Introduction
Exposure to war-zone stress confers significant risk for a broad range of detrimental mental health effects, in particular posttraumatic stress disorder (PTSD) and substance use disorders (SUDs). Among Veterans from the most recent conflicts, Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) in Afghanistan and Iraq, approximately 15–17% suffer from PTSD (1–4) and up to 24% demonstrate alcohol misuse (5–6). Furthermore, OEF/OIF Veterans with, as compared to without, PTSD are more than twice as likely to have an alcohol use disorder (3).
Despite the relative frequency of PTSD and comorbid SUDs, empirical evidence needed to guide treatment is sparse. Historically, the standard of care has been the sequential model in which the SUD is treated first and trauma work deferred until the patient achieves some length of sustained abstinence (e.g., 6 months). This deferment is based primarily on the concern that trauma work will lead to substance use exacerbation. Contrary to these early, largely anecdotal concerns, a burgeoning literature examining integrative models, in which both disorders are simultaneously addressed, documents significant improvement in substance use severity, PTSD symptomatology and global functioning outcomes (7–8). Compelling evidence is also provided by studies investigating the temporal course of improvement in symptoms. These studies show that patients who achieve improvement in PTSD are significantly more likely to show subsequent improvement in substance use, but the reciprocal relationship is less robust, with only minimal evidence that improvement in substance use yields improvement in PTSD (9–10). Taken together, the accumulating data highlight the critical need to address PTSD in order to optimize treatment for PTSD/SUD patients.
In response to this need, a cognitive-behavioral treatment that represents a synthesis of theory-based and empirically-validated treatments for PTSD (11) and substance use disorders (12) was designed. COPE (Concurrent Treatment of PTSD and Substance Use Disorders using Prolonged Exposure) consists of 12, individual, 90-minute sessions that integrate relapse prevention for substance use with Prolonged Exposure (PE) for PTSD. The substance use treatment component is designed to help patients identify triggers (e.g., environmental, emotional) and high-risk situations for substance use, and effectively manage cravings through a variety of techniques (e.g., stimulus control, decision delay, cognitive restructuring). Patients are taught a technique called “Urge Surfing,” which encourages patients to sit with the craving, and observe the natural rise and fall of the urge to use substances. Urge Surfing is synergistic with exposure-based techniques and teaches patients that cravings, like anxiety, do not last forever and that they are capable of ‘riding out the wave’ of both anxiety and cravings. In addition, COPE teaches patients skills to manage anger, a symptom of PTSD and a frequent trigger for relapse for SUDs (6). The PTSD treatment component is designed to normalize common reactions to trauma, and reduce PTSD symptoms via in-vivo and imaginal exposure. In-vivo exposure involves having patients repeatedly confront safe, but anxiogenic situations that serve as trauma reminders and are avoided. Imaginal exposure involves having patients repeatedly revisit the memory of the traumatic event to help organize the memory, gain new perspective, decrease emotional reactivity to the memory, and enhance self competence. Based on promising preliminary findings demonstrating the feasibility, safety and efficacy of COPE among civilian samples (8, 13), we applied COPE to a U.S. Marine returning from Iraq. The following measures were used for diagnostic assessment and to monitor progress: Mini International Neuropsychiatric Interview (MINI; 14) assessed psychiatric diagnoses, Clinician Administered PTSD Scale (CAPS; 15) assessed PTSD diagnosis and symptoms, PTSD Checklist-Military (PCL-M; 16) monitored weekly PTSD severity, Beck Depression Inventory (BDI-II; 17) assessed weekly depressive symptoms, Timeline Follow-Back (TLFB; 18) monitored self-report daily use of substances, urine drug screens (UDS) assessed illicit drug use, and breathalyzer tests assessed recent alcohol use. An independent assessor conducted the MINI, CAPS and TLFB.
Case Presentation
The patient was a 25-year-old, single, Caucasian Marine Veteran with a history of three OIF deployments (21 months total) where he engaged in reconnaissance duties and served as a gunner. While on a mission, the patient witnessed the shooting of a close comrade. He assisted in providing medical care to his wounded comrade, who died in the patient’s arms while en route to a hospital. After returning to the U.S., the patient experienced daily intrusive memories and nightmares about the shooting. He avoided crowds and social situations, engaged in heavy alcohol use, and grew distant from family and friends. He reported severe hyperarousal in crowded stores and became physically violent in situations where he felt provoked. At baseline, the patient scored in the clinical range for PTSD (CAPS Total Score = 71; PCL-M Total Score = 53), exhibited mild depression (BDI Total Score = 17), had a positive breathalyzer, and consumed approximately 12.5 beers per day on 50/60 days (83.3%) prior to baseline.
