeuvres in primary care practices. CMAJ. 2012;184(2):135–143. doi: 10.1503/cmaj.110407. http://pubmedcentralcanada.ca/pmcc/articles/pmid/22143227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Booth Gillian L, Hux Janet E, Fang Jiming, Chan Benjamin T B. Time trends and geographic disparities in acute complications of diabetes in Ontario, Canada. Diabetes Care. 2005;28(5):1045–1050. doi: 10.2337/diacare.28.5.1045. http://care.diabetesjournals.org/cgi/doi/10.2337/diacare.28.5.1045. [DOI] [PubMed] [Google Scholar]
- 38.Secrest Aaron M, Costacou Tina, Gutelius Bruce, Miller Rachel G, Songer Thomas J, Orchard Trevor J. Associations between socioeconomic status and major complications in type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complication (EDC) Study. Ann Epidemiol. 2011;21(5):374–381. doi: 10.1016/j.annepidem.2011.02.007. http://pubmedcentralcanada.ca/pmcc/articles/pmid/21458731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.A statistical profile on the health of First Nations in Canada: health services utilization in western Canada, 2000. Ottawa (ON): Health Canada; 2009. [accessed 2011 May]. http://www.hc-sc.gc.ca/fniah-spnia/pubs/aborig-autoch/2009-stats-profil-vol2/index-eng.php. [Google Scholar]
- 40.Martens P, Bond R, Jebamani L, Burchill C, Roos N, Derksen S, Beaulieu M, Steinbach C, MacWilliam L, Walid R, Dik N, Tanner-Spence M, Leader A, Elias B, O'Neil J. The health and health care use of registered First Nations people living in Manitoba: a population-based study. Winnipeg (MB): Manitoba Centre for Health Policy; 2002. http://mchp-appserv.cpe.umanitoba.ca/reference/rfn_report.pdf. [Google Scholar]
- 41.Carrière G, Garner R, Sanmartin C, LHAD Research Team . Acute-care hospitalizations and Aboriginal identity in Canada, 2001/2002. Ottawa (ON): Statistics Canada; 2010. http://www.statcan.gc.ca/pub/82-622-x/82-622-x2010005-eng.pdf. [Google Scholar]
- 42.Young T K, Reading J, Elias B, O’Neil J D. Type 2 diabetes mellitus in Canada’s First Nations: status of an epidemic in progress. CMAJ. 2000;163(5):561–566. http://pubmedcentralcanada.ca/pmcc/articles/pmid/11006768. [PMC free article] [PubMed] [Google Scholar]
- 43.Chaturvedi N, Stephenson J. M., Fuller J. H. The relationship between socioeconomic status and diabetes control and complications in the EURODIAB IDDM Complications Study. Diabetes Care. 1996 May 1;19(5):423–430. doi: 10.2337/diacare.19.5.423. http://care.diabetesjournals.org/cgi/doi/10.2337/diacare.19.5.423. [DOI] [PubMed] [Google Scholar]
- 44.Hassan Krishnavathana, Loar Robert, Anderson Barbara J, Heptulla Rubina A. The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J Pediatr. 2006;149(4):526–531. doi: 10.1016/j.jpeds.2006.05.039. http://linkinghub.elsevier.com/retrieve/pii/S002234760600480X. [DOI] [PubMed] [Google Scholar]
- 45.Aboriginal Diabetes Initiative: program framework 2010–2015. Ottawa (ON): Health Canada; 2011. [accessed 2012 Jan.]. http://www.hc-sc.gc.ca/fniah-spnia/pubs/diseases-maladies/_diabete/2010-2015-frame-cadre/index-eng.php. [Google Scholar]
- 46.Engelhardt Katrin, Ahn Byung C, Cho Sung-Il, Joung Hyojee. Predictors of interest in nutrition topics and willingness to participate in local nutrition programmes. J Public Health (Oxf) 2006 Jun 29;29(1):9–12. doi: 10.1093/pubmed/fdl024. http://jpubhealth.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16809793. [DOI] [PubMed] [Google Scholar]
- 47.Glazier Richard H, Bajcar Jana, Kennie Natalie R, Willson Kristie. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29(7):1675–1688. doi: 10.2337/dc05-1942. http://www.scholaruniverse.com/ncbi-linkout?id=16801602. [DOI] [PubMed] [Google Scholar]
- 48.Gelberg L, Gallagher T C, Andersen R M, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–220. doi: 10.2105/AJPH.87.2.217. http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hill-Briggs Felicia, Lazo Mariana, Peyrot Mark, Doswell Angela, Chang Yi-Ting, Hill Martha N, Levine David, Wang Nae-Yuh, Brancati Frederick L. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med. 2011;26(9):972–978. doi: 10.1007/s11606-011-1689-6. http://www.springerlink.com/index/10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huckfeldt Peter J, Meeker Daniella, Peters Anne, Guterman Jeffrey J, Diaz Guillermo, Jr, Goldman Dana P. Diabetes management for low-income patients in Los Angeles: two strategies improved disease control in the short term. Health Aff (Millwood) 2012;31(1):168–176. doi: 10.1377/hlthaff.2011.0930. [DOI] [PMC free article] [PubMed] [Google Scholar]