Abstract
Background
Concerns about psychoactive prescription drug abuse among youth are growing worldwide, but the majority of published studies remain from the US and Canada impeding cross-cultural comparisons. This study examines the prevalence, sources, motivations and substance-use correlates of commonly abused medications among youth from Lebanon.
Methods
An IRB-approved cross-sectional study was conducted (May 2010) at the American University of Beirut. Proportionate cluster sampling was used to generate a representative sample of AUB students (n=570). A self-filled anonymous questionnaire was administered.
Results
Lifetime medical and nonmedical prevalence of medications were (respectively): pain (36.9%, 15.1%), anxiety (8.3%, 4.6%), sleeping (6.5%, 5/8%) and stimulants (2.6%, 3.5%). Gender differences were not observed. Lebanese were least likely to report non-medical use. Nonmedical users mostly used the drugs for their intended purpose (e.g., sleeping to help in sleep, stimulants to increase alertness). Parents and pharmacists (without a doctor’s prescription) were the top two sources of all medications but stimulants whereby friends predominated. Diversion was observed in about 20% of the medical users. Lifetime marijuana users and past year alcohol abusers were three times as likely to use any prescription drug nonmedically.
Conclusions
In Lebanon, as in Western cultures, a considerable proportion of youth may be self-medicating. The absence of medical supervision coupled with motivations such as “to get high” renders this issue a high priority on the national youth agenda. Besides larger more comprehensive surveys, the findings signal the immediate need to raise awareness among youth, parents, health professionals and other stakeholders, as well as to reinforce relevant policies.
Keywords: prescription drugs, self-medication, diversion, nonmedical use, students, Lebanon
1. Introduction
Nonmedical use of psychoactive prescription medications is a major and growing public health concern (Friedman, 2006; Kuehn, 2006; Zarocostas, 2007). Recent studies, mostly from the US, point towards an increasing prevalence (Figueiras et al., 2000; Haydon et al., 2005; Kuehn, 2006; Blanco et al., 2007; Johnston, 2009), one that is growing at a faster rate than most illegal drugs (Blanco et al., 2007; McCabe et al., 2005; Catalano et al., 2010). Opioid pain relievers are in fact the second most commonly abused drug following marijuana (Blanco et al., 2007; Catalano et al., 2010). Youth aged 18-25 are particularly vulnerable, showing by far the highest percentage of nonmedical use (Blanco et al., 2007), particularly with regards to pain medications and stimulants (Compton and Volkow, 2006; Johnston et al., 2008). Though much of the data comes from the Western world (Compton and Volkow, 2006; Fischer and Rehm, 2008; Garnier et al., 2009; Haydon et al., 2005; Levine and Coupey, 2009; McCabe et al., 2009; McCauley et al., 2010), a recent UN panel has declared the issue a worldwide problem, exceeding that of illegal drug use (Zarocostas, 2007).
Nonmedical use has been defined as use of prescription medications without a doctor’s prescription, or for longer periods than prescribed, or for reasons other than the medication’s intended medical purpose (e.g., to get a high feeling) (McCabe and Boyd, 2005; McCabe et al., 2005; Kroutil et al., 2006; McCabe et al., 2006). High and increasing rates have been attributed to the fact that these medications are legally manufactured, prescribed by medical professionals, and characterized by the misconception that they are risk-free or safer than illegal drugs (Friedman, 2006; Kuehn, 2006; Johnston, 2009). Yet, what is perhaps largely unknown to most is that despite their therapeutic properties, these medications are associated with serious health risks when taken without medical supervision. Psychoactive prescription drugs, for example, are highly addictive since they operate on the same receptors and brain systems as illegal drugs. Moreover, young nonmedical users may face dangerous adverse reactions from interactions and contraindications with other medicines or substances like alcohol, or fatal overdose and poisonings (Volkow, 2005).
Since nonmedical users do not obtain their medication based on a doctor’s prescription, several studies have investigated possible other sources and delineated peers and parents as one of the main outlets for obtaining psychoactive medications (McCabe et al., 2005; Levine and Coupey, 2009). Moreover, the practice of diversion (or being approached to sell, trade or give away prescribed medication) is quite common among medical users in college, especially during stressful events (McCabe et al., 2005; Boyd et al., 2007; Goldsworthy et al., 2008).
Up to our knowledge, no published regional studies have examined the issue of psychoactive prescription medication use among Arab youth. In Lebanon, nonmedical use of prescription is not a new phenomenon (Nassar et al., 1973). The only substance use monitoring survey on private university students in Lebanon pointed towards an increase in tranquilizer (10.2% to 13.1%) and stimulant use (1.8% to 4.3%) from 1991 to 1999 (Karam et al., 2000). In a sample of a younger high school population surveyed in 2001, the lifetime prevalence for nonmedical use of tranquilizers and barbiturates/medicinal opiates was 3.3% and 1.2%, respectively (Karam et al., 2003). Still, available studies from Lebanon remain mostly descriptive of the proportion of users, without careful examination of the underlying motives, possible sources, and association with other illegal substance use.
Recent anecdotal reports suggest that self-medication may be increasing among the Lebanese to cope with their mental health symptoms resulting from the irregular invasions, internal conflicts, and political instability (Solberg, 2008). It has been suggested that the sales of psychotropic medications often increase during and after times of war and tensions (Solberg, 2008), and prescription drug sales regulations tend to fluctuate. In reality, numerous influential factors may have either led to an increase (e.g., July 2006 war, internal political unrests) or a decrease in the prevalence rates (e.g., relatively stricter sales’ measures), all of which are speculations until supported by epidemiological surveys.
