Abstract
Endosonography (EUS)-guided biliary drainage is a novel therapeutic option for patients with biliary obstruction after failed endoscopic retrograde cholangiopancreatography (ERCP). Many case reports and series worldwide have shown satisfactory clinical outcomes in terms of technical and clinical success rates, which approach 80%–100%. However, these procedures need to be performed by experts to minimize the possible complications, which have been reported in as many as 14–35% of patients. The most common complications encountered in these procedures are bile leakage, pneumoperitoneum, peritonitis, and stent related complications such as stent migration. Here, we report the case of a female patient who had cholangiocarcinoma and underwent EUS-guided hepaticogastrostomy after failed ERCP; stent malposition occurred during the procedure, leading to biloma formation that was successfully treated with EUS-guided biloma drainage.
Key words: iatrogenic biloma, endosonography-guided hepaticogastrostomy
Introduction
Endosonography (EUS)-guided biliary drainage (BD) is a novel EUS-based therapeutic approach that can be used for patients after failed endoscopic retrograde cholangiopancreatography (ERCP) for BD.1 The overall failure rate of ERCP is reported to be 5%–10%.2 Failure could result from surgically altered anatomy or malignant tumor invasion; bile duct cannulation is unsuccessful in such cases. Before the era of EUS-guided therapy, most patients had to undergo percutaneous transhepatic drainage (PTBD) or surgery. These 2 platforms, however, carried a significant mortality rate of 5–32%.3,4 The first EUS-guided choledochoduodenostomy was reported by Giovannini et al.5 in 2001, followed by many case reports and series worldwide. The first case series by Giovannini et al.6 on EUS-guided hepaticogastrostomy was published in 2007. In 2008, the EUS working group published an article that summarized EUS-BD indications, techniques, and complications.7 Subsequently, these BD procedures were considered an effective alternative to surgery and PTBD due to similar success rate but less complications. The complication rate reported for EUS-BD performed by experts was 0–10%. The most common complications are bile leakage, pneumoperitoneum, peritonitis and stent migration.8–11 Here, we report an unusual complication that occurred during self-expendable metal stent (SEMS) deployment and led to stent malposition and biloma formation. The complication could be successfully corrected using an endoscopic approach.
Case report
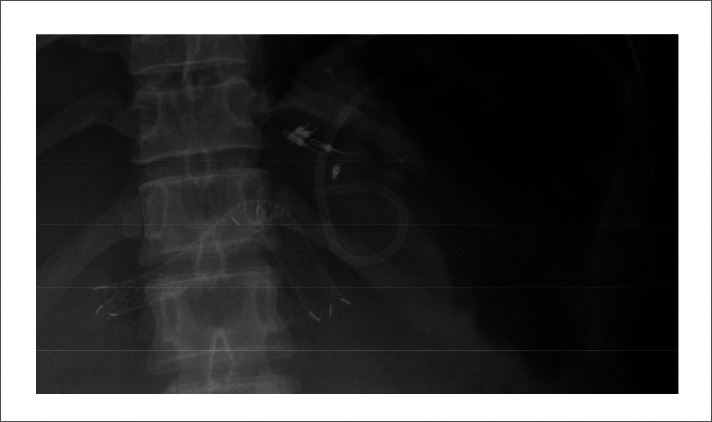
The patient was a 53-year-old woman who was a known case of unresectable cholangiocarcinoma and lung metastasis and had been referred for EUS-BD due to failed ERCP. EUS-guided hepaticogastrostomy was performed for the patient using the sequential dilatation technique.12 During SEMS deployment, the distal end of the SEMS accidentally slipped out of the gastric wall with acute angulation at the mid portion (Fig. 1). Neither free air nor contrast leakage was seen. We terminated the procedure and applied multiple metal clips to close the gastric wall defect. Physical examination did not show any signs of peritonitis. The surgeon recommended conservative treatment. The patient was discharged 1 week later without any other complications. Two weeks later, she developed abdominal discomfort. A computed tomography (CT) scan showed loculated fluid (4.5 × 3.5-cm area) at the intraperitoneal end of the expanded SEMS, which resembled a biloma. The patient refused surgery; therefore, she was rescheduled for drainage collection 2 weeks later. Under general anesthesia, the curvilinear echoscope was used to localize the biloma (Fig. 2). A 19-gauge needle was punctured through the gastric wall into biloma, and the aspirated content was found to have a deep green color. Contrast injection was performed. The needle tract was dilated using tapered-tip Teflon catheters (sizes 7.0 and 8.5), followed by insertion of a 7-Fr 7-cm double pigtail stent with satisfactory drainage (Fig. 3, Fig. 4). The patient was hospitalized for 5 days. A follow-up CT scan showed no residual fluid collection. The patient died 4 months later from massive pulmonary metastasis. To our knowledge, this is the first report of successful conservative treatment for iatrogenic intra-abdominal collection following EUS-BD.
