Abstract
Aims
Canagliflozin is a sodium glucose co-transporter 2 inhibitor in development for treatment of type 2 diabetes mellitus (T2DM). This study evaluated the efficacy and safety of canagliflozin in subjects with T2DM and stage 3 chronic kidney disease [CKD; estimated glomerular filtration rate (eGFR) ≥30 and <50 ml/min/1.73 m2].
Methods
In this randomized, double-blind, placebo-controlled, phase 3 trial, subjects (N = 269) received canagliflozin 100 or 300 mg or placebo daily. The primary efficacy endpoint was change from baseline in HbA1c at week 26. Prespecified secondary endpoints were change in fasting plasma glucose (FPG) and proportion of subjects reaching HbA1c <7.0%. Safety was assessed based on adverse event (AE) reports; renal safety parameters (e.g. eGFR, blood urea nitrogen and albumin/creatinine ratio) were also evaluated.
Results
Both canagliflozin 100 and 300 mg reduced HbA1c from baseline compared with placebo at week 26 (–0.33, –0.44 and –0.03%; p < 0.05). Numerical reductions in FPG and higher proportions of subjects reaching HbA1c < 7.0% were observed with canagliflozin 100 and 300 mg versus placebo (27.3, 32.6 and 17.2%). Overall AE rates were similar for canagliflozin 100 and 300 mg and placebo (78.9, 74.2 and 74.4%). Slightly higher rates of urinary tract infections and AEs related to osmotic diuresis and reduced intravascular volume were observed with canagliflozin 300 mg compared with other groups. Transient changes in renal function parameters that trended towards baseline over 26 weeks were observed with canagliflozin.
Conclusion
Canagliflozin improved glycaemic control and was generally well tolerated in subjects with T2DM and Stage 3 CKD.
Keywords: type 2 diabetes, sodium glucose co-transporter 2 (SGLT2) inhibitor, diabetic nephropathy
Introduction
Progression of chronic kidney disease (CKD), leading to end-stage renal failure, is a common complication in patients with type 2 diabetes mellitus (T2DM) 1. Antihyperglycaemic agent (AHA) treatment options are limited as a number of classes of agents may have decreased efficacy and be associated with increased risk of adverse effects in patients with CKD 2. For example, there are labelled restrictions on the use of thiazolidinediones, metformin, sulphonylureas, and, more recently, glucagon-like peptide-1 (GLP-1) agonists in this cohort 3,4. Moreover, AHAs commonly used in this population, such as sulphonylureas, have been associated with an increased risk of hypoglycaemia and weight gain 3–5. Thus, new treatment options are needed for this growing population of patients with co-existing T2DM and renal insufficiency 1.
Canagliflozin is an inhibitor of the sodium glucose co-transporter 2 (SGLT2) in development for the treatment of patients with T2DM. Canagliflozin lowers the renal threshold for glucose (RTG) and increases urinary glucose excretion (UGE), resulting in decreased plasma glucose in patients with hyperglycaemia, as well as a mild osmotic diuresis and a net caloric loss (by loss of glucose) promoting weight loss 6–10. Because the rate of UGE is proportional to the glomerular filtration rate (GFR) (as well as to the blood glucose concentration) 7,8,11, the effect of canagliflozin to augment UGE would be anticipated to be diminished in subjects with CKD. Therefore, the efficacy of canagliflozin in improving glycaemic control and reducing body weight may be affected in this subject population. In addition to assessing the efficacy response to canagliflozin in this population, it is also important to assess the safety and tolerability profile of SGLT2 inhibition in subjects with CKD.
This phase 3 study evaluated the efficacy and safety of canagliflozin compared with placebo in subjects with inadequately controlled T2DM and stage 3 CKD. This study included subjects with a lower, more restricted estimated glomerular filtration rate (eGFR) range of ≥30 and <50 ml/min/1.73 m2 based upon the modification of diet in renal disease (MDRD) equation 12, compared with the typical eGFR range for stage 3 CKD of ≥30 and <60 ml/min/1.73 m2 .
Materials and Methods
Study Design and Subjects
This 52-week, randomized, double-blind, placebo-controlled, phase 3 study was conducted at 89 centres in 19 countries and consisted of an AHA adjustment period (if required; consisting of a dose titration period of up to 4 weeks and an 8-week dose stable period); a 2-week, single-blind, placebo run-in period; a 26-week, double-blind, core treatment period; and a 26-week, double-blind, extension period (data to be reported in a separate publication). Eligible subjects were men and women aged ≥25 years with T2DM who had inadequate glycaemic control (HbA1c ≥7.0 and ≤10.5%) and stage 3 CKD (eGFR ≥30 and <50 ml/min/1.73 m2), and were either not on AHA therapy or were on a stable AHA regimen (monotherapy or combination therapy with any approved agent including metformin, sulphonylurea, dipeptidyl peptidase-4 (DPP-4) inhibitor, α-glucosidase inhibitor, GLP-1 analogue, pioglitazone or insulin) for ≥8 weeks (≥12 weeks with pioglitazone) prior to the week –2 visit. Subjects were required to have generally stable renal function, as determined by a ≤25% decrease in eGFR from the screening to the week –2 visits. Subjects on AHA regimens not consistent with local prescribing guidelines (e.g. metformin therapy) underwent an AHA adjustment period of up to 12 weeks before the placebo run-in period. Subjects were to remain on their stable AHA regimens through the completion of the 52-week treatment period (unless glycaemic rescue criteria were met, as discussed below).
Subjects were excluded if they had repeated fasting plasma glucose (FPG) >15.0 mmol/l (270 mg/dl) during the pretreatment phase; a history of T1DM; renal disease that required immunosuppressive therapy, dialysis or transplant; nephrotic syndrome or inflammatory renal disease; New York Heart Association Class III-IV cardiovascular disease; myocardial infarction, unstable angina, revascularization procedure or cerebrovascular accident within 3 months prior to screening; or haemoglobin concentration <100 g/l (10 g/dl) at screening.
The study protocol and amendments were approved by the institutional review boards at participating institutions and the study was conducted under the guidelines of Good Clinical Practices and the Declaration of Helsinki. All subjects provided written informed consent prior to participation.
Randomization and Study Treatments
Eligible subjects were randomly assigned to receive once-daily oral doses of canagliflozin 100 or 300 mg or placebo in a 1 : 1 : 1 ratio using an Interactive Voice Response System/Interactive Web Response System. Randomization was balanced by using permuted blocks of six subjects per block and stratified based on (i) the presence or absence of atherosclerotic cardiovascular disease (e.g. history of myocardial infarction, documented angina, transient ischemic attack or stroke or peripheral vascular disease) and (ii) whether a subject required an AHA adjustment period prior to randomization.
During the double-blind, core treatment period, glycaemic rescue therapy (up-titration of current AHAs or step-wise addition of oral or non-oral AHAs) was initiated if FPG >15.0 mmol/l (270 mg/dl) after day 1 to week 6, >13.3 mmol/l (240 mg/dl) after week 6 to week 12, and >11.1 mmol/l (200 mg/dl) after week 12 to week 26. After randomization, HbA1c and FPG values were masked to the study centres unless these values met the prespecified glycaemic criteria for the initiation of rescue medication or after glycaemic rescue medication was started.