Given previous data and the current global trends, prescription medication use among youth in Lebanon warrants closer attention, particularly since the latest survey (2001) was conducted prior to the enforcement of stricter sale measures in 2003. This study aims at addressing several research questions including: what are the most commonly used prescription medications among youth in Lebanon, both medically, and nonmedically?; Is diversion a common practice among medical users?; what are the major sources for obtaining these medications among nonmedical users?; what are the most commonly reported reasons for use among nonmedical users?; and, what is the youth’s perception in Lebanon with respect to the availability of these medications? Findings would not only add to the scant scientific literature from the region, but would also help create evidence-based awareness messages to raise awareness among youth and other stakeholders, and stir policy changes and drug prevention efforts. Given the paucity or absence of comparable data from countries other than the US (and Canada), this study further provides a much needed unique opportunity to compare data across cultures (Fischer and Rehm, 2008), while highlighting important contextual differences.
2. Methodology
2.1 Participants
This study was approved by the AUB Institutional Review Board (IRB). A representative sample of undergraduate and graduate students at AUB, a large non-profit private university, was selected. AUB has a diverse student population with around 66 countries represented, mostly regional. The sample (n=570) was selected using a proportionate cluster sampling technique to ensure representation by faculty and year of education (undergraduate/graduate). Of the classrooms selected, 52.2% of the class professors agreed to participate, 9% refused to take part in the survey mainly due to timing since the survey took place during the last month of the academic year (due to delays in the IRB review process), and the remaining 38.8% did not respond despite several attempts. Of the participating classes, 86% of the students available in the classrooms agreed to participate, or 60.0% of the registered students.
A self-filled anonymous questionnaire was distributed, as in other major drug use surveys (Harrison, 1997; Johnston and O’malley, 1997), during class hours, with careful consideration to timing, avoiding all major examination periods. An informed consent attached to the questionnaire clearly stressed anonymity and confidentiality, voluntary participation, and other ethical considerations that would in turn help minimize non-response (Harrison, 1997).
2.2 Measures
Several demographics were assessed (e.g., gender, age, nationality, marital status, living arrangement, average grade in the preceding semester, socioeconomic status (SES)). SES was a self-perceived measure: “Compared to other people your age, how well-off do you think you/your family is?” and the response categories included: a little or a lot poorer than most, about the same as most, a little or a lot richer than most.
Past year alcohol use and DSM-IV defined abuse, as well as the lifetime and past year use of various illegal substances was also assessed. Questions on the medical and nonmedical use of the four most commonly abused classes of psychoactive drugs (i.e., pain, sleeping, anxiety, stimulants) were abstracted from the Student Life Survey questionnaire developed by University of Michigan (McCabe et al., 2005; Boyd et al., 2006; McCabe et al., 2007). Market available trade names were used to increase identification and reduce information errors.
Medical use, defined as the use of medications “based on a doctor’s prescription”, was assessed by the following question (for example): “Based on a doctor’s prescription, have you ever taken any sleeping medication (e.g., Stilnox®, Ambien®)? In other words, has a doctor prescribed for you a sleeping medication?” The same question was posed for lifetime and past 12 months. Medical users of any prescription medication were also asked about ever diverting their medication, defined as ever being approached to sell, to trade or give away the medications (McCabe et al., 2006; El-Aneed et al., 2009).
Nonmedical use was defined as using prescription drugs that were prescribed for somebody else, or using the medications for longer periods than prescribed, or for reasons other than what the medication is intended for (e.g., to get high) (McCabe et al., 2005; McCabe et al., 2006; Kuehn, 2007; Garnier et al., 2009; McCabe et al., 2009). Specifically, the following question was posed (for example): “Have you used any pain medication (e.g., DiAntalvic®, Vicodin®, Defalgan and Codeine®, Tramal®, and other) for nonmedical purposes?”, after having defined the term. Both lifetime and past 12 month use were assessed. Nonmedical users were further asked about source(s) of obtaining their psychoactive prescription medications as well as reason(s) for use (more than one source/reason may have been reported).
Perceived availability and accessibility to these medications was also assessed: “How difficult would you say it is for you to get each of the following types of drugs if you wanted some?” against a likert scale (probably impossible to very easy).
2.3 Data analyses
Sampling weights were calculated to yield a weighted sample size to represent the entire AUB student population. Pearson’s Chi-square test and binary logistic regressions were conducted using Stata (version 10); all analyses were weighed to account for the non-response rate and maintain the proportionate sampling initially conducted.
3. Results
3.1 Demographic characteristics
The sample was comprised of slightly more females (51.6%); average age of the students was 19.92 ± 0.08 years. The majority was Lebanese (60.4%); an additional 26.9% held “dual citizenship”; about 13% were Arabs and other foreigners. About 65% reported that their grades were mostly 80’s or 90’s in the preceding semester; very few were failing (3.3%). The majority had no partner (87.9%). About 60% perceived themselves as well of as others their age, 10% a little/lot poorer, and 30% a little/lot richer. Students predominantly lived at home with their parents or family (spouse/children) (73.6%), but 13.4% reported living in an apartment (either alone or with a partner/roommate), and another 13% lived in dorms.
