Abstract
Language impairment (LI) and reading disability (RD) are common pediatric neurobehavioral disorders that frequently co-occur, suggesting they share etiological determinants. Recently, our group identified prenatal nicotine exposure as a factor for RD and poor reading performance. Using smoking questionnaire and language data from the Avon Longitudinal Study of Parents and Children, we first determined if this risk could be expanded to other communication disorders by evaluating whether prenatal nicotine exposure increases risk for LI and poor performance on language tasks. Prenatal nicotine exposure increased LI risk (OR = 1.60; p = 0.0305) in a dose-response fashion with low (OR = 1.25; p = 0.1202) and high (OR = 3.84; p = 0.0002) exposures. Next, hypothesizing that the effects of prenatal nicotine may also implicate genes that function in nicotine related pathways, we determined whether known nicotine dependence (ND) genes associate with performance on language tasks. We assessed the association of 33 variants previously implicated in ND with LI and language abilities, finding association between ANKK1/DRD2 and performance on language tasks (p≤0.0003). The associations of markers within ANKK1 were replicated in a separate LI case-control cohort (p<0.05). Our results show that smoking during pregnancy increases the risk for LI and poor performance on language tasks and that ANKK1/DRD2 contributes to language performance. More precisely, these findings suggest that prenatal environmental factors influence in utero development of neural circuits vital to language. Our association of ANKK1/DRD2 further implicates the role of nicotine-related pathways and dopamine signaling in language processing, particularly in comprehension and phonological memory.
Introduction
Language impairment (LI) and reading disability (RD) have prevalences of 5–8% and 5–17%, respectively, in schoolchildren [1]–[2], and together comprise the majority of learning disabilities. LI and RD are characterized by difficulty in the understanding and/or utilization of verbal and written language, respectively, despite normal development and adequate educational opportunity [1]–[2]. LI and RD are related disorders, as both involve deficits in the integration and utilization of communicative tools. Impaired phonological skills have been implicated in both LI and RD [1]–[7]. LI and RD are frequently comorbid; as children with LI are at higher risk of developing RD than their typically developing peers [1]–[2], [8]. The degree of relatedness and the frequent comorbidity of LI and RD indicate they may share risk factors. Twin and family studies have shown that both LI and RD have a significant genetic component, with heritability estimates of 45–73% and 54–84%, respectively [8]–[10]. However, specific environmental and genetic risk factors for LI and RD, and the extent to which they are shared between the two disorders, remain largely unknown.
One possible environmental risk factor for LI and RD is exposure of the developing fetus to toxins and substances in utero via the maternal environment and behavior, specifically smoking or nicotine exposure. The harm of prenatal nicotine exposure has been well-documented [11]–[13]. Despite this, studies estimate 14–37% of women smoke during pregnancy [14]. Prenatal nicotine exposure is a risk factor for several neurobehavioral conditions such as Attention Deficit-Hyperactivity Disorder (ADHD), learning disabilities, and substance abuse [15]–[17]. Some studies have expanded these findings to RD, LI, and neurocognition [18]–[19], [21]; while others have argued that nicotine variables may capture factors not adequately controlled for in statistical models, such as socioeconomic status [20]–[21]. Our recent work showed an association between prenatal nicotine exposure and poor reading performance in schoolchildren, after adjustment for a wide range of confounders, including socioeconomic status, type of school attended, birth weight, and gestational age [22]. However, further study is necessary to determine whether prenatal nicotine exposure also influences language abilities and LI.
The implication of prenatal nicotine exposure in communication performance raises the question of how this exposure exerts its effects. One possibility is that genetic variants previously associated with nicotine dependence (ND) and nicotine-related pathways may have pleiotropic effects. That is, genetic variants that predispose individuals to ND may also contribute to communication processes. Studies of ND have revealed that it has a significant genetic component and identified several candidate genes, including DRD2, ANKK1, CHRNA4, and CHRNB2. Many of these genes are involved in neuronal signaling pathways, including the cholinergic and dopaminergic neurotransmitter pathways. The implication of various signaling pathways further suggests that variation in these genes may affect multiple cerebral processes, such as addiction, language, and reading. Several of these ND genes, including BDNF, DRD2, and ANKK1, have been associated with neurobehavioral phenotypes [23]–[24]. ANKK1 and DRD2 have been associated with autism, executive functioning, and verbal ability [25]–[26]. However, these reports are few in number, and replication in larger cohorts is needed.
The present study expands on our previous work to examine prenatal nicotine exposure and its related pathways with regard to LI and its associated language domains. First, we analyze the relationship of prenatal nicotine exposure with performance on language tasks and LI. Due to nicotine’s detrimental effects on brain function, we hypothesize that prenatal smoking exposure will also be a risk factor for poor language performance and LI. Second, we assess whether known ND variants contribute to language abilities. ND genes have known neurological functions, particularly in neuronal signaling; therefore, we also hypothesize ND variants associate with language performance and LI.
Materials and Methods
Subjects
The Avon Longitudinal Study of Parents and Children (ALSPAC) is a population-based, birth cohort in Avon, United Kingdom. Subjects were recruited before birth, resulting in a total of 15,458 fetuses, of whom 14,701 were alive at 1 year of age. Recruitment, participants, and study methodologies are described in detail elsewhere (http://www.bristol.ac.uk/alspac) [27]–[28]. 7170 subjects completed language measures at age 8 years. Subjects with IQ ≤75 on the Wechsler Intelligence Scale for Children (WISC-III) Total IQ were excluded from the present study [29]. To prevent population stratification in genetic analyses, subjects of non-European descent were also removed. Additionally, samples with genotyping call rate <0.80 were excluding from analyses, leaving a final sample size of 5579 individuals. Ethical approval was obtained from ALSPAC Ethics and Law Committee, Local UK Research Ethics Committees, and Yale Human Investigation Committee.