Study Endpoints and Assessments
The prespecified primary efficacy endpoint was the change from baseline in HbA1c at week 26. Prespecified secondary efficacy endpoints evaluated at week 26 were the proportion of subjects reaching HbA1c <7.0% and change from baseline in FPG. Other efficacy endpoints included change from baseline in blood pressure (BP) and percent change from baseline in body weight and fasting plasma lipids.
Overall safety and tolerability were assessed by adverse event (AE) reports, safety laboratory tests, vital sign measurements, physical examinations and 12-lead electrocardiograms. Selected AEs of interest, including genital mycotic infections and urinary tract infections (UTIs), were prespecified for additional data collection. Events of hypoglycaemia were collected using a separate case report form that collected concurrent fingerstick glucose values and the presence of symptoms indicating a severe event (i.e. requiring the assistance of another individual or resulting in seizure or loss of consciousness). Measures of renal function, including eGFR, serum creatinine, blood urea nitrogen (BUN) and urine albumin/creatinine ratio (ACR) were also assessed.
Statistical Analyses
Sample size calculation was based on demonstrating the superiority of canagliflozin to placebo, as measured by the change in HbA1c from baseline to week 26. An estimated 61 randomized subjects per group were needed to achieve ≥90% power, assuming a group difference of 0.5% and a common standard deviation (SD) of 0.85% (based on relevant information from patients with T2DM and renal impairment), and using a two-sample, two-sided t-test with a type I error rate of 0.05. In order to provide additional safety information for canagliflozin, this study planned a modestly greater sample size of 80 randomized subjects per treatment group (∼240 total subjects) for enrolment.
Efficacy analyses were conducted using the modified intent-to-treat (mITT) population, which consisted of all randomized subjects who received ≥1 dose of study drug, according to the randomized treatment assignment. The last observation carried forward (LOCF) approach was used to impute missing data. If subjects received rescue therapy, all postrescue data were censored and the last postbaseline value prior to the initiation of rescue therapy was used for analyses. Safety analyses were performed in randomized subjects who received ≥1 dose of study drug according to the predominant treatment received (the allocation of treatment assignment in the efficacy and safety analyses were the same as no subject took incorrect double-blind study drug for a predominant part of the double-blind treatment period).
Primary and continuous secondary efficacy endpoints were assessed using an analysis of covariance (ancova) model with treatment and stratification factors as fixed effects and corresponding baseline values and baseline eGFR as covariates. Least squares (LS) mean differences and two-sided 95% confidence intervals (CIs) were estimated based on this model for the comparison of each canagliflozin group versus placebo. The categorical secondary endpoint (proportion of subjects reaching HbA1c < 7.0%) was analyzed using a logistic model with treatment and stratification factors as fixed effects and baseline HbA1c and eGFR values as covariates. Renal safety parameters, including change in eGFR and ACR, were analyzed using an ancova model with treatment and stratification factors as fixed effects and adjusting for the baseline covariate. Differences in LS means between groups (each canagliflozin dose vs. placebo) and two-sided 95% CIs were estimated. All statistical tests were interpreted at a two-sided significance level of 5% and all CIs at a two-sided confidence level of 95%.
A closed testing of prespecified primary and secondary endpoints based on the treatment difference was implemented in order to preserve the overall type I error rate at 5%. The p values for the treatment comparisons were calculated and are reported for prespecified comparisons only. If a prespecified comparison was not found to be statistically significant, subsequent prespecified tests were not to be conducted; descriptive statistics (95% CI for between-group differences) are provided.
Results
Subject Disposition and Baseline Characteristics
Of the 272 randomized subjects, 269 received ≥1 dose of study drug and were included in the mITT analysis population (figure 1). A total of 35 (12.9%) subjects discontinued before the week 26 visit, with fewer discontinuations in the canagliflozin 300 mg group compared with the canagliflozin 100 mg and placebo groups. A smaller proportion of subjects treated with canagliflozin 100 or 300 mg received glycaemic rescue therapy before the week 26 visit compared with those treated with placebo (4.4, 3.3 and 14.3%, respectively). Baseline demographic and disease characteristics were similar across treatment groups (Table 1). Mean baseline HbA1c was 8.0%, mean age was 68.5 years and mean body mass index was 33.0 kg/m2; the mean duration of T2DM for subjects was 16.3 years. Mean baseline eGFR was 39.4 ml/min/1.73 m2 and median baseline ACR was 30.0 µg/mg. Approximately 80% of subjects had a history of ≥1 diabetic microvascular complication, with nephropathy being the most common complication. A total of 98% of subjects were on background AHA therapy at baseline, with insulin (74%) and sulphonylureas (31%) being the most common background therapies (Table 2). Most subjects were on antihypertensive therapy (Table 1), including agents acting on the renin-angiotensin system (87%), diuretics (73%), β-blocking agents (56%) and calcium channel blockers (42%).
Figure 1.
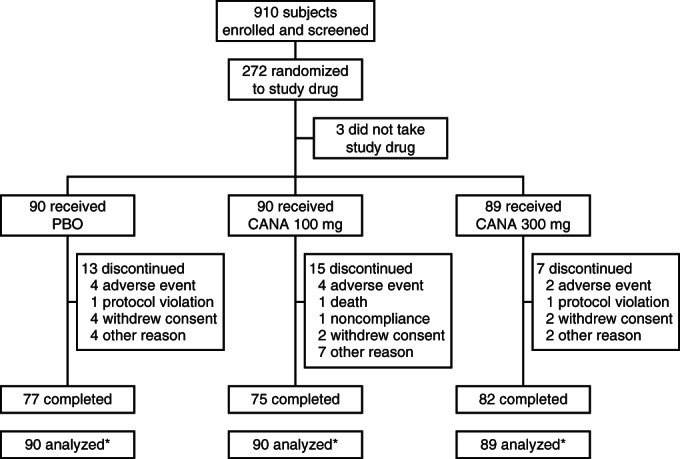
Study flow diagram. PBO, placebo; CANA, canagliflozin; mITT, modified intent-to-treat. *mITT analysis set.
Table 1.