3.2. Medical and nonmedical use of prescription medications
3.2.1 Use of any prescription medications
Table 1 presents the weighted lifetime prevalence of each prescription medication use, both medically (i.e. based on a doctor’s prescription) and nonmedically (i.e. without a doctor’s prescription, or for longer periods than prescribed, or for nonmedical reasons). Psychoactive pain relievers rank the highest, and stimulants the lowest, both medically and non-medically (Table 1). The ratio of lifetime prevalence of nonmedical use to medical use of each prescription drug was 0.89 for sleeping pills, 0.56 for anxiety medications, 0.41 for pain relievers, and only in the case of stimulants did nonmedical use surpass that of medical (1.34) (Table 1).
Table 1.
Weighted lifetime medical and nonmedical use of psychoactive prescription medications by demographic characteristic of a sample of American University of Beirut students (n=570)
| Sleeping medications | Anxiety medications | Stimulant medications | Pain medications | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Med. N (%) | p | Non-med. N (%) | p | Med. N (%) | p | Non-med. N (%) | p | Med. N (%) | p | Non-med. N (%) | P | Med. N (%) | p | Non-med. N (%) | p | |
| Overall | 34 (6.52) | 34 (5.81) | 49 (8.25) | 28 (4.59) | 11 (2.60) | 19 (3.49) | 226 (36.89) | 89 (15.12) | ||||||||
|
| ||||||||||||||||
| Gender | ||||||||||||||||
| Male | 12 (5.65) | 0.517 | 10 (3.93) | 0.082 | 19 (9.32) | 0.363 | 8 (3.51) | 0.257 | 8 (4.27) | 0.081 | 9 (4.42) | 0.273 | 84 (32.98) | 0.085 | 27 (11.86) | 0.053 |
| Female | 21 (7.19) | 24 (7.88) | 28 (6.96) | 20 (5.86) | 3 (1.23) | 9 (2.54) | 137 (40.91) | 61 (18.75) | ||||||||
| Nationality | ||||||||||||||||
| Lebanese | 16 (5.36) | 0.289 | 12 (3.15) | 0.010 | 31 (8.53) | 0.094 | 18 (4.38) | 0.655 | 4 (1.88) | 0.331 | 6 (2.57) | 0.362 | 136 (36.25) | 0.851 | 51 (13.05) | 0.143 |
| Lebanese and other (“dual citizenship”) | 11 (7.17) | 14 (9.91) | 9 (4.94) | 8 (5.91) | 6 (4.59) | 8 (4.54) | 55 (35.50) | 30 (20.72) | ||||||||
| Foreign (Arab/other) | 7 (10.93) | 8 (10.03) | 9 (14.37) | 2 (3.05) | 1 (1.91) | 5 (5.72) | 32 (39.65) | 8 (13.76) | ||||||||
| Marital status* | ||||||||||||||||
| No partner | 24 (5.16) | 0.002 | 30 (5.87) | 0.924 | 39 (7.54) | 0.135 | 23 (4.32) | 0.418 | 10 (2.94) | < 0.001 | 17 (3.64) | 0.660 | 190 (35.36) | 0.133 | 79 (15.69) | 0.414 |
| With a partner | 10 (16.64) | 4 (5.55) | 10 (13.71) | 5 (6.81) | 1 (0.18) | 2 (2.48) | 34 (45.67) | 10 (11.33) | ||||||||
| SES | ||||||||||||||||
| A little/lot poorer than most | 3 (7.71) | 0.438 | 4 (9.79) | 0.113 | 6 (15.41) | 0.202 | 5 (10.88) | 0.040 | 1 (3.04) | 0.312 | 4 (9.63) | 0.054 | 25 (47.58) | 0.275 | 13 (25.38) | 0.081 |
| About the same as most | 18 (5.32) | 14 (3.96) | 27 (7.21) | 15 (2.89) | 5 (1.62) | 8 (2.31) | 132 (36.12) | 45 (12.72) | ||||||||
| A little/lot richer than most | 13 (8.70) | 16 (8.29) | 16 (8.26) | 8 (5.97) | 5 (4.45) | 7 (3.90) | 66 (34.63) | 31 (16.91) | ||||||||
| Living arrangement** | ||||||||||||||||
| Dorms | 3 (4.79) | 0.006 | 4 (6.77) | 0.650 | 3 (5.99) | 0.025 | 1 (0.93) | 0.210 | 1 (2.29) | 0.957 | 1 (0.38) | 0.003 | 34 (46.2) | 0.073 | 14 (18.93) | 0.148 |
| At home, with family | 20 (5.15) | 22 (5.31) | 34 (7.05) | 22 (5.34) | 8 (2.52) | 11 (3.00) | 166 (37.08) | 68 (15.94) | ||||||||
| In an apartment | 10 (16.18) | 7 (8.11) | 11 (17.68) | 4 (4.39) | 1 (1.83) | 7 (9.57) | 21 (26.30) | 6 (7.48) | ||||||||
No partner includes either single or divorced; with a partner includes either in a serious relationship, or engaged, or married.
In an apartment either alone or with a partner/roommate
p: p-value generated using Pearson’s Chi-square test; significance level is set at α = 0.05;
Med.: Medical use defined as use based on a doctor’s prescription note
Non-med.: Nonmedical use defined as use without a doctor’s note prescription or for longer periods than prescribed or for reasons other than what the medication is intended for
Further analyses showed that about 2 in 5 (43.0%) of AUB students reported lifetime medical use of any of the surveyed prescription drugs, and 1 in 4 (25.2%) in the preceding year. Specifically, 33.6% of the sample has used one type of medication, 7.7% have used two types and 1.6% reported use of three types of medications in their lifetime. With regards to nonmedical use, approximately 1 in 5 (21.6%) students admitted to ever using any prescription medication (14.6% in the past year). Particularly, 16.2% have used one type of medication nonmedically, 3.2% have used two types, and 1.7% of the students nonmedically used three/four types in their lifetime.
