Abstract
Context:
Evaluating the translatability and feasibility of an intervention program has become as important as determining the effectiveness of the intervention.
Objective:
To evaluate the applicability of a 3-month jump-landing training program in basketball players, using the RE-AIM (reach, effectiveness, adoption, implementation, and maintenance) framework.
Design:
Randomized controlled trial.
Setting:
National and regional basketball teams.
Patients or Other Participants:
Twenty-four teams of the second highest national division and regional basketball divisions in Flanders, Belgium, were randomly assigned (1:1) to a control group and intervention group. A total of 243 athletes (control group = 129, intervention group = 114), ages 15 to 41 years, volunteered.
Intervention(s):
All exercises in the intervention program followed a progressive development, emphasizing lower extremity alignment during jump-landing activities.
Main Outcome Measure(s):
The results of the process evaluation of the intervention program were based on the 5 dimensions of the RE-AIM framework. The injury incidence density, hazard ratios, and 95% confidence intervals were determined.
Results:
The participation rate of the total sample was 100% (reach). The hazard ratio was different between the intervention group and the control group (0.40 [95% confidence interval = 0.16, 0.99]; effectiveness). Of the 12 teams in the intervention group, 8 teams (66.7%) agreed to participate in the study (adoption). Eight of the participating coaches (66.7%) felt positively about the intervention program and stated that they had implemented the training sessions of the program as intended (implementation). All coaches except 1 (87.5%) intended to continue the intervention program the next season (maintenance).
Conclusions:
Compliance of the coaches in this coach-supervised jump-landing training program was high. In addition, the program was effective in preventing lower extremity injuries.
Key Words: athletic injuries, lower extremity injuries, injury prevention
Key Points.
We used the RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework to assess the translatability and feasibility of a jump-landing training program for preventing lower extremity injuries in basketball players.
Reach, adoption, implementation, and maintenance of the coach-supervised program were rated highly.
The RE-AIM framework is a promising tool for measuring the effects of injury-prevention programs in real-life situations.
Basketball is one of the most popular sports in the world: An estimated 11% of the world's population plays basketball. Basketball is becoming increasingly more popular and is on the way to surpassing the popularity of American football worldwide.1 In Flanders, Belgium, more than 45 000 athletes2 play competitive basketball, and the popularity of the sport continues to grow at all levels from recreational to professional.1,3 In basketball, about one-third of playing time is spent performing relatively high-intensity movements, such as running and jumping.4 A previous study5 in Flanders demonstrated an injury incidence of 9.8 per 1000 exposure hours in basketball, compared with 2.8 per 1000 exposure hours in volleyball.
Most basketball injuries (up to 60%) affect the lower extremities.1,6 In Flemish competition, Cumps et al5 noted that both acute (3.1/1000 hours) and overuse (2.5/1000 hours) lower extremity injuries were inherent to basketball. Proper jump-landing movement patterns are essential for efficiently absorbing the generated impact forces and are thought to be strongly related to the athlete's risk for lower extremity injuries such as patellar tendinopathy and ankle injuries.7–9 The jump-landing maneuver is arguably the most common injury mechanism for these lower extremity injuries.10–12 Negative consequences of injuries are, among other factors, the loss of productivity and high health care cost.13 The high incidence of injuries in basketball and their negative effect on future sports participation call for preventive measures.5
Despite the number of studies published on evidence-based interventions,9,14–16 it is clear that sport–injury-prevention efforts are currently hindered by a limited understanding of their implementation context.17 We need to evaluate the effectiveness of injury prevention in the real-world context of sports under natural and uncontrolled conditions. One way to accomplish this is to use existing health-promotion frameworks to evaluate injury-prevention research efforts. One such model is the RE-AIM evaluation framework designed by Glasgow, Vogt, and Boles18 to evaluate the translatability and feasibility of an intervention program. This framework consists of 5 dimensions18:
Reach: The percentage and representativeness of individuals willing to participate;
Effectiveness: The effect of the intervention on the targeted outcomes;
Adoption: The extent to which the included settings represent the wider population and are adequately described;
Implementation: The degree to which intervention is implemented as intended in the real world; and
Maintenance: The extent to which the program is sustained over time.
Evaluating the 5 dimensions of the RE-AIM framework not only identifies the translatability and feasibility of a program but also defines its limitations.18 Thus, the RE-AIM framework is used to determine if coaches can and will implement an intervention program.19–21 The purpose of our study was to evaluate the applicability of a 3-month jump-landing training program in basketball players using the RE-AIM framework.
METHODS
Study Design
We conducted a randomized controlled trial during 1 season, which included an intervention program that lasted 3 months and a follow-up that lasted 6 months. The study protocol was reviewed and approved by the local ethical committee of the Vrije Universiteit Brussel. The study design has previously been described in detail.22 A brief overview of the materials and methods is presented below.