Baseline demographic and disease characteristics*
| Characteristic | PBO (n = 90) | CANA 100 mg (n = 90) | CANA 300 mg (n = 89) | Total (N = 269) |
|---|---|---|---|---|
| Sex, n (%) | ||||
| Male | 57 (63.3) | 58 (64.4) | 48 (53.9) | 163 (60.6) |
| Female | 33 (36.7) | 32 (35.6) | 41 (46.1) | 106 (39.4) |
| Age, years | 68.2 ± 8.4 | 69.5 ± 8.2 | 67.9 ± 8.2 | 68.5 ± 8.3 |
| Race, n (%)† | ||||
| White | 78 (86.7) | 71 (78.9) | 66 (74.2) | 215 (79.9) |
| Black or African American | 0 | 3 (3.3) | 2 (2.2) | 5 (1.9) |
| Asian | 7 (7.8) | 9 (10.0) | 11 (12.4) | 27 (10.0) |
| Other‡ | 5 (5.6) | 7 (7.8) | 10 (11.2) | 22 (8.2) |
| HbA1c, % | 8.0 ± 0.9 | 7.9 ± 0.9 | 8.0 ± 0.8 | 8.0 ± 0.9 |
| FPG, mmol/l (mg/dl) | 8.9 ± 2.4 (160.4 ± 43.2) | 9.4 ± 2.6 (169.4 ± 46.3) | 8.8 ± 3.2 (158.6 ± 58.0) | 9.1 ± 2.8 (164.0 ± 49.6) |
| Body weight, kg | 92.8 ± 17.4 | 90.5 ± 18.4 | 90.2 ± 18.1 | 91.2 ± 18.0 |
| BMI, kg/m2 | 33.1 ± 6.5 | 32.4 ± 5.5 | 33.4 ± 6.5 | 33.0 ± 6.2 |
| Duration of T2DM, years | 16.4 ± 10.1 | 15.6 ± 7.4 | 17.0 ± 7.8 | 16.3 ± 8.5 |
| eGFR, ml/min/1.73 m2 | 40.1 ± 6.8 | 39.7 ± 6.9 | 38.5 ± 6.9 | 39.4 ± 6.9 |
| Median ACR, µg/mg | 31.3 | 23.7 | 30.1 | 30.0 |
| Microvascular complications, n (%) | 74 (82.2) | 73 (81.1) | 69 (77.5) | 216 (80.3) |
| Neuropathy | 45 (50.0) | 36 (40.0) | 38 (42.7) | 119 (44.2) |
| Retinopathy | 25 (27.8) | 27 (30.0) | 36 (40.4) | 88 (32.7) |
| Nephropathy | 61 (67.8) | 69 (76.7) | 65 (73.0) | 195 (72.5) |
| History of ASCVD, n (%) | 51 (56.7) | 50 (55.6) | 46 (51.7) | 147 (54.6) |
| Antihypertensive therapy at baseline, n (%) | ||||
| Agents acting on the renin-angiotensin system | 77 (85.6) | 79 (87.8) | 79 (88.8) | 235 (87.4) |
| Diuretics | 62 (68.9) | 65 (72.2) | 70 (78.7) | 197 (73.2) |
| β-blocking agents | 50 (55.6) | 51 (56.7) | 50 (56.2) | 151 (56.1) |
| Calcium channel blockers | 33 (36.7) | 40 (44.4) | 39 (43.8) | 112 (41.6) |
| Antihyperlipidemic therapy at baseline, n (%) | 70 (77.8) | 74 (82.2) | 68 (76.4) | 212 (78.8) |
PBO, placebo; CANA, canagliflozin; FPG, fasting plasma glucose; BMI, body mass index; T2DM, type 2 diabetes mellitus; eGFR, estimated glomerular filtration rate; ACR, albumin/creatinine ratio; ASCVD, atherosclerotic cardiovascular disease; SD, standard deviation.
Data are mean ± SD unless otherwise indicated.
Percentages may not total 100.0% due to rounding.
Includes American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, other and unknown.
Table 2.
AHA therapies at baseline (mITT)
| Subjects, n (%) | ||||
|---|---|---|---|---|
| PBO (n = 90) | CANA 100 mg (n = 90) | CANA 300 mg (n = 89) | Total (N = 269) | |
| Total subjects with AHA therapy | 88 (97.8) | 87 (96.7) | 88 (98.9) | 263 (97.8) |
| AHAs (alone or in combination) | ||||
| Sulphonylureas | 33 (36.7) | 24 (26.7) | 27 (30.3) | 84 (31.2) |
| Thiazolidinediones* | 7 (7.8) | 3 (3.3) | 7 (7.9) | 17 (6.3) |
| DPP-4 inhibitors | 5 (5.6) | 7 (7.8) | 8 (9.0) | 20 (7.4) |
| Biguanide | 1 (1.1) | 1 (1.1) | 2 (2.2) | 4 (1.5) |
| Other AHAs† | 7 (7.8) | 6 (6.7) | 10 (11.2) | 23 (8.6) |
| Insulin‡ | 66 (73.3) | 67 (74.4) | 66 (74.2) | 199 (74.0) |
| Combinations§ | ||||
| Sulphonylurea + insulin | 11 (12.2) | 7 (7.8) | 10 (11.2) | 28 (10.4) |
| Other AHA¶ + insulin | 12 (13.3) | 8 (8.9) | 10 (11.2) | 30 (11.2) |
| Biguanide + insulin | 0 | 1 (1.1) | 2 (2.2) | 3 (1.1) |
| Biguanide + sulphonylurea | 1 (1.1) | 0 | 0 | 1 (0.4) |
AHA, antihyperglycaemic agent; mITT, modified intent-to-treat; PBO, placebo; CANA, canagliflozin; DPP-4, dipeptidyl peptidase-4; GLP-1, glucagon-like peptide-1.
All subjects were on pioglitazone.
Including α-glucosidase inhibitors, GLP-1 agonists, glinides and other AHAs.
Including basal + bolus insulin, basal insulin alone and bolus insulin alone.
Subset of subjects on combinations of the AHAs listed above.
Including α-glucosidase inhibitors, thiazolidinediones, DPP-4 inhibitors, GLP-1 agonists, glinides and other AHAs.
Efficacy
Glycaemic Efficacy Endpoints
HbA1c was significantly reduced from baseline with canagliflozin 100 and 300 mg compared with placebo at week 26 (figure 2A). Differences in LS mean changes relative to placebo were –0.30% for canagliflozin 100 mg (p < 0.05) and –0.40% for canagliflozin 300 mg (p < 0.001). A numerically higher proportion of subjects treated with canagliflozin 100 or 300 mg than with placebo achieved HbA1c < 7.0% at week 26 (27.3, 32.6 and 17.2%, respectively; figure 2B). Canagliflozin 100 and 300 mg provided numerically greater reductions from baseline in FPG at week 26 compared with placebo (figure 2C), with differences in LS mean changes (95% CI) of –0.85 (–1.6, –0.1) and –0.67 (–1.4, 0.1) mmol/l [–15.4 (–28.5, –2.3) and –12.2 (–25.4, 1.0) mg/dl], respectively. The comparison of canagliflozin 300 mg versus placebo in change in FPG was not statistically significant and, therefore, the statistical comparison of canagliflozin 100 mg versus placebo did not proceed based on the closed testing procedure.
Figure 2.