ALSPAC Language Measures
Language measures were collected during clinical interviews at age 8 years. An adaptation of the Nonword Repetition Task (NWR), in which subjects repeated recordings of nonwords, was used to assess short-term phonological memory and processing abilities [30]. Children also completed the Wechsler Objective Language Dimensions (WOLD) verbal comprehension task at age 8 years [31], where they answered questions about a paragraph read aloud by an examiner describing a presented picture. We focused on these measures because individuals with LI are known to consistently perform poorly on NWR and WOLD comprehension tasks, and these tasks are commonly used in genetic and epidemiologic studies of LI [32]–[33]. Z-scores were calculated for each subject on each individual measure, and to capture deficits in two of the primary domains of LI, the average z-score of NWR and WOLD comprehension tasks was calculated. To assess the risk imparted to severe LI, we defined LI cases as scoring ≥2.0 standard deviations below sample means on either task.
Exposure and Covariate Variables
Questionnaires for smoking frequency and cigarette brand were completed by mothers at gestational age 8, 18, and 32 weeks and at 8 weeks following birth. Although cigarettes contain thousands of compounds, nicotine is the most prevalent, pharmacologically active ingredient that is likely responsible for smoking’s deleterious effects. Therefore, we calculated the level of nicotine exposure for each time point based upon the nicotine content of the cigarette brands smoked. Because of limited power to divide nicotine exposure into trimesters, we used the maximum nicotine exposure to derive prenatal nicotine exposure [22], [34]–[35]. First, prenatal nicotine exposure was dichotomized into exposed and non-exposed groups. To examine dose-response, prenatal nicotine exposure was further categorized into three groups: no exposure (0 mg*day−1), low exposure (≤17 mg*day−1), and high exposure (>17 mg*day−1) [36]. 17 mg was chosen as it is the average amount of nicotine in one pack of cigarettes.
Due to the interdependence between overall cognition and communication, subjects with WISC-III Total IQ scores ≤75 were excluded from analysis [37]. To further control for the effects of IQ, WISC-III Performance IQ scores were included as a covariate in analyses [29]. Performance IQ was chosen to prevent controlling for language abilities captured by Verbal and Total IQ scores. In addition to Performance IQ, we adjusted for the following 11 covariates to control for known confounding relationships with language: mother’s age at delivery, maternal prenatal alcohol consumption [38], maternal social class, child-parent interaction time, mother’s attendance at antenatal classes, sex, ADHD status, school type, gestational age, birthweight, and resuscitation status [39] (Table S1).
Statistical and Genetic Analyses
First, SAS 9.2 was used to statistically analyze the association of prenatal nicotine exposure with language performance in the ALSPAC cohort. Dichotomized prenatal nicotine exposure status was examined first, followed by dosage categories. For quantitative measures, we fitted crude linear regression models, with prenatal nicotine exposure as the predictor for each language outcome. Next, multivariable regression models adjusted for covariates were used to identify specific effects of prenatal nicotine exposure. We used logistic regression models to fit prenatal nicotine exposure and covariates for each dichotomized language measure. Odds ratios (OR) were calculated for exposed/non-exposed, then for the low and high dosage categories.
Next, 33 single nucleotide polymorphisms (SNPs) in 12 genes, previously implicated in ND, nicotine pathways, and/or substance dependencies, were genotyped on the Sequenom platform (San Diego, CA), following the manufacturers guidelines at the Yale Center for Genome Analysis (Orange, CT) (Table 1). 32 of the 33 ND variants had call rates ≥90%, were biallelic, had minor allele frequencies ≥0.01, and were in Hardy-Weinberg equilibrium (p≥0.001). To correct for the 32 genetic association tests performed in the ALSPAC cohort, Bonferroni correction was applied to adjust for multiple testing (α = 0.05/32 = 1.56×10−3). Since these ND variants have a prior relationship with nicotine and/or addiction, we created a subsample of subjects not exposed to nicotine and repeated associations to avoid possible confounding.
Table 1. Nicotine dependence (ND) markers genotyped in the ALSPAC sample.
| Variant | Gene | Location | MAF | Variant | Gene | Location | MAF |
| rs2072660 | CHRNB2 | 1q21.3 | 0.240 | rs10893365 | PKNOX2 | 11q24.2 | 0.171 |
| rs2072661 | CHRNB2 | 1q21.3 | 0.244 | rs10893366 | PKNOX2 | 11q24.2 | 0.168 |
| rs12466358 | CHRND | 2q31 | 0.253 | rs11220015 | PKNOX2 | 11q24.2 | 0.174 |
| rs13277254 | CHRNB3 | 8p21 | 0.212 | rs11602925 | PKNOX2 | 11q24.2 | 0.176 |
| rs4950 | CHRNB3 | 8p21 | 0.214 | rs12284594 | PKNOX2 | 11q24.2 | 0.170 |
| rs6474413 | CHRNB3 | 8p21 | 0.214 | rs1426153 | PKNOX2 | 11q24.2 | 0.174 |
| rs4075274 | NTRK2 | 9q21.33 | 0.434 | rs750338 | PKNOX2 | 11q24.2 | 0.227 |
| rs2030324 | BDNF | 11p14.1 | 0.469 | rs1051730 | CHRNA3 | 15q25 | 0.329 |
| rs4274224 | DRD2 | 11q23.1 | 0.493 | rs1317266 | CHRNA3 | 15q25 | 0.226 |
| rs4648318 | DRD2 | 11q23.1 | 0.239 | rs578776 | CHRNA3 | 15q25 | 0.281 |
| rs7131056 | DRD2 | 11q23.1 | 0.425 | rs6495308 | CHRNA3 | 15q25 | 0.231 |
| rs6278 | DRD2 | 11q23.1 | 0.153 | rs8034191 | LOC123688 | 15q25 | 0.331 |
| rs11604671 | ANKK1 | 11q23.1 | 0.488 | rs16969968 | CHRNA5 | 15q25 | REMOVED |
| rs1800497 | ANKK1 | 11q23.1 | 0.197 | rs2229959 | CHRNA4 | 20q13.33 | 0.113 |
| rs2734849 | ANKK1 | 11q23.1 | 0.485 | rs2236196 | CHRNA4 | 20q13.33 | 0.252 |
| rs4938013 | ANKK1 | 11q23.1 | 0.321 | rs2273504 | CHRNA4 | 20q13.33 | 0.162 |
| rs7118900 | ANKK1 | 11q23.1 | 0.185 |
Abbreviations: ND, nicotine dependence; MAF, minor allele frequency.
