Abstract
Until recently, only one study was published on cognitive-behavioral therapy (CBT) of posttraumatic stress disorder (PTSD) in individual therapy via videoconference (Germain, Marchand, Bouchard, Drouin, & Guay, 2009); however, it only assessed the posttreatment effect. This study presents the follow-up of Germain et al.’s (2009) study. The main goal was to compare the effectiveness after six months of CBT for PTSD either face-to-face (n = 24) or by videoconference (n = 12). Each participant received CBT for 16 to 25 weeks and completed various questionnaires before and after treatment and at a six-month follow-up. The two treatments had equivalent levels of symptom reduction (Modified PTSD Symptom Scale: η2 < 0.01, p > .05) and proportion of patients with a clinically significant change in symptoms (42% for face-to-face vs. 38% for videoconferencing, p > .05). Thus, CBT for PTSD via videoconference seems to be a viable alternative when adequate face-to-face treatments are less available.
Keywords: cognitive-behavioral therapy, diverse trauma, telepsychotherapy, videoconference
Currently, cognitive-behavioral therapy (CBT) is the most empirically validated treatment for posttraumatic stress disorder (PTSD); its efficacy was confirmed in two meta-analyses (Bradley, Greene, Russ, Dutra, & Westen, 2005; Van Etten & Taylor, 1998). However, access to state-of-the-art psychotherapy such as CBT treatment for PTSD is still limited and uneven. For example, it was shown that less than 20% of the hospitals in Canada had an anxiety disorders clinic and these clinics were mainly in urban areas (Swinson, Cos, Kerr, & Kuch, 1992). Similar situations can be expected in many industrialized countries. Access to these specialized services can therefore be problematic for individuals living outside major urban centers, and especially in rural regions. This uneven access to professional resources is also exacerbated by the fact that some people with severe or chronic problems cannot travel to the available resources for a variety of reasons (e.g., disability, avoidance behaviors, lack of energy; Riemer-Reiss, 2000).
In that context, telepsychotherapy offered by videoconference constitutes an interesting solution. Videoconferencing is a technological procedure that allows individuals to see and hear each other on a computer monitor or video screen in real time. Hence, it enables individuals in different locations to interact simultaneously. Telepsychotherapy via videoconference can thus serve as a solution to provide these specialized services remotely, to mitigate the unequal distribution of resources, and to reduce the increasingly high cost of health care (Koocher & Morray, 2000; Riemer-Reiss, 2000). Moreover, telepsychotherapy opens up the possibility of offering psychological services to people who cannot travel to the places where the most effective health care services are located or cannot receive the services they need within a reasonable time period (Jerome et al., 2000). It can increase timely access to mental health care, while reducing travel, wait lists, and transfers of clients to specialized centers. Furthermore, telepsychotherapy makes it easier for local clinics to provide their patients in special situations (e.g., linguistic or cultural minorities) with psychological services adapted to their needs. Finally, telepsychotherapy can allow for an extremely fast reallocation of additional professional resources for crisis situations such as natural disasters and mass shootings, which can rapidly overload the locally available professional resources. Videoconferencing psychotherapy is thus an innovative intervention and it is important to empirically examine its effectiveness before promoting its use.
EFFICACY OF CBT VIA VIDEOCONFERENCE FOR ANXIETY DISORDERS
The efficacy of CBT via videoconference has already been compared to face-to-face treatments for various problems including panic attacks (Allard et al., 2007; Bouchard et al., 2004) and PTSD (Frueh et al., 2007; Germain, Marchand, Bouchard, Drouin, & Guay, 2009; Morland, Pierce, & Wong, 2004), and the results suggest that the efficacy of a videoconference treatment is equivalent to that of a face-to-face treatment. Frueh et al.’s (2007) study and Morland et al.’s (2004) study compared the efficacy of a group CBT with veterans via either videoconferencing or face-to-face treatment. Germain et al.’s (2009) study assessed individual CBT for PTSD with civilians and showed that individual CBT via videoconferencing was as effective as it was face-to-face (n = 24 and n = 44, respectively, for the intent-to-treat sample). Participants improved significantly between the beginning and the end of their therapy with regard to posttraumatic symptomatology, levels of anxiety and depression, level of functioning in their everyday life, and perception of their physical and mental health. However, only the impact of the intervention one week posttreatment was published because the follow-up was not completed at that time.
This study presents, for the first time, the follow-up of Germain et al.’s (2009) preliminary study, the intent-to-treat results for the whole study (see later), and a new indicator of relative efficacy. The first goal is to compare, six months after the end of the psychotherapy, the effectiveness of a video-conference administration of a CBT for PTSD to a face-to-face administration. The second goal is to present, both for the posttreatment assessment and the follow-up assessment, two global indicators of treatment efficacy (proportions of reliable changes and of clinically significant changes) and a new indicator called relative efficacy. Relative efficacy represents the expected efficacy of videoconference treatments as a proportion of the expected efficacy of face-to-face treatments. This index is designed to help clinicians, managers, board members, and public agencies make an informed decision when they have to decide whether or not a videoconference treatment program should be implemented.