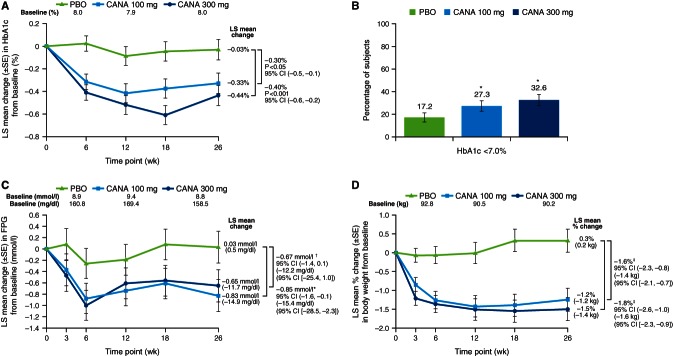
Effects on efficacy parameters (LOCF). Change in HbA1c (A), proportion of subjects reaching HbA1c <7.0% (B), change in FPG (C), and percent change in body weight (D). LOCF, last observation carried forward; FPG, fasting plasma glucose; PBO, placebo; CANA, canagliflozin; LS, least squares; SE, standard error; CI, confidence interval; NS, not significant. *Statistical comparison for CANA versus PBO not performed owing to multiplicity control. †p = NS for CANA versus PBO. ‡Statistical comparison for CANA versus PBO not performed (not prespecified).
Other Efficacy Endpoints
Canagliflozin 100 and 300 mg provided reductions from baseline in body weight over 26 weeks, whereas placebo was associated with a slight increase in body weight (figure 2D). Differences in LS mean percent changes (95% CI) relative to placebo at week 26 were –1.6% (–2.3, –0.8) and –1.8% (–2.6, –1.0) for canagliflozin 100 and 300 mg, respectively, corresponding to absolute changes of –1.4 and –1.6 kg, respectively.
Both canagliflozin 100 and 300 mg were associated with greater decreases from baseline in systolic and diastolic BP compared with placebo at week 26 (LS mean changes of –6.1, –6.4 and –0.3 mmHg, respectively, in systolic BP and –2.6, –3.5 and –1.4 mmHg, respectively, in diastolic BP; Table 3). No notable changes in pulse rate were observed with canagliflozin 100 or 300 mg compared with placebo (mean change of –1.9, –1.1 and –2.5 beats/min, respectively). Canagliflozin 100 and 300 mg increased high-density lipoprotein cholesterol (HDL-C) compared with placebo (LS mean percent changes of 4.0, 3.0 and 1.5%, respectively; Table 3). An increase in triglycerides (LS mean percent changes of 11.9, 6.2 and 7.9%, respectively) and a decrease in low-density lipoprotein cholesterol (LDL-C; LS mean percent changes of –1.0, 6.4 and 6.3%, respectively) were seen with canagliflozin 300 mg compared with canagliflozin 100 mg and placebo. There was no notable difference in non–HDL-C between the canagliflozin 300 mg and placebo groups (LS mean percent changes of 2.8 and 3.8%, respectively).
Table 3.
Summary of blood pressure and fasting plasma lipid findings at week 26 (LOCF)*
| Parameter | PBO (n = 90) | CANA 100 mg (n = 90) | CANA 300 mg (n = 89) |
|---|---|---|---|
| Systolic BP, n | 89 | 90 | 89 |
| Mean ± SD baseline, mmHg | 132.1 ± 13.6 | 135.9 ± 13.1 | 136.7 ± 15.0 |
| LS mean ± SE change | –0.3 ± 1.5 | –6.1 ± 1.5 | –6.4 ± 1.5 |
| Difference versus PBO (95% CI) | –5.7 (–9.5, –1.9) | –6.1 (–10.0, –2.3) | |
| Diastolic BP, n | 89 | 90 | 89 |
| Mean ± SD baseline, mmHg | 73.9 ± 9.0 | 73.5 ± 8.8 | 75.7 ± 7.8 |
| LS mean ± SE change | –1.4 ± 0.9 | –2.6 ± 0.9 | –3.5 ± 0.9 |
| Difference versus PBO (95% CI) | –1.2 (–3.4, 1.0) | –2.1 (–4.3, 0.2) | |
| Triglycerides, n | 75 | 82 | 85 |
| Mean ± SD baseline, mmol/l (mg/dl) | 2.0 ± 1.1 (179.4 ± 96.2) | 1.9 ± 0.9 (164.9 ± 81.1) | 2.1 ± 1.2 (189.3 ±103.5) |
| LS mean ± SE change, mmol/l (mg/dl) | –0.01 ± 0.11 (–0.7 ± 10.0) | 0.02 ± 0.11 (1.8 ± 9.7) | 0.22 ± 0.11 (19.5 ± 9.5) |
| Median (IQR) percent change | 2.8 (–18.4, 22.8) | –1.0 (–20.3, 17.3) | 2.5 (–16.1, 25.8) |
| LS mean ± SE percent change | 7.9 ± 4.8 | 6.2 ± 4.6 | 11.9 ± 4.6 |
| Difference versus PBO (95% CI) | –1.7 (–13.8, 10.5) | 3.9 (–8.1, 15.9) | |
| LDL-C, n | 75 | 82 | 84 |
| Mean ± SD baseline, mmol/l (mg/dl) | 2.5 ± 1.0 (96.3 ± 39.0) | 2.4 ± 0.9 (91.3 ± 33.4) | 2.3 ± 0.9 (87.2 ± 33.9) |
| LS mean ± SE change, mmol/l (mg/dl) | 0.06 ± 0.08 (2.4 ± 3.0) | 0.09 ± 0.08 (3.5 ± 2.9) | –0.08 ± 0.08 (–3.1 ± 2.9) |
| Median (IQR) percent change | 0.0 (–14.2, 22.3) | 1.3 (–9.0, 15.5) | 0.2 (–16.7, 16.1) |
| LS mean ± SE percent change | 6.3 ± 3.6 | 6.4 ± 3.5 | –1.0 ± 3.4 |
| Difference versus PBO (95% CI) | 0.1 (–8.9, 9.2) | –7.2 (–16.3, 1.8) | |
| HDL-C, n | 75 | 82 | 85 |
| Mean ± SD baseline, mmol/l (mg/dl) | 1.1 ± 0.3 (42.6 ± 10.0) | 1.1 ± 0.2 (43.1 ± 8.6) | 1.2 ± 0.3 (44.3 ± 12.2) |
| LS mean ± SE change, mmol/l (mg/dl) | 0.00 ± 0.02 (0.1 ± 0.7) | 0.03 ± 0.02 (1.3 ± 0.7) | 0.02 ± 0.02 (0.8 ± 0.7) |
| Median (IQR) percent change | 1.6 (–7.3, 8.2) | 2.3 (–6.6, 10.9) | 2.1 (–7.3, 11.8) |
| LS mean ± SE percent change | 1.5 ± 1.8 | 4.0 ± 1.7 | 3.0 ± 1.7 |
| Difference versus PBO (95% CI) | 2.5 (–1.9, 7.0) | 1.5 (–3.0, 5.9) | |
| LDL-C/HDL-C, n | 75 | 82 | 84 |
| Mean ± SD baseline, mol/mol | 2.3 ± 1.0 | 2.2 ± 0.9 | 2.1 ± 0.8 |
| LS mean ± SE change | 0.04 ± 0.08 | 0.02 ± 0.07 | –0.15 ± 0.07 |
| Median (IQR) percent change | –0.5 (–12.9, 16.6) | –2.2 (–13.0, 13.8) | 3.3 (–19.5, 12.4) |
| LS mean ± SE percent change | 4.7 ± 3.8 | 4.7 ± 3.7 | –4.3 ± 3.7 |
| Difference versus PBO (95% CI) | 0.0 (–9.7, 9.7) | –8.9 (–18.6, 0.8) | |
| Non–HDL-C, n | 75 | 81 | 85 |
| Mean ± SD baseline, mmol/l (mg/dl) | 3.4 ± 1.1 (131.9 ± 41.9) | 3.2 ± 0.9 (123.9 ± 36.2) | 3.3 ± 1.0 (125.7 ± 39.4) |
| LS mean ± SE change, mmol/l (mg/dl) | 0.06 ± 0.09 (2.2 ± 3.5) | 0.10 ± 0.09 (4.0 ± 3.4) | 0.02 ± 0.09 (0.9 ± 3.4) |
| Median (IQR) percent change | –1.0 (–13.7, 15.0) | 0.8 (–9.3, 12.0) | 1.9 (–11.5, 12.0) |
| LS mean ± SE percent change | 3.8 ± 2.9 | 5.1 ± 2.8 | 2.8 ± 2.8 |
| Difference versus PBO (95% CI) | 1.2 (–6.1, 8.6) | –1.1 (–8.3, 6.2) |
LOCF, last observation carried forward; PBO, placebo; CANA, canagliflozin; BP, blood pressure; SD, standard deviation; LS, least squares; SE, standard error; CI, confidence interval; IQR, interquartile range; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol.
