Abstract
Background
Pheochromocytoma (paraganglioma) of the urinary bladder is a rare tumor. Herein we sought to review the contemporary literature on pheochromocytomas of the urinary bladder in order to further illustrate the presentation, treatment options and outcomes of patients diagnosed with these tumors.
Methods
A comprehensive review of the current literature was conducted according to the PRISMA guidelines by accessing the NCBI PubMed database and using the search terms “paraganglioma, pheochromocytoma, bladder.” This search resulted in the identification of 186 articles published between January 1980 and April 2012 of which 80 articles were ultimately included in our analysis.
Results
Pheochromocytomas usually occurred in young adult Caucasians (mean age, 43.3 years; range,11–84 years). According to the literature, the most common symptoms and signs of pheochromocytomas of the urinary bladder were hypertension, headache, and hematuria. Of the 77 cases that commented on catecholamine production, 65 patients had biochemically functional tumors. Approximately 20% of patients were treated by transurethral resection alone, 70% by partial cystectomy and 10% by radical cystectomy. The 75 patients with follow-up information had a mean follow-up of 35 months. At the time of last follow-up, 15 (14.2%) had disease recurrence, 10 (9.4%) had metastasis, and 65 (61.3%) were alive.
Conclusions
Pheochromocytomas of the urinary bladder tend to be functional and occur mostly in young adult Caucasians. Patients with localized tumors have an extremely favorable prognosis and may be managed by less aggressive modalities, whereas patients with metastatic disease have a significant reduction in survival rates despite aggressive treatment.
Keywords: Paraganglioma, Pheochromocytoma, Bladder, Treatment, Diagnosis, Prognosis
Background
Pheochromocytoma of the urinary bladder is a rare tumor that originates from chromaffin tissue of the sympathetic nervous system associated with the urinary bladder wall. Pheochromocytomas are tumors of the sympathetic nervous tissue and may be non-functional or functional, i.e., secrete catecholamine causing paroxysmal hypertension, palpitation, and micturition syncope [1]. Typically these tumors possess the capacity to invade and thus are deemed malignant, yet lack mitoses and cellular dissociation that are usually associated with malignant tumors [2]. Numerous, small series case reports have been published in the English literature since it was first reported in 1953 by Zimmerman et al.[3]. Herein we sought to review the contemporary literature on pheochromocytoma of the urinary bladder in hopes of further clarifying presentation, treatment options and outcomes of patients with pheochromocytomas of the urinary bladder.
Methods
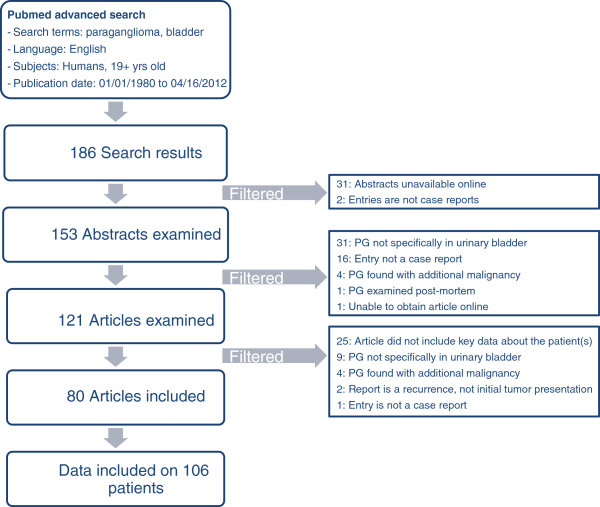
A review of the current literate was conducted by accessing the NCBI PubMed database (http://www.ncbi.nlm.nih.gov/pubmed). Filters applied in an advanced search included: the search terms of “paraganglioma, pheochromocytoma, bladder”; English language; human subjects 19 years of age and older; publication dates of January 1980 to April 2012. Figure 1 illustrates the work-flow of the comprehensive literature review, which adhered to the PRISMA systematic review guidelines [4]. This search delivered 186 results from which 153 abstracts were reviewed. A total of 121 articles were ultimately reviewed in full. Patient characteristics were divided into “primary” and “secondary” demographics for ease of data recording. Reasons for exclusion included missing any primary demographic (patient age, sex, presenting symptoms, type of surgery) or more than three secondary demographics (patient race, catecholamine levels, tumor size, tumor grade and stage, last follow up). Due to failure to report primary demographics and/or secondary demographics, an additional 25 articles eventually were excluded from final analysis. Thus the final analysis comprised 80 articles that reported on 106 patients. Relevant clinical, pathologic, laboratory, radiologic and follow-up data from these 80 articles were collected in a database, which allowed the reporting of descriptive statistics.
Figure 1.
Literature search schema.