3.2.2 Demographic differences
As shown in Table 1, no statistically significant gender differences were observed across all medications, though the proportion of users was generally higher in females except for stimulants. Nationality was significantly correlated with nonmedical use of sleeping medications (lowest proportions reported in Lebanese) (Table 1). Marital status was significantly related to lifetime medical use of sleeping (higher in those with a partner) and stimulant medications (higher in youth with no partner). Moreover, perceived SES was significantly associated with nonmedical use of anxiety medications (highest proportions among “a little/lot poorer than most”) (Table 1). Students living in an apartment (alone or with a partner/roommate) were also significantly more likely to report medical use of sleeping and anxiety medications and nonmedical use of stimulants (Table 1).
3.2.3 Mutually exclusive groups of prescription drug users
Table 2 suggests that very few students reported “nonmedical use only” across all four medications (lifetime: 2.5%-4.7%; past year: 1.2%-3.3%). Even in the case of the most commonly reported medication (i.e. pain), most students reported ever taking the drug for medical purposes only, followed by medical and nonmedical use, and last for nonmedical use only (Table 2).
Table 2.
Weighted lifetime and past-year use of psychoactive prescription drugs among a sample of American University of Beirut students (n=570)
| Lifetime | Past-year | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Non-user | Medical use only | Nonmedical use only | Medical and Nonmedical use* | Non-user | Medical use only | Nonmedical use only | Medical and Nonmedical use* | |
|
| ||||||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Sleeping | 506 (89.22) | 24 (4.97) | 26 (4.73) | 8 (1.08) | 521 (94.53) | 10 (2.21) | 16 (3.26) | 0 |
| Anxiety | 497 (89.41) | 36 (5.99) | 16 (2.50) | 12 (2.10) | 507 (94.15) | 19 (3.43) | 8 (1.15) | 5 (1.27) |
| Stimulant | 534 (94.90) | 7 (1.62) | 15 (2.46) | 4 (1.03) | 539 (97.47) | 2 (0.33) | 10 (1.90) | 1 (0.31) |
| Pain | 312 (58.86) | 158 (26.02) | 22 (3.75) | 67 (11.38) | 353 (77.50) | 69 (14.22) | 14 (2.53) | 28 (5.76) |
Respondents who had missing responses on either medical or nonmedical use were excluded
3.3 Sources of obtaining prescription medications among nonmedical users
Lifetime nonmedical use of any prescription drug was reported by 21.6% (n = 126) of the sample. Figure 1 illustrates the top five sources for these medications, within each drug category. The leading reported source(s) were parent(s) (in all medications but stimulants), followed by pharmacists without a prescription note (for sleeping and pain), and doctors (for anxiety) (Figure 1). Friends (both AUB and non-AUB) were important sources for nonmedical stimulant users (Figure 1).
Figure 1.
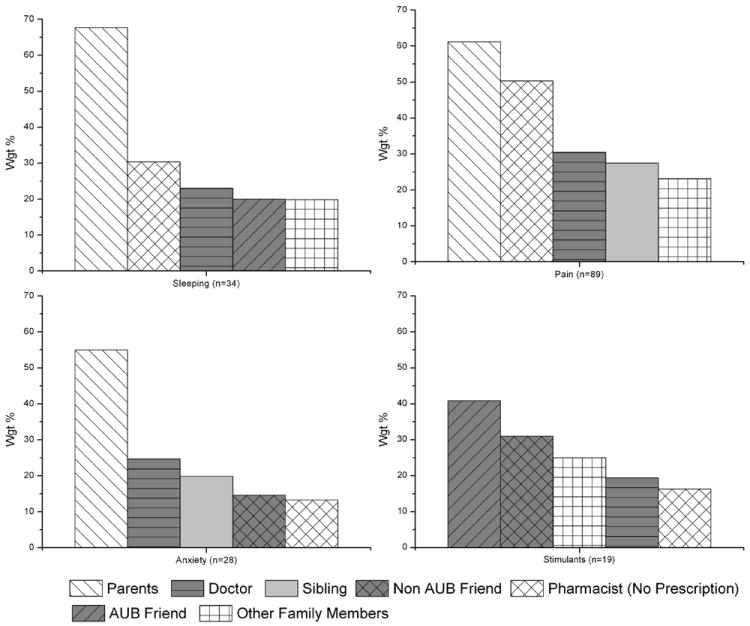
Weighted estimates of the top 5 reported sources of psychoactive prescription drugs among lifetime nonmedical users of each drug class among American University of Beirut students
3.4 Reported reasons among nonmedical users
As noted in Figure 2, the leading and most commonly reported reasons for nonmedical use fell under the intended purpose (highlighted in darker grey), true for all medications. More specifically, sleeping medications were mainly used to help in sleep and decrease anxiety; anxiety medications were mainly used to decrease anxiety and to help in sleep; stimulants were used to help students concentrate, increase alertness, or help in studying; and finally, pain medications were used to relieve pain and help in sleep (Figure 2).
Figure 2.