Associated variants were then examined in the Iowa LI cohort. The Iowa LI cohort is comprised of 219 LI cases and 209 sex- and age-matched, unrelated controls collected at the University of Iowa. Subjects completed various language measures, including the Peabody Picture Vocabulary Test (PPVT) and NWR, which were used to derive a composite language score, which was dichotomized into case-control status at −1.14 standard deviations [40]. Single marker analysis in both cohorts was performed with linear and logistic regression under additive models using SNP & Variation Suite (SVS) v7.6.4 (Golden Helix, Bozeman, MT). Haplotype regions were constructed following the 4-gamete rule using HaploView v4.2, and haplotype association tests were performed using PLINK v1.07.
Results
Prenatal Nicotine Exposure and Language
In the ALSPAC sample, subjects exposed to prenatal nicotine performed on average 4.75–5.39% worse on language measures compared to non-exposed subjects (Table 2). When separated into nicotine dosage categories, those exposed to high levels of prenatal nicotine performed on average the worst on all measures compared to low (ranging from 6.20–7.95% worse) and no exposure (ranging from 9.63–11.58%) groups (Table 2).
Table 2. Descriptive statistics of language scores among exposure groups.
| Non-smoking | Any Exposure | Low | High | |||||
| N | Mean(SD) | N | Mean(SD) | N | Mean(SD) | N | Mean(SD) | |
| NWR | 4720 | 7.37(2.43) | 758 | 7.02(2.48) | 615 | 7.10(2.45) | 143 | 6.66(2.56) |
| Comprehension | 4724 | 7.60(1.91) | 760 | 7.19(1.93) | 617 | 7.30(1.93) | 143 | 6.72(1.88) |
Abbreviations: SD, standard deviation; NWR, nonword repetition.
Crude linear regression analyses comparing groups exposed to prenatal nicotine to the non-exposed groups showed that prenatal nicotine exposure is associated with performance on NWR and comprehension tasks (p≤0.0002) (Table 3). After adjusting for covariates, the association with average performance on the NWR/comprehension tasks persisted (p = 0.0262), while there was a trend with the NWR task (p = 0.0799). Crude analyses for exposure dosage showed a deleterious effect of prenatal nicotine exposure on NWR and comprehension tasks (p≤0.0002) (Table 4). After covariate adjustment, there was a negative effect of high dose of prenatal nicotine exposure on comprehension (p = 0.0011) and average performance on NWR/comprehension (p = 0.0011), with trend toward a negative effect of high exposure for the NWR task alone (p = 0.0729).
Table 3. Effects of any prenatal nicotine exposure on language performance.
| Crude Model | Adjusted Model | |||||
| Exposed | Overall | Exposed | Overall | |||
| Measure | Beta | p-value | p-value | Beta | p-value | p-value |
| NWR | −0.14 | 0.0002 | 0.0002 | −0.09 | 0.0799 | 0.0799 |
| Comprehension | −0.21 | <0.0001 | <0.0001 | −0.08 | 0.1123 | 0.1123 |
| Avg NWR Comp | −0.18 | <0.0001 | <0.0001 | −0.09 | 0.0262 | 0.0262 |
Abbreviations: NWR, nonword repetition; Avg NWR Comp. average of z-scores of nonword repetition and verbal comprehension tasks.
Table 4. Effects of prenatal nicotine dosage on language performance.
| Crude Model | Adjusted Model | |||||||||
| Low | High | Overall | Low | High | Overall | |||||
| Measure | Beta | p-value | Beta | p-value | p-value | Beta | p-value | Beta | p-value | p-value |
| NWR | −0.11 | 0.0102 | −0.29 | 0.0006 | 0.0002 | −0.07 | 0.2174 | −0.22 | 0.0729 | 0.1085 |
| Comprehension | −0.16 | <.0002 | −0.46 | <0.0001 | <0.0001 | −0.02 | 0.7426 | −0.47 | 0.0002 | 0.0011 |
| Avg NWR Comp | −0.13 | <0.0001 | −0.37 | <0.0001 | <0.0001 | −0.05 | 0.2868 | −0.35 | 0.0003 | 0.0011 |
Abbreviations: NWR, nonword repetition; Avg NWR Comp. average of z-scores of nonword repetition and verbal comprehension tasks.
In ALSPAC, LI had a prevalence of 4.90%, which is consistent with estimates in the general population [1]–[2]. Exposure to prenatal nicotine increased risk for LI, after controlling for covariates (OR = 1.60 [1.04–2.45]; p = 0.0305) (Table 5). Risk of developing LI occurred in a dose response fashion with low (OR = 1.25 [0.76–2.04]; p = 0.1202) and high (OR = 3.85 [1.87–7.94]; p = 0.0009) prenatal nicotine exposure levels (Table 6).
Table 5. LI risk based on prenatal nicotine exposure.
| Crude Model | Adjusted Model | ||
| OR | p-value | OR | p-value |
| 1.77 (1.31–2.40) | 0.0002 | 1.60 (1.04–2.45) | 0.0305 |
Abbreviation: OR, odds ratio.
