Abstract
Facial burns are generally considered severe. This is due to the possibility of respiratory complications. First responders check the nostrils for singed hairs. In severe cases there may be soot around the nose and mouth and coughing may produce phlegm that includes ash. Facial and inhalational burns compromise airways. They pose difficulties in pre-hospital resuscitation and are challenge to clinicians managing surviving burn victims in the intensive care setting. Management problems – resuscitation, airway maintenance and clinical treatment of facial injuries are compounded if the victim is child. Inhalational burns reduce survivability, certainly in adult victim. In our retrospective study we found that facial burns dominated in male gender, liquids and scalds are the most common causes of facial burns in children whereas the flame and electricity were the most common causes of facial burns in adults. We came to the conclusion in our study that surgical treatment minimizes complications and duration of recovery.
Key words: facial burns, texture, deeply burned.
1. INTRODUCTION
The head and neck region is the most frequent site where a burn injury occurs. These percentages vary between 27 to 60%, depending on country, the setting and the definition of what constitutes a facial burn. Children represent 25 to 50 % of the total burn population and the prevalence of facial burns in children is between 24 and 52 % (1). The face is a psychologically significant area of the body and its disfigurement has been found to have numerous potential psychosocial consequences for patients. Facial burns are extremely common, making up at least 30 to 50% of minor to moderate burns. Facial burns are also present in over 50% of large burns, the vast majority being partial thickness. Because of the difficulty and complexity of wound care including pain and the frequent cleansing to avoid infection, partial thickness burns of the face, often require hospital care (2-6). Superficial second-degree facial burns usually heal spontaneously without scarring or pigmentary changes. Medium-thickness second-degree burns, which epithelialize in 10 to 14 days, often heal without scarring, although long-term alterations in skin pigmentation and texture are frequent. Medium to deep second-degree burns, which epithelialize in 14 to 28 days or longer, must be carefully monitored because they are prone to the development of late hypertrophic scarring (7)? In the face, full-thickness burns are rare since the high vascularity of the face rapidly dissipates the heat. (8, 9).
Also facial burns are often caused by flash burns, which usually cause partial-thickness burns. However, full-thickness burns can be seen, especially in contact burns and in the event of prolonged exposure to the heating source, for example if the patient was sub- or unconscious or paralyzed at the time of accident. In addition, in some places (e.g. the nose and ears) facial skin is very thin and more vulnerable to deep burns. If nose and ears are deeply burned, the anatomical structures can change or disappear (8).
2. OBJECTIVE
The objective of this study is to understand the causes of facial burns, depth of facial burns, localization, distribution of facial burns by gender and over years, the methods of treatments.
3. MATERIALS AND METHODS
This is a retrospective study that included 350 patients with facial burns treated in 2006-2011 period in Department of Plastic and Reconstructive Surgery Kosova. The data was collected and analyzed from the archives and protocols of the University Clinical Center of Kosova.
4. RESULTS
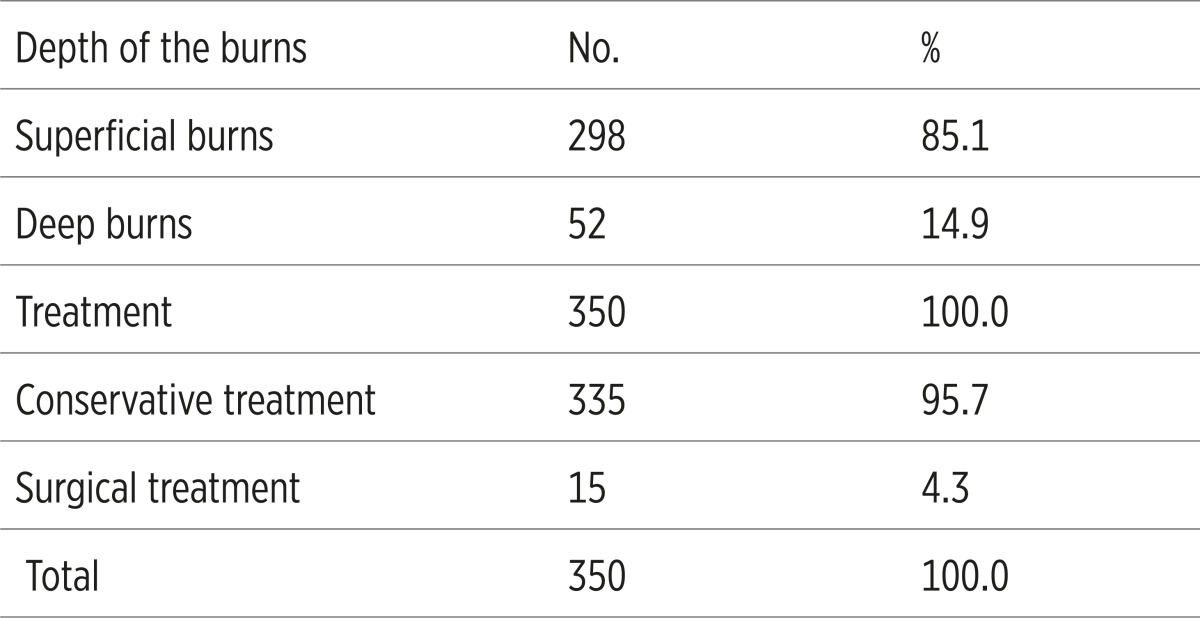
In this retrospective study we included 350 patients in 6 year period with facial burns. Facial burns were predominant in male patients with 291 cases or 83.1% while only 59 were female or 16.9% (Table 1). Scald and liquid was responsible for burns in 156 cases or 44.6%, followed by burns due to flame and fire burns in 109 cases or 31.1% and in 85 cases or 24.3% the cause of facial burns were flame due electricity (Table 1). Nineteen or 5.4% of patients had only a facial burn and 331 of patients or 94.6% were patients who except face have burned other parts of the body (Table 1). Superficial burns were present in 298 cases or 85.1 %, and deep burns were present with 52 cases or 14.9%. Conservative treatments were applied in 335 cases or 95.7% with cleaning of burned surface and therefore surgical treatment were applied in 15 cases or 4.3% (Table 2).