Results
Eighty articles on pheochromocytoma of the urinary bladder were identified on Pubmed and were incorporated in our analysis, which included 106 patients [4-82]. The demographics and presenting symptomology are summarized in Table 1. The mean patient age was 43.3 years (range, 11–84 years). The male-to-female ratio was 1.07 to 1. The most common symptoms were hypertension (54.7%), headache (48.1%), hematuria (47.2%) and syncope/palpitations (43.4%). Micturition attacks were reported in 52.8% of patients.
Table 1.
Demographics and presenting symptoms
| Variable | N (%) |
|---|---|
|
Total Patients |
106 |
|
Sex |
|
| Males |
55 |
| Female |
51 |
|
Age |
|
| Mean age (years) |
43.3 |
| Age range (years) |
11-84 |
|
Presenting symptom(s) |
|
| Micturition attacks |
56 (52.8) |
| Hypertension |
58 (54.7) |
| Headache |
51 (48.1) |
| Hematuria |
50 (47.2) |
| Syncope/palpitations |
46 (43.4) |
| Diaphoresis |
21 (19.8) |
| Micturition disturbances (e.g., urgency, dysuria) |
11 (10.4) |
| Dizziness |
10 (9.4) |
| Abdominal/flank pain |
6 (5.7) |
| Dyspnea/chest pain |
5 (4.7) |
| Malaise |
3 (2.8) |
| Incidental finding |
3 (2.8) |
| Other |
11 (10.4) |
|
Catecholamines |
|
| ↑ VMA, metanephrine, or catecholamines |
65 (61.3) |
| Unknown/not mentioned |
29 (27.4) |
|
Tumor size |
|
| Mean (cm) |
3.9 |
| Median (range) (cm) |
3.45 (1.0-9.1) |
| Unknown/not mentioned | 26 (24.5) |
Average tumor size was 3.9 cm (median 3.45, range 1–9.1 cm). Few studies (n = 7) reported exact tumor stage by the TNM criteria. Of the 106 patients, 65 (61.3%) were noted to have a functional paraganglioma as evident by elevated VMA, metanephrine and/or catecholamines. Furthermore, limited articles reported on CD56, Chromagranin A, and synaptophysin immunohistochemical staining.
The most commonly reported treatment for patients with paraganglioma of the urinary bladder was partial cystectomy 73 (68.9%). Other treatment options for localized/locally advanced paraganglioma of the urinary bladder include TURBT (21; 19.8%) and radical cystectomy (12; 11.3%). Thirty-one patients included in this study did not have known follow-up. Mean follow of the remaining cohort was 34.6 months (median 18; range 0.75-372 months). Fifteen patients (14.2%) were noted to develop a recurrence of the tumor, while 60 patients (56.6%) had no evidence of disease. Metastatic recurrence was noted in ten patients (9.4%). Ten patients (9.4%) were deceased at last follow-up. Of these 10 patients who died, four (3.8%) presented with locally advanced or metastatic disease. Thus, patients who presented with localized paraganglioma of the urinary bladder have a significantly improved survival compared to patients who presented with locally advanced/metastatic disease.
Discussion
Pheochromocytomas of the urinary bladder are exceedingly rare tumors accounting for less than 0.05% of all bladder tumors and less than 1% of all pheochromocytomas. In the genitourinary tract, the urinary bladder is the most common site for pheochromocytomas (79.2%), followed by the urethra (12.7%), pelvis (4.9%), and ureter (3.2%) [82,83]. Furthermore, approximately 10% of all extra adrenal pheochromocytomas are malignant [83]. Since this is such a rare condition, limited, large reports are available to direct clinical decision making. We extensively reviewed the English literature on this subject and report the largest analysis of pheochromocytomas involving the urinary bladder. Our study improves upon previous large reviews [5,84]. For example, Tsai et al. includes one study dating back to 1911, and then eleven studies between 1989 and 2000 [5]. Our study includes 80 studies between 1980 and 2012, offering a better view for analyzing contemporary outcomes. In addition, we have a total of 106 patients included in our study, the most of any literature review to date, while Tsai et al. only reported on 53 patients. Lastly, our review used a multitude of demographics to depict the disease process of bladder pheochromocytomas, including presenting symptoms, tumor functionality, tumor size, treatment modality and outcomes.
Symptoms reported in the current literature range from the typical micturition attacks of headache and palpitations to more abstract signs such as paraesthesias and dyspnea. While select patients may lack more common presenting symptoms of bladder pheochromocytoma, e.g., hypertension, others may develop hematuria and lower urinary tract symptoms, testifying to the variability in which this disease can present itself. Furthermore, the consequences of hypertension itself may muddle the initial diagnostic picture of these patients. Patients often seek medical attention only when their hypertension has become so advanced as to cause syncope, retinopathy, or intracranial hemorrhage [85]. Physicians must constantly be wary of an undiagnosed pheochromocytoma in the setting of unexplained hypertension or associated symptoms.