Table 6. LI risk based on prenatal nicotine dosage.
| Crude Model | Adjusted Model | ||||||
| Low OR | p-value | High OR | p-value | Low OR | p-value | High OR | p-value |
| 1.43 (1.00–2.05) | 0.2514 | 3.33 (2.02–5.52) | <0.0001 | 1.25 (0.76–2.04) | 0.1202 | 3.85 (1.87–7.94) | 0.0009 |
Abbreviation: OR, odds ratio.
Association of ND Markers to Language
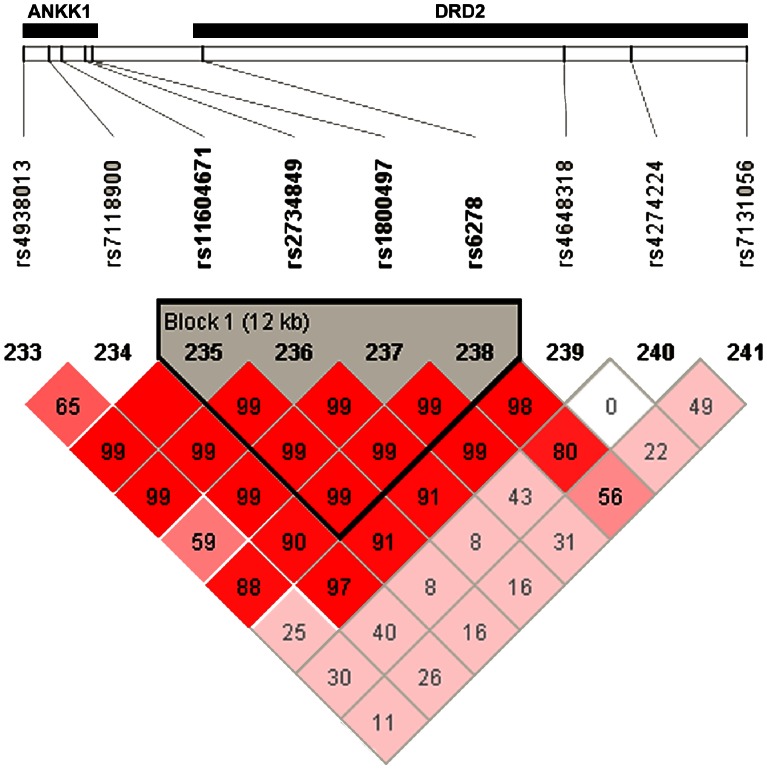
Single-marker analysis revealed associations between SNPs within ANKK1 and language performance as measured by the average z-score on NWR/comprehension tasks (p≤1.9×10−3) (Table 7). Haplotype associations were similar, showing association between a haplotype containing ANKK1 and DRD2 markers and language performance (Table 8). This haplotype included a majority of the significant SNPs from single marker analysis, suggesting these markers captured the same variability in the locus. Interestingly, the ANKK1 haplotype block contained a marker in the DRD2 gene located adjacent to ANKK1 (rs6278) (Figure 1). These associations persisted when examined in ALSPAC subjects not exposed to prenatal nicotine (Table 7). There was no evidence of interaction between prenatal nicotine exposure and ND variants in the ALSPAC sample. Associations of SNPs within ANKK1 (rs2734849 and rs11604671) were replicated in the Iowa LI cohort with LI case-control status (OR = 1.4 [1.1–2.0]; p≤7.41×10−3) (Table 9).
Table 7. Single marker genetic associations with average of Nonword Repetition and Verbal Comprehension tasks.
| Variant | Gene | p-value | No SMK p-valuea |
| rs2734849 | ANKK1 | 2.0×10−4 | 1.9×10−4 |
| rs11604671 | ANKK1 | 2.3×10−4 | 2.2×10−4 |
| rs4938013 | ANKK1 | 1.2×10−3 | 6.8×10−4 |
| rs7118900 | ANKK1 | 1.2×10−3 | 1.2×10−3 |
| rs1800497 | ANKK1 | 1.9×10−3 | 2.6×10−3 |
| rs6278 | DRD2 | 8.8×10−3 | 1.7×10−2 |
No SMKg p-value refer to associations in cohort of subjects not exposed to prenatal nicotine.
Table 8. Haplotype Association of ANKK1/DRD2 with average of Nonword Repetition and Verbal Comprehension tasks.
| Variants | Genes | Haplotype | Beta | p-value |
| rs11604671, rs2734849, rs1800497, rs6278 | ANKK1/DRD2 | ACCG | 0.053 | 3.2×10−4 |
Figure 1. Linkage disequilibrium between ANKK1 and DRD2.
Linkage disequilibrium (LD), as measured by D’, among markers in the ANKK1 and DRD2 genes. There is a 12kb haplotype block spanning the two genes (markers: rs11604671, rs2734849, rs1800497, and rs6278).
Table 9. Replication of genetic associations in Iowa LI cohort.
| Variant | Gene | Trait | p-value | OR |
| rs11604671 | ANKK1 | Case-Control | 3.84×10−3 | 1.4 (1.1–2.0) |
| rs2734849 | ANKK1 | Case-Control | 7.41×10−3 | 1.4 (1.1–2.0) |
| rs1800497 | ANKK1 | Case-Control | 1.9×10−2 | 1.5 (1.1–2.1) |
| rs11604671 | ANKK1 | GORT Comp | 3.3×10−2 | N/A |
| rs11604671 | ANKK1 | PPVT | 2.5×10−2 | N/A |
Abbreviations: OR, odds ratio; GORT Comp, Gray Oral Reading Test Comprehension; PPVT, Peabody Picture Vocabulary Test.
Discussion
Our investigation examined the effects of prenatal nicotine exposure and nicotine-related genetic variants on LI and performance on language tasks. We found increased risk of LI and poor performance on language tasks in subjects exposed to prenatal nicotine. In addition, there was a genetic association between single markers within ANKK1 and a haplotype spanning ANKK1/DRD2 and language performance, further implicating nicotine-related and dopamine pathways in language. These findings show the importance of the prenatal environment and dopamine to language and cognitive development.