Treatment and Progress
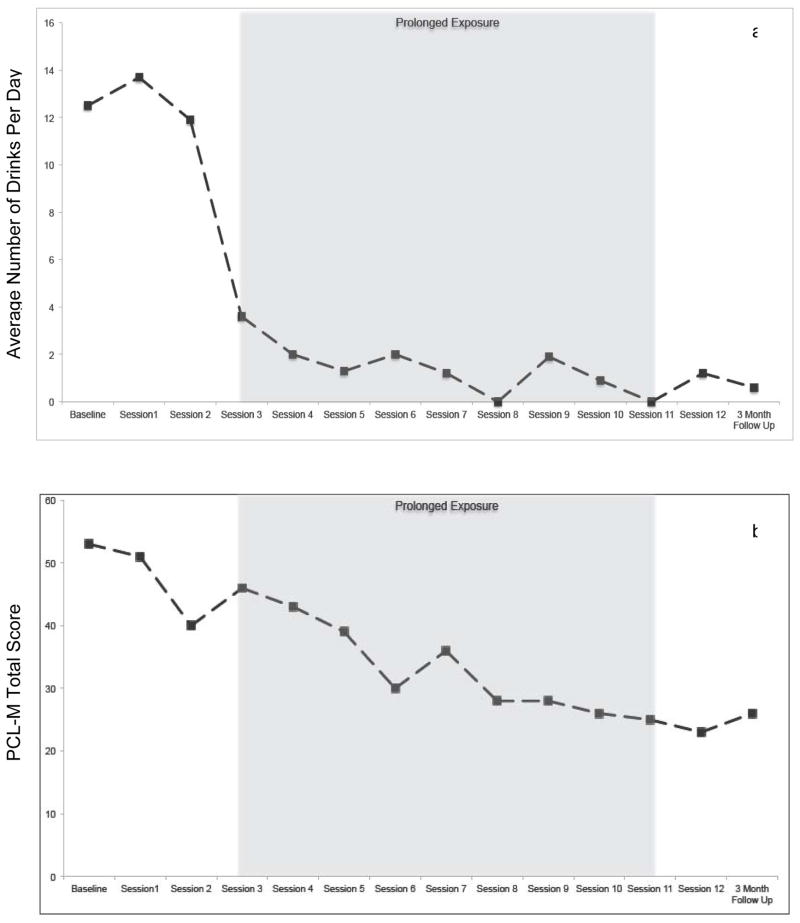
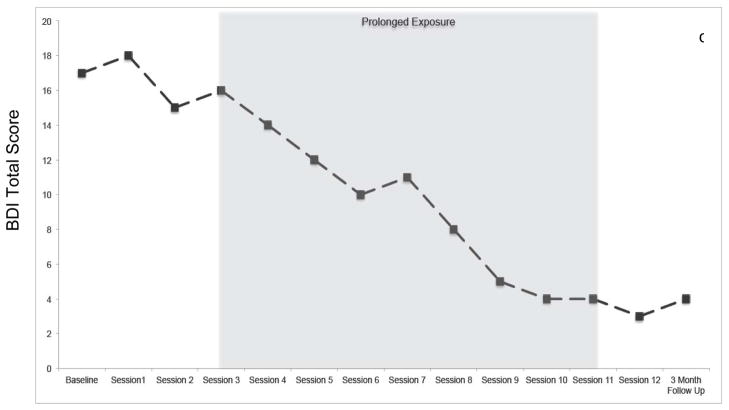
Each session consisted of a substance use and a PTSD treatment component. In the first 30 minutes of each session, the clinician evaluated the patient’s alcohol consumption since the last session, assessed high-risk situations encountered, and discussed techniques for managing cravings. At session 1, the patient’s identified goal was to reduce alcohol consumption from 12.5 to 5.0 standard drinks per day, three days per week. Sessions 2–3 focused on learning skills to manage cravings and thoughts about using alcohol. By session 3, the patient’s alcohol use frequency and severity had responded rapidly (Figure 1a) and remained low through follow-up. All UDS and breathalyzer tests after baseline were negative.
Figure 1.
(a–c). Improvement in alcohol use severity, PTSD symptomatology and depression during treatment and at 3-month follow up.
Note. PCL-M = PTSD Checklist-Military. BDI = Beck Depression Inventory. In-vivo exposures began at session 3 and imaginal exposures began at session 4.
