Abstract
Large perigastric or periduodenal pseudocysts are a potential cause of gastric outlet obstruction, usually requiring interventional drainage of the pseudocysts. In contrary most of the small pseudocysts are asymptomatic and require no therapy. However, certain small pseudocysts can produce clinically significant problem depending on their location. Here we report a case of small pseudocyst (12.0 mm in width) with a unique shape and location causing significant Gastric outlet obstruction treated successfully with endoscopy.
Key words: pancreatic pseudocyst, gastric outlet obstruction
Introduction
Gastric outlet obstruction (GOO) is a clinical syndrome characterized by epigastric abdominal pain and post-prandial vomiting due to mechanical obstruction. The etiologies of GOO are usually isolated gastric pathology, duodenal pathology or extra-luminal disease causing external compression at the gastric or duodenal wall.
Severe acute pancreatitis, chronic pancreatitis and large size pancreatic pseudocysts are among the extra-luminal causes of GOO often requiring interventional therapy. Small pancreatic pseudocysts are usually asymptomatic and require no therapy. However, in rare occasion, they may produce significant symptoms depending upon their location (i.e. small pancreatic pseudocyst could cause biliary obstruction). GOO due to external compression caused by small pseudocyst is extremely rare. Here we report a case of significant GOO caused by small pseudocyst (12.0 mm) with a unique shape and location, successfully treated with endoscopy.
Case
52-year-old Caucasian male was referred to our clinic for the evaluation of epigastric abdominal pain associated with nausea, vomiting and early satiety for few weeks. Past medical history was significant for chronic pancreatitis, thought to be secondary to heavy smoking and alcohol use. His medications were nutritional supplements only.
The physical examination was unremarkable except for mild to moderate epigastric tenderness. Laboratory tests including completed blood count, complete metabolic profile, liver function tests and pancreatic enzymes were with in normal limit. CAT scan of abdomen revealed dilated pancreatic duct and small peripancreatic fluid collection (pseudocyst) surrounding the pylorus. The patient underwent upper endoscopy, ERCP and EUS for further evaluation and management. The upper endoscopy revealed external compression surrounding the pyloric channel causing significant pyloric stenosis (Fig. 1, Fig. 2). The endosonographic examination showed donut shaped anechoic cystic lesion, 12.0 mm in width, encircling the pylorus in 360 degrees (Fig. 3). The ERCP revealed no communication between the pancreatic duct and the pseudocyst. Endoscopic Cystogastrostomy was performed and two double pigtail stents (10 French × 4 cm & 7 French × 4 cm) were placed successfully at the ostomy site adjacent to the pylorus (Fig. 4), complete resolution of the pyloric stenosis was noted immediately after the pseudocyst drainage. The patient's symptoms improved after the procedure and follow up CAT scan after 4 weeks revealed complete resolution of the pseudocyst. The cystogastrostomy stents were removed 2 weeks later. The patient continued to be asymptomatic in a 6 month follow up.
Figure 1.
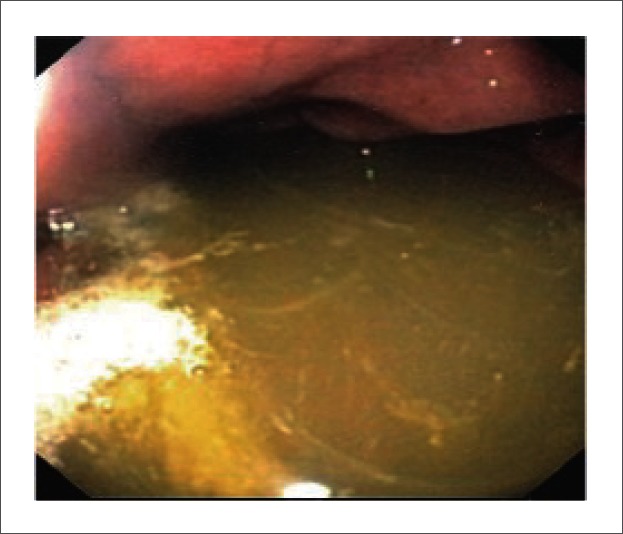
Retained fluid in the stomach due to gastric outlet obstruction
Figure 2.