Prenatal Nicotine Exposure and Language
We found an association of prenatal nicotine exposure on language performance and LI, after adjusting for known covariates, such as socioeconomic status, type of school attended, and parent interaction. This relationship appears to be specific to language skills and independent of overall cognitive skills, as Performance IQ was accounted for in all final models. These results expand upon our previous findings, showing the detrimental effects of prenatal nicotine exposure on phonology, reading fluency, reading comprehension, and reading accuracy. These components are foundational to the development of reading and language skills in children. Our previous study found that deficits in reading comprehension similar to the ones we found in verbal comprehension, suggesting prenatal nicotine exposure exerts an effect on how children ascertain meaning in verbal and written language.
The negative effects of prenatal nicotine exposure on reading and language may reflect changes in gene expression resulting from epigenetic modifications due to the nicotine exposure [41]. Future studies should examine how nicotine exposure interacts with genes associated with communication, such as DCDC2, KIAA0319, and FOXP2, and their epigenetic regulation. One investigation demonstrated the contribution of 5′ regions marked by acetylated H3 histones in KIAA0319 to RD, suggesting the importance of epigenetic regulation to language [42]. Epigenetic studies in combination with neurotoxicological studies should be explored to determine whether and how nicotine exposure alters gene expression and cellular function.
In addition to possible changes directly to gene regulation, mouse and rat models have shown that prenatal nicotine exposure permanently affects neurochemical signaling pathways, including dopaminergic pathways, and alter their developmental trajectories over the lifespan [43]–[45]. Animals exposed to gestational nicotine have higher dopamine turnover in the frontal cortex [44], [46]. These results from animal models, in conjunction with our findings implicating prenatal nicotine and dopamine signaling in LI, suggest that deficits and permanent changes in dopamine activity resulting from exposure and genetic variants have a substantial influence upon language skills and development. These implications, however, still must be explored and confirmed in human studies, possibly through magnetic resonance spectroscopy (MRS). MRS would permit in vivo monitoring of dopamine signaling in the human brain. MRS could specifically interrogate the influence of prenatal nicotine exposure on dopaminergic signaling, gene expression, and language in the same subjects.
ANKK1/DRD2 and Language
Single marker and haplotype analyses showed association between language performance and ANKK1-DRD2. In addition to past associations with ND, ANKK1 and DRD2 have been associated with other neurobehavioral traits including alcohol dependence, reinforcement learning, working memory, and executive function [47]–[51]. Dopamine is a key neurotransmitter in the corticostriatal system that subserves procedural and reinforcement learning. Animal and human studies, using dopamine agonists and/or antagonists, show that alterations in dopamine receptor function change reinforcement learning [52]. Recently, reinforcement learning was shown to be associated with individual differences in language in a task influenced by dopamine signaling [53]–[54]. Additionally, past studies have associated ANKK1/DRD2 to working memory. Working memory is directly associated with language skills in children, and in fact, impairments in working memory have been proposed to play a direct role in the development of language deficits seen in children with LI [55]–[56]. Changes in dopaminergic function, whether from genetic predisposition (ANKK1/DRD2) or environmental exposure (prenatal nicotine), yield alterations in working memory and reinforcement learning. These changes, which arise via permanent alterations in dopamine function, appear to then influence language development as well as other neurobehavioral domains, including nicotine and substance use.
Despite the wide range of literature examining ANKK1/DRD2 and neurobehavioral traits, there have been limited reports examining the role of ANKK1 and DRD2 specifically in language and language-related domains. Beaver et al. reported an association between DRD2 and performance on an abbreviated form of the PPVT [26]. The PPVT is a standardized measure of expressive and receptive vocabulary, which may be analogous to deficits measured in our verbal and reading comprehension tasks, although the tasks in this study measure higher order cognitive processing. Our findings expand the role of ANKK1 and DRD2 from known effects on working memory, reinforcement learning, and predisposition to nicotine use to now include verbal language. Additionally, these findings point to a role for dopamine as a mechanism in processes involved in language development. In this regard, these findings and the implications of prenatal nicotine exposure on brain neurochemistry support the notion that procedural learning, rooted in the dopamine rich basal ganglia, plays an important role in language development [57]–[59].
The relationship between the neighboring genes ANKK1 and DRD2 has been a source of controversy. In our study, we found association between language and a haplotype block stretching across ANKK1 and DRD2, suggesting that we, like most studies, are unable to refine our associations to a single gene. However, previous work has shown that the rs1800497 polymorphism is associated with the number of D2 dopamine binding sites and glucose metabolism in the central nervous system [60]–[62]. Reduced dopamine signaling and glucose metabolism may adversely affect high order cognitive functioning including verbal language processing. Functionally, there is limited evidence on how ANKK1 and DRD2 may interact. Huang et al. suggested ANKK1 may influence DRD2 expression via NF-kB signaling [63]. However, evidence supporting this hypothesis is limited and in vivo analyses are needed to discern any functional relationship between ANKK1 and DRD2. Additionally, associations of ANKK1 and DRD2 may reflect linkage disequilibrium in the locus, and may be capturing the signal from a single, unidentified causative variant.