During the remaining 60 minutes of each session, PTSD was addressed. In sessions 1–3, education on fear and avoidance, the rationale for concurrent treatment, breathing retraining (a relaxation exercise), and the rationale for in-vivo and imaginal exposures were provided. In session 3, the clinician and patient constructed an in-vivo hierarchy comprised of safe situations being avoided. The patient selected two in-vivo exposures to complete each week, starting with situations that provoked a moderate amount of subjective discomfort (e.g., going to a movie theatre, calling a friend), gradually moving up to situations associated with greater discomfort (e.g., going to a crowded festival). As a result of engaging in the in-vivo exposures, the patient was able to visit family, develop new friendships, engage in social activities, and begin dating again. The application of in-vivo exposures among patients with co-occurring SUDs requires carefully assessment. Situations that increase exposure to substances or have a high probability of inducing craving are not included on the hierarchy. For example, if the trauma occurred in a bar where the patient previously drank alcohol, this would not be a safe in-vivo exposure assignment. Patients must be instructed not to use any substances before, during or immediately after engaging in exposures. Alcohol use in this context would represent a “safety behavior” that would dilute the exposure’s therapeutic effects.
Imaginal exposures (sessions 4–11) consisted of repeatedly recounting the memory of the shooting, in the present tense with eyes closed for 30–45 minutes. This was followed by approximately 10 minutes of processing, and discussing the thoughts and feeling that came to mind during the imaginal exposure. Starting in session 8, “hot spots” (the most distressing parts of the trauma memory) were repeated. Finally, in session 11, the entire memory was revisited. The patient listened to a recording of the imaginal exposure each day, and reported that this daily exercise helped him to do the imaginal exposures in session. Processing focused primarily on the patient’s feelings of guilt in two areas; 1) his belief that he should have been able to prevent his comrade’s death by locating the enemy sniper ahead of time, and 2) his belief that he should have been the one who was killed, as opposed to his comrade. Through a series of questions (i.e., “What did you do differently than what you were trained to do?” and “How would it have made it any better had you been the one killed?”), the patient was able to realize that he did everything he was trained to do as a Marine and yet not he, nor any of his other comrades, were able to prevent the shooting. In addition, he realized that his own death would not have resulted in an improved outcome. As a result of these cognitive shifts, the patient was better able to accept both outcomes as unfair “circumstances of war.” The reaction of the patient’s senior commanding officer following the death of his comrade was also an important part of processing. The patient felt angry and vulnerable when he saw his commanding officer “break down” outside the hospital.
Several challenges occurred during treatment. For example, during session 1 the patient related a desire to reduce, rather than abstain from, alcohol use. Although abstinence may be an ideal goal, the therapist found it most effective to meet the patient ‘where he was at’ by using a non-confrontational approach. By session 4, the patient had surpassed his goal and was abstaining from alcohol the majority of each week. Another challenge involved two separate instances during the patient’s in-vivo exposure assignments (i.e., social activities) where he felt provoked and became physically violent with other men. Anger was discussed as a common symptom of PTSD, and skills for managing anger were reviewed and role-played in session to help prevent future violent episodes.
In the final session, the patient’s progress toward accomplishing treatment goals established during the first session was reviewed, areas for continued focus were discussed, and an emergency plan to help prevent relapse of alcohol use was generated. At session 12, the patient scored in the non-clinical range for PTSD (CAPS Total Score = 42; PCL-M Total Score = 23) and depression (BDI Total Score = 3), all of which were reliable changes as defined by Jacobson’s Reliable Change Index (19) and based on standard deviations and scale reliabilities reported in Veterans with PTSD (20). Treatment gains were maintained at the 3 month follow-up visit.
Discussion
We presented this case to stimulate discussion of improved models of treatment for PTSD and co-occurring SUDs. This case builds on an established body of knowledge demonstrating the efficacy of exposure-based treatments, as well as a burgeoning literature of promising results from integrative PTSD/SUD interventions, and is the first to report on the use of an exposure-based, integrative treatment among OEF/OIF Veterans. Investigations of combat Veterans from previous eras demonstrate the chronicity and disability associated with PTSD and SUDs, and highlight the urgent need for effective PTSD/SUD interventions for OEF/OIF Veterans.
Similar to previous studies among civilians, the application of trauma work did not result in exacerbated substance use. In particular, no increase in alcohol use was observed at the onset of in-vivo or imaginal exposures. Although the patient continued to drink at a significantly reduced level during the course of therapy, substantial gains in PTSD symptoms and overall functioning were achieved. This is important as it demonstrates that abstinence, although a goal that has been widely thought to maximize benefits of treatment, is not essential before commencing trauma work and is not necessary for individuals to achieve substantial PTSD improvement. Abstinence is, however, the safest goal and it is possible that had the patient abstained from all substance use, further improvements in PTSD would have been realized.