METHOD
Participants
Sixty-eight participants with PTSD as a primary diagnosis took part in the study (44 in the face-to-face condition and 24 in the videoconference condition). These numbers are larger than those published in Germain et al.’s (2009) preliminary study because this article includes the non-completers (i.e., the dropouts), whereas the previous article exclusively presented results for the completers. However, the two articles refer to the same sample. Participants were recruited through public advertisement in newspapers and through references from psychiatrists and other health practitioners who knew about one of the two anxiety clinics involved in the project. These health practitioners were informed that the anxiety clinics provided CBT treatments for individuals diagnosed with PTSD and they gave the contact information of the closest of the two anxiety clinics to their patients when they judged it relevant. These referring practitioners were not involved in the evaluation, nor in the treatment provided at the anxiety clinic. One of the clinics was in Montréal and the other was in a remote region. Individuals were excluded from the study if they had a secondary diagnosis of schizophrenia, organic brain disorder (e.g., dementia), severe personality disorder, intellectual disability, substance abuse or dependency, or a physical condition that would contraindicate participation in the study, especially in the videoconferencing condition (e.g., epilepsy or vision problems). In addition, each participant had to agree to continue using the psychotropic medication already prescribed to him or her and to refrain from starting a new psychotropic medication and from participating in any other form of psychotherapy during the treatment. This requirement was explained to participants just before the signature of the consent form. We did not monitor the participants’ compliance with these requirements, but their primary caregiver was informed of the requirements and participants were asked to inform their therapist of any subsequent change. All therapists administered treatment from Montréal. Because face-to-face treatment was only provided at Montréal, a completely random assignment to treatment conditions was impossible. Participants recruited in Montréal were randomly assigned but those in the remote region were automatically assigned to the videoconference condition.
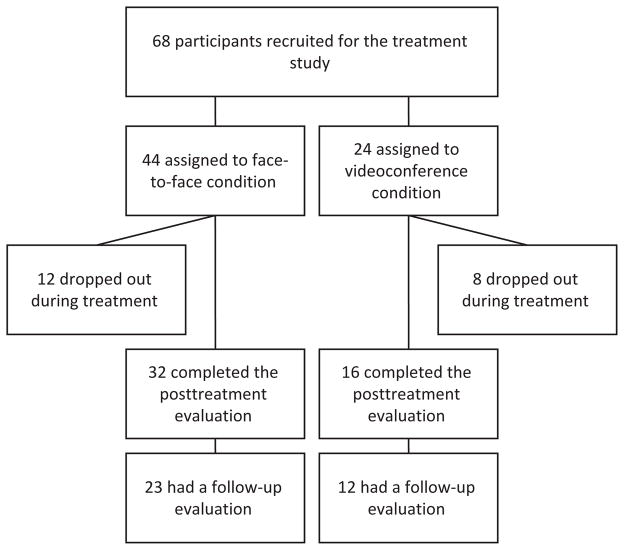
A total of 32 of the 44 individuals who were assigned the face-to-face condition (i.e., 73%) and 16 of the 24 individuals (i.e., 67%) who were assigned the videoconference condition completed the treatment. Out of these, 24 individuals in the face-to-face condition and 12 individuals in the videoconference condition continued until the follow-up evaluation. The complete flowchart of the participants is presented in Figure 1.
FIGURE 1.
Study flowchart.
No statistical difference was found between the two groups (videoconference vs. face-to-face) on their pretreatment symptomatology, sociodemographic information, time since trauma, or on the proportion of individuals for each type of trauma (p > .05) except for the proportion of individuals in a relationship (i.e., married or common law), which was higher for those in the face-to-face condition (58% vs. 30%). The characteristics of the sample were thus calculated for the whole group (n = 68) instead of separately (n = 44 vs. n = 24). The average age was 42.1 years old (SD = 12.1, range = 18–65), 64% of the participants were female, and 40% had a university degree (vs. 60% with either a high school or college degree). In addition, self-report measures of the treatment expectancies and the therapeutic alliance showed equivalent levels for the two treatment modalities (for more details, see Germain, Marchand, Bouchard, Guay, & Drouin, 2010). The clinical characteristics of the whole sample are presented in Table 1.
TABLE 1.
Descriptive Statistics of the Complete Intent-to-Treat Sample
| Variable | M (SD) or % | Range |
|---|---|---|
| Type of trauma | 36% | |
| Physical or sexual aggression | 36% | |
| Traffic accident | 22% | |
| Witnessing to a traumatic event | 16% | |
| Othera | 25% | |
| Time since trauma (months) | 64.5 (79.4) | 1–411 |
| PTSD symptoms | ||
| MPSS (PTSD-specific) | 73.1 (22.0) | 23–115 |
| BDI (depression) | 28.2 (11.6) | 3–56 |
| BAI (anxiety) | 22.4 (12.6) | 1–58 |
| Comorbid disorders | ||
| Mood disorders only | 24% | |
| Anxiety disorders only | 22% | |
| Mood and anxiety disorders | 16% | |
| None | 37% |
Note. n = 68. PTSD = posttraumatic stress disorder; MPSS = Modified PTSD Symptom Scale; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory.
The Other category includes victims of workplace accidents, war veterans, and victims of psychological harassment.
Material
Videoconferencing system
The equipment in the therapy room included, at each of the two anxiety clinics, an 81-cm television screen, a video camera, a phone, a fax machine, and either a Tandberg 2500 or a Tandberg 5000 system. Videoconferencing data were transmitted at 384 kilobytes per second and a technician remained available in case of technical problems. The fax machine was used to allow the therapist to send and receive written material during the therapy (e.g., exercises, schemas, etc.) but all the questionnaires were provided on site.