Limitations
This investigation is subject to several limitations. First, the use of maximum amount of prenatal nicotine exposure may be an overestimation due to possible reductions and cessations of smoking during the prenatal period. However, the smoking data obtained accurately reflects the exposure since the information was collected in the pre/perinatal period. Second, although we controlled for many factors associated with language, this study cannot control for all possible, unmeasured factors that may confound associations. However, our models encompass a broad range of covariates relative to other previous studies. Third, due to the design of the ALSPAC cohort and amount of time following subjects, missing data are to be expected. The subsample used to complete association analyses has various demographic and environmental differences compared to the overall sample, which is more representative of the general population in the Avon region of the United Kingdom (Table S2). These factors were controlled for in the analysis of prenatal nicotine exposure, but our findings must be replicated in a more diverse, representative sample before being expanded to the general population. Fourth, there are inherent differences between our discovery cohort, ALSPAC, and our replication cohort, Iowa LI. Subjects in ALSPAC were recruited during the prenatal period, and investigators aimed to collect a sample that reflected the general population in the Avon region of the United Kingdom. Iowa LI is a case-control cohort that recruited cases with LI and matched controls. Therefore, genetic associations of ANKK1/DRD2 in the two cohorts are not identical. However, the initial and replicated associations do suggest that ANKK1/DRD2 and dopamine signaling modulate language skills in children.
Conclusions
Prenatal nicotine exposure has a negative effect on language abilities in schoolchildren. These results support the growing body of evidence that the development of communication skills begins during fetal development. Future studies should determine the effects of exposure to first-hand nicotine exposure and other prenatal and postnatal toxins. The genetic associations of ANKK1 and DRD2 with language performance further suggest that nicotine-related pathways modulate verbal language processing. More specifically, we implicate dopamine signaling in the comprehension and processing of verbal language. Other factors in dopamine and other major neurotransmitter signaling pathways should be examined.
Supporting Information
Distribution of covariates among smoking groups. Values are either percentages or means (SD). *Indicates χ2 two-tailed p-value <0.05 from univariate analyses of each covariate and prenatal nicotine exposure outcome. **Indicates ANOVA p-value <0.05 from comparison of each covariate and prenatal nicotine exposure outcome.
(DOC)
Comparison of those included in analyses and the overall ALSPAC cohort. Data are presented as either percentages or mean (SD).
(DOC)
Acknowledgments
We thank all the families and participants who took part in these studies. We also wish to acknowledge the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. We thank Dr. David E. Odd for useful clarifications on the resuscitation data. We are also grateful to the Yale Center for Genome Analysis, specifically Irina Tikhonova and Anna Rogers, for genotyping services.
Funding Statement
The UK Medical Research Council, the Wellcome Trust and the University of Bristol provide core support for ALSPAC. This research was funded by R01NS43530 (J.R.G.), T32 MH014235 (K.C.), and T32 GM007223 (J.D.E.) from the National Institutes of Health (NIH) along with F31DC012270 from the National Institute on Deafness and Other Communication Disorders (J.D.E.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Newbury DF, Fisher SE, Monaco AP (2010) Recent advances in the genetics of language impairment. Genome Med 2(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pennington BF, Bishop DVM (2009) Relations among speech, language, and reading disorders. Annu Rev Psychol 60: 283–306. [DOI] [PubMed] [Google Scholar]
- 3. Wise JC, Sevcik RA, Morris RD, Lovett MW, Wolf M (1999) The relationship among reception and expressive vocabulary, listening comprehension, pre-reading skills, word identification skills, and reading comprehension by children with reading disabilities. J Speech Lang Hear Res 50(4): 1093–9. [DOI] [PubMed] [Google Scholar]
- 4. Catts HW, Adlof SM, Hogan TP, Weismer SE (2005) Are specific language impairment and dyslexia distinct disorders? J Speech Lang Hear Res 48(6): 1378–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gathercole S, Baddeley AD (1990) Phonological memory deficits in language disordered children: Is there a causal connection? Journal of Memory and Language 29: 336–360. [Google Scholar]
- 6.Gathercole SE, Baddeley AD (1993) Working memory and language. Mahwah, NJ: Lawrence Erlbaum.
- 7. Nithart C, Demont E, Majerus S, Leybaert J, Poncelet M, et al. (2009) Reading disabilities in SLI and dyslexia reselt from distinct phonological impairments. Dev Neuropsychol 34(3): 296–311. [DOI] [PubMed] [Google Scholar]
- 8. Pennington BF (2006) From single to multiple deficit models of developmental disorders. Cognition 101(2): 385–413. [DOI] [PubMed] [Google Scholar]
- 9. Viding E, Spinath FM, Price TS, Bishop DV, Dale PS, et al. (2004) Genetic and environmental influence on language impairment in 4-year-old same-sex and opposite-sex twins. J Child Psychol Psychiatry 45(2): 315–25. [DOI] [PubMed] [Google Scholar]