Participants
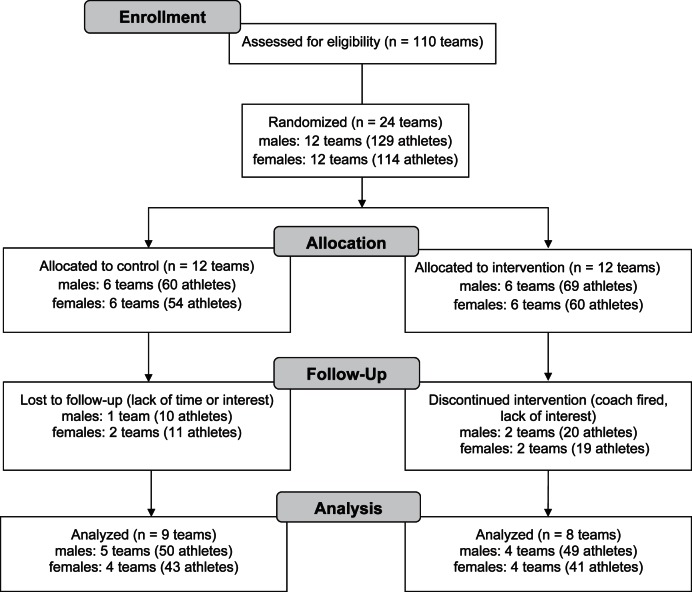
The participants (n = 243) were male (n = 129) or female (n = 114) athletes (Figure 1) from all divisions except the elite (highest) level of Belgian basketball competition.22 Teams were included only if they were hosted in Flanders and mastered the Dutch language. The study was conducted in accordance with the ethical institutional rules for human research and with the Declaration of Helsinki for Medical Research involving human participants. Written informed consent was obtained from each athlete.
Figure 1.
Flow chart showing participant-selection procedures.
Interventions
Teams in the intervention group performed the training program during their regular warm-up, twice a week for 5 to 10 minutes. Teams in the control group were unaware of the existence of an intervention program and did not alter their training sessions. A personal visit by 1 of the involved researchers (sport physiotherapist) with each of the coaches was organized to inform them about the intervention program. During this meeting, the coaches of the intervention teams received DVDs with specific information on the intervention program. The DVD contained detailed information (pictures, videos, and coach's instructions) on how to correctly perform the exercises of the intervention. In addition, a poster illustrating the exercises of the jump-landing program and a handout with written instructions were provided. The coaches received these detailed instructions because they were responsible for supervising and instructing the athletes.
The exercises of the intervention program were based on literature research, including studies investigating prevention programs for acute knee injuries.14,16,23,24 The intervention program (Table 1; Appendix S1 (284KB, pdf) , available online at http://dx.doi.org/10.4085/1062-6050-48.3.18.S1) administered at the start of the 2010–2011 athletic season was targeted at improving the athletes' jump-landing technique, and lasted 3 months.22 During the first month, the exercises focused on basic techniques such as athletic positions, lunges, and side-to-side jumps. In addition, the importance of lower extremity alignment was emphasized. For the next month, the focus shifted to fundamental exercises such as tuck jumps, squat jumps, 1-legged jumps, and jumps on unstable surfaces. Finally, in the third month, which is the performance phase, more complex and sport-specific exercises such as maximal jumps, lay-ups, and running and cutting movements were introduced. No extra equipment was needed to perform the intervention program because every gym contained the required equipment, such as benches and balls.
Table 1.
Overview of the Jump-Landing–Technique Intervention Programa
| Week |
Month |
||||||||
| 1: Technique |
2: Fundamentals |
3: Performance |
|||||||
| Exercise |
Repetitions or Hold Time |
Left and Right Limbs? |
Exercise |
Repetitions or Hold Time |
Left and Right Limbs? |
Exercise |
Repetitions or Hold Time |
Left and Right Limbs? |
|
| 1 | Cocontraction | 10 | Yes | Core stability | 15 | X-hop | 6 | Yes (cycles) | |
| Wall squat | 10 | Pelvic bridge | 10 | Hop-hop-hold | 8 | Yes | |||
| Lateral jump and hold | 8 | Yes | Repeated tuck-jumps | 10 s | Mattress jump | 30 s | |||
| Front lunge | 10 | Squat jump | 10 | Single-legged 90°b | 8 | Yes | |||
| Step-hold | 8 | Yes | Jump, single-legged hold | 8 | Yes | Maximum-squat jump-hold | 10 | Yes | |
| 2 | Cocontraction | 10 | Yes | Pelvic bridge, single-legged | 10 | Crossover-hop-hop-hold | 8 | Yes | |
| Squat | 10 | Prone bridge (elbow-knee) hip extension, shoulder flexion | 10 | Yes | Single-legged 4-way hop-holdb | 3 | Yes (cycles) | ||
| Step-hold | 8 | Yes | Side-to-side tuck jump | 10 s | Single-legged 90° ballb | 8 | Yes | ||
| Walking lunge | 10 | Single-legged lateral hop, hold | 8 | Yes | Step, jump up, down, vertical jump | 5 | Yes | ||
| Lateral jump and hold | 8 | Yes | Hop, hold | 8 | Yes | Maximum-squat jump-hold | 10 | ||
| 3 | Squat | 10 | Single-legged pelvic bridgeb | 10 | Yes | Single-legged 4-way hop-hold ballb | 4 | Yes (cycles) | |
| Lateral jump and hold | 8 | Yes | Prone bridge hip extension | 10 | Yes | Single-legged 180° | 10 | Yes | |
| Single tuck-jump, soft landing | 10 | Yes | Side-to-side tuck jump | 10 | Yes | Jump, jump, jump, vertical jump | 10 | ||
| Lunge jump | 10 s | Lateral hop | 10 s | Mattress jump | 40 s | ||||
| Lateral jump | 10 | Two-legged 90° | 8 | Yes | Running, jump down on 1 leg, jump | 8 | Yes | ||
| 4 | Squat jump | 10 | Single-legged pelvic bridge ball | 10 | Yes | Single-legged 180° | 10 | Yes | |
| Lateral jump | 10 s | Prone bridge hip extension, opposed shoulder flexionb | 10 | Yes | Jump, jump, jump, vertical jump | 15 | |||
| Double tuck jump | 8 | Lateral hop with ball | 10 s | Running, jump down on 1 leg, jump | 10 | Yes | |||
| Broad jump | 10 | Yes | Single-legged lateral hop-hold | 5 | Yes | Lay-upc | 10 | ||
| Scissor jump | 8 | Single-legged 90° | 8 | Yes | Height jumpc | 10 | |||
Performed 2×/wk for 10 min, with 1-min rest between repetitions.