Modified PTSD Symptom Scale
The Modified PTSD Symptom Scale (MPSS [French-Canadian version]; Guay, Marchand, Iucci, & Martin, 2002; Resick, Falsetti, Resnick, & Kilpatrick, 1991) is a self-administered 17-item questionnaire that measures the frequency and severity of PTSD symptoms experienced during the last two weeks. The maximum overall score for PTSD is 119. A score of 50 or more is generally the cutoff point in determining the presence of PTSD (Guay et al., 2002). The MPSS has excellent internal consistency, with an alpha of .97 for the overall scale and .95 for each subscale (frequency and severity). It also has excellent construct validity, with a sensitivity level of .97 and a specificity level of .90 (Guay et al., 2002). The MPSS was used in this study as the main indicator of symptomatology.
The Beck Depression Inventory–Second Edition
The Beck Depression Inventory–Second Edition (BDI–II [French-Canadian version]; Beck, Steer, Ball, & Ranieri, 1996) includes 21 items enumerating depression symptoms. For each item, a list of four statements describes different symptom intensity. The respondent chooses the statement best reflecting his or her state over the last seven days. Each item is rated on a scale from 0 to 3, and total score ranges from 0 to 63. The BDI–II has been extensively validated and good psychometric properties have been reported (Beck et al., 1996; Dozois, Dobson, & Ahnberg, 1998). For the French version, Cronbach’s alpha is .82 and the 3-month test–retest reliability is .75 (Gauthier, Morin, Thériault, & Lawson, 1982). The BDI–II total score was used as a secondary indicator of symptomatology for depressive symptoms.
The Beck Anxiety Inventory
The Beck Anxiety Inventory (BAI [French version]; Beck & Steer, 1993) is a 21-item self-report questionnaire targeting cognitive and somatic symptoms of anxiety. The respondent chooses the statement best reflecting his or her state over the last seven days. Each item is rated on a scale from 0 to 3, and total score ranges from 0 to 63. This instrument has good psychometric properties (Freeston, Ladouceur, Thibodeau, Gagnon, & Rhéaume, 1992). Cronbach’s alphas were .85 to .93 in samples suffering from anxiety disorders (Beck & Steer, 1993). The BAI total score was used as a secondary indicator of symptomatology for anxious symptoms.
SF-12 Version 2.0 Health Survey
The SF-12 Version 2.0 Health Survey (SF12 [French version]) is a 12-item self-administered scale assessing perceived health with two dimensions, perceived physical health (SF12-physical) and perceived mental health (SF12-mental; Ware, Kosinski, Turner-Bowker, & Gandeck, 2007). The original English version was validated, and 2-week test–retest reliability coefficients are very good (r = .76–.89; Ware, Kosinski, & Keller, 1996). The scores were calculated according to the scoring method of the SF–12 presented in the User’s Manual for the SF-12v2™ Health Survey and the 1998 norms (Ware et al., 2007). The SF12-mental and SF12-physical were used as secondary indicators of symptomatology.
Procedure
After being recruited, participants were administered 16 to 25 weekly 60-minute sessions of CBT for PTSD, either face-to face or via videoconference. Symptom levels were evaluated one month before the intervention, at pre-treatment, at posttreatment, and at the follow-up evaluation (six months after treatment). The research project was approved by the Ethics Board Committee of the Louis H. Lafontaine Hospital, of the Pierre-Janet Hospital, and of the universities involved in the project. The details of the procedure are summarized in this section.
Assessment interviews
The first interview began with an explanation of the protocol, requirements, and purpose of the project, and signature of the consent form. After that, the diagnosis of PTSD was established using a semistructured diagnostic interview, the Structured Clinical Interview for DSM–IV (SCID–IV; First, Spitzer, Gibbon, & Williams, 1995). Interviews were audiotaped. The interrater reliability of the SCID assessment between two independent evaluators was evaluated from audiotapes and resulted in a kappa of 0.84. This interview also allowed one to assess the presence of comorbid disorders in participants. In addition, participants were required to fill out self-report questionnaires. The four evaluation interviews (i.e., one month before treatment, at pretreatment, at posttreatment, and for the follow-up at six months) followed the same procedure. The assessment interviews were never done by the treating psychologist.