Statistical comparison for CANA 100 and 300 mg versus PBO not performed (not prespecified).
Safety
Overall Safety and Tolerability
The overall incidence of AEs, serious AEs and study discontinuations due to AEs was similar for canagliflozin 100 and 300 mg and placebo (Table 4). The incidence of drug-related AEs was higher in both canagliflozin groups compared with placebo, largely because of a higher incidence of several specific AEs discussed below.
Table 4.
Summary of overall safety and selected AEs*
| Subjects, n (%) | |||
|---|---|---|---|
| PBO (n = 90) | CANA 100 mg (n = 90) | CANA 300 mg (n = 89) | |
| Any AE | 67 (74.4) | 71 (78.9) | 66 (74.2) |
| AEs leading to discontinuation | 5 (5.6) | 4 (4.4) | 2 (2.2) |
| AEs related to study drug† | 20 (22.2) | 23 (25.6) | 29 (32.6) |
| Serious AEs | 16 (17.8) | 10 (11.1) | 10 (11.2) |
| Deaths | 1 (1.1) | 1 (1.1) | 0 |
| Selected AEs | |||
| UTI | 5 (5.6) | 5 (5.6) | 7 (7.9) |
| Genital mycotic infection | |||
| Male†,§ | 0 | 1 (1.7) | 1 (2.1) |
| Female¶,‖ | 0 | 1 (3.1) | 1 (2.4) |
| Osmotic diuresis-related AEs | |||
| Pollakiuria** | 1 (1.1) | 2 (2.2) | 4 (4.5) |
| Polyuria†† | 0 | 0 | 0 |
| Volume-related AEs | |||
| Postural dizziness | 0 | 1 (1.1) | 2 (2.2) |
| Orthostatic hypotension | 0 | 0 | 1 (1.1) |
AE, adverse event; PBO, placebo; CANA, canagliflozin; UTI, urinary tract infection.
All AEs are reported for regardless of rescue medication, except for osmotic diuresis- and volume-related AEs, which are reported for prior to initiation of rescue therapy.
Possibly, probably or very likely related to study drug, as assessed by investigators.
PBO, n = 57; CANA 100 mg, n = 58; CANA 300 mg, n = 48.
Including balanitis and posthitis.
PBO, n = 33; CANA 100 mg, n = 32; CANA 300 mg, n = 41.
Including vulvovaginal mycotic infection.
Increased urine frequency.
Increased urine volume.
Canagliflozin was associated with slightly higher rates of genital mycotic infections in males and females compared with placebo (Table 4), but incidences were low across groups and none led to study discontinuation. The incidence of UTIs was higher with canagliflozin 300 mg compared with canagliflozin 100 mg and placebo, with no upper UTI AEs reported. All events were considered by investigators to be mild or moderate in severity, with none leading to study discontinuation. Incidences of pollakiuria (increased urine frequency) and AEs related to reduced intravascular volume (i.e. postural dizziness and orthostatic hypotension) were increased with canagliflozin 300 mg relative to canagliflozin 100 mg and placebo; these were low across groups, generally mild or moderate in intensity and infrequently led to discontinuation. There was no report of polyuria (increased urine volume) in any group.
Most subjects (96.3%) were on background AHA therapy associated with an increased risk of hypoglycaemia (i.e. insulin or sulphonylurea agents). Among these subjects, the proportion with documented hypoglycaemia episodes was higher with canagliflozin 100 and 300 mg (52.9 and 51.2%, respectively) compared with placebo (36.4%). Six subjects experienced severe hypoglycaemia episodes [4 (4.7%), 1 (1.2%) and 1 (1.1%) with canagliflozin 100 and 300 mg and placebo, respectively]. There were no documented hypoglycaemia episodes reported among subjects who were not on insulin or a sulphonylurea agent.
Overall, only small differences in safety laboratory parameters were observed with canagliflozin 100 and 300 mg relative to placebo (Table 5). At week 26, similar increases in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were observed with canagliflozin 100 mg (mean percent changes of 10.1 and 5.5%, respectively) and placebo (8.2 and 4.3%, respectively), whereas decreases were seen with canagliflozin 300 mg (–4.4 and –4.3%, respectively). Increases in serum magnesium were seen with canagliflozin 100 and 300 mg, whereas no change was observed with placebo (mean percent changes of 9.1, 14.6 and 0.0%, respectively). Dose-related increases in serum phosphate were seen with canagliflozin 100 and 300 mg compared with placebo (mean percent changes of 4.9, 9.5 and 1.0%, respectively). Canagliflozin 100 and 300 mg were associated with non–dose-related increases in haemoglobin compared with a minimal change with placebo (mean percent changes of 5.3, 3.1 and –0.5%, respectively); corresponding changes in haematocrit were observed (mean percent changes of 6.0, 4.8 and –0.1%, respectively; Table 5).
Table 5.