Pheochromocytomas can be treated in a number of ways, including catecholamine blockade, surgery, chemotherapy, and radiation therapy. The standard treatment modality for localized or locally advanced pheochromocytomas is surgery, while metastatic or recurrent tumora are treated with palliative therapy [86]. Furthermore, physicians must be aware of poor prognostic indicators, such as large tumor size, advanced stage (≥T3), multifocal tumors, DNA ploidy, and CgA expression [84]. The cyclophosphamide, vincristine, and dacarbazine (the Averbuch protocol) has been shown to be effective against advanced malignant pheochromocytoma [87]. Radiation therapy with 131I-MIBG radiation therapy has been used with good efficacy for the treatment of MIBG-avid metastases [88]. Approximately 70% of patients included in our literature review underwent partial cystectomy as a means of primary treatment. Including those who underwent radical cystectomy, over 80% of patients were initially treated with aggressive surgical excision. Of the 75 patients with reported follow up, 15 (20%) experienced recurrence or metastasis at the time of last follow-up, illustrating that good symptomatic control and lower morbidity can be achieved with the surgical resection. It is important to note, however, that 4 of these 75 patients (5.3%) did have recurrence or metastases that ultimately caused their death. In the face of metastatic pheochromocytoma, surgical treatment is rarely curative. It may, however, adequately prolong survival by reducing comorbid conditions (i.e. hypertension) and reducing tumor burden, but adjunct therapies are usually indicated [89]. Thus patients should be counseled according to their individual presentation and disease status.
Furthermore, with a lack of high quality data and the lack of organizational guidelines (e.g., EAU, NCCN and AUA) on post-operative follow-up, we recommend no follow-up studies in patients with benign, localized disease. In patients with functional tumors, regardless of stage, VMA, metanephrine and catecholamines levels should be monitored within one month post-surgery, then every six months for two years. Furthermore if regional or metastatic is documented then axial imaging of the abdomen/pelvis should be performed every three months for one year, then every six months for one year, then yearly for three years.
The main limitations of our study relate to its retrospective nature and the large disparity among reporting styles of various institutions. For example, the vast majority of case reports included in this study report on patients presenting with localized or regional disease rather than metastatic disease. This may represent a bias toward reporting on patient’s who’s therapeutic timeline can better be used as an educational platform. The lack of uniformity on how oncologic cases are presented makes it difficult to characterize the true disease course of bladder pheochromocytoma. Information such as patient race, diagnostic findings, and laboratory values should be included whenever possible to better illustrate the pathophysiologic process. Currently, there is no standard staging system for pheochromocytomas. The National Cancer Institute at the National Institute of Health recommends dividing patients into three categories: localized, regional, and metastatic disease. In terms of grade and cellular classification of these tumors, the NCI identifies four pathologic features associated with malignancy: large tumor size, increased number of mitosis, DNA aneuploidy, and extensive tumor necrosis [86]. The complete tumor stage and grade are vital additions to any oncologic case report. Describing these characteristics and developing standard reporting criteria will enable future investigations to better collect and analyze information from case reports.
Conclusions
In summary, pheochromocytomas of the urinary bladder tend to be functional and occur mostly in young adult Caucasians. Initial presentation is extremely varied in these cancers, necessitating a low threshold of suspicion in the face of hypertension or hematuria. Patients with localized tumors have a favorable prognosis and may be managed by less radical modalities, whereas patients with metastatic disease have a significantly reduced survival rate. Moving forward, it would be helpful to standardize the reporting guidelines of pheochromocytomas cases to better understand the natural process and outcomes.
Abbreviations
AUA: American Urological Association; VMA: vanillylmandelic acid; H&E: Hematoxylin and eosin; IHC: Immunohistochemical
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JAB, BS: Acquisition of data, statistical analysis and drafting manuscript. AL, MD: Pathologic interpretation of case report and acquisition pathologic images. JH, MD: Analysis of data and drafting of manuscript. CJR, MD, MBA: Study concept and design, drafting of manuscript. All authors have read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Jonathan A Beilan, Email: jabeilan@knights.ucf.edu.
Adrienne Lawton, Email: Adrienne.Lawton@orlandohealth.com.
Julio Hajdenberg, Email: Julio.Hajdenberg@orlandohealth.com.
Charles J Rosser, Email: charles.rosser@orlandohealth.com.
Funding
Articles not available to the general public were retrieved through the University of Central Florida College of Medicine Library system and the UCF COM interlibrary loan system ILLiad. No other funding or outside resources were used for the completion of this study.