Exercise on a mattress.
Sport-specific jumps for basketball; can be adjusted to the athlete's sport.
Outcomes
Researchers were appointed to supervise weekly the completion of the injury-registration and exposure-measurement forms and to determine if all exercises in the intervention program were being performed. The researchers observed solely whether the program was executed and whether the required forms were adequately completed by the coaches (injury registration and exposure time). Under no circumstances did they interfere with the intervention program. One goal was independent implementation of the intervention program by the coaches. However, if questions arose in the intervention group, the researchers were allowed to answer questions regarding the content of the program.
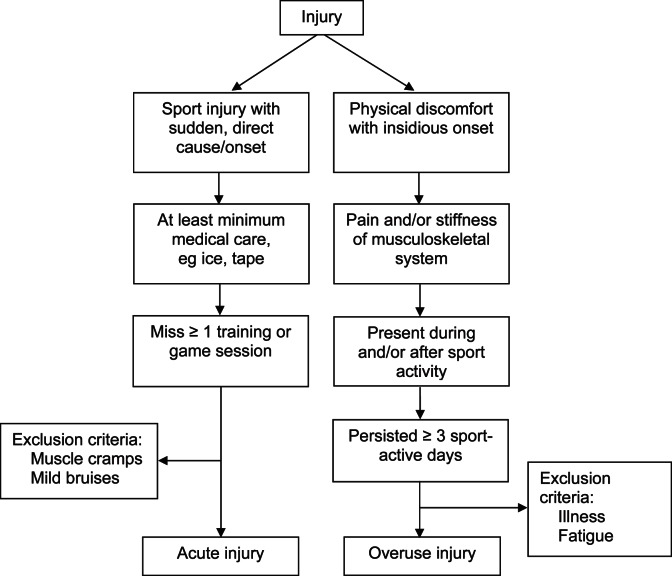
At baseline, all athletes completed a questionnaire that asked about demographic information, a history of previous injuries, and past and current sports participation.5,14 So that we could determine the effectiveness of this injury-prevention program, all acute and overuse injuries that occurred during the 2010–2011 season were registered for both the intervention and control teams by the coaches using flow charts (Figure 2).5,22 If an injury occurred, the coach and athlete completed the injury-registration form (written version of the BLITS Online Injury Diary, Vrije Universiteit Brussel, Belgium)25 within 1 week of injury onset. To enable us to determine the hours of exposure to basketball and adherence to the intervention program, the coaches of the intervention group quantitatively recorded, on a weekly basis, whether the prevention program (duration = 3 months) was carried out and logged the attendance rate of each player during training. The coaches of the control group were also asked to register the attendance rate and exposure hours of each athlete. Only the time exposed to basketball activities and the injuries sustained in relation to these activities were considered for determining the injury incidence density.
Figure 2.
Injury definitions.
In addition, the coaches completed a questionnaire at follow-up (April–May 2011), after the prevention program was completed. A Likert scale ranging from agree to completely disagree was used to evaluate the potential of the intervention in terms of translation and feasibility. The coaches also answered questions on how many times the athletes performed the exercises and whether the exercises were performed as described. They were asked whether, in their opinions, the jump-landing injury-prevention program could become part of their future training sessions.
The training program was evaluated for translatability and feasibility to determine the generalizability to real-world application. For this purpose, the 5 dimensions of the RE-AIM framework were used: Reach, effectiveness, adoption, implementation, and maintenance. Except for effectiveness, where the intervention and control groups were compared, only the intervention group was taken into account. More information on calculating these dimensions is provided in the statistical analysis.