Treatment
Participants in the videoconferencing condition received an average of 21 one-hour sessions of CBT and those in the face-to-face condition received an average of 19 one-hour sessions. The therapy consisted of five successive modules: A psychoeducational module about PTSD (conceptualization of PTSD, information on normal stress reactions), anxiety and stress management training (problem solving, cognitive restructuring, progressive relaxation), imaginary exposure to avoided situations, in vivo exposure to avoided situations (when relevant), and relapse-prevention strategies (definition of relapse, identification of associated risks; Foa, 2000). Therapy was administered by psychologists who had an average of 5 years of experience with CBT and in-depth knowledge of PTSD. Four psychologists treated most participants and provided therapy to participants in both conditions, making it possible to mitigate any potential bias attributable to the therapists. Seven other therapists took part in the project more sporadically and each of them treated from one to five participants. For logistical reasons, they were only involved in the face-to-face condition. Supervision by a psychologist with approximately 20 years of experience with the treatment of PTSD was also available twice a month for the therapists. All therapists were female. The average number of years of experience of the therapists was equivalent between conditions. The treatment protocol proposed a specific number of sessions for each of the five successive modules, but that number remained partly flexible and adapted to each participant’s needs. Sessions were audiotaped to assess therapeutic integrity. Integrity was assessed for a random sample of 25% of the treatment sessions and included sessions from each of the five successive modules of the psychotherapy (e.g., the psychoeducational module, the anxiety and stress management training) to ensure an adequate assessment. The assessment of treatment integrity was done by four separate evaluators trained in CBT who used a treatment rating chart to assess a subsample of the sessions. None of the sessions were assessed by more than one evaluator, so no measure of interrater agreement could be calculated. However, there was no statistical difference in the average treatment integrity between evaluators, and there was no statistical difference in treatment integrity between the two conditions. The mean overall integrity rating was 95%, which implies that 95% of the interventions conformed to the treatment protocol (i.e., CBT techniques for the treatment of PTSD), and 5% of the interventions did not conform to the treatment protocol (e.g., reassurance, passive listening, psychodynamic interpretations, distraction).
Analytic procedure
Germain et al.’s (2009) sample exclusively included the participants who completed the treatment (i.e., the completers). For this article, the main analyses used an intent-to-treat (ITT) approach; that is, they included both completers and noncompleters. Readers should thus be careful when comparing number of participants and effect sizes between the two. The ITT approach was implemented using the last-observation-carried-forward method. ITT analyses of treatment effects are considered to provide more valid and reliable results than as-treated (AT) analyses (e.g., Ellenberg, 1996). However, for a treatment equivalence study such as this one, an ITT approach can also produce a liberal bias because it artificially reduces the difference between the two group means. Consequently, AT analyses (i.e., analyses of the completers) were also done to confirm that a potential equivalence was not due to a methodological artifact of the ITT approach. Preliminary analyses were also done to assess the presence of validity problems with the AT analyses.
To compare the effectiveness of the videoconference and the face-to-face treatment after six months, a separate analysis of variance (ANOVA) for repeated measures was computed for the main indicator of symptomatology (MPSS-total) and for each of the secondary indicators of symptomatology. To compare treatment efficacy in more clinical terms, the proportion of reliable changes and of clinically significant changes were compared between the two conditions both at posttreatment and after six months. Finally, the index of relative efficacy was calculated both at posttreatment and after six months to facilitate decisions concerning the implementation of a videoconference treatment program. The details of the calculations are presented next.
RESULTS
Preliminary Analyses
Preliminary analyses confirmed that (a) the proportion of dropouts between the face-to-face condition and the videoconference conditions were not statistically different, both at posttreatment and follow-up (p > .05), and (b) individuals who dropped out (either before or after the posttreatment evaluation) were not statistically different from the others (p > .05) on their pretreatment level of symptomatology, sociodemographic information, and the proportion of individuals for each type of trauma. Consequently, it was decided that threats to the validity were not major enough to prevent the AT analyses to be useful as complementary analyses.
Descriptive Statistics
Nearly half (46%) of the participants assigned to the videoconference condition and 48% of the participants in the face-to-face condition no longer met the diagnostic criteria for PTSD at the posttest (ITT proportions). At the six-month follow-up, the proportion of participants who no longer met the diagnostic criteria for PTSD was 33% for the videoconference condition and 56% for the face-to-face condition. Group differences were assessed using the Newcombe–Wilson method without corrections (Newcombe, 1998) but none was statistically significant (p > .05). The size of the symptom reduction effect (i.e., the pretest–posttest difference) for both videoconference and face-to-face psychotherapy was first evaluated for each of the seven outcome variables both at posttreatment and at follow-up using an ITT approach (see Table 2 for details). The main AT results are also presented.
TABLE 2.
Mean Symptoms Reduction from Pretreatment and 95% Confidence Intervals at Posttreatment and at Follow-Up Both for Videoconference and Face-to-Face Cognitive-Behavioral Therapy
| Face-to-face
|
Videoconference
|
|||
|---|---|---|---|---|
| M | 95% CI | M | 95% CI | |
| At follow-up (ITT results) | n = 32 | n = 16 | ||
| MPSS-total | −23.0 | −32.1 to −13.8 | −22.8 | −34.7 to −10.9 |
| MPSS-fr | −9.5 | −13.4 to −5.5 | −9.3 | −14.1 to −4.6 |
| MPSS-se | −13.5 | −18.8 to −8.1 | −13.5 | −20.8 to −6.1 |
| BDI | −7.2 | −11.0 to −3.3 | −6.5 | −11.7 to −1.3 |
| BAI | −3.7 | −7.4 to 0.1 | −6.2 | −11.9 to −0.4 |
| SF12-physical | 1.8 | 0.2 to 3.5 | 5.2 | 2.4 to 7.9 |
| SF12-mental | 5.5 | 1.7 to 9.3 | 4.1 | −0.7 to 8.9 |
| At posttreatment (ITT results) | n = 23 | n = 12 | ||
| MPSS-total | −24.6 | −34.2 to −15.0 | −17.6 | −29.0 to −6.3 |
| MPSS-fr | −10.4 | −14.5 to −6.3 | −7.0 | −11.6 to −2.4 |
| MPSS-se | −14.2 | −19.8 to −8.5 | −10.6 | −17.6 to −3.7 |
| BDI | −6.7 | −11.4 to −2.0 | −5.8 | −11.2 to −0.4 |
| BAI | −5.0 | −8.5 to −1.5 | −7.0 | −12.7 to −1.3 |
| SF12-physical | 2.5 | 0.5 to 4.4 | 5.1 | 2.0 to 8.2 |
| SF12-mental | 5.8 | 1.5 to 10.0 | 4.0 | 0.0 to 8.0 |
| Main as-treated results | ||||
| MPSS-total (follow-up) | −33.4 | −47.1 to −19.7 | −38.1 | −58.0 to −18.2 |
| MPSS-total (posttreatment) | −33.8 | −45.6 to −21.9 | −25.3 | 42.2 to −8.5 |
Note. A negative effect implies a symptom reduction except for the SF-12, for which the logic is reversed.