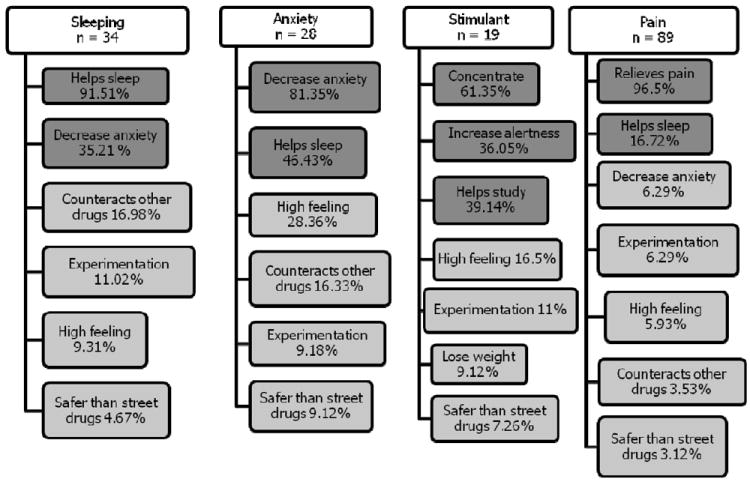
Weighted estimates of reported reasons for use of psychoactive prescription medications among lifetime nonmedical users of each drug class in descending order Darker grey background: Intended purpose of medication; lighter grey background: Non-intended purpose of medication.
Preliminary data indicate that intentions to use may not only vary by class of medication, but also by source of obtaining the medication within each class (Figure 3). For instance, those who reported obtaining their medications from their parents mostly used them the intended medical purpose (true for sleeping, anxiety, and pain). This is contrast to stimulants, whereby users whose sources were a doctor or a pharmacist were more likely to use it for its intended purpose only, as opposed to those who obtained them from friends (AUB or outside), and family members (other than parents) (Figure 3).
Figure 3.
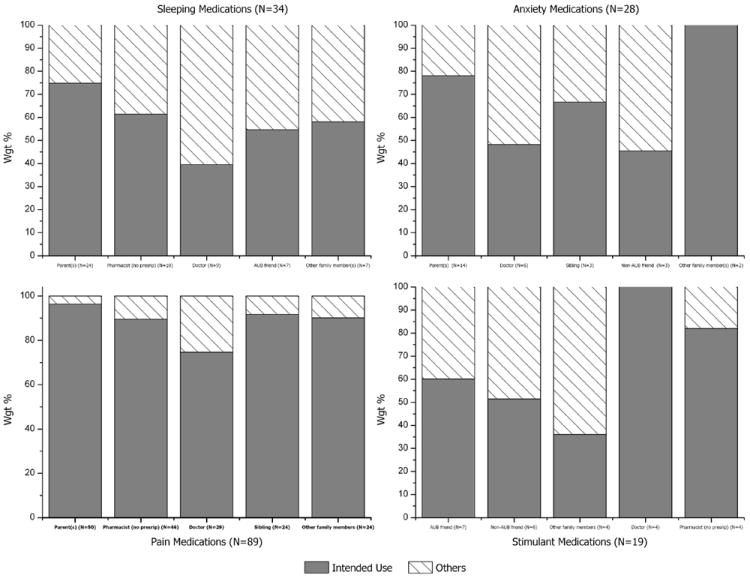
Weighted estimates of intended* motives for use (darker grey) of psychoactive prescription medications by source among nonmedical lifetime users of each drug class (*Sleeping and anxiety medications: helps sleep, decrease anxiety; stimulants: increased concentration/alertness, helps study; pain medications: relieves pain, helps sleep)
3.5 Diversion of prescription medications among medical users
Among students who reported being prescribed any of the medications at least once in their lifetime (43.0% of the sample, n=254), about 1 in 4 (18.9%, n=51) reported ever having been approached to divert at least one of their prescription drugs. The range of diversion across the four classes of medications was 15.2% - 48.9%, lowest for pain and highest for stimulants. Interestingly, further analyses showed that males were approached mostly to divert stimulants versus anxiety pills in females.
3.6 Perceived availability of the medications
The majority of the total sample of students reported that it would be easy/very easy to obtain prescription drugs without a prescription if they wanted some: pain relievers (63.4%), sleeping (55.2%), anxiety (43.4%), and stimulants (33.4%).
3.7 Substance use correlates
Slightly more than half of the sample reported past year use of alcohol (n=300, 55.5%), and almost half of those (n=133, 45.4%) reported drinking 1 or 2 times per week or more. Moreover, 50.1% reported at least one DSM-IV alcohol abuse symptom (keeping in mind that 74 students were missing on all criteria; 23.9% of the total sample). Nonmedical users of any psychoactive drug (but not medical users) were at a significantly higher odds of alcohol abuse compared to non-users (OR: 3.11, 95% Confidence Interval (CI): 1.43, 6.76; p-value: 0.004)
Almost 1 in 5 (19.38%, n=107) reported lifetime marijuana use (only 3 students reported other illegal drug use excluding marijuana). Both medical users and nonmedical users of any psychoactive medication were more likely to report lifetime marijuana use, greater odds observed among nonmedical users [medical use: OR: 1.78, 95% CI: 1.08, 2.92; p-value: 0.023; nonmedical use: OR: 3.28, 95% CI: 1.84, 5.83; p-value<0.001].
4. Discussion
This study, the first of its kind from the region, sheds light on the prevalence, patterns, and substance-use correlates of psychoactive prescription drug use in a university sample from Lebanon,. Despite global trends and concerns, there are no other local or regional published studies from the Arab world that investigate this timely issue in such breadth. This creates a truly missed opportunity for conducting cross-national comparisons within the Middle East region, but would hopefully stir regional substance use researchers in this direction.