Sample Size
The prevalence of lower extremity injuries in basketball in Flanders is about 78% in 1 season.13 We considered a difference of 50% in the incidence of lower extremity injuries between the intervention and control groups after a follow-up of 1 season to be clinically relevant. To detect the intended difference of 50% in the incidence of lower extremity injuries with a power of 90% and an α of 5%, a total of 34 participants per group were needed. Assuming a dropout rate of about 20%, we needed a total of 82 athletes to detect a potentially clinically relevant effect of the intervention. However, because teams served as units of randomization, a cluster effect was taken into account. Therefore, for an intracluster correlation coefficient of 20%, 220 athletes from 24 teams needed to be included at baseline.
Recruitment
Based on a power analysis, we assigned 24 of the 110 Flemish teams of the regional, second, and third national divisions using computerized randomization. Randomization and group allocation (1:1) took place before teams were contacted. If an assigned team was not willing to participate, the team was replaced with another team from the backup randomization list. This backup randomization list was created to guarantee the required number of teams based on power analysis, and the procedure was the same for the intervention and control groups. Neither group was aware of the other, which was important to avoid motivational bias, known as the Hawthorne effect.26
Statistical Analyses
A Pearson χ2 test (nominal data) and independent-samples t test (ratio data) were used to determine homogeneity for all demographic data (P < .05). Injury incidence density, henceforth addressed in this article as incidence, and corresponding 95% confidence intervals (95% CIs) were calculated for the number of new injuries per 1000 exposure hours. If an athlete suffered multiple injuries, only the first injury was considered in the analysis, and the athlete was removed from the study to determine effectiveness. Because the unit of allocation was teams, we performed a multilevel Cox proportional hazard regression analysis using SPSS (version 19.0; Chicago, IL) to estimate the hazard ratios (HRs) and 95% CIs. More information on the calculations of the different dimensions of the RE-AIM framework is provided in Table 2.
Table 2.
Calculations of the Dimensions of the RE-AIM Framework
| RE-AIM |
Numerator |
Denominator |
| Reach, % | ||
| Setting level | Eligible teams in IG | Randomized IG teams |
| Individual level | Eligible athletes in IG | Athletes on randomized IG teams |
| Representativeness | Eligible teams in IG | Teams playing at described competition levels (Flanders, Belgium) |
| Effectiveness (injury incidence density and hazard ratio) | ||
| Setting level | Difference in lower extremity injury risk per 1000 exposure hours between the IG and control group | |
| Adoption, % | ||
| Setting level | Teams approached that agreed to participate and implement the program | Eligible teams |
| Implementation | ||
| Setting level | Coaches who successfully implemented key program elements | Coaches of randomized IG teams |
| Individual level | Program sessions followed by athletes of randomized IG teams | Program sessions that ideally needed to be followed by randomized IG teams |
| Adherence | Program sessions followed by IG athletes who eventually implemented the program | Program sessions that ideally needed to be followed by IG teams that eventually implemented the program |
| Maintenance | Proportion of coaches who planned to continue the intervention program in future seasons | |
Abbreviations: IG, intervention group; RE-AIM, reach, effectiveness, adoption, implementation, maintenance.
RESULTS
Reach
Twenty-four teams were asked to participate in the study. After randomization, 12 teams were allocated to the intervention group. Of these 12 teams, all (100%) agreed to participate (setting level). This also represents a reach of approximately 11.8% of all the participating teams (12 of 102 teams) at all national levels of the Flemish basketball competition (representativeness). From the 12 teams in the intervention group, a total of 129 athletes agreed to participate in the study (individual level). Of the athletes who started the injury-prevention program, all were eligible to follow the program (100%). An overview of the baseline data for the intervention and control groups and the dropouts (age, height, weight, body mass index) is provided in Table 3. The athletes participating in this study were homogeneous for these demographic data.
Table 3.
Participants' Demographic Information
| Group |
Sex |
n |
Mean ± SD |
|||
| Age, y |
Height, cm |
Weight, kg |
Body Mass Index, kg/m2 |
|||
| Groups | ||||||
| Control | Men | 50 | 26.7 ± 5.2 | 189.2 ± 8.2 | 87.7 ± 10.8 | 24.5 ± 2.2 |
| Women | 43 | 22.9 ± 3.9 | 174.1 ± 6.9 | 64.6 ± 8.4 | 21.2 ± 1.9 | |
| Intervention | Men | 49 | 24.9 ± 4.9 | 189.9 ± 7.6 | 87.2 ± 12.1 | 24.1 ± 2.6 |
| Women | 41 | 23.7 ± 5.8 | 173.5 ± 5.8 | 65.3 ± 8.9 | 21.7 ± 2.3 | |
| Group dropouts | ||||||
| Control | Men | 10 | 24.5 ± 7.6 | 193.0 ± 7.2 | 90.5 ± 12.3 | 24 ± 2.5 |
| Women | 11 | 19.5 ± 4.0 | 172.2 ± 5.7 | 61.4 ± 7.0 | 20.6 ± 1.8 | |
| Intervention | Men | 20 | 23.8 ± 5.7 | 192.0 ± 5.7 | 89.3 ± 16.9 | 24.2 ± 1.5 |
| Women | 19 | 20.5 ± 4.7 | 172.5 ± 6.7 | 61.9 ± 9.7 | 20.8 ± 2.7 | |
Effectiveness
Overall Injuries.