Figure 1.
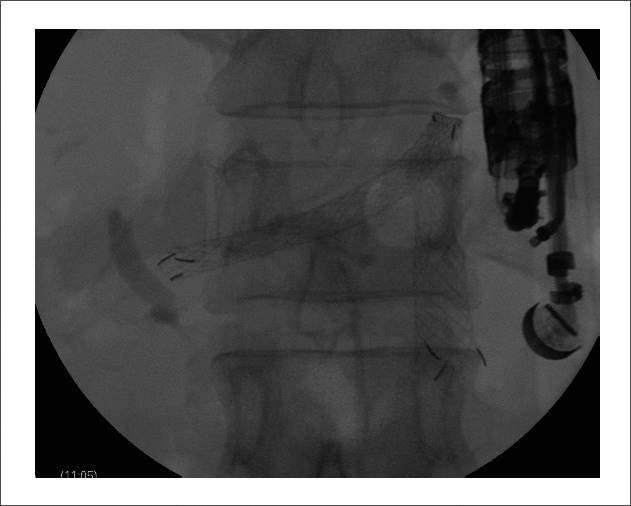
The self-expandable metal stent accidentally slipped out of the gastric wall during stent deployment. The acute angle of the stent can be seen.
Figure 2.

Echo view of the fluid collection, with the distal end of the self-expandable metal stent located within this region.
Figure 3.
Radiographic view showing the self-expandable metal stent and the double pigtail stent.
Figure 4.
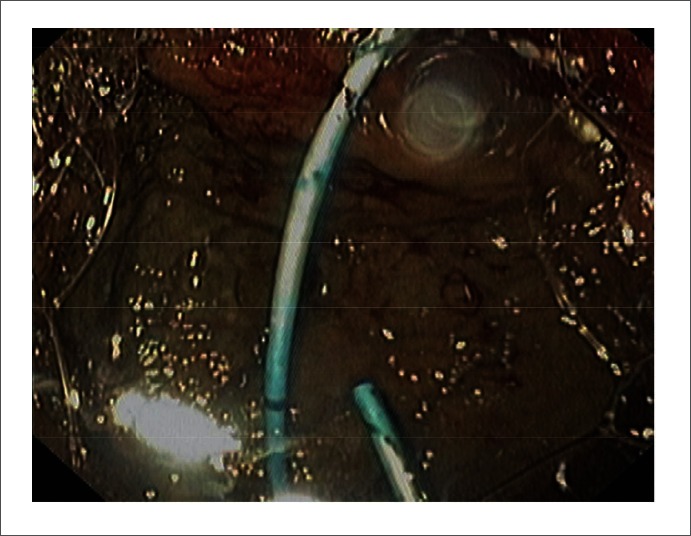
Endoscopic view of the double pigtail stent.