The findings suggest that a considerable proportion of youth in Lebanon (about 20%, 95% CI: 18%, 26%) may be taking psychoactive prescription medications without medical supervision. Though used mostly for the intended medical purpose, this behavior is not entirely risk-free (Boyd et al., 2009). From a medical point of view, these users are not receiving the needed counseling; may be experiencing increased side-effects, contraindications, and perceived treatment ineffectiveness (Goldsworthy et al., 2008).
Pain relievers were the most commonly abused prescription drugs in our study, a finding that corroborates international findings among youth in the US (McCabe et al., 2005) and Canada (Brands et al., 2010). Stimulant use among AUB students however was relatively low, compared to anxiety and sleeping pills. No gender differences across the four medications were observed however; this is similar to other studies reporting no differences (Blanco et al., 2007; Catalano et al., 2010), and in contrast to other who found a higher proportion in boys (Levine and Coupey, 2009), or girls (Simoni-Wastila et al., 2008). Cotto and her colleagues interestingly clarified that age may be a significant moderator, and that males may be more likely to use while females are at a higher risk of dependence (Cotto et al., 2010).
Nonmedical users in this sample, as in western cultures, are also at danger of abusing alcohol, and using illegal drugs (Garnier et al., 2009; Simoni-Wastila et al., 2008; Catalano et al., 2010; McCauley et al., 2010). In addition to the significant proportion of youth who admitted using these drugs to “get high”, 17 students in this study admitted to ingesting alcohol simultaneously with a psychoactive prescription drug (a behavior of well-known adverse health consequences).
In the absence of a doctor’s recommendation, the crucial question becomes: “where from do these students obtain prescription medications?” The top most reported sources in this study were parents, doctors, pharmacists (without a prescription), and friends (particularly in the case of stimulants), similar to that reported by youth in other cultures (McCabe et al., 2005; Levine and Coupey, 2009). These findings highlight the need to target multiple various sources. Highest on the list are parents (except for stimulants), whether the supply is direct or indirect by leaving prescription drugs unattended at home (Solberg, 2008). Perhaps, the greater ‘social acceptance’ for using these medications is another contributing factor to their misuse. It is worth noting here that public marketing of medications in Lebanon is prohibited (World Health Organization, 2007), and online purchase of medications is uncommon.
Pharmacists (without a doctor’s prescription) were among the top 5 sources of obtaining these medications in this survey (second-most commonly reported source for sleeping and pain medications). In Lebanon, there are about 1923 registered community pharmacies, each serving an average of 2000 people (World Health Organization, 2007). Since 2003, stricter measures have been taken to prevent any drug sales without a doctor’s prescription, but the implementation of the laws remains questionable. If regulations were truly being enforced, pharmacists (without a prescription) would not have arisen as one of the leading sources of medication.
Doctors, as shown in this study, may be potentially contributing to the increased availability of and accessibility to these psychoactive prescription medications. While the mechanisms remain unclear, it is possible that physicians who are family members or family friends may be an outlet. In a country where the health care system is not centralized, one physician may also be unaware of another’s prescription note, potentially leading to multiple simultaneous prescriptions. Diversion is also a potential source for misuse; 20% of the lifetime medical users in this study diverted their medication, similar to other settings (22.9%) (Haydon et al., 2005; Goldsworthy et al., 2008).
Irrespective of the source, a considerable proportion of students in this sample perceive access to such drugs as easy/very easy (33%-63%), higher than what was reported earlier (2001) among private high school students from Lebanon (23%-44%) (Karam et al., 2003). Ultimately, a holistic approach to addressing the issue of availability and accessibility would have to involve the collective involvement of all stakeholders, including pharmacists, health professionals, families, and medical consumers.
Youth who self-medicate require close attention, and may need to be approached differently. This is particularly relevant in cultures where pharmacists may sell psychoactive drugs without a prescription, as they struggle between providing medical advice and service to those who cannot afford a doctor’s note and meeting the requirements of the regulations enacted by their government (Hurwitz, 2005; Kheir et al., 2008). It is expected that national authorities ensure the availability of accessible, affordable means of treatment and coping strategies while enforcing the rules and regulations (Dib et al., 2004).
Despite its importance, the study is not void of limitations, including, recall bias given its cross-sectional nature and underreporting of important information (e.g., age of onset of use); missing ages of onset impeded further the exploration of conversion from medical to nonmedical use. Lack of representativeness to other non-AUB youth despite AUB’s heterogeneous student population is also a drawback. While probably comparable other private universities, our results may not be applicable to peers attending public universities, or even non-college youth. The focus on AUB students stemmed from the limited financial and time constraints (the funding being a one-year limited grant).
All things considered, the present study has generated markedly important findings, providing an informative perspective on the problem, and corroborating (for the most part) behaviors among youth elsewhere – thus, giving us less reason to believe that the situation would be drastically different in other university populations in Lebanon. Still, further research studies, particularly investigating underlying risk factors that may be particular to Lebanon (e.g., wars, internal strife, and economic difficulties) are strongly encouraged.
Coupled with more recent anecdotal reports (Solberg, 2008), the findings are essential for shaping current policies and prevention practices, and informing the design of future research endeavors. For instance, we found that the definition of nonmedical use, as defined in this and other studies, (Kroutil et al., 2006; McCabe et al., 2006) is far from ideal. The definition as it stands includes notions of legality versus illegality (use with or without a doctor’s prescription), tolerance (use for longer periods than prescribed), sources of drugs (prescribed for somebody else), and motivations for use (to get high). Clearly, these are not mutually exclusive groups of users as someone may be using medication that is intended for somebody else for its intended purpose, or to get high; while both groups face health risks, one may be self-medicating for financial reasons, and another may be involved in poly-drug use, and each must be approached differently. Clearer more accurate definitions are thus needed, as stressed by other colleagues (Compton and Volkow, 2006).