ITT = intent-to-treat; MPSS = Modified PTSD Symptom Scale; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; SF12 = SF-12 Version 2.0 Health Survey.
Treatment Comparison after Six Months
A separate ANOVA for repeated measures was done on the ITT data for the follow-up on each of the seven outcome variables to evaluate if there was a group effect (overall videoconference vs. face-to-face differences), a time effect (overall follow-up vs. baseline difference), or an interaction (i.e., a differential effect of group over time). As seen in Table 3, a time effect was systematically found for each outcome (i.e., symptoms are less intense at follow-up than at baseline) but none of the group or interaction effects were statistically or clinically significant (i.e., η2 ≤ 0.02) except for the interaction for the SF12-physical, which shows a slight advantage for the videoconference condition. Thus, the effects of videoconference psychotherapy on symptoms after six months are generally not statistically different from the effects of face-to-face psychotherapy on symptoms.
TABLE 3.
Comparison between Videoconference and Face-to-Face Psychotherapy at Follow-Up (Intent-to-Treat Results)
| Outcome | Time effect
|
Group effect
|
Interaction effect
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| F(1, 65) | p | η2 | F(1, 65) | p | n2 | F(1, 65) | p | η2 | |
| MPSS-total | 37.86 | .00 | 0.37 | 0.46 | .50 | 0.01 | 0.00 | .98 | 0.00 |
| MPSS-frequency | 36.02 | .00 | 0.36 | 0.09 | .77 | 0.00 | 0.00 | .96 | 0.00 |
| MPSS-severity | 36.87 | .00 | 0.36 | 0.84 | .36 | 0.01 | 0.00 | 1.00 | 0.00 |
| BDI | 18.46 | .00 | 0.22 | 0.19 | .67 | 0.00 | 0.05 | .83 | 0.00 |
| BAI | 9.60 | .00 | 0.13 | 0.02 | .90 | 0.00 | 0.58 | .45 | 0.01 |
| SF12-physical | 22.67 | .00 | 0.26 | 0.77 | .38 | 0.01 | 5.10 | .03 | 0.07 |
| SF12-mental | 9.94 | .00 | 0.13 | 1.61 | .21 | 0.02 | 0.21 | .65 | 0.00 |
Note. MPSS = Modified PTSD Symptom Scale; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; SF12 = SF-12 Version 2.0 Health Survey.
Using the AT data, the ANOVAs produced extremely similar F and p values and slightly larger effect sizes (i.e., η2 values), resulting in identical statistical decisions except for the interaction for the SF12-physical (p = .07). The quasi-equivalence between the ITT results and the AT results supports the idea that the lack of statistically significant differential effect of group over time for most symptom scales in the ITT analyses was not due to methodological artifacts specific to the ITT procedure.
Clinically Relevant Indicators of Change at Posttreatment and after Six Months
Clinically relevant indicators of change are more and more frequently presented in clinical studies in addition to traditional measures of symptom reduction. For this study, both Jacobson’s Reliable Change Index (RC) and Clinically Significant Change—criterion C (CS) were computed as indicators of change (Jacobson & Truax, 1991). Each indicator was computed both for the MPSS-severity and the MPSS-frequency and then averaged between the two MPSS subscales to produce a value based on the global MPSS score. The results are presented both for the posttreatment and the follow-up and both for the ITT and AT analyses (see Table 4). As an example of interpretation (using the ITT results), 38% of the participants in the videoconference condition had a clinically significant improvement between their pretreatment evaluation and their follow-up evaluation. We could thus expect between 21% and 57% of patients to have such a clinically significant improvement in similar conditions, with a 95% level of confidence.
TABLE 4.