To evaluate the effectiveness of the training program, we analyzed the program, taking cluster allocation into account (Table 4). The overall incidence of lower extremity injuries was 3.6/1000 hours (95% CI = 1.9, 5.25) in the intervention group and 5.4/1000 hours (95% CI = 3.4, 7.3) in the control group. The risk of a lower extremity injury was lower in the former than in the latter (HR = 0.40 [95% CI = 0.16, 0.99]).
Table 4.
Effectiveness of Jump-Landing Intervention Program in Preventing Injuries
| Injury Type |
Exposure, h |
Injuries, n |
Injury Incidence Density (95% CI) |
Hazard Ratio (CG Versus IG) |
| Lower extremity | ||||
| CG | 5226.5 | 28 | 5.4 (3.4, 7.3) | 0.40 (0.16, 0.99)a |
| IG | 5009.7 | 18 | 3.6 (1.9, 5.25) | |
| Acute | ||||
| CG | 5226.5 | 21 | 4.0 (2.3, 5.7) | 0.37 (0.12, 1.1) |
| IG | 5009.7 | 15 | 3.0 (1.48, 4.5) | |
| Overuse | ||||
| CG | 5226.5 | 7 | 1.4 (0.35–2.33) | 0.47 (95% CI: 0.09–2.56) |
| IG | 5009.7 | 5 | 1.0 (0.12–1.87) | |
Abbreviations: CI, confidence interval; CG, control group; IG, intervention group.
Difference between control and intervention groups (P < .05).
Acute Lower Extremity Injuries.
For acute lower extremity injuries, the incidences in the control group (4.0 [95% CI = 2.3, 5.7]) and intervention group (3.0 [95% CI = 1.48, 4.5]) were not different. The control group had an increased risk of acute injuries, although it was not significantly different (HR = 0.37 [95% CI = 0.12, 1.1]).
Overuse Lower Extremity Injuries.
The risk of overuse injuries in the control group (incidence = 1.4 [95% CI = 0.35, 2.33]) and the intervention group (incidence = 1.0 [95% CI = 0.12, 1.87]) was not different, as confirmed by the HR (0.47 [95% CI = 0.09, 2.56]).
Adoption
At the start of the study, all teams (100%) agreed to take part. Two of the 12 teams in the intervention group were no longer willing to participate at the first follow-up (2 weeks after the start), and 2 other teams dropped out in the following month, resulting in an adoption rate of 66.7%. After the study, all coaches of the remaining teams acknowledged the importance of incorporating injury-prevention training in their schedules. Two coaches specifically mentioned that they felt that their athletes were stronger and performed better after the jump-landing training program. The participating coaches agreed (37.5%, n = 3) or totally agreed (50%, n = 4) that the provided information was thorough enough that they could understand and correctly instruct their athletes in the exercises. One coach did not use the handouts because the information on the DVD provided him with sufficient information to conduct the intervention program.
Implementation
Of all participating teams, 66.7% (n = 8) performed the jump-landing program at least twice a week, as recommended (setting level), and were convinced of the positive effects of the training. Session attendance among the athletes initially participating in this study was 60% of the prescribed training time (individual level). The 4 teams that never started the intervention program were considered dropouts and were excluded from the adherence analysis. Adherence among the athletes who completed the program was 86%. The average number of program sessions missed by individual athletes was 2 ± 3 sessions.
Maintenance
Only 1 coach found the program to be time consuming; nonetheless, the team completed the intervention program. Other coaches found the jump-landing program to be easily compatible with their training and considered it time well spent. Of the participating coaches, 75% (n = 6) indicated that they definitely would like to use the injury-prevention program, preferably during the preseason. All coaches who integrated the jump-landing program into their training sessions indicated that they were aware of the importance of injury prevention and found the program to be compatible with their normal training intensity and strategy.
DISCUSSION
Main Findings
At present, our understanding of the implementation possibilities of a coach-supervised injury-prevention program is limited. The main purpose of this study was to determine the translatability and feasibility of a coach-supervised exercise program on jump-landing technique to reduce injury occurrence using the 5 dimensions of the RE-AIM framework.18 Our results are important because they combine lower extremity injury-rate data after an injury-prevention program with information about the implementation aspects.
The RE-AIM framework is a relatively new concept, and although it is gaining in popularity, there is still no easy way to generate an overall RE-AIM score. We found no information on what is defined as a good or inadequate percentage of the different dimensions of the framework (reach, effectiveness, adoption, implementation, maintenance). Furthermore, comparisons with previous research are limited; although several groups14,24,27,28 studied coach-supervised intervention programs, only one27 addressed all the different dimensions of the RE-AIM framework.