- 10. Bishop DV, Hayiou-Thomas ME (2008) Heritability of specific language impairment depends on diagnostic criteria. Genes Brain Behav 7(3): 365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ginzel KH, Maritz GS, Marks DF, Neubrger M, Pauly JR, et al. (2007) Critical review: nicotine for the fetus, the infant and the adolescent. J Health Psychol 12(2): 215–24. [DOI] [PubMed] [Google Scholar]
- 12. Weitzman M, Byrd RS, Aligne CA, Moss M (2002) The effects of tobacco exposure on children’s behavioral and cognitive functioning: implications for clinical and public health policy and future research. Neurotoxicol Teratol 2(3): 397–406. [DOI] [PubMed] [Google Scholar]
- 13. Ernst M, Moolchan ET, Robinson ML (2001) Behavioral and neural consequences of prenatal exposure to nicotine. J Am Acad Child Adolesc Psychiatry 40(6): 630–41. [DOI] [PubMed] [Google Scholar]
- 14. Ward C, Lewis S, Coleman T (2007) Prevalence of maternal smoking and environmental tobacco smoke exposure during pregnancy and impact on birth weight: retrospective study using Millennium Cohort. BMC Public Health 7: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dwyer JB, Broide RS, Leslie FM (2008) Nicotine and brain development. Birth Defects Res C Embryo Today 84(1): 30–44. [DOI] [PubMed] [Google Scholar]
- 16. Pauly JR, Slotkin TA (2008) Maternal tobacco smoking, nicotine replacement, and neurobehavioural development. Acta Paediatr 97(10): 1331–7. [DOI] [PubMed] [Google Scholar]
- 17. Rogers JM (2009) Tobacco and pregnancy. Reprod Toxicol 28(2): 152–60. [DOI] [PubMed] [Google Scholar]
- 18. Fried PA, O’Connell CM, Watkinson B (1992) 60- and 72- Month Follow-up of Children Prenatally Exposed to Marijuana, Cigarettes, and Alcohol: Cognitive and Language Assessments. Developmental and Behavioral Pediatrics 13(6): 383–91. [PubMed] [Google Scholar]
- 19. Fried PA, Watkinson B, Siegel LS (1997) Reading and Language in 9- to 12- Year Olds Prenatally Exposed to Cigarettes and Marijuana. Neurotoxicol Teratol 19(3): 171–83. [DOI] [PubMed] [Google Scholar]
- 20. Tomblin JB, Hammer CS, Zhang X (1998) The association of parental tobacco use and SLI. Int J Lang Commun Disord 33(4): 357–68. [DOI] [PubMed] [Google Scholar]
- 21. Kafouri S, Leonard G, Perron M, Richer L, Seguin JR, et al. (2009) Maternal cigarette smoking during pregnancy and cognitive performance in adolescence. Int J Epidemiol 38: 158–172. [DOI] [PubMed] [Google Scholar]
- 22. Cho K, Frijters JC, Zhang H, Miller LL, Gruen JR (2013) Prenatal exposure to nicotine and impaired reading performance. J Pediatr 162(4): 713–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bekinschtein P, Cammarota M, Katche C, Slipczuk L, Rossato JI, et al. (2008) BDNF is essential to promote persistence of long-term memory storage. Proc Natl Acad Sci USA 105(7): 2711–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bertolino A, Blasi G (2009) The genetics of schizophrenia. Neuroscience 164(1): 288–99. [DOI] [PubMed] [Google Scholar]
- 25. Hettinger JA, Liu X, Hudson ML, Lee A, Cohen IL, et al. (2012) DRD2 and PPP1R1B (DARPP-32) polymorphisms independently confer risk for autism spectrum disorders and additively predict affected status in male-only affected sib-pair families. Behav Brain Funct 8(1): 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Beaver KM, Delisi M, Vaughn MG, Wright JP (2010) Association between the A1 allele of the DRD2 gene and reduced verbal abilities in adolescence and early adulthood J Neural Transm. 117(7): 827–30. [DOI] [PubMed] [Google Scholar]
- 27. Golding J, Pembrey M, Jones R (2001) ALSPAC Study Team (2001) ALSPAC–the Avon Longitudinal Study of Parents and Children. I. Study methodology. Paediatr Perinat Epidemiol 15(1): 74–87. [DOI] [PubMed] [Google Scholar]
- 28. Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, et al. (2012) Cohort Profile: The ‘Children of the 90s’–the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol 42(1): 111–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wechsler D, Golombok S, Rust J (1992) WISC-IIIUK: Wechsler Intelligence Scale for Children. Sidcup, UK: Psychological Corporation.
- 30.Gathercole SE, Baddeley AD (1996) The children’s test of nonword repetition. London: The Psychological Corportationl.
- 31.Wechsler D (1996) Wechsler objective language dimensions (WOLD). London: The Psychological Corporation.
- 32. Bishop DVM, North T, Donlan C (1996) Nonword repetition as a behavioural marker for inherited language impairment: evidence from a twin study. J Child Physiol Psychiatry 37: 391–403. [DOI] [PubMed] [Google Scholar]
- 33. Newbury DF, Winchester L, Addis L, Paracchini S, Buckingham LL, et al. (2009) CMIP and ATP2C2 modulate phonological short-term memory in language impairment. Am J Hum Genet 85(2): 264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Buka SL, Shenassa ED, Niaura R (2003) Elevated risk of tobacco dependence among offspring of mothers who smoked during pregnancy: a 30-year prospective study. Am J Psychiatry 160(11): 1978–84. [DOI] [PubMed] [Google Scholar]
- 35. Stroud LR, Paster RL, Goodwin MS, Shenassa E, Buka S, et al. (2009) Maternal smoking during pregnancy and neonatal behavior: a large-scale community study. Pediatrics 123(5): e842–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.US Federal Trade Commission (2000) Tar, Nicotine, and Carbon Monoxide of the Smoke of 1294 Varieties of Domestic Cigarettes for the Year 1998. Washington DC: US Federal Trade Commission.
- 37. Stuebing KK, Fletcher JM, LeDoux JM, Lyon GR, Shaywitz SE, et al. (2002) Validity of IQ-discrepancy classifications of reading disabilities: A meta-analysis. American Educational Research Journal 39: 469–518. [Google Scholar]
- 38.Stratton K, Howe C, Battaglia F (1996) Fetal Alcohol Syndrome: diagnosis, Epidemiology, Prevention, and Treatment. Washington, DC: Institute of Medicine, National Academy Press.