Conclusions
Evidenced-based interventions that effectively address PTSD and co-occurring SUDs are vitally needed in VA-based as well as civilian-based healthcare settings. This case report adds to accumulating data demonstrating the feasibility, safety and efficacy of integrative PTSD/SUD interventions employing exposure-based methods. The patient, a young, treatment naïve, OIF Marine Veteran with severe alcohol dependence and PTSD exhibited significant improvements after completing a 12-session integrative intervention. These promising findings warrant further examination in order to optimize treatment outcomes as well as durability of effects.
Acknowledgments
The authors would like to acknowledge support from NIDA grant DA021228 (SEB). We thank Drs. Katherine Mills and Denise Hien for assistance with manual development and testing.
References
- 1.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Eng J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 2.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- 3.Shea MT, Vujanovic AA, Mansielf AK, Sevin E, Liu F. Posttraumatic stress disorder symptoms and functional impairment among OEF and OIF National Guard and Reserve Veterans. J Trauma Stress. 2010;23:100–107. doi: 10.1002/jts.20497. [DOI] [PubMed] [Google Scholar]
- 4.Booth-Kewley S, Larson GE, Highfill-McCoy RM, Garland CF, Gaskin TA. Psychological consequences of the wars in Iraq and Afghanistan. J Trauma Stress. 2010;23:69–77. doi: 10.1002/jts.20485. [DOI] [PubMed] [Google Scholar]
- 5.Bray RM, Pemberton MR, Lane ME, Hourani LL, Mattiko MJ, Babeu LA. Substance use and mental health trends among U.S. active duty personnel: Key findings from the 2008 DoD Health Behavior Survey. Mil Med. 2010;6:390–399. doi: 10.7205/milmed-d-09-00132. [DOI] [PubMed] [Google Scholar]
- 6.Elbogen EB, Wagner HR, Fuller SR, Calhoun PS, Kinneer PM, Beckham JC. Correlates of anger and hostility in Iraq and Afghanistan war Veterans. Am J Psychiat. 2010;167:1051–1058. doi: 10.1176/appi.ajp.2010.09050739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Back SE. Toward an improved model of treating co-occurring PTSD and substance use disorders. Am J Psychiat. 2010;167:11–13. doi: 10.1176/appi.ajp.2009.09111602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brady KT, Dansky BS, Back SE, Foa AB, Carroll KM. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Preliminary findings. J Subst Abuse Treat. 2001;21:47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- 9.Hien DA, Jiang H, Campbell ANC, Hu MC, Miele GM, Cohen LR, Brigham GS, Captick C, Kulaga A, Robinson J, Suarez-Morales L, Nunes EV. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s clinical trials network. Am J Psychiat. 2010;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Back SE, Brady KT, Sonne SC, Verduin ML. Symptom improvement in co-occurring PTSD and alcohol dependence. J Nerv Ment Dis. 2006;194:690–696. doi: 10.1097/01.nmd.0000235794.12794.8a. [DOI] [PubMed] [Google Scholar]
- 11.Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences, therapist guide. New York: Oxford University Press; 2007. [Google Scholar]
- 12.Carroll KM. A Cognitive–behavioral approach: Treating cocaine addiction. Rockville, MD: National Institute on Drug Abuse; 1998. [Google Scholar]
- 13.Mills KL, Teesson M, Back SE, Baker A, Hopwood S, Brady K, Sannibale C. A randomized controlled trial of an integrated treatment for substance use and PTSD incorporating exposure therapy: preliminary findings. Abstracts Presented at the 2008 Annual Meeting of the College on Problems of Drug Dependence; ( http://www.cpdd.vcu.edu/Pages/Meetings/CPDD08AbstractBook2.pdf. [Google Scholar]
- 14.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiat. 1998;59:22–33. [PubMed] [Google Scholar]
- 15.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. J Trauma Stress. 1990;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 16.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist: reliability, validity and diagnostic utility. Annual meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- 17.Beck AT, Steer RA, Brown GK. Beck Depression Inventory--II (BDI-II) San Antonio, TX: Harcourt Assessment; 1996. [Google Scholar]
- 18.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–73. [Google Scholar]
- 19.Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 20.Gros DF, Simms LJ, Acierno R. Specificity of posttraumatic stress disorder symptoms: An investigation of comorbidity between posttraumatic stress disorder symptoms and depression in treatment-seeking Veterans. J Nerv Ment Dis. 2010;198:885–890. doi: 10.1097/NMD.0b013e3181fe7410. [DOI] [PubMed] [Google Scholar]