In total, all teams randomized to the intervention group agreed to participate, and all athletes in the intervention group were eligible to participate in the intervention program, resulting in a reach of 100% at both the setting and individual levels. However, 2 weeks after the start, several teams in the intervention group (n = 4/12) reported not being willing to participate any longer, resulting in an adoption rate of 66.7%. In our study, reach at the initial level was higher than in the study of Labella et al28 (100% and 36.8%, respectively). In their study, a coach-led neuromuscular warm-up was performed with the aim of reducing lower extremity injuries in female public high school soccer and basketball athletes. The dropout rate in our coach-supervised training program was higher than theirs (33% versus 5.2%). This difference can be explained by the fact that, at the start of the study by Labella et al,28 a large number of coaches refused to participate. Coaches in both investigations gave similar reasons for declining to participate (eg, lack of time or interest). In our study, however, 1 coach dropped out because he was fired, yet the dropout rates of both the intervention and control groups were similar in our study.
An important finding is that the attendance rate of the teams of the intervention group that completed the jump-landing intervention program was 86% (implementation). The session attendance rate of all teams originally randomized to the intervention group was 60%, a result comparable with other studies.27,28 We did not investigate the demographic data of the coaches. The literature suggests that coaches who were older or overweight or appeared less physically fit tended to include fewer prescribed exercises.27 Not only can knowledge and beliefs influence the attitude toward injury prevention,29 but apparently the coach's demographic characteristics can, too.27
The coaches found the jump-landing program to be easily compatible with their training and worth the invested time. A total of 75% of the coaches (n = 67) in the intervention group intended to continue the training program during the following season (maintenance), preferably in the preseason. This suggests that coaches are aware that sufficient preparation of athletes is important in preventing injuries. Preseason conditioning can have a positive influence on injury prevention.16,30 However, we investigated 1 season only, so we do not know if coaches can implement the warm-up consistently over several seasons or need retraining to maintain compliance.
The intervention group had 5009.7 exposure hours (n = 90 athletes), and the control group had 5226.5 exposure hours (n = 93 athletes). The intervention group had 18 lower extremity injuries (incidence = 3.6 [95% CI = 1.9, 5.25]), whereas the control group sustained 28 lower extremity injuries (incidence = 5.4 [95% CI = 3.4, 7.3]). The HR shows that the risk (effectiveness) of a lower extremity injury was lower in the intervention group than in the control group (HR= 0.40 [95% CI = 0.16, 0.99]). Labella et al28 reported an injury rate of 1.78/1000 hours (95% CI = 1.29, 2.28) in the intervention group and 4.19/1000 hours (95% CI = 3.35, 5.02) in the control group. The difference in injury rate can be attributed to our taking only the first injury into account, unlike Labella et al, who calculated the overall injury rate. Myklebust et al14 and Mandelbaum et al24 reported only anterior cruciate ligament injuries, so comparisons for injury incidence are difficult.
Although the RE-AIM framework provides an indication of the translatability and feasibility of the intervention program, no cutoff points exist to describe what is defined as good or excellent reach, adoption, effectiveness, implementation, and maintenance. The RE-AIM framework is relatively new, and researchers are constantly improving the framework. This method might be promising for future researchers whose purpose is to investigate implementing interventions in real-life situations.
Limitations
The fact that the questionnaires used for the evaluations were based on self-reports by the coaches is a limitation to this study. The coaches of each team recorded injuries, exposure, and compliance. The validity and reliability of their recordings, however, were not monitored. When the registration forms were not completed during or immediately after a training session or match, the coaches had to complete the registration forms in a retrospective manner within 1 week. A thorough data registration was performed to ensure that all information on effectiveness was provided: Any missing information or consistencies on the injury-registration and exposure forms were addressed. Minimal follow-up to optimize correct registration was conducted by contacting the coaches weekly. Consequently, recall bias is presumably small because most coaches followed the protocol and submitted their registration forms on a weekly basis.
The injury-prevention program was evaluated for effectiveness with regard to injury incidence, translatability, and feasibility. These factors are important for detecting the overall injury-prevention effect in real-life situations. An intervention that is not adequately adopted or sustained is unlikely to have a significant effect. The coach-supervised intervention program is an easy-to-use training program. Coaches indicated that it was easy to integrate into their regular teaching routines and that they intended to implement the program during the following seasons. However, we studied only 1 season, so we do not know if coaches will actually implement the injury-prevention program consistently over several seasons.
Another limitation is the high dropout rate, reducing the total number of athletes in the intervention group to 90 and in the control group to 93. Because of all the measurements during the season, participating in the study required much more time than simply participating in the intervention. It is possible that the extra time required for the evaluation process discouraged coaches from participating. As mentioned before, the number of dropouts in the intervention and control groups, however, was similar. Furthermore, baseline variables of players who were lost to follow-up did not differ from the other players. Bias due to selective dropout is consequently believed to be limited.