- 39. Odd DE, Lewis G, Whitelaw A, Gunnell D (2009) Resuscitation at birth and cognition at 8 years of age: a cohort study. Lancet 373(9675): 1615–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Weismer SE, Tomblin JB, Zhang X, Buckwalter P, Chynoweth JG, et al. (2000) Nonword repetition performance in school-age children with and without language impairment. J Speech Lang Hear Res 43(4): 865–78. [DOI] [PubMed] [Google Scholar]
- 41. Mill J, Petronis A (2008) Pre- and peri-natal environmental risks for attention-deficit hyperactivity disorder (ADHD): the potential role of epigenetic processes in mediating susceptibility. J Child Psychol Psychiatry 49(10): 1020–30. [DOI] [PubMed] [Google Scholar]
- 42. Couto JM, Livne-Bar I, Huang K, Xu Z, Cate-Carter T, et al. (2010) Association of reading disabilities with regions marked by acetylated H3 histones in KIAA0319. Am J Med Genet B Neuropsychiatr Genet 153B(2): 447–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Slotkin TA, Seidler FJ (2010) Mimicking maternal smoking and pharmacotherapy of preterm labor: interactions of fetal nicotine and dexamethasone on serotonin and dopamine synaptic function in adolescence and adulthood. Brain Res Bull 82: 124–34. [DOI] [PubMed] [Google Scholar]
- 44. Muneoka K, Ogawa T, Kamei K, Muraoka S, Tomiyoshi R, et al. (1997) Prenatal nicotine exposure affects the development of the central serotonergic system as well as the dopaminergic system in rat offspring: involvement of route of drug administrations. Brain Res Dev Brain Res 102(1): 117–26. [DOI] [PubMed] [Google Scholar]
- 45. Slotkin TA (1998) Fetal nicotine or cocaine exposure: which one is worse? J Pharmacol Exp Ther 285(3): 931–45. [PubMed] [Google Scholar]
- 46. Zhu J, Zhang X, Xu Y, Spencer TJ, Biederman J, et al. (2012) Prenatal nicotine exposure mouse model showing hyperactivity, reduced cingulated cortex volume, reduced dopamine turnover, and responsiveness to oral methylphenidate treatment. J Neurosci 32(27): 9410–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yang BZ, Kranzler HR, Zhao H, Gruen JR, Luo X, et al. (2007) Association of haplotypic variants in DRD2, ANKK1, TTC12, and NCAM1 to alcohol dependence in independent case control and family samples. Hum Mol Genet 16(23): 2844–53. [DOI] [PubMed] [Google Scholar]
- 48. London ED, Berman SM, Mohammadian P, Ritchie R, Mandelkern MA, et al. (2009) Effect of the TaqIA polymorphism on ethanol response in the brain. Psychiatry Res 174(3): 163–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bolton JL, Marioni RE, Deary IJ, Harris SE, Stewart MC, et al. (2010) Association between polymorphisms of the dopamine receptor D2 and catechol-o-methyl transferase genes and cognitive function. Behav Genet 40(5): 630–8. [DOI] [PubMed] [Google Scholar]
- 50. Bertolino A, Taurisano P, Pisciotta NM, Blasi G, Fazio L, et al. (2010) Genetically determined measures of striatal D2 signaling predict prefrontal activity during working memory performance. PLoS One 5(2): e9348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McAllister TW, Flashman LA, Harker Rhodes C, Tyler AL, Moore JH, et al. (2008) Single nucleotide polymorphisms in ANKK1 and the dopamine D2 receptor gene affect cognitive outcome shortly after traumatic brain injury: a replication and extension study. Brain Inj 22(9): 705–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wise RA (2004) Dopamine, learning and motivation. Nat Rev Neurosci 5(6): 483–94. [DOI] [PubMed] [Google Scholar]
- 53. Frank MJ, O’Reilly R (2006) A mechanistic account of striatal dopaminefunction in human cognition: Psychopharmacological studes with cabergoline and haloperidol. Behav Neurosci 120: 497–517. [DOI] [PubMed] [Google Scholar]
- 54. Lee J, Tomblin JB (2012) Reinforcement learning in young adults with developmental language impairment. Brain Lang 123(3): 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gathercole SE, Baddeley AD (1990) Phonological memory deficits in language disordered children: Is there a causal connection? J Mem Lang 29: 336–60. [Google Scholar]
- 56. Montgomery W (2003) Working memory and comprehension in children with specific language impairment: what we know so far. J Commun Disord 36(3): 221–31. [DOI] [PubMed] [Google Scholar]
- 57. Ullman MT (2004) Contributions of memory circuits to language: the declarative/procedural model. Cognition 92(1–2): 231–270. [DOI] [PubMed] [Google Scholar]
- 58. Nicolson RI, Fawcett AJ (2007) Procedural learning difficulties: reuniting the developmental disorders? Trends Neurosci 30(4): 135–141. [DOI] [PubMed] [Google Scholar]
- 59.Gupta P, Dell GS (1999) The emergence of language from serial order and procedural memory. In: MacWhinney B, ed. The Emergence of Language, 28th Carnegie Mellon Symposium on Cognition. Hillsdale, NJ: Lawrence Erlbaum: 447–482.
- 60. Berman SM, Noble EP (1995) Reduced visuospatial performance in children with the D2 dopamine receptor A1 allele. Behav Genet 25(1): 45–58. [DOI] [PubMed] [Google Scholar]
- 61. Noble EP, Blum K, Ritchie T, Montgomery A, Sheridan PJ (1991) Allelic association of the D2 dopamine receptor gene with receptor-binding characteristics in alcoholism. Arch Gen Psychiatry 48(7): 648–54. [DOI] [PubMed] [Google Scholar]
- 62. Noble EP, Gottschalk LA, Fallin JH, Ritchie TL, Wu JC (1997) D2 dopamine receptor polymorphism and brain regional glucose metabolism. Am J Med Genet 74(2): 162–6. [PubMed] [Google Scholar]
- 63. Huang W, Payne TJ, Ma JZ, Beuten K, Dupont RT, et al. (2009) Significant association of ANKK1 and detection of a functional polymorphism with nicotine dependence in an African-American sample. Neuropsychopharmacology 34(2): 319–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distribution of covariates among smoking groups. Values are either percentages or means (SD). *Indicates χ2 two-tailed p-value <0.05 from univariate analyses of each covariate and prenatal nicotine exposure outcome. **Indicates ANOVA p-value <0.05 from comparison of each covariate and prenatal nicotine exposure outcome.
(DOC)
Comparison of those included in analyses and the overall ALSPAC cohort. Data are presented as either percentages or mean (SD).
(DOC)