Endoscopic view of stenotic pylorus caused by encircling pancreatic pseudocyst
Figure 3.
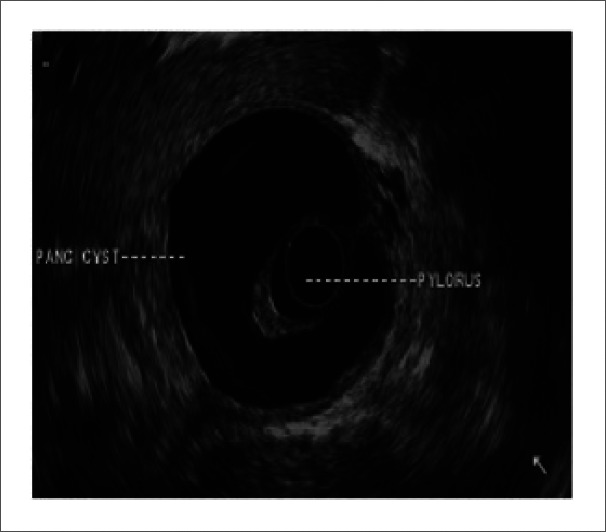
Endosonographic view of donut shaped pseudocyst encircling the pylorus
Figure 4.
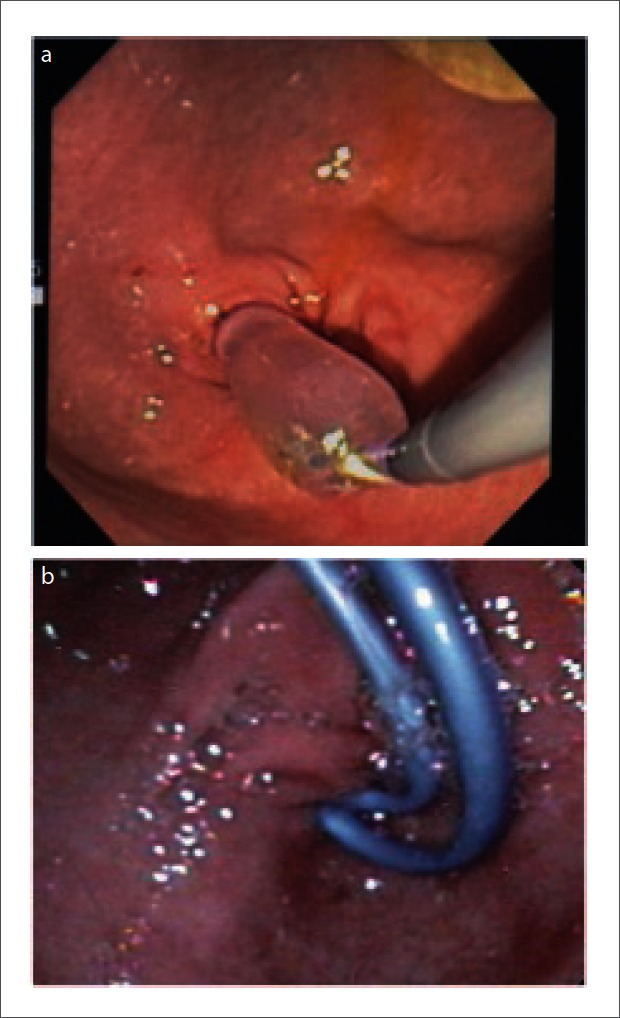
a: Endoscopic cystgastrostomy with tract dilation using balloon dilator; b: Placement of 2 double pigtail stents for cyst drainage.