References
- Sheps SG, Jiang NS, Klee GG. Recent developments in the diagnosis and treatment of pheochromocytoma. Mayo Clin Proc. 1990;65:88–95. doi: 10.1016/S0025-6196(12)62113-2. [DOI] [PubMed] [Google Scholar]
- Zhou M, Epstein JI, Young RH. Paraganglioma of the urinary bladder: a lesion that may be misdiagnosed as urothelial carcinoma in transurethral resection specimens. Am J Surg Pathol. 2004;28:94–100. doi: 10.1097/00000478-200401000-00011. [DOI] [PubMed] [Google Scholar]
- Zimmerman IJ, Biron RE, Macmahon HE. Pheochromocytoma of the urinary bladder. N Engl J Med. 1953;249:25–26. doi: 10.1056/NEJM195307022490106. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai CC, Wu WJ, Chueh KS, Li WM, Huang CH, Wu CC, Lee MH, Chen SM. Paraganglioma of the urinary bladder first presented by bladder bloody tamponade: two case reports and review of the literatures. Kaohsiung J Med Sci. 2011;27(3):108–113. doi: 10.1016/j.kjms.2010.05.005. [DOI] [PubMed] [Google Scholar]
- Nayyar R, Singh P, Gupta NP. Robotic management of pheochromocytoma of the vesicoureteric junction. JSLS: Journal of the Society of Laparoendoscopic Surgeons/Society of Laparoendoscopic Surgeons. 2010;14:309–312. doi: 10.4293/108680810X12785289145042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey R, Garg R, Roy K, Darlong V, Punj J, Kumar A. Perianesthetic management of the first robotic partial cystectomy in bladder pheochromocytoma. A case report. Minerva Anestesiol. 2010;76:294–297. [PubMed] [Google Scholar]
- Oderda M, Michelon F, Appendino M. Primary bladder phaeochromocytoma diagnosed by a Vet. Scand J Urol Nephrol. 2010;44:186–189. doi: 10.3109/00365591003639202. [DOI] [PubMed] [Google Scholar]
- Vesin C, Cadi P, Thony F. A rare cause of complicated hypertension: urinary bladder paraganglioma. South Med J. 2009;102:1173–1175. doi: 10.1097/SMJ.0b013e3181b357de. [DOI] [PubMed] [Google Scholar]
- Huang Y, Tian XJ, Ma LL. Pre-peritoneal laparoscopic partial cystectomy of the bladder pheochromocytoma. Chin Med J. 2009;122:1234–1237. [PubMed] [Google Scholar]
- Dhawan DR, Ganpule A, Muthu V, Desai MR. Laparoscopic management of calcified paraganglioma of bladder. Urol J. 2008;5:126–128. [PubMed] [Google Scholar]
- Im SH, Kim NH. Thunderclap headache after micturition in bladder pheochromocytoma. Headache. 2008;48:965–967. doi: 10.1111/j.1526-4610.2008.01031.x. [DOI] [PubMed] [Google Scholar]
- Siatelis A, Konstantinidis C, Volanis D, Leontara V, Thoma-Tsagli E, Delakas D. Pheochromocytoma of the urinary bladder: report of 2 cases and review of literature. Italian J Urol Nephrol. 2008;60:137–140. [PubMed] [Google Scholar]
- Kappers MH, van den Meiracker AH, Alwani RA, Kats E, Baggen MG. Paraganglioma of the urinary bladder. Neth J Med. 2008;66:163–165. [PubMed] [Google Scholar]
- Zwahlen D, Fishman PN, Honey J, Milosevic M, Tannock I. Malignant pheochromocytoma of the urinary bladder. Can J Urol. 2007;14:3455–3457. [PubMed] [Google Scholar]
- Bhalani SM, Casalino DD, Manvar AM. Paraganglioma of the bladder. J Urol. 2011;186:279–280. doi: 10.1016/j.juro.2011.04.032. [DOI] [PubMed] [Google Scholar]
- Kang SG, Kang SH, Choi H, Ko YH, Park HS, Cheon J. Robot-assisted partial cystectomy of a bladder pheochromocytoma. Urol Int. 2011;87:241–244. doi: 10.1159/000324269. [DOI] [PubMed] [Google Scholar]
- Havekes B, Corssmit EP, Jansen JC, van der Mey AG, Vriends AH, Romijn JA. Malignant paragangliomas associated with mutations in the succinate dehydrogenase D gene. J Clin Endocrinol Metabol. 2007;92:1245–1248. doi: 10.1210/jc.2006-1993. [DOI] [PubMed] [Google Scholar]