Rates of Success and 95% Confidence Intervals in Terms of Reliable Change and Clinically Significant Change both for Intent-to-Treat (ITT) and As-Treated (AT) Analyses
| Face-to-face
|
Videoconference
|
|||
|---|---|---|---|---|
| Success rate | 95% CI | Success rate | 95% CI | |
| At follow-up (ITT) | n = 32 | n = 16 | ||
| Reliable change | 55% | 40–69% | 56% | 37–74% |
| Clinically significant change | 42% | 28–57% | 38% | 21–57% |
| At posttreatment (ITT) | n = 23 | n = 12 | ||
| Reliable change | 55% | 40–69% | 48% | 30–67% |
| Clinically significant change | 47% | 33–61% | 33% | 18–53% |
| At follow-up (AT) | n = 32 | n = 16 | ||
| Reliable change | 74% | 54–87% | 87% | 57–97% |
| Clinically significant change | 57% | 37–75% | 52% | 27–76% |
| At posttreatment (AT) | n = 23 | n = 12 | ||
| Reliable change | 73% | 55–85% | 71% | 47–88% |
| Clinically significant change | 61% | 44–77% | 49% | 27–71% |
Relative Efficacy of Videoconference at Posttreatment and after Six Months
Confidence intervals of the relative efficacy of the videoconference condition were calculated to assess the consequences of implementing a videoconference program. Relative confidence intervals were calculated for the two most clinically relevant indicators, the main outcome variable (MPSS-total) and the Clinically Significant Change. An adaptation of Tryon’s (2001) inferential confidence intervals (ICIs) was used, and the confidence intervals represent the range of probable values of the decrease (or increase) in efficacy (i.e., mean symptom reduction or rate of success) that would result from choosing to implement a videoconference program instead of a face-to-face program (the reference group). This probability is expressed as a proportion of the efficacy that would be expected from a face-to-face program in similar conditions (for a similar use of Tryon’s ICI, see Beaulieu-Prévost & Zadra, 2007).
To compute the mean of the relative efficacy, we subtracted the face-to-face value from the videoconference value and divided the result by the face-to-face value. To compute the confidence intervals of the relative efficacy, the steps were to (a) calculate Tryon’s ICI for the difference between the two groups (for more details, see Tryon, 2001); (b) calculate the lower limit of the confidence interval by subtracting the upper limit of the face-to-face condition from the lower limit of the videoconference condition and dividing the result by the upper limit of the face-to-face condition; and (c) calculate the upper limit of the confidence interval by subtracting the lower limit of the face-to-face condition from the upper limit of the videoconference condition and dividing the result by the lower limit of the face-to-face condition. The results are presented in Table 5.
TABLE 5.
Relative Efficacy and 95% Confidence Intervals of Videoconference Compared to Face-to-Face in Terms of MPSS Total Score and Clinically Significant Change
| At posttreatment
|
At follow-up
|
|||
|---|---|---|---|---|
| Efficacy | 95% CI | Efficacy | 95% CI | |
| Intent-to-treat results | ||||
| MPSS-total | −28% | −68 to +41% | −1% | −50 to +85% |
| Clinically significant change | −28% | −63 to +26% | −10% | −53 to +58% |
| As-treated results | ||||
| MPSS-total | −25% | −66 to +42% | +14% | −40 to +110% |
| Clinically significant change | −21% | −57 to +30% | −9% | −51 to +60% |
Note. MPSS = MPSS = Modified PTSD Symptom Scale.
Interpretation and Use of Relative Efficacy Indicators
As mentioned earlier, the data presented in Table 5 can be used to assess the relative efficacy of the videoconference condition in comparison to the traditional face-to-face condition and to decide whether or not it is an adequate decision to implement a videoconference treatment program. However, because this method is new, two examples of interpretations follow. First, by using the ITT result of the MPSS-total as the indicator of therapeutic success, it can be estimated (with a 95% confidence level) that after six months, choosing to implement videoconference treatments would result in the worst case scenario in 50% less symptom reduction on average than with a face-to-face treatment program, in the best case scenario in 85% more symptom reduction on average than with a face-to-face treatment program (i.e., nearly twice the efficacy compared to face-to-face treatments), and in the most probable scenario in 1% less symptom reduction on average than with a face-to-face treatment program. Second, if the ITT result of the CS index is used as the indicator of therapeutic success, it can be estimated (with a 95% confidence level) that after six months, choosing to implement videoconference treatments would result in the worst case scenario in 53% less patients with a clinically significant change than with a face-to-face treatment program, in the best case scenario in 58% more patients with a clinically significant change than with a face-to-face treatment program, and in the most probable scenario in 10% less patients with a clinically significant change than with a face-to-face treatment program. The ITT results should be used to assess the relative efficacy of videoconference treatments for a population of PTSD patients entering treatment (including those who will eventually drop out of the treatment), whereas the AT results should be used to assess the relative efficacy of videoconference treatments for those who will continue the treatment until the end.
DISCUSSION
The study shows that the efficacy of a standard CBT for PTSD is equivalent whether done face-to-face or by videoconference. The levels of post-traumatic symptoms, anxiety, depression, and perceived health improved substantially during treatment in both conditions and these gains were maintained after six months. The proportion of dropouts was also equivalent between the two conditions, which suggests that the videoconference condition is not associated with increased risks of treatment noncompletion. This equivalence between videoconference and face-to-face CBT is consistent with the literature (e.g., Bouchard et al., 2004) and expands on it by showing that it also applies to the treatment of PTSD and that the efficacy is maintained for at least six months.
There were still technical difficulties related to the videoconference condition. The signal was occasionally interrupted, the quality of the sound and image were suboptimal, and there was a short delay between the therapists’ and the clients’ responses. Consequently, the spontaneity of the exchanges was somewhat restricted and the therapists were occasionally unsure of their clients’ emotional expression. However, the results of the study demonstrate that these difficulties did not interfere with treatment efficacy.