Mean percent changes in clinical laboratory parameters from baseline to week 26*
| PBO | CANA 100 mg | CANA 300 mg | |
|---|---|---|---|
| ALT, n | 63 | 70 | 78 |
| Mean baseline, U/l | 23.7 | 20.8 | 22.9 |
| Mean ± SD percent change | 8.2 ± 48.5 | 10.1 ± 40.4 | –4.4 ± 34.8 |
| Alkaline phosphatase, n | 63 | 70 | 78 |
| Mean baseline, U/l | 79.3 | 77.8 | 80.2 |
| Mean ± SD percent change | 5.3 ± 17.7 | 7.0 ± 19.6 | –2.1 ± 15.5 |
| AST, n | 62 | 67 | 78 |
| Mean baseline, U/l | 23.6 | 21.9 | 23.7 |
| Mean ± SD percent change | 4.3 ± 30.9 | 5.5 ± 31.3 | –4.3 ± 20.7 |
| Bilirubin, n | 63 | 70 | 78 |
| Mean baseline, µmol/l | 7.7 | 8.2 | 8.1 |
| Mean ± SD percent change | 4.1 ± 31.6 | 4.5 ± 31.9 | 7.4 ± 41.8 |
| Magnesium, n | 63 | 70 | 78 |
| Mean baseline, mmol/l | 0.8 | 0.8 | 0.8 |
| Mean ± SD percent change | 0.0 ± 9.3 | 9.1 ± 10.4 | 14.6 ± 12.9 |
| Phosphate, n | 63 | 70 | 77 |
| Mean baseline, mmol/l | 1.2 | 1.2 | 1.2 |
| Mean ± SD percent change | 1.0 ± 16.5 | 4.9 ± 16.0 | 9.5 ± 20.5 |
| Urate, n | 63 | 70 | 78 |
| Mean baseline, µmol/l | 433.7 | 434.4 | 442.5 |
| Mean ± SD percent change | 2.5 ± 18.6 | –0.3 ± 16.9 | –2.0 ± 20.0 |
| Haemoglobin, n | 62 | 69 | 76 |
| Mean baseline, g/l | 136.2 | 133.8 | 130.9 |
| Mean ± SD percent change | –0.5 ± 8.1 | 5.3 ± 7.4 | 3.1 ± 5.9 |
| Haematocrit, n | 62 | 69 | 76 |
| Mean baseline, % | 40.8 | 40.1 | 39.2 |
| Mean ± SD percent change | –0.1 ± 9.1 | 6.0 ± 7.6 | 4.8 ± 6.9 |
PBO, placebo; CANA, canagliflozin; ALT, alanine aminotransferase; SD, standard deviation; AST, aspartate aminotransferase.
Statistical comparison for CANA 100 and 300 mg versus PBO not performed (not prespecified).
Measures of Renal Function
Changes in renal function parameters were observed with both canagliflozin doses compared with placebo. Decreases in eGFR from baseline were observed in all treatment groups and were larger in the canagliflozin 100 and 300 mg groups relative to the placebo group: LS mean percent changes of –9.1, –10.1 and –4.5%, respectively. The reductions in eGFR with canagliflozin were largest at week 3 (the first postbaseline measurement) and then trended back towards baseline over the 26-week treatment period (figure 3A). Increases in BUN were observed with canagliflozin 100 and 300 mg compared with placebo (LS mean percent changes of 12.1, 12.5 and 4.9%, respectively); these increases also occurred early and then trended towards baseline over the remaining treatment period. Canagliflozin 100 and 300 mg were associated with greater decreases in urine ACR compared with placebo, with median percent reductions of –29.9, –20.9 and –7.5%, respectively (figure 3B). Progression of albuminuria from baseline to week 26 was examined (i.e. from normoalbuminuria to micro- or macroalbuminuria, or from micro- to macroalbuminuria), with a lower proportion of subjects in the canagliflozin 100 and 300 mg groups progressing relative to those in the placebo group [5.1, 8.3 and 11.8%, respectively; odds ratio (95% CI) of 0.33 (0.08, 1.48) and 0.51 (0.14, 1.91) for the pairwise comparisons of canagliflozin 100 and 300 mg to placebo, respectively].
Figure 3.
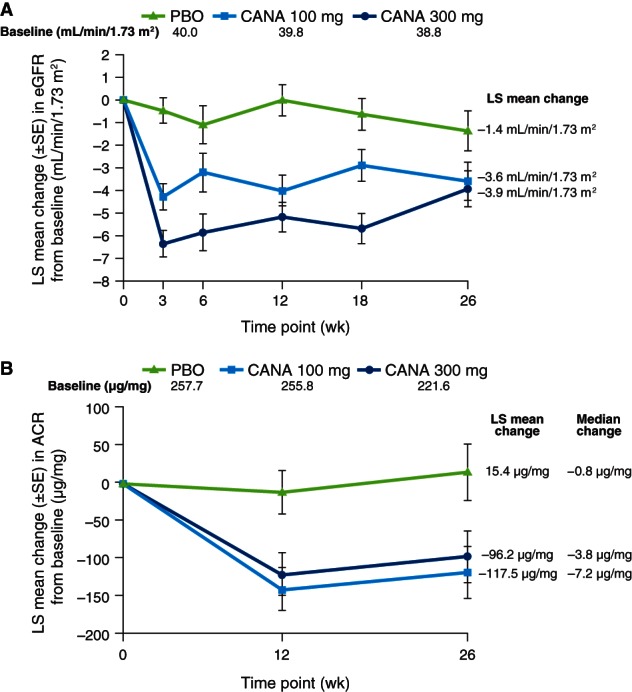
Change in eGFR (A) and ACR (B) over time. #eGFR, estimated glomerular filtration rate; ACR, albumin/creatinine ratio; PBO, placebo; CANA, canagliflozin; LS, least squares; SE, standard error. *Statistical comparison for CANA versus PBO not performed (not prespecified).
Discussion
This study examined the efficacy and safety of canagliflozin in subjects with T2DM and stage 3 CKD, but in a lower, more restricted eGFR range of this classification (i.e. 30 to <50 ml/min/1.73 m2 rather than to <60 ml/min/1.73 m2). In this study population, both canagliflozin doses significantly lowered HbA1c compared with placebo over 26 weeks of therapy. Reductions in HbA1c with canagliflozin 100 and 300 mg (differences in LS mean changes vs. placebo of –0.30 and –0.40%, respectively) were clinically useful, particularly in the setting of stage 3 CKD in which available oral AHA therapy options are limited.
In addition to providing reductions in HbA1c, a numerically greater proportion of subjects treated with canagliflozin (including about a third of subjects in the canagliflozin 300 mg group) achieved HbA1c <7.0% than those treated with placebo, indicating that canagliflozin provides meaningful clinical value in this patient population. Both canagliflozin doses provided numerically greater reductions in FPG compared with placebo, although these differences did not achieve statistical significance. A smaller proportion of subjects treated with canagliflozin required glycaemic rescue therapy compared with placebo-treated subjects. Both canagliflozin doses were also associated with reductions in body weight relative to placebo. The mechanism by which canagliflozin reduces body weight is thought to be related to the loss of calories associated with induction of UGE, although through the osmotic diuretic effect, reduced fluid volume may also contribute to the reduction in body weight – this may be particularly relevant in patients with renal impairment who tend to have sodium and fluid retention, and therefore have excessive fluid volume. Also likely related to the osmotic diuretic effect, canagliflozin provided numerically greater reductions in systolic and diastolic BP compared with placebo, an important observation given the often difficult-to-treat hypertension in patients with stage 3 CKD.