The HR showed a difference between groups, indicating that the intervention program was effective in preventing lower extremity injuries. Due to the high dropout rate, our sample size was probably too small to detect a significant effect for individual groups. Future researchers should focus on larger-scale implementation to distinguish between male and female athletes and acute and overuse lower extremity injuries. It might also be valuable to investigate if the effectiveness relates to all injuries, new injuries, and reinjuries. This information would be helpful in promoting the implementation and maintenance of our coach-supervised jump-landing intervention program. Representativeness was approximately 11.8% of all participating teams at all national levels of Flemish basketball competition. Before translating the effectiveness and applicability of this intervention program, we must bear in mind that the study was done on only a small portion of the basketball population; however, the results are very promising.
Strengths of the Injury-Prevention Program
An injury-prevention protocol requiring active participation from physicians or physical therapists or expensive equipment would limit the potential for future use, so this coach-instructed jump-landing program is an important development in preventing injuries in real-life settings. It was developed to address previously identified risk factors for lower extremity acute and overuse injuries related to jump landings.19 The intervention program was designed based on information about injury mechanisms and effective prevention strategies from previous studies.16,23 The thorough instructions on the DVDs that were provided to the coaches allowed them to correctly implement the injury-prevention program and to train their athletes accordingly. Cumps et al25 implemented a balance-training program for basketball athletes and found that the 20-minute session was quite lengthy given that most teams trained only 2 or 3 times per week for 1.5 or 2 hours each. The exercises per session were therefore kept to a minimum, and the choice was made to have several (at least 2) sessions per week. This schedule made the program less time consuming and easier to implement compared with intensive intervention programs lasting 20 minutes per session. To improve injury-prevention awareness, both coaches and athletes should be educated.
The effect of injury-prevention awareness was minimized by not informing the control group of the intervention group and vice versa. This was done in order to avoid any motivational bias, and the teams were instructed not to alter their normal training frequency or strategy. The long-term effectiveness of the jump-landing training program in preventing lower extremity injuries and whether the potential protection persists remains to be seen. However, given these results, we can conclude that introducing the jump-landing program will reduce the number of lower extremity injuries in general and acute injuries in particular, which would likely indicate sustainable injury prevention. Previous researchers31,32 have shown the importance of incorporating instructions for jump-landing techniques into the intervention program. When investigating the merits of the program, we should focus on its effectiveness in preventing injuries but also take a closer look at its influence on the jump-landing technique itself. After all, athletes who are defined as being at risk are likely to benefit from specific intervention programs designed to improve jump-landing technique.16,33–35
CONCLUSIONS
We used the RE-AIM evaluation framework to evaluate a jump-landing injury-prevention program for translatability and feasibility. Overall reach, adoption, implementation, and maintenance of this coach-supervised intervention program were high. Most coaches found the jump-landing program to be readily compatible with their current training regimens and believed that time spent on injury prevention was time well spent. They intended to make this program part of their regular training routine. In addition, lower extremity injuries were fewer in the intervention group than in the control group. To confirm these results and investigate if differences can be found for acute and overuse injuries in female and male athletes, further research on a larger scale is needed. The RE-AIM is a promising tool to measure the effect of injury-prevention programs in real-life situations.
ACKNOWLEDGMENTS
This study was financially supported by the Flemish Government through the establishment of the policy “Research Center Sports, Youth and Culture.” We thank all the athletes and people responsible for successful participation on a voluntary basis.
SUPPLEMENTAL MATERIAL
Found at DOI: http://dx.doi.org/10.4085/1062-6050-48.3.18.S1
REFERENCES
- 1.Harmer PA. Basketball injuries. Med Sport Sci. 2005;49:31–61. doi: 10.1159/000085341. [DOI] [PubMed] [Google Scholar]
- 2.Royal Belgian Basketball Federation. 2012 Aug; http://www.basketbelgium.be. Accessed. [Google Scholar]
- 3.Schiltz M, Lehance C, Maquet D, Bury T, Crieland JM, Croisier JL. Explosive strength imbalances in professional basketball players. J Athl Train. 2009;44(1):39–47. doi: 10.4085/1062-6050-44.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Backx FJ, Beijer HJ, Bol E, Erich WB. Injuries in high-risk persons and high risk-sports: a longitudinal study of 1818 school children. Am J Sports Med. 1991;19(2):124–130. doi: 10.1177/036354659101900206. [DOI] [PubMed] [Google Scholar]