Some elements should still be taken into account before generalizing the results. The main limitation is that participants could not be randomly assigned to the treatment condition. Preliminary analyses showed that the two groups were equivalent in terms of pretreatment symptomatology, therapeutic expectations and alliance, and sociodemographic characteristics (except for the proportion of individuals in a relationship), but it is still possible that the two groups were not equivalent on potentially important variables not measured in this study. In addition, because a small proportion of the therapists were only involved in the face-to-face condition, the presence of a therapist effect in the results cannot be completely ruled out. Also, even though the main indicators of improvement were quite comparable between the two groups, there was a noticeable but statistically nonsignificant trend for participants at the six-month follow-up to lose their PTSD diagnosis more frequently after a face-to-face therapy (56%) than after video-conference therapy (33%) and a slight but statistically nonsignificant trend for face-to-face treatments to be more associated with improvement at posttreatment. Thus, randomized treatment studies with more participants are still required before a strong argument for the equivalence of videoconference and face-to-face treatments of PTSD can be offered.
This study also has important methodological strengths that should be taken into account. It used a larger sample than most other studies, the protocol was based on a standardized treatment manual and on reliable and valid clinical measures, and it included a six-month follow-up. Compared to other videoconference studies on PTSD, this study has the largest sample and it is the only one to include a six-month follow-up to assess individual CBT (instead of group therapy), and to be done with civilians.
The decision to implement videoconference psychotherapy for PTSD can only be taken on a case-by-case basis and it is influenced by factors such as the relative cost and availability of each option and by the definition of success used by the decision maker (i.e., symptom reduction, rate of reliable changes, rate of clinically significant changes). However, the measures of relative efficacy can already inform decision makers about the relative risks and advantages of each option because they provide estimations for the worst, average, and best case scenarios in terms of relative efficacy. Incidentally, the ITT values and the AT values are very similar so the following conclusion applies to both populations.
As mentioned earlier, a replication of this study with a randomized design and a larger sample will be necessary before concluding with certainty that videoconferencing is equivalent to face-to-face delivery of CBT for PTSD. However, these preliminary results can help clinicians, health care managers, and policymakers make informed decisions about the use of videoconferencing to treat PTSD. For clinicians, these results suggest that a relatively equivalent PTSD symptom reduction could be expected from a videoconference CBT treatment and a face-to-face CBT treatment. For health care managers, the results suggest that at least in situations in which the cost of implementing videoconference treatments is not a major problem, it could potentially be a viable alternative to face-to-face treatments of PTSD in terms of treatment efficiency, especially when adequate face-to-face treatments are less available (e.g., in remote and rural areas). For policymakers, making videoconference treatments more available as a treatment option in a network of clinics and hospitals (e.g., a country’s public health care system) could be a potential solution to improve the efficiency and flexibility of the whole network at a structural level.
Whenever possible, it is probably better to keep face-to-face interventions as the primary way to deliver psychotherapeutic services, even if treatment equivalence is later confirmed. Videoconferencing requires more technical resources (e.g., a technician on site) and is still less reliable than face-to-face interventions due to its additional technological complexity and reliance on the communication network. It also tends to centralize the resources in the health care network compared to face-to-face services. However, considering that videoconference CBT treatments are potentially as efficient as face-to-face treatments (at least for PTSD), developing CBT videoconferencing resources in a health care network that mainly delivers face-to-face services might be an interesting solution to attempt to improve the efficiency and flexibility of the health care network.
Acknowledgments
This study was made possible because of (a) a grant from the Social Sciences and Humanities Research Council of Canada (SSHRC); (b) research and infrastructure funding from the Canada Research Chairs, the Canadian Institutes of Health Research, and the Canada Foundation for Innovation; (c) a fellowship from the Fond Uniprix; and (d) an SSHRC Graduate Scholarship. We are thankful to the Centre de recherche Fernand-Séguin and the Centre d’étude sur le trauma at the Hôpital Louis-H. Lafontaine, the Centre hospitalier Pierre-Janet, and the cyberpsychology laboratory at the Université du Québec en Outaouais for their ongoing support throughout the project. The authors also thank the psychologists and the participants who took part in the project, without whom this study could not have become a reality.
Contributor Information
ANDRÉ MARCHAND, Département de psychologie, Université du Québec à Montréal, Montréal, Québec, Canada; and Centre d’Étude du Trauma, Hôpital Louis-H. Lafontaine, Montréal, Québec, Canada.
DOMINIC BEAULIEU-PRÉVOST, Centre d’Étude du Trauma, Hôpital Louis-H. Lafontaine, Montréal, Québec, Canada; and Département de psychologie, Université de Montréal, Montréal, Québec, Canada.
STÉPHANE GUAY, Centre d’Étude du Trauma, Hôpital Louis-H. Lafontaine, Montréal, Québec, Canada; and Département de psychologie, Université de Montréal, Montréal, Québec, Canada.
STÉPHANE BOUCHARD, Département de psychologie, Université du Québec en Outaouais, Gatineau, Québec, Canada.
MARC SIMON DROUIN, Département de psychologie, Université du Québec à Montréal, Montréal, Québec, Canada.
VANESSA GERMAIN, Département de psychologie, Université du Québec à Montréal, Montréal, Québec, Canada.