The efficacy on glycaemic parameters and body weight reduction observed with canagliflozin in this population of subjects was less than that seen in subjects with T2DM who have normal or only mildly impaired renal function 10,14–17. This is not unexpected because the rate of UGE is related to both plasma glucose concentration and eGFR; with lower eGFR, the ability of canagliflozin to augment UGE is attenuated 7,8,11. With lesser increases in UGE, the glucose-lowering efficacy of canagliflozin is also reduced. Results from the current study are consistent with those from a phase 1 canagliflozin study showing reduced UGE and decreased RTG lowering in subjects with stage 3 CKD compared with subjects with normal renal function 18. Owing to the limited amount of UGE observed with canagliflozin treatment in patients with more severe renal insufficiency 18, SGLT2 inhibitors are not expected to be efficacious for patients with an eGFR <30 ml/min/1.73 m2 (i.e. stages 4 or 5 CKD) or for dialysis patients.
Both canagliflozin doses were well tolerated, and incidences of AEs, serious AEs and study discontinuations due to AEs were similar across treatment groups. The AEs associated with SGLT2 inhibition seen in other canagliflozin phase 3 studies 14–17, including genital mycotic infections, a small increase in UTIs (with no reports of upper UTI AEs), and AEs related to osmotic diuresis (i.e. pollakiuria and polyuria), were also seen in this study, although at lower rates, which may reflect the attenuation of UGE in this study population.
Canagliflozin acts by lowering RTG; this value is typically 10.0 mmol/l (180 mg/dl) in normal individuals, raised in patients with T2DM to approximately 13.3 mmol/l (240 mg/dl), and reduced to levels of approximately 4.4 to 5.0 mmol/l (80-90 mg/dl) in patients treated with canagliflozin 9,10. Because the usual threshold for hypoglycaemia is approximately 3.9 mmol/l (70 mg/dl), this would suggest a low risk for hypoglycaemia with canagliflozin – as has been observed in studies of healthy volunteers and patients with T2DM 7,9,10,16. When an agent not associated with hypoglycaemia is added to the regimen of a medication that is associated with hypoglycaemia, like insulin or a sulphonylurea agent, an increase in hypoglycaemia is usually observed 19–23. This was seen in this study for subjects on background therapy with insulin or a sulphonylurea agent, in whom both canagliflozin doses were associated with the expected higher incidences of hypoglycaemia relative to placebo. Importantly, the rate of severe hypoglycaemia in subjects on such agents was low and there were no documented hypoglycaemia episodes among subjects not on insulin or a sulphonylurea agent.
Because the kidney is a target organ with canagliflozin treatment, the effects of canagliflozin on renal function were carefully assessed in this study. Canagliflozin 100 and 300 mg were associated with some changes in renal function (assessed by eGFR, serum creatinine, BUN and ACR) early on, with subsequently stable or improving eGFR values over the 26-week core treatment period (compared with a gradual, small decline in the placebo group). These transient changes in renal function with canagliflozin may be related to a mild osmotic diuretic effect of this agent, with small reductions in plasma volume, leading to a mild prerenal pattern. The proportion of subjects with progression of albuminuria with canagliflozin was slightly less than with placebo; the decrease in the ACR along with the stable renal function after the small initial decline is reassuring with regard to the lack of renal injury with this agent. The urinary ACR has been used as a biomarker, with reduction suggesting prevention of progression of renal injury 24,25, as seen with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs); whether the reduction in ACR seen with canagliflozin, along with stable renal function (after the small initial decrease), indicates the potential for renal protection with canagliflozin can only be assessed with longer-term and larger studies.
As noted, the efficacy observed with canagliflozin in this renal-impaired population with T2DM was less than that observed in subjects with normal or only mildly impaired renal function. Nonetheless, this agent still provides important clinical value in this setting. It is important to note that physicians managing such patients have limited options, with several agents restricted (e.g. metformin or thiazolidinediones), and other agents that must be used carefully owing to safety concerns, including sulphonylurea agents and insulin that can lead to sodium retention, weight gain and hypoglycaemia. Treatment with canagliflozin added on to subjects' stable diabetes treatment regimens lowered HbA1c and resulted in more patients reaching HbA1c goal compared with placebo, indicating clinical utility. Additional studies are needed to assess the efficacy and safety of canagliflozin monotherapy in patients with renal impairment. It is interesting to note that another SGLT2 inhibitor, dapagliflozin, has not demonstrated HbA1c-lowering efficacy in this patient population 26; whether this indicates differences between agents in this class or differences in study design remains to be determined.
In conclusion, canagliflozin 100 and 300 mg significantly reduced HbA1c and were associated with numerical reductions in FPG, body weight and BP compared with placebo after 26 weeks of therapy in subjects with T2DM and stage 3 CKD (eGFR ≥30 and <50 ml/min/1.73 m2). Canagliflozin was generally well tolerated, with an expected increase in hypoglycaemia among the >95% of subjects on insulin or a sulphonylurea agent. Canagliflozin was associated with transient changes in renal function parameters that recovered towards baseline over the study period. These findings suggest that canagliflozin may be an appropriate treatment option for patients with T2DM and stage 3 CKD.
Acknowledgments
This study was sponsored by Janssen Research & Development, LLC. The authors thank all investigators, study teams and patients for participating in this study. Editorial support was provided by Lisa Shannon, PharmD, of MedErgy, and was funded by Janssen Global Services, LLC. Canagliflozin is being developed by Janssen Research & Development, LLC, in collaboration with Mitsubishi Tanabe Pharma Corporation.
This study was previously presented, in part, in abstract form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, PA, 8–12 June 2012; the 48th Annual Meeting of the European Association for the Study of Diabetes, Berlin, Germany, 1–5 October 2012; the 15th Annual Canadian Diabetes Association/Canadian Society of Endocrinology and Metabolism Professional Conference, Vancouver, Canada, 10–13 October 2012 and the American Society of Nephrology Kidney Week 2012, San Diego, California, 30 October to 4 November 2012.
Conflict of Interest
J.-F. Y. has received research support from Sanofi, Pfizer, NovoNordisk, Merck, Novartis, Janssen and Medtronic; served on advisory panels for Sanofi, Merck, GlaxoSmithKline, Eli Lilly, Bayer, Pfizer, NovoNordisk, Lifescan, Roche, Novartis, Bristol-Myers Squibb, AstraZeneca and Janssen; and served as a lecturer for Sanofi, Merck, GlaxoSmithKline, Eli Lilly, Bayer, Pfizer, NovoNordisk, Roche, Abbott, Bristol-Myers Squibb, AstraZeneca, Medtronic and Janssen. G. B. has received research support (direct funding to The University of Chicago Medicine) from Forest Labs; served as a national clinical trial principal investigator for Medtronic and Relypsa; consulted for Takeda, Abbott, CVRx, Johnson & Johnson, Eli Lilly, and the Food and Drug Administration; participated in a speaker bureau for Takeda, served as a board member for the National Kidney Foundation and the American Society of Hypertension; and served as an editor for the American Journal of Nephrology and as an associated editor for the Diabetes Care and Nephrology Dialysis Transplantation journals. B. C. has received research support from NovoNordisk and Sanofi; and served on advisory panels for Amgen, Genfit, Janssen, Eli Lilly, NovoNordisk, MSD and Sanofi. D. Y. has served on advisory panels for Johnson & Johnson. E. D.-N. has received research support from Novartis, Bristol-Myers Squibb and Pfizer; and served as a speaker for Novartis, Pfizer and Alexion. L. X., K. F., E. W., K. U. and G. M. are full-time employees of Janssen Research & Development, LLC.