Table 1.
Case distribution by gender, cause and localization
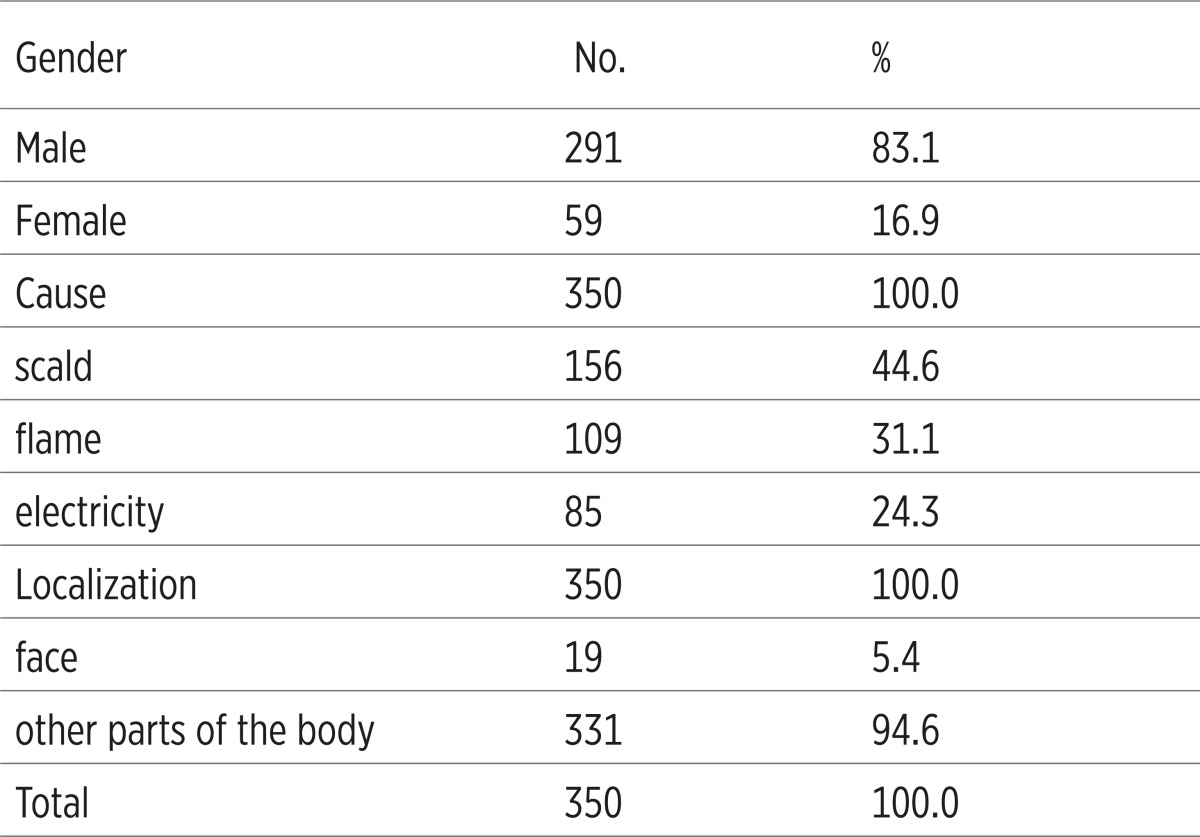 |
Table 2.