Discussion
Stent malposition is an uncommon complication of EUS-BD. In the present case, the stent accidentally slipped out of the gastric wall during deployment. The patient did not develop generalized peritonitis but developed symptomatic biloma later. We hypothesized that the absence of generalized bile peritonitis could be due to 2 possible reasons. The first one is that dilatation of the neotract by using only a tapered tip Teflon catheter made the tract so small that it prevented sudden expansion of the SEMS. Second, the neotract between the gastric cardia and intra-hepatic bile duct in segment II was more easily created and the space between these 2 organs was narrower than the neotract connecting the proximal gastric body and intra-hepatic bile duct segment III. Consequently, the SEMS slipped out of the gastric wall and the stent angulation occurred. This angulation prevented sudden leakage of bile, which might have led to the generalized bile peritonitis. EUS-guided drainage of the biloma and intra-abdominal fluid collection have been reported earlier only by Shami et al. and Piraca et al.13,14 Both groups reported biloma drainage as a consequence of surgery, and these procedures were found to be feasible and safe. The technique we used in this case did not differ from those used for pancreatic pseudocyst drainage, and the clinical outcome was satisfactory. We found that the techniques we used, that is, non-cauterization without balloon dilatation, might be beneficial for minimizing EUS-BD-related complications.
Abbreviations
- EUS
endosonography
- ERCP
endoscopic retrograde cholangiopancreatography
- BD
biliary drainage
- PTBD
percutaneous transhepatic drainage
- SEMS
self-expendable metal stent
- CT
computed tomography
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
References
- 1.Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, et al. Endoscopic ultrasound-guided choledochoduodenostomy in patients with failed endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2008;14:6078–6082. doi: 10.3748/wjg.14.6078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giovannini M, Bories E. EUS-guided biliary drainage. Gastroenterol Res Pract. 2012;2012:348719. doi: 10.1155/2012/348719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tarantino I, Barresi L, Fabbri C, Traina M. Endoscopic ultrasound guided biliary drainage. World J Gastrointest Endosc. 2012;4:306–311. doi: 10.4253/wjge.v4.i7.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chavalitdhamrong D, Draganov PV. Endoscopic ultrasound-guided biliary drainage. World J Gastroenterol. 2012;18:491–497. doi: 10.3748/wjg.v18.i6.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33:898–900. doi: 10.1055/s-2001-17324. [DOI] [PubMed] [Google Scholar]
- 6.Bories E, Pesenti C, Caillol F, Lopes C, Giovannini M. Transgastric endoscopic ultrasonography-guided biliary drainage: results of a pilot study. Endoscopy. 2007;39:287–291. doi: 10.1055/s-2007-966212. [DOI] [PubMed] [Google Scholar]
- 7.Itoi T, Yamao K. EUS 2008 Working Group document: evaluation of EUS-guided choledochoduodenostomy (with video) Gastrointest Endosc. 2009;69:S8–S12. doi: 10.1016/j.gie.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Yamao K, Hara K, Mizuno N, Sawaki A, Hijioka S, Niwa Y, et al. EUS-guided biliary drainage. Gut Liver. 2010;4:S67–S75. doi: 10.5009/gnl.2010.4.S1.S67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Artifon EL, Ferreira FC, Sakai P. Endoscopic ultrasound-guided biliary drainage. Korean J Radiol. 2012;13:S74–S82. doi: 10.3348/kjr.2012.13.S1.S74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamao K. EUS-guided choledochoduodenostomy. Gastrointest Endosc. 2009;69:S194–S199. doi: 10.1016/j.gie.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 11.Park do H. Endoscopic ultrasonography-guided hepaticogastrostomy. Gastrointest Endosc Clin N Am. 2012;22:271–280. doi: 10.1016/j.giec.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Prachayakul V, Aswakul P, Kachinthorn U. Tapered-tip Teflon catheter: another device for sequential dilation in endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2011;43:E213–E214. doi: 10.1055/s-0030-1256395. [DOI] [PubMed] [Google Scholar]
- 13.Shami VM, Talreja JP, Mahajan A, Phillips MS, Yeaton P, Kahaleh M. EUS-guided drainage of bilomas: a new alternative? Gastrointest Endosc. 2008;67:136–140. doi: 10.1016/j.gie.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 14.Piraka C, Shah RJ, Fukami N, Chathadi KV, Chen YK. EUS-guided transesophageal, transgastric, and transcolonic drainage of intra-abdominal fluid collections and abscesses. Gastrointest Endosc. 2009;70:786–792. doi: 10.1016/j.gie.2009.04.049. [DOI] [PubMed] [Google Scholar]