- Tsutsui A, Omoto K, Eto M, Naito S. Unsuspected pheochromocytoma of the urinary bladder in an 81-year-old woman. Hinyokika Kiyo Acta Urologica Japonica. 2006;52:577–579. [PubMed] [Google Scholar]
- Bozbora A, Barbaros U, Erbil Y, Kilicarslan I, Yildizhan E, Ozarmagan S. Laparoscopic treatment of hypertension after micturition: Bladder pheochromocytoma. J Soc Laparoendoscopic Surgeons/Society of Laparoendoscopic Surgeons. 2006;10:263–266. [PMC free article] [PubMed] [Google Scholar]
- Dilbaz B, Bayoglu Y, Oral S, Cavusoglu D, Uluoglu O, Dilbaz S. Laparoscopic resection of urinary bladder paraganglioma: a case report. Surg Laparosc Endosc Percutan Tech. 2006;16:58–61. doi: 10.1097/01.sle.0000202194.51699.2a. [DOI] [PubMed] [Google Scholar]
- Segawa N, Osafune T. Malignant pheochromocytoma of the urinary bladder. Hinyokika Kiyo Acta Urologica Japonica. 2005;51:291–296. [PubMed] [Google Scholar]
- Minagawa T, Sato T, Furuhata M, Hirabayashi N, Kato H. Extra-adrenal pheochromocytoma (paraganglioma) of the urinary bladder: a case report. Hinyokika Kiyo Acta Urologica Japonica. 2004;50:787–790. [PubMed] [Google Scholar]
- Pastor-Guzman JM, Lopez-Garcia S, Gimenez-Bachs JM. Paraganglioma of the bladder: controversy regarding treatment. Urol Int. 2004;73:270–275. doi: 10.1159/000080841. [DOI] [PubMed] [Google Scholar]
- Jacob S, Prabhakar BR, Kakkar N, Mammen K. Paraganglioma of the urinary bladder–a case report. Indian J Pathol Microbiol. 2003;46:652–653. [PubMed] [Google Scholar]
- Yoshida S, Nakagomi K, Goto S, Kobayashi S. Malignant pheochromocytoma of the urinary bladder: effectiveness of radiotherapy in conjunction with chemotherapy. Int J Urol. 2004;11:175–177. doi: 10.1111/j.1442-2042.2003.00758.x. [DOI] [PubMed] [Google Scholar]
- Gasic S, Heinz-Peer G, Kurtaran A, Pirich C, Kratzik C, Koller A. Paroxysmal hypertension during micturition. Am J Hypertens. 2004;17:100–101. doi: 10.1016/j.amjhyper.2003.08.014. [DOI] [PubMed] [Google Scholar]
- Onishi T, Sakata Y, Yonemura S, Sugimura Y. Pheochromocytoma of the urinary bladder without typical symptoms. Int J Urol. 2003;10:398–400. doi: 10.1046/j.1442-2042.2003.00645.x. [DOI] [PubMed] [Google Scholar]
- Kang WY, Shen JT, Chai CY. Paraganglioma of the urinary bladder: a case report. Kaohsiung J Med Sci. 2003;19:136–140. doi: 10.1016/S1607-551X(09)70462-0. [DOI] [PubMed] [Google Scholar]
- Doran F, Varinli S, Bayazit Y, Bal N, Ozdemir S. Pheochromocytoma of the urinary bladder. Acta Pathol Microbiol Immunol Scand. 2002;110:733–736. doi: 10.1034/j.1600-0463.2002.1101007.x. [DOI] [PubMed] [Google Scholar]
- Tan SM, Chan ST. An undiagnosed phaeochromocytoma of the urinary bladder. Anaesth Intensive Care. 2002;30:668–670. doi: 10.1177/0310057X0203000521. [DOI] [PubMed] [Google Scholar]
- Lamarre-Cliche M, Hernigou A, Boutouyrie P, Plouin PF, Azizi M. Images in cardiovascular medicine. Pheochromocytoma of the urinary bladder. Circulation. 2002;106:2143–2144. doi: 10.1161/01.CIR.0000037120.95689.D8. [DOI] [PubMed] [Google Scholar]
- Ali-el-Dein B. el-Sobky E, el-Baz M, Shaaban AA. Abdominal and pelvic extra-adrenal paraganglioma: a review of literature and a report on 7 cases. In Vivo. 2002;16:249–254. [PubMed] [Google Scholar]
- Dewan M, Rasshid M, Elmalik EM, Ansari MA, Morad N. Lessons to be learned: a case study approach. Paraganglioma of the urinary bladder. J R Soc Promot Health. 2001;121:193–198. doi: 10.1177/146642400112100317. [DOI] [PubMed] [Google Scholar]
- Moritani H, Sakamoto M, Yoshida Y, Nasu H, Nemoto R, Nakamura I. Pheochromocytoma of the urinary bladder revealed with cerebral hemorrhage. Intern Med. 2001;40:638–642. doi: 10.2169/internalmedicine.40.638. [DOI] [PubMed] [Google Scholar]