Discussion
Pancreatic pseudocyst is a well-recognized complication of pancreatitis.1 Limited natural history data suggest that up to 40 percent of pseudocysts resolve without intervention.2,3 However, symptomatic pseudocysts present when they cause external compression to the adjacent organs, get infected, bleed or rupture.4 Large pancreatic pseudocyst causing external compression is well-documented cause of gastric outlet obstruction.5 Our patient presented with significant gastric outlet obstruction caused by a small pancreatic pseudocyst due to its unusual location and shape. The size of the pancreatic pseudocyst was only 12.0 mm in width, encircling the pylorus in a donut shape and causing significant gastric outlet obstruction.
The diagnosis of GOO caused by small pancreatic pseudocyst can be made radiologically and/or endoscopically. Interventional endoscopic, percutaneous, or surgical drainage is needed for the treatment of symptomatic obstructive pancreatic pseudocyst.
Endoscopic drainage has shown outstanding results in multiple reports using cystgastrostomy or cystoduodenostomy approach.6 Resolution rate reaches up to 89% with recurrence rates ranging from 6–18%.7 Surgical drainage are reserved for recurrence or for endoscopic failures and may be associated with substantial morbidity (25%) and mortality (5%).8–10
In our case, EUS-guided endoscopic cystgastrostomy was successfully performed despite the small size and the unique shape of the pseudocyst. Small dilator balloon (12 mm) over the wire was enough to dilate the stoma of the cystgastrostomy and only two small pigtail stents were used to drain the pseudocyst due to the limited size of it.
Conclusion
Small pancreatic pseudocysts may cause significant symptomatic gastric outlet obstruction when they have a certain shape and location. EUS guided cystgastrostomy still considered to be the optimal therapy despite the small size of the pseudocyst.
Abbreviations
- GOO
gastric outlet obstruction
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
Conflict of interest
None.
References
- 1.Vitello JM. Gastric intramural pseudocyst with associated gastric outlet obstruction: recognition and management. South Med J. 1996;89:534–537. doi: 10.1097/00007611-199605000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol. 2009;15:38–47. doi: 10.3748/wjg.15.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheruvu CV, Clarke MG, Prentice M, Eyre-Brook IA. Conservative treatment as an option in the management of pancreatic pseudocyst. Ann R Coll Surg Engl. 2003;85:313–316. doi: 10.1308/003588403769162413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Risti B, Marincek B, Jost R, Decurtins M, Ammann R. Hemosuccus pancreaticus as a source of obscure upper gastrointestinal bleeding: three cases and literature review. Am J Gastroenterol. 1995;90:1878–1880. [PubMed] [Google Scholar]
- 5.Fitzgibbons TJ, Green G, Silberman H, Eliasoph J, Halls JM, Yellin AE. Management of Crohn's disease involving the duodenum, including duodenal cutaneous fistula. Arch Surg. 1980;115:1022–1028. doi: 10.1001/archsurg.1980.01380090006003. [DOI] [PubMed] [Google Scholar]
- 6.Adams DB, Anderson MC. Percutaneous catheter drainage compared with internal drainage in the management of pancreatic pseudocyst. Ann Surg. 1992;215:571–576. doi: 10.1097/00000658-199206000-00003. discussion 6–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arvanitakis M, Delhaye M, Bali MA, Matos C, Le Moin O, Deviere J. Endoscopic treatment of external pancreatic fistulas: when draining the main pancreatic duct is not enough. Am J Gastroenterol. 2007;102:516–524. doi: 10.1111/j.1572-0241.2006.01014.x. [DOI] [PubMed] [Google Scholar]
- 8.Kohler H, Becker HD. [Pancreatic hemorrhage. A contribution to the differential diagnosis of gastrointestinal bleeding] Chirurg. 1984;55:526–527. [PubMed] [Google Scholar]
- 9.Gumaste VV, Pitchumoni CS. Pancreatic pseudocyst. Gastroenterologist. 1996;4:33–43. [PubMed] [Google Scholar]
- 10.Bergman S, Melvin WS. Operative and nonoperative management of pancreatic pseudocysts. Surg Clin North Am. 2007;87:1447–1460. doi: 10.1016/j.suc.2007.09.003. [DOI] [PubMed] [Google Scholar]