Overall, our findings highlight the pressing need for (1) increased parental awareness on the potential dangers of psychoactive prescription drug use; and (2) reinforcement of the laws and regulations relevant to pharmacists and other health care providers. On the research-level, a qualitative study may prove instrumental in further understanding prescription drug use behaviors among youth in Lebanon, and shaping future quantitative research instruments as part of larger, more comprehensive studies.
In conclusion, despite distinct cultures and regulatory restrictions, our study corroborated on several grounds findings from the US and Canada, with regards to the most commonly abused medications (i.e. opioid pain relievers), sources (i.e. parents, peers), diversion estimates (about 20%), and increased likelihood of abuse of other substances (e.g., alcohol, marijuana). More so, nonmedical users in Lebanon as in other parts of the world seem to use the drug largely for its intended purpose, rendering ‘self-medication’ a global phenomenon and concern. Furthermore, the literature on gender differences is inconclusive, and our study supports those that could not delineate any statistically significant variations.
Clearly, the present study provides a unique opportunity to compare youth behaviors from different cultures, while highlighting important contextual differences and local particularities needed for further local research, and evidence-based policy and practice.
Acknowledgments
The authors would like to extend their gratitude and appreciation to Dr. Sean Esteban McCabe at University of Michigan for sharing with us the instrument administered as part of the Student Life Survey. We would also like to thank Ms. Reem Saad, Eleine Khoury, and Lynn Itani for their invaluable assistance in data collection, and of course the University Research Board at the American University of Beirut for funding the research study.
References
- Blanco C, Alderson D, Ogburn E, Grant BF, Nunes EV, Hatzenbuehler ML, Hasin DS. Changes in the prevalence of non-medical prescription drug use and drug use disorders in the United States: 1991-1992 and 2001-2002. Drug Alcohol Depend. 2007;90:252–260. doi: 10.1016/j.drugalcdep.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Boyd CJ, Esteban McCabe S, Teter CJ. Medical and nonmedical use of prescription pain medication by youth in a Detroit-area public school district. Drug Alcohol Depend. 2006;81:37–45. doi: 10.1016/j.drugalcdep.2005.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE, Cranford JA, Young A. Prescription drug abuse and diversion among adolescents in a southeast Michigan school district. Archives of Pediatrics and Adolescent Medicine. 2007;161:276. doi: 10.1001/archpedi.161.3.276. [DOI] [PubMed] [Google Scholar]
- Boyd CJ, Young A, Grey M, McCabe SE. Adolescents’ nonmedical use of prescription medications and other problem behaviors. Journal of Adolescent Health. 2009;45:543–550. doi: 10.1016/j.jadohealth.2009.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brands B, Paglia-Boak A, Sproule BA, Leslie K, Adlaf EM. Nonmedical use of opioid analgesics among Ontario students. Canadian Family Physician. 2010;56:256. [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, White HR, Fleming CB, Haggerty KP. Is nonmedical prescription opiate use a unique form of illicit drug use? Addict Behav. 2010 doi: 10.1016/j.addbeh.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81:103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Cotto JH, Davis E, Dowling GJ, Elcano JC, Staton AB, Weiss SRB. Gender effects on drug use, abuse, and dependence: A special analysis of results from the national survey on drug use and health. Gender medicine. 2010;7:402–413. doi: 10.1016/j.genm.2010.09.004. [DOI] [PubMed] [Google Scholar]
- Dib JG, Saade S, Merhi F. Pharmacy Practice in Lebanon. American journal of health-system pharmacy. 2004;61:794. doi: 10.1093/ajhp/61.8.794. [DOI] [PubMed] [Google Scholar]
- El-Aneed A, Alaghehbandan R, Gladney N, Collins K, MacDonald D, Fischer B. Prescription drug abuse and methods of diversion: The potential role of a pharmacy network. J Subst Use. 2009;14:75–83. [Google Scholar]
- Figueiras A, Caamano F, Gestal-Otero JJ. Sociodemographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16:19–26. doi: 10.1023/a:1007608702063. [DOI] [PubMed] [Google Scholar]
- Fischer B, Rehm J. Nonmedical use of prescription opioids: furthering a meaningful research agenda. The Journal of Pain. 2008;9:490–493. doi: 10.1016/j.jpain.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Friedman RA. The changing face of teenage drug abuse—the trend toward prescription drugs. N Engl J Med. 2006;354:1448–1450. doi: 10.1056/NEJMp068010. [DOI] [PubMed] [Google Scholar]
- Garnier LM, Arria AM, Caldeira KM, Vincent KB, O’Grady KE, Wish ED. Nonmedical prescription analgesic use and concurrent alcohol consumption among college students. Am J Drug Alcohol Abuse. 2009;35:334–338. doi: 10.1080/00952990903075059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsworthy RC, Schwartz NC, Mayhorn CB. Beyond abuse and exposure: framing the impact of prescription-medication sharing. Am J Public Health. 2008;98:1115. doi: 10.2105/AJPH.2007.123257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison L. The validity of self-reported drug use in survey research: an overview and critique of research methods. The validity of self-reported drug use: Improving the accuracy of survey estimates. 1997:17–36. [PubMed] [Google Scholar]