- Kozlowski PM, Mihm F, Winfield HN. Laparoscopic management of bladder pheochromocytoma. Urology. 2001;57:365. doi: 10.1016/s0090-4295(00)00899-2. [DOI] [PubMed] [Google Scholar]
- Seki N, Mukai S, Gamachi A, Migita T, Maeda K, Ogata N. A case of bladder pheochromocytoma. Urol Int. 2001;66:57–60. doi: 10.1159/000056569. [DOI] [PubMed] [Google Scholar]
- Baima C, Casetta G, Vella R, Tizzani A. Bladder pheochromocytoma: a 3-year follow-up after transurethral resection (TURB) Urol Int. 2000;65:176–178. doi: 10.1159/000064868. [DOI] [PubMed] [Google Scholar]
- Gyftopoulos K, Perimenis P, Ravazoula P, Athanassopoulos A, Barbalias GA. Pheochromocytoma of the urinary bladder presenting only with macroscopic hematuria. Urol Int. 2000;65:173–175. doi: 10.1159/000064867. [DOI] [PubMed] [Google Scholar]
- Rajaratnam S, Seshadri MS, Gopalakrishnan G, Chandi SM. Phaeochromocytoma of the urinary bladder. J Assoc Physicians India. 1999;47(2):246–247. [PubMed] [Google Scholar]
- Singh DV, Seth A, Gupta NP, Kumar M. Calcified nonfunctional paraganglioma of the urinary bladder mistaken as bladder calculus: a diagnostic pitfall. BJU Int. 2000;85:1152–1153. doi: 10.1046/j.1464-410x.2000.00687.x. [DOI] [PubMed] [Google Scholar]
- Panichi S, Dell'Anna G, Innocenti P, Nesi G. Paraganglioma of the bladder: report of a case. Annali Italiani Di Chirurgia. 1999;70:937–939. [PubMed] [Google Scholar]
- Sanjoaquín MT, Fraile JR, Gutiérrez A, Canal MI, Navia J. Hypertensive crisis during a transurethral resection of the bladder: nondiagnosed bladder paraganglioma. Anesth Analg. 2000;90(3):556–558. doi: 10.1097/00000539-200003000-00011. [DOI] [PubMed] [Google Scholar]
- Kato H, Suzuki M, Mukai M, Aizawa S. Clinicopathological study of pheochromocytoma of the urinary bladder: immunohistochemical, flow cytometric and ultrastructural findings with review of the literature. Pathol Int. 1999;49:1093–1099. doi: 10.1046/j.1440-1827.1999.00985.x. [DOI] [PubMed] [Google Scholar]
- Shono T, Sakai H, Minami Y, Suzu H, Kanetake H, Saito Y. Paraganglioma of the urinary bladder: a case report and review of the Japanese literature. Urol Int. 1999;62:102–105. doi: 10.1159/000030367. [DOI] [PubMed] [Google Scholar]
- Fujishima S, Abe I, Kaseda S. Ambulatory blood pressure monitoring in diagnosing a pheochromocytoma of the urinary bladder. A case report. Angiology. 1997;48:655–658. doi: 10.1177/000331979704800714. [DOI] [PubMed] [Google Scholar]
- Piedrola G, Lopez E, Rueda MD, Lopez R, Serrano J, Sancho M. Malignant pheochromocytoma of the bladder: current controversies. Eur Urol. 1997;31:122–125. doi: 10.1159/000474432. [DOI] [PubMed] [Google Scholar]
- Asbury WL Jr, Hatcher PA, Gould HR, Reeves WA, Wilson DD. Bladder pheochromocytoma with ring calcification. Abdom Imaging. 1996;21:275–277. doi: 10.1007/s002619900064. [DOI] [PubMed] [Google Scholar]
- Lee SP, Wang GG, Hwang SC, Chen MT, Lin HD. Pheochromocytoma of the urinary bladder: a case report. Chin Med J. 1996;57:297–300. [PubMed] [Google Scholar]
- Nesi G, Vezzosi V, Amorosi A, Menghetti I, Selli C. Paraganglioma of the urinary bladder. Urol Int. 1996;56:250–253. doi: 10.1159/000282853. [DOI] [PubMed] [Google Scholar]
- Kyriakidis A, Dimitriou D, Stiakakis I. A clinical diagnosis of urinary bladder (extra-adrenal) phaeochromocytoma. Acta Urol Belg. 1995;63:65–66. [PubMed] [Google Scholar]
- Takimoto E, Ueda W. Unsuspected pheochromocytoma of the urinary bladder. Anesth Analg. 1995;80:1243–1244. doi: 10.1097/00000539-199506000-00031. [DOI] [PubMed] [Google Scholar]