- 5.Cumps E, Verhagen E, Meeusen R. Prospective epidemiological study of basketball injuries during one competitive season: ankle sprains and overuse knee injuries. J Sport Sci Med. 2007;6(2):204–211. [PMC free article] [PubMed] [Google Scholar]
- 6.Dick R, Hertel J, Agel J, Grossman J, Marshall SW. Descriptive epidemiology of collegiate men's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):194–201. [PMC free article] [PubMed] [Google Scholar]
- 7.Bisseling RW, Hof AL, Bredeweg SW, Zwerver J, Muider T. Are the take-off and landing phase dynamics of the volleyball spike jump related to patellar tendinopathy? Br J Sports Med. 2008;42(6):483–489. doi: 10.1136/bjsm.2007.044057. [DOI] [PubMed] [Google Scholar]
- 8.Reeser JC, Verhagen E, Briner WW, Askeland TI, Bahr R. Strategies for the prevention of volleyball related injuries. Br J Sports Med. 2006;40(7):594–600. doi: 10.1136/bjsm.2005.018234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bahr R, Lian O, Bahr IA. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports. 1997;7(3):172–177. doi: 10.1111/j.1600-0838.1997.tb00135.x. [DOI] [PubMed] [Google Scholar]
- 10.Ferretti A, Papandrea P, Conteduca F, Mariani PP. Knee ligament injuries in volleyball players. Am J Sports Med. 1992;20(2):203–207. doi: 10.1177/036354659202000219. [DOI] [PubMed] [Google Scholar]
- 11.Agel J, Olson DE, Dick R, Arendt EA, Marshall SW, Sikka RS. Descriptive epidemiology of collegiate women's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):202–210. [PMC free article] [PubMed] [Google Scholar]
- 12.Harringe ML, Renstrom P, Werner S. Injury incidence, mechanism and diagnosis in top-level teamgym: a prospective study conducted over one season. Scand J Med Sci Sports. 2007;17(2):115–119. doi: 10.1111/j.1600-0838.2006.00546.x. [DOI] [PubMed] [Google Scholar]
- 13.Cumps E, Verhagen E, Annemans L, Meeusen R. Injury rate and socioeconomic costs resulting from sports injuries in Flanders: data derived from sports insurance statistics 2003. Br J Sports Med. 2008;42(9):767–772. doi: 10.1136/bjsm.2007.037937. [DOI] [PubMed] [Google Scholar]
- 14.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35(3):368–373. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 17.Finch CF, Donaldson A. A sports setting matrix for understanding the implementation context for community sport. Br J Sports Med. 2010;44(13):973–978. doi: 10.1136/bjsm.2008.056069. [DOI] [PubMed] [Google Scholar]
- 18.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collard DC, Chinapaw MJ, Verhagen EA, van Mechelen W. Process evaluation of a school based physical activity related injury prevention programme using the RE-AIM framework. BMC Pediatr. 2010;10:86. doi: 10.1186/1471-2431-10-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Antikainen I, Ellis R. A. RE-AIM evaluation of theory-based physical activity interventions. J Sport Exerc Psychol. 2011;33(2):198–214. doi: 10.1123/jsep.33.2.198. [DOI] [PubMed] [Google Scholar]
- 21.Shubert TE, Altpeter M, Busby-Whitehead J. Using the RE-AIM framework to translate a research-based falls prevention intervention into a community-based program: lessons learned. J Safety Res. 2011;42(6):509–516. doi: 10.1016/j.jsr.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Aerts I, Cumps E, Verhagen E, Meeusen R. Efficacy of a 3 month training program on the jump-landing technique in jump-landing sports: design of a cluster randomized controlled trial. BMC Musculoskel Dis. 2010;11:281. doi: 10.1186/1471-2474-11-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 24.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 25.Knaepen K, Cumps E, Zinzen E, Meeusen R. Low-back problems in recreational self-contained underwater breathing apparatus divers: prevalence and specific risk factors. Ergonomics. 2009;52(4):461–473. doi: 10.1080/00140130802707766. [DOI] [PubMed] [Google Scholar]
- 26.Cumps E, Verhagen E, Meeusen R. Efficacy of a sports specific balance training programme on the incidence of ankle sprains in basketball. J Sport Sci Med. 2007;6(2):212–219. [PMC free article] [PubMed] [Google Scholar]
- 27.Berthelot JM, Le Goff B, Maugars Y. The Hawthorne effect: stronger than the placebo effect? Joint Bone Spine. 2011;78(4):335–336. doi: 10.1016/j.jbspin.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 28.LaBella CR, Huxford MR, Grissom J, Kim K-Y, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165(11):1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 29.Soligard T, Nilstad A, Steffen K, et al. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med. 2010;44(11):787–793. doi: 10.1136/bjsm.2009.070672. [DOI] [PubMed] [Google Scholar]
- 30.Walter SD, Sutton JR, McIntosh JM, Connolly C. The aetiology of sport injuries: a review of methodologies. Sports Med. 1985;2(1):47–58. doi: 10.2165/00007256-198502010-00005. [DOI] [PubMed] [Google Scholar]
- 31.Heidt RS, Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 32.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 33.Onate JA, Guskiewicz KM, Marshall SW, Giuliani C, Yu B, Garrett WE. Instruction of jump-landing technique using videotape feedback: altering lower extremity motion patterns. Am J Sports Med. 2005;33(6):831–842. doi: 10.1177/0363546504271499. [DOI] [PubMed] [Google Scholar]
- 34.Myer GD, Ford KR, Hewett TE. Methodological approaches and rationale for training to prevent anterior cruciate ligament injuries in female athletes. Scand J Med Sci Sports. 2004;14(5):275–285. doi: 10.1111/j.1600-0838.2004.00410.x. [DOI] [PubMed] [Google Scholar]
- 35.Myer GD, Chu DA, Brent JL, Hewett TE. Trunk and hip control neuromuscular training for the prevention of knee joint injury. Clin Sports Med. 2008;27(3):425–448. doi: 10.1016/j.csm.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.