Depth of the burns and treatment
 |
5. DISCUSSION
Facial and inhalational burns compromise airways. They pose difficulties in pre-hospital resuscitation and are challenge to clinicians managing surviving burn victims in the intensive care setting (10-11). In this retrospective study we included 350 patients in 6 year period with facial burns. Facial burns were predominant in male patients with 291 cases or 83.1% while only 59 were female or 16.9%. A similar study of 1061 patients with facial burns by Castana et al. reported that females predominated, with an incidence of 61%, compared to a male incidence of 39% (12). Scald and liquid was responsible for burns in 156 cases or 44.6%, followed by burns due to flame and fire burns in 109 cases or 31.1% and in 85 cases or 24.3% the cause of facial burns were flame due electricity. Another similar study of 277 patients conducted by Mustafa H.Ali reported that scalds were the main causes of burn injuries with 49.1%, followed by flame burns with 37.5% (13). Nineteen or 5.4% of patients had only a facial burn and 331 of patients or 94.6% were patients who except face have burned other parts of the body. Superficial burns were present in 298 cases or 85.1%, and deep burns were present with 52 cases or 14.9%. Conservative treatments were applied in 335 cases or 95.7% with cleaning of burned surface and therefore surgical treatment were applied in 15 cases or 4.3%.
6. CONCLUSION
Facial burns are generally considered severe. This is due to the possibility of respiratory complications. First responders check the nostrils for singed hairs. In severe cases there may be soot around the nose and mouth and coughing may produce phlegm that includes ash. Facial and inhalational burns compromise airways. They pose difficulties in pre-hospital resuscitation and are challenge to clinicians managing surviving burn victims in the intensive care setting. Management problems – resuscitation, airway maintenance and clinical treatment of facial injuries are compounded if the victim is child. Inhalational burns reduce survivability, certainly in adult victim. In our retrospective study we found that facial burns dominated in male gender, liquids and scalds are the most common causes of facial burns in children whereas the flame and electricity were the most common causes of facial burns in adults. We came to the conclusion in our study that surgical treatment minimizes complications and duration of recovery.
Conflict of interest
None declared.
REFERENCES
- 1.Hop MJ. Master thesis, University of Groningen, Dept. of Medicine. 2008. Epidemiology of facial burns in Burn Centre Groningen. [Google Scholar]
- 2.Robert H. Demling, Leslie Desanti. Management of partial thickness facial burns (comparison of topical antibiotics and bioengineered skin substitutes) Burns. 1999;25:256–261. doi: 10.1016/s0305-4179(98)00165-x. [DOI] [PubMed] [Google Scholar]
- 3.Roper-Hall M. Immediate treatment of thermal and chemical burns. In: Troutman R, editor. Plastics and reconstructive surgery. Washington: Butterworth; 1962. p. 1991. [Google Scholar]
- 4.Dowling J, Foley, Moncrieff J. Chondritis in the burned ear. Plastic Reconstr. Surg. 1968;42:115–20. doi: 10.1097/00006534-196808000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Baker R, Jones C, Sanders C, et al. Degree of burn, location and length of hospital stay as predictors of psychosocial status and physical functioning. J. Burn Care Rehab. 1998;17:372–32. doi: 10.1097/00004630-199607000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Comitte on trauma. American College of Surgeons. In Resources for optimum care of the injured patient. Chicago. H: The American College of Surgeons; 1990. Resources for optimum care of patients with burn injury; p. 58. [Google Scholar]
- 7.Joseph G. McCarthy, Robert D. Galiano, Sean G. Boutros. Current therapy in Plastic Surgery. Saunders Elsevier; 2006. pp. 184–93. [Google Scholar]
- 8.Van Baar ME, Oen IMMH, Middelkoop E, Nieuwenhuis MK. Topical treatment for facial burns (Protocol) Cochrane Database of Systematic Reviews. 2009;(4) doi: 10.1002/14651858.CD008058.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Choi M, Panthaki ZJ. Tangential Excision of Burn Wounds. Journal of Craniofacial Surgery. 2008;19(4):1056–60. doi: 10.1097/SCS.0b013e318175f4f9. [DOI] [PubMed] [Google Scholar]
- 10.Caroline Acton, et al. Facial burns in children: A series analysis with implications for resuscitation and forensic odontology. Australian Dental Journal. 1999;44(1):20–24. doi: 10.1111/j.1834-7819.1999.tb00531.x. [DOI] [PubMed] [Google Scholar]
- 11.Muguti GI, Doolabh DP, Chakanyuka C, Fleming AN. A review of burns treated over a one year period at Mpilo Central Hospital, Zimbabwe. J R Coll Surg Edinb. 1994;39:214–217. [PubMed] [Google Scholar]
- 12.Castana, et al. Epidemiological survey of burn victims treated as emergency cases in our hospital in the last five years. Ann Burns Fire Disasters. 2008 Dec 31;21(4):171–174. [PMC free article] [PubMed] [Google Scholar]
- 13.Mustafa H. Ali. Pattern of burn injuries at King Fahad Hospital, Al-Baha: A study of 277 cases. Annals of Saudi Medicine. 1997;17(1):104–107. doi: 10.5144/0256-4947.1997.104. [DOI] [PubMed] [Google Scholar]