- Nargund VH, Gouldesbrough DR, Stewart PA. A self-made diagnosis of phaeochromocytoma of the urinary bladder. Br J Urol. 1994;73:220–222. doi: 10.1111/j.1464-410X.1994.tb07506.x. [DOI] [PubMed] [Google Scholar]
- Thrasher JB, Rajan RR, Perez LM, Humphrey PA, Anderson EE. Pheochromocytoma of urinary bladder: contemporary methods of diagnosis and treatment options. Urology. 1993;41:435–439. doi: 10.1016/0090-4295(93)90503-3. [DOI] [PubMed] [Google Scholar]
- Suzuki Y, Nakada T, Suzuki H. Primary bladder pheochromocytoma without hypertension. Int Urol Nephrol. 1993;25:153–158. [PubMed] [Google Scholar]
- Misawa T, Shibasaki T, Toshima R. A case of pheochromocytoma of the urinary bladder in a long-term hemodialysis patient. Nephron. 1993;64:443–446. doi: 10.1159/000187368. [DOI] [PubMed] [Google Scholar]
- Jurincic C, Gasser A, Metz KA, Kjelstrup T, Klippel KF. Pheochromocytoma of the urinary bladder. Urol Int. 1992;48:232–234. doi: 10.1159/000282341. [DOI] [PubMed] [Google Scholar]
- Hansen LU, Jess P, Hermansen K, Lorentzen M. Phaeochromocytoma–an unusual cause of haematuria. Scand J Urol Nephrol. 1992;26:319–321. doi: 10.3109/00365599209180893. [DOI] [PubMed] [Google Scholar]
- Grignon DJ, Ro JY, Mackay B. Paraganglioma of the urinary bladder: immunohistochemical, ultrastructural, and DNA flow cytometric studies. Hum Pathol. 1991;22:1162–1169. doi: 10.1016/0046-8177(91)90271-P. [DOI] [PubMed] [Google Scholar]
- Frydenberg M, Ferguson R, Langdon P, Rogers J, McCarthy S. Malignant phaeochromocytoma of the bladder–active or inactive. Br J Urol. 1991;67:548–549. doi: 10.1111/j.1464-410X.1991.tb15205.x. [DOI] [PubMed] [Google Scholar]
- Sweetser PM, Ohl DA, Thompson NW. Pheochromocytoma of the urinary bladder. Surgery. 1991;109:677–681. [PubMed] [Google Scholar]
- Warshawsky R, Bow SN, Waldbaum RS, Cintron J. Bladder pheochromocytoma with MR correlation. J Comput Assist Tomogr. 1989;13:714–716. doi: 10.1097/00004728-198907000-00036. [DOI] [PubMed] [Google Scholar]
- Punekar S, Gulanikar A, Sobti MK, Sane SY, Pardanani DS. Pheochromocytoma of the urinary bladder-report of 2 cases with review of literature. J Postgrad Med. 1989;35:90–92. [PubMed] [Google Scholar]
- Splinter WM, Milne B, Nickel C, Loomis C. Perioperative management for resection of a malignant non-chromaffin paraganglioma of the bladder. Can J Anaesth. 1989;36:215–218. doi: 10.1007/BF03011448. [DOI] [PubMed] [Google Scholar]
- Salo JO, Miettinen M, Makinen J, Lehtonen T. Pheochromocytoma of the urinary bladder. Report of 2 cases with ultrastructural and immunohistochemical analyses. Eur Urol. 1989;16:237–239. doi: 10.1159/000471579. [DOI] [PubMed] [Google Scholar]
- Liu SM, Wu JS. Pheochromocytoma of the urinary bladder–a case report. Chin Med J. 1988;42:491–494. [PubMed] [Google Scholar]
- Lenders JW, Sluiter HE, Rosenbusch G, Thien T. A pheochromocytoma of the urinary bladder. Eur J Radiol. 1987;7:274–275. [PubMed] [Google Scholar]
- Cariem AK, Green JA, Fraser AG, Smith LR. Phaeochromocytoma of the bladder. A case report. South African Med J. 1987;71:178–179. [PubMed] [Google Scholar]
- Sakashita S, Tanda K, Togashi M. Paraganglioma of urinary bladder, visualization with 131I-MIBG scintigraphy. Urol Int. 1987;42:237–240. doi: 10.1159/000281913. [DOI] [PubMed] [Google Scholar]
- Burton EM, Schellhammer PF, Weaver DL, Woolfitt RA. Paraganglioma of urinary bladder in a patient with neurofibromatosis. Urology. 1986;27:550–552. doi: 10.1016/0090-4295(86)90341-9. [DOI] [PubMed] [Google Scholar]
- Davaris P, Petraki K, Arvanitis D, Papacharalammpous N, Morakis A, Zorzos S. Urinary bladder paraganglioma (U.B.P.) Pathol Res Pract. 1986;181:101–106. doi: 10.1016/S0344-0338(86)80196-0. [DOI] [PubMed] [Google Scholar]