References
- Allard M, Bouchard S, Marchand A, Cournoyer LG, Green-Demers I, Renaud P. L’efficacité de la psychothérapie pour le trouble panique en videoconference: Réplication et alliance thérapeutique [The efficacy of psychotherapy for panic disorder via videoconference: Replication and therapeutic alliance] Revue Québécoise de Psychologie. 2007;28:43–64. [Google Scholar]
- Beaulieu-Prévost D, Zadra A. Absorption, thinness of boundaries and attitude towards dreams as correlates of dream recall frequency: Two decades of research seen through a meta-analysis. Journal of Sleep Research. 2007;16:51–59. doi: 10.1111/j.1365-2869.2007.00572.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. 2. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories–IA and –II in psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Bouchard S, Paquin B, Payeur R, Allard M, Rivard V, Fournier T, et al. Delivering cognitive-behavior therapy for panic disorder with agoraphobia in videoconference. Telemedicine Journal and e-Health. 2004;10:13–25. doi: 10.1089/153056204773644535. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory–II. Psychological Assessment. 1998;10:83–89. [Google Scholar]
- Ellenberg JH. Intent-to-treat analysis versus as-treated analysis. Drug Information Journal. 1996;30:535–544. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM–IV Disorders: Patient edition. New York: New York State Psychiatric Institute, Biometrics Research Department; 1995. [Google Scholar]
- Foa EB. Psychosocial treatment of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2000;61:43–51. [PubMed] [Google Scholar]
- Freeston MH, Ladouceur R, Thibodeau N, Gagnon F, Rhéaume J. L’inventaire d’anxiété de Beck: Propriétés psychométriques d’une traduction française [Beck Anxiety Inventory: Psychometric properties of a French translation] L’Encéphale. 1992:47–55. [PubMed] [Google Scholar]
- Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized trial of telepsychiatry for post-traumatic stress disorder. Journal of Telemedicine & Telecare. 2007;13:142–147. doi: 10.1258/135763307780677604. [DOI] [PubMed] [Google Scholar]
- Gauthier J, Morin C, Thériault F, Lawson JS. Adaptation française d’une mesure d’auto-évaluation de l’intensité de la dépression [French adaptation of a self-reported measure of depression intensity] Canadian Journal of Behavioural Science. 1982;14:211–218. [Google Scholar]
- Germain V, Marchand A, Bouchard S, Drouin MS, Guay S. Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cognitive Behaviour Therapy. 2009;38:42–53. doi: 10.1080/16506070802473494. [DOI] [PubMed] [Google Scholar]
- Germain V, Marchand A, Bouchard S, Guay S, Drouin MS. Assessment of the therapeutic alliance in face-to-face or videoconference treatment for posttraumatic stress disorder. Cyberpsychology, Behavior, and Social Networking. 2010;13:29–35. doi: 10.1089/cyber.2009.0139. [DOI] [PubMed] [Google Scholar]
- Guay S, Marchand A, Iucci S, Martin A. Validation de la version québécoise de l’échelle modifiée des symptômes du trouble de stress post-traumatique auprès d’un échantillon clinique [Validation of the Quebec version of the Modified PTSD Symptoms Scale with a clinical sample] Revue Québécoise de Psychologie. 2002;23:257–270. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jerome LW, DeLeon PH, James LC, Folen R, Earles J, Gedney JJ. The coming age of telecommunication in psychological research and practice. American Psychologist. 2000;55:407–421. doi: 10.1037/0003-066X.55.4.407. [DOI] [PubMed] [Google Scholar]
- Koocher GP, Morray E. Regulation of telepsychology: A survey of state attorneys general. Professional Psychology: Research and Practice. 2000;31:503–508. [Google Scholar]
- Morland LA, Pierce K, Wong MY. Telemedicine and coping skills groups for Pacific Islander veterans with post-traumatic stress disorder: A pilot study. Journal of Telemedicine & Telecare. 2004;10:286–289. doi: 10.1258/1357633042026387. [DOI] [PubMed] [Google Scholar]
- Newcombe RG. Interval estimation for the difference between independent proportions: Comparison of eleven methods. Statistics in Medicine. 1998;17:873–890. doi: 10.1002/(sici)1097-0258(19980430)17:8<873::aid-sim779>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Resick PA, Falsetti SA, Resnick HS, Kilpatrick DG. The Modified PTSD Symptom Scale—Self-report. Charleston, SC: Crime Victims Treatment and Research Center, Medical University of South Carolina; 1991. [Google Scholar]
- Riemer-Reiss ML. Utilizing distance technology for mental health counseling. Journal of Mental Health Counseling. 2000;22:189–203. [Google Scholar]
- Swinson RP, Cos BJ, Kerr SA, Kuch KD. A survey of anxiety disorders clinics in Canadian hospitals. Canadian Journal of Psychiatry. 1992;37:188–191. doi: 10.1177/070674379203700308. [DOI] [PubMed] [Google Scholar]
- Tryon WW. Evaluating statistical difference, equivalence, and indeterminacy using inferential confidence intervals: An integrated alternative method of conducting null hypothesis statistical tests. Psychological Methods. 2001;6:371–386. [PubMed] [Google Scholar]
- Van Etten ML, Taylor S. Comparative efficacy of treatments for post-traumatic stress disorder: A meta-analysis. Clinical Psychology and Psychotherapy. 1998;5:126–144. [Google Scholar]
- Ware JE, Jr, Kosinski M, Keller SD. A 12-item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Kosinski M, Turner-Bowker DM, Gandeck B. User’s manual for the SF-12v2™ Health Survey (with a supplement documenting the SF-12® Health Survey) Lincoln, RI: QualityMetric Incorporated; 2007. [Google Scholar]