J.-F. Y., G. B., B. C., D. Y., E. D.-N, K. F., and G. M. contributed to the conduct of the study and the acquisition, analysis and interpretation of data, and reviewed and approved the manuscript. L. X. contributed to the analysis and interpretation of data, and reviewed and approved the manuscript. E. W. and K. U. contributed to the design and conduct of the study, contributed to the acquisition, analysis and interpretation of data, and reviewed and approved the manuscript.
References
- 1.Kramer H, Molitch ME. Screening for kidney disease in adults with diabetes. Diabetes Care. 2005;28:1813–1816. doi: 10.2337/diacare.28.7.1813. [DOI] [PubMed] [Google Scholar]
- 2.Flynn C, Bakris G. Noninsulin glucose-lowering agents for the treatment of patients on dialysis. Nat Rev Nephrol. 2013;9:147–153. doi: 10.1038/nrneph.2013.12. [DOI] [PubMed] [Google Scholar]
- 3.Cavanaugh KL. Diabetes management issues for patients with chronic kidney disease. Clin Diabetes. 2007;25:90–97. [Google Scholar]
- 4.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012;35:1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 6.Nomura S, Sakamaki S, Hongu M, et al. Discovery of canagliflozin, a novel C-glucoside with thiophene ring, as sodium-dependent glucose cotransporter 2 inhibitor for the treatment of type 2 diabetes mellitus. J Med Chem. 2010;53:6355–6360. doi: 10.1021/jm100332n. [DOI] [PubMed] [Google Scholar]
- 7.Sha S, Devineni D, Ghosh A, et al. Canagliflozin, a novel inhibitor of sodium glucose co-transporter 2, dose dependently reduces calculated renal threshold for glucose excretion and increases urinary glucose excretion in healthy subjects. Diabetes Obes Metab. 2011;13:669–672. doi: 10.1111/j.1463-1326.2011.01406.x. [DOI] [PubMed] [Google Scholar]
- 8.Liang Y, Arakawa K, Ueta K, et al. Effect of canagliflozin on renal threshold for glucose, glycemia, and body weight in normal and diabetic animal models. PLoS One. 2012;7:e30555. doi: 10.1371/journal.pone.0030555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devineni D, Morrow L, Hompesch M, et al. Canagliflozin improves glycemic control over 28 days in subjects with type 2 diabetes not optimally controlled on insulin. Diabetes Obes Metab. 2012;14:539–545. doi: 10.1111/j.1463-1326.2012.01558.x. [DOI] [PubMed] [Google Scholar]
- 10.Rosenstock J, Aggarwal N, Polidori D, et al. Dose-ranging effects of canagliflozin, a sodium-glucose cotransporter 2 inhibitor, as add-on to metformin in subjects with type 2 diabetes. Diabetes Care. 2012;35:1232–1238. doi: 10.2337/dc11-1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polidori D, Sakai M, Devineni D. Exposure-response modeling of canagliflozin effects on the renal glucose threshold in subjects with type 2 diabetes (T2DM) (Abstract 1072-P) Diabetes. 2011;60(Suppl. 1):A294. [Google Scholar]
- 12.Levey AS, Coresh J, Greene T, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53:766–772. doi: 10.1373/clinchem.2006.077180. [DOI] [PubMed] [Google Scholar]
- 13. National Kidney Foundation. Kidney disease outcomes quality initiative. clinical practice guidelines for chronic kidney disease: evaluation, classification and stratification. 2002. [DOI] [PubMed]
- 14.Niskanen L, Cefalu WT, Leiter LA, et al. Efficacy and safety of canagliflozin, a sodium glucose co-transporter 2 inhibitor, compared with glimepiride in patients with type 2 diabetes on background metformin (Abstract 763) Diabetologia. 2012;55(Suppl. 1):S314. [Google Scholar]
- 15.Schernthaner G, Gross J, Fu M, et al. Efficacy and safety of canagliflozin, a sodium glucose co-transporter 2 inhibitor, compared with sitagliptin in patients with type 2 diabetes on metformin plus sulphonylurea (Abstract 243) Diabetologia. 2012;55(Suppl. 1):S108. [Google Scholar]
- 16.Stenlof K, Cefalu WT, Tong C, et al. Canagliflozin, a sodium glucose co-transporter 2 inhibitor, improves glycaemic control in subjects with type 2 diabetes inadequately controlled with diet and exercise (Abstract 760) Diabetologia. 2012;55(Suppl. 1):S312–313. [Google Scholar]
- 17.Wilding J, Mathieu C, Deng L, et al. Canagliflozin, a sodium glucose co-transporter 2 inhibitor, improves glycaemia in subjects with type 2 diabetes inadequately controlled with metformin plus sulphonylurea (Abstract 766) Diabetologia. 2012;55(Suppl. 1):S315–316. [Google Scholar]
- 18.Devineni D, Marbury TC, Curtin CR, et al. Effects of renal function on canagliflozin (CANA) pharmacokinetics (PK) and pharmacodynamics (PD) in non-diabetic subjects (Abstract PUB295) J Am Soc Nephrol. 2012;23:961A. [Google Scholar]
- 19.Buse JB, Henry RR, Han J, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care. 2004;27:2628–2635. doi: 10.2337/diacare.27.11.2628. [DOI] [PubMed] [Google Scholar]
- 20.Hermansen K, Kipnes M, Luo E, Fanurik D, Khatami H, Stein P. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab. 2007;9:733–745. doi: 10.1111/j.1463-1326.2007.00744.x. [DOI] [PubMed] [Google Scholar]
- 21.Kendall DM, Riddle MC, Rosenstock J, et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care. 2005;28:1083–1091. doi: 10.2337/diacare.28.5.1083. [DOI] [PubMed] [Google Scholar]
- 22.Strojek K, Yoon KH, Hruba V, Elze M, Langkilde AM, Parikh S. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomized, 24-week, double-blind, placebo-controlled trial. Diabetes Obes Metab. 2011;13:928–938. doi: 10.1111/j.1463-1326.2011.01434.x. [DOI] [PubMed] [Google Scholar]
- 23.Wilding JP, Woo V, Soler NG, et al. Long-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial. Ann Intern Med. 2012;156:405–415. doi: 10.7326/0003-4819-156-6-201203200-00003. [DOI] [PubMed] [Google Scholar]
- 24.de Zeeuw D, Remuzzi G, Parving HH, et al. Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney Int. 2004;65:2309–2320. doi: 10.1111/j.1523-1755.2004.00653.x. [DOI] [PubMed] [Google Scholar]
- 25. The National Kidney Disease Education Program (NKDEP). Urine albumin-to-creatinine ratio (UACR) in evaluating patients with diabetes for kidney disease. 2010.
- 26.Kohan DE, Fioretto P, List J, Tang W. Efficacy and safety of dapagliflozin in patients with type 2 diabetes and moderate renal impairment (Abstract TH-PO524) J Am Soc Nephrol. 2011;22(Suppl):232-A. [Google Scholar]