- Malossini G, Lotto A, Pisa R, Petracco S, Bianchi G. Pheochromocytoma of the urinary bladder. Acta Urol Belg. 1986;54:84–91. [PubMed] [Google Scholar]
- McCormick SR, Dodds PR, Kraus PA, Lowell DM. Nonepithelial neoplasms arising within vesical diverticula. Urology. 1985;25:405–408. doi: 10.1016/0090-4295(85)90502-3. [DOI] [PubMed] [Google Scholar]
- Jurascheck F, Egloff H, Buemi A, Laedlein-Greilsammer D. Paraganglioma of urinary bladder. Urology. 1983;22:659–663. doi: 10.1016/0090-4295(83)90322-9. [DOI] [PubMed] [Google Scholar]
- Miller JL, Immelman EJ, Roman TE, Mervis B. Phaeochromocytoma of the urinary bladder localized by selective venous sampling and computed tomography. Postgrad Med J. 1983;59:533–535. doi: 10.1136/pgmj.59.694.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S, Bulusu NV, Lowe P. Primary vesical pheochromocytoma. Urology. 1983;21:20–25. doi: 10.1016/0090-4295(83)90116-4. [DOI] [PubMed] [Google Scholar]
- Khan O, Williams G, Chisholm GD, Welbourn RB. Phaeochromocytomas of the bladder. J R Soc Med. 1982;75:17–20. doi: 10.1177/014107688207500105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochi K, Yoshioka S, Morita M, Takeuchi M. Pheochromocytoma of bladder. Urology. 1981;17:228–230. doi: 10.1016/0090-4295(81)90034-0. [DOI] [PubMed] [Google Scholar]
- Khan O, Williams G. Micturition with headache: phaeochromocytoma of the bladder. Eur Urol. 1981;7:112–114. doi: 10.1159/000473193. [DOI] [PubMed] [Google Scholar]
- Hamberger B, Arner S, Backman KA. Pheochromocytoma of the bladder. A case report. Scand J Urol Nephrol. 1981;15:333–335. doi: 10.3109/00365598109179629. [DOI] [PubMed] [Google Scholar]
- Flanigan RC, Wittmann RP, Huhn RG, Davis CJ. Malignant pheochromocytoma of urinary bladder. Urology. 1980;16:386–388. doi: 10.1016/0090-4295(80)90144-2. [DOI] [PubMed] [Google Scholar]
- Das S, Lowe P. Malignant pheochromocytoma of the bladder. J Urol. 1980;123:282–284. doi: 10.1016/s0022-5347(17)55898-x. [DOI] [PubMed] [Google Scholar]
- Hanji AM, Rohan VS, Patel JJ, Tankshali RA. Pheochromocytoma of the urinary bladder: a rare cause of severe hypertension. Saudi J Kidney Dis Transpl. 2012;23(4):813–816. doi: 10.4103/1319-2442.98167. [DOI] [PubMed] [Google Scholar]
- Deng JH, Li HZ, Zhang YS, Liu GH. Functional paragangliomas of the urinary bladder: a report of 9 cases. Chin J Cancer. 2010;29(8):729–734. doi: 10.5732/cjc.009.10703. PubMed PMID: 20663319. [DOI] [PubMed] [Google Scholar]
- Zeitlin I, Dessau H, Lorberboym M, Beigel Y. Malignant pheochromocytoma of the urinary bladder: challenges in diagnosis and management. Israel Med Assoc J. 2011;13:311–313. [PubMed] [Google Scholar]
- National Cancer Institute at the National Institute of Health. http://www.cancer.gov/cancertopics/pdq/treatment/pheochromocytoma/HealthProfessional/page2. Accessed 2/27/2012.
- Averbuch SD, Steakley CS, Young RC. Malignant pheochromocytoma: effective treatment with a combination of cyclophosphamide, vincristine, and dacarbazine. Ann Intern Med. 1988;109(4):267–273. doi: 10.7326/0003-4819-109-4-267. [DOI] [PubMed] [Google Scholar]
- Gonias S, Goldsby R, Matthay KK. Phase II study of high-dose [131I] metaiodobenzylguanidine therapy for patients with metastatic pheochromocytoma and paraganglioma. J Clin Oncol: official journal of the American Society of Clinical Oncology. 2009;27(25):4162–4168. doi: 10.1200/JCO.2008.21.3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahm P, Gschwend JE. Malignant non-urothelial neoplasms of the urinary bladder: a review. Eur Urol. 2003;44:672–681. doi: 10.1016/S0302-2838(03)00416-0. [DOI] [PubMed] [Google Scholar]