- Haydon E, Rehm J, Fischer B, Monga N, Adlaf E. Prescription drug abuse in Canada and the diversion of prescription drugs into the illicit drug market. Canadian journal of public health. 2005;96:459–461. doi: 10.1007/BF03405190. Commentary. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurwitz W. The challenge of prescription drug misuse: A review and commentary. Pain Medicine. 2005;6:152–161. doi: 10.1111/j.1526-4637.2005.05024.x. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Bachman JG, Schulenberg JE. Overview of Key Findings, 2007. Vol. 76 National Institute on Drug Abuse (NIDA); 2008. Monitoring the Future: National Results on Adolescent Drug Use. [Google Scholar]
- Johnston LD, O’malley PM. The recanting of earlier reported drug use by young adults. NIDA Res Monogr. 1997;167:59–80. [PubMed] [Google Scholar]
- Johnston LD. Prescription drug use by adolescents: what we are learning and what we still need to know. J Adolesc Health. 2009;45:539–540. doi: 10.1016/j.jadohealth.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Karam E, Melhem N, Mansour C, Maalouf W, Saliba S, Chami A. Use and abuse of licit and illicit substances: prevalence and risk factors among students in Lebanon. Eur Addict Res. 2000;6:189–197. doi: 10.1159/000052045. [DOI] [PubMed] [Google Scholar]
- Karam EG, Ghandour L, Maalouf W, Yamout K. Substance use and misuse in Lebanon: the Lebanon Rapid Situation Assessment and Response Study. UNODC Report 2003 [Google Scholar]
- Kheir N, Zaidan M, Younes H, El Hajj M, Wilbur K, Jewesson PJ. Pharmacy education and practice in 13 Middle Eastern countries. Am J Pharm Educ. 2008;72 doi: 10.5688/aj7206133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroutil LA, Van Brunt DL, Herman-Stahl MA, Heller DC, Bray RM, Penne MA. Nonmedical use of prescription stimulants in the United States. Drug Alcohol Depend. 2006;84:135–143. doi: 10.1016/j.drugalcdep.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Kuehn BM. Prescription drug abuse rises globally. JAMA: The Journal of the American Medical Association. 2007;297:1306. doi: 10.1001/jama.297.12.1306. [DOI] [PubMed] [Google Scholar]
- Kuehn BM. Shift seen in patterns of drug use among teens. JAMA: the journal of the American Medical Association. 2006;295:612. doi: 10.1001/jama.295.6.612. [DOI] [PubMed] [Google Scholar]
- Levine SB, Coupey SM. Nonmedical use of prescription medications: an emerging risk behavior among rural adolescents. Journal of Adolescent Health. 2009;44:407–409. doi: 10.1016/j.jadohealth.2008.08.010. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ. Sources of prescription drugs for illicit use. Addict Behav. 2005;30:1342–1350. doi: 10.1016/j.addbeh.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Cranford JA, Teter CJ. Motives for nonmedical use of prescription opioids among high school seniors in the United States: self-treatment and beyond. Archives of Pediatrics and Adolescent Medicine. 2009;163:739. doi: 10.1001/archpediatrics.2009.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ, Teter CJ. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict Behav. 2007;32:562–575. doi: 10.1016/j.addbeh.2006.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Illicit use of prescription pain medication among college students. Drug Alcohol Depend. 2005;77:37–47. doi: 10.1016/j.drugalcdep.2004.07.005. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, and diversion of abusable prescription drugs. Journal of American College Health. 2006;54:269–278. doi: 10.3200/JACH.54.5.269-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ, Knight JR, Wechsler H. Nonmedical use of prescription opioids among US college students: Prevalence and correlates from a national survey. Addict Behav. 2005;30:789–805. doi: 10.1016/j.addbeh.2004.08.024. [DOI] [PubMed] [Google Scholar]
- McCauley JL, Danielson CK, Amstadter AB, Ruggiero KJ, Resnick HS, Hanson RF, Smith DW, Saunders BE, Kilpatrick DG. The role of traumatic event history in non-medical use of prescription drugs among a nationally representative sample of US adolescents. Journal of Child Psychology and Psychiatry. 2010;51:84–93. doi: 10.1111/j.1469-7610.2009.02134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassar NT, Melikian LH, Der-Karabetian A. Studies in the non medical use of drugs in Lebanon. I. The non medical use of marijuana, LSD, and amphetamine by students at the American University of Beirut. J Med Liban. 1973;26:215–232. [PubMed] [Google Scholar]
- RTI International, United States, SAMHSA, Office of Applied Studies, United States. Results From the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings 2010 [Google Scholar]
- Simoni-Wastila L, Yang HWK, Lawler J. Correlates of prescription drug nonmedical use and problem use by adolescents. Journal of Addiction Medicine. 2008;2:31. doi: 10.1097/ADM.0b013e31815b5590. [DOI] [PubMed] [Google Scholar]
- Solberg KE. Lebanese turn to drugs to treat mental-health problems. The Lancet. 2008;372:1137–1138. doi: 10.1016/s0140-6736(08)61463-4. [DOI] [PubMed] [Google Scholar]
- Volkow ND. Prescription Drugs Abuse and Addiction 2005 [Google Scholar]
- World Health Organization. Measuring Transparency to Improve Good Governance in the Public Pharmaceutical Sector 2007 [Google Scholar]
- Zarocostas J. Misuse of prescription drugs could soon exceed that of illicit narcotics, UN panel warns. BMJ: British Medical Journal. 2007;334:444. doi: 10.1136/bmj.39140.394410.DB. [DOI] [PMC free article] [PubMed] [Google Scholar]


