Abstract
Context:
Noncontact anterior cruciate ligament injury has been reported to occur during the later stages of a game when fatigue is most likely present. Few researchers have focused on progressive changes in lower extremity biomechanics that occur throughout fatiguing.
Objective:
To evaluate the effects of a sequential fatigue protocol on lower extremity biomechanics during a sidestep-cutting task (SS).
Design:
Controlled laboratory study.
Setting:
Laboratory.
Patients or Other Participants:
Eighteen uninjured female collegiate soccer players (age = 19.2 ± 0.9 years, height = 1.66 ± 0.5 m, mass = 61.6 ± 5.1 kg) volunteered.
Intervention(s):
The independent variable was fatigue level, with 3 levels (prefatigue, 50% fatigue, and 100% fatigue). Using 3-dimensional motion capture, we assessed lower extremity biomechanics during the SS. Participants alternated between a fatigue protocol that solicited different muscle groups and mimicked actual sport situations and unanticipated SS trials. The process was repeated until fatigue was attained.
Main Outcome Measure(s):
Dependent variables were hip- and knee-flexion and abduction angles and internal moments measured at initial contact and peak stance and defined as measures obtained between 0% and 50% of stance phase.
Results:
Knee-flexion angle decreased from prefatigue (−17° ± 5°) to 50% fatigue (−16° ± 6°) and to 100% fatigue (−14° ± 4°) (F2,34 = 5.112, P = .004). Knee flexion at peak stance increased from prefatigue (−52.9° ± 5.6°) to 50% fatigue (−56.1° ± 7.2°) but decreased from 50% to 100% fatigue (−50.5° ± 7.1°) (F2,34 = 8.282, P = 001). Knee-adduction moment at peak stance increased from prefatigue (0.49 ± 0.23 Nm/kgm) to 50% fatigue (0.55 ± 0.25 Nm/kgm) but decreased from 50% to 100% fatigue (0.37 ± 0.24) (F2,34 = 3.755, P = 03). Hip-flexion angle increased from prefatigue (45.4° ± 10.9°) to 50% fatigue (46.2° ± 11.2°) but decreased from 50% to 100% fatigue (40.9° ± 11.3°) (F2,34 = 6.542, P = .004). Hip flexion at peak stance increased from prefatigue (49.8° ± 9.9°) to 50% fatigue (52.9° ± 12.1°) but decreased from 50% to 100% fatigue (46.3° ± 12.9°) (F2,34 = 8.639, P = 001). Hip-abduction angle at initial contact decreased from prefatigue (−13.8° ± 6.6°) to 50% fatigue (−9.1° ± 6.5°) and to 100% fatigue (−7.8° ± 6.5°) (F2,34 = 11.228, P < .001). Hip-adduction moment decreased from prefatigue (0.14 ± 0.13 Nm/kgm) to 50% fatigue (0.08 ± 0.13 Nm/kgm) and to 100% fatigue (0.06 ± 0.05 Nm/kg) (F2,34 = 5.767, P = .007).
Conclusions:
The detrimental effects of fatigue on sagittal and frontal mechanics of the hip and knee were visible at 50% of the participants' maximal fatigue and became more marked at 100% fatigue. Anterior cruciate ligament injury-prevention programs should emphasize feedback on proper mechanics throughout an entire practice and not only at the beginning of practice.
Key Words: anterior cruciate ligament, knee, fatiguing, kinematics, kinetics
Key Points.
A progressive change in lower extremity mechanics occurred for knee-flexion angle, hip-abduction angle, and internal hip-adduction moment.
Hip flexion at initial contact and peak stance and knee flexion at peak stance had subtle altered patterns from prefatigue to 50% fatigue and a sudden change at 100% fatigue.
As participants progressed from prefatigue to 50% fatigue, they adopted a posture that may protect knee structures during hip flexion at initial and peak stance and knee flexion at peak stance.
Fatigue consistently is implicated as a mechanism of injury for the lower extremity in athletes. Acute and extended periods of fatigue can occur within peripheral and central control systems,1 the latter of which is considered the predominant cause of injury.2 In previous longitudinal studies3–5 over a competitive season, investigators have demonstrated that injuries occur at a greater rate in the latter portion of practices and games and the latter portion of the season. Decomposition of neuromuscular control has been the focus of researchers studying injuries due to fatigue.6
Deficiencies in neuromuscular control can predispose an athlete to an increased risk of lower extremity injury.7,8 For athletes who initially do not demonstrate such deficiencies in neuromuscular control, the onset of fatigue can decrease neuromuscular control to levels that increase the likelihood of injury. Researchers2,9 have viewed the effects of fatigue during single-leg landings and stop-jump tasks and have demonstrated that fatigue alters neuromuscular control. When coupled with simulated gamelike tasks requiring decision-making processes, the effects of fatigue may exacerbate the risk factors for lower extremity injury.1 Specifically, fatigue alters knee-flexion angle and moments, hip internal rotation, and knee-abduction angles and moments.1,2,6,9 These variables have been identified as potential risk factors for anterior cruciate ligament (ACL) injuries.10,11 Furthermore, Hewett et al8 found that knee-valgus angle and moment predicted ACL injury. When the ACL tears during a noncontact mechanism, the lower extremity typically is positioned with the foot firmly planted on the ground, knee abducted and near full extension, femur internally rotated, and tibia externally rotated.12–16 In several observational studies,12,17,18 investigators have shown that ACL injuries occur shortly after initial contact (approximately 40 milliseconds) and with a decreased knee-flexion angle.
A short-term fatigue protocol that uses common athletic skills is of interest for assessing lower extremity biomechanical changes throughout the fatiguing process.6 To our knowledge, only a few researchers2,6,9,19 have included drills that athletes commonly use (eg, soccer skills) in their fatigue protocols. A regimen that incorporates athletic drills specific to the athletic event (eg, cut right, up-and-down) and deceleration and accelerations (eg, 5-10-5) with changes in direction has not been applied in a fatigue protocol. We wanted to understand how multiple neuromuscular demands solicited through specific athletic drills (eg, deceleration, acceleration) performed during cutting and pivoting tasks commonly are associated with ACL tears.14 Therefore, the purpose of our study was to evaluate the effects of a short-term fatigue protocol on lower extremity biomechanics during a sidestep-cutting task. We hypothesized that throughout the fatigue protocol (prefatigue, 50% fatigue, and 100% fatigue), participants would have a sequential (1) decrease in knee- and hip-flexion angles, (2) increase in knee- and hip-abduction angles, and (2) increase in internal knee-adduction moment.
METHODS
Participants
Based on the effects of fatigue on lower extremity biomechanics reported in the literature1,2,9 and to achieve 80% statistical power with an α level of .05, a convenience sample of 18 National Collegiate Athletic Association (NCAA) Division I female soccer players (age = 19.2 ± 0.9 years, height = 1.66 ± 0.05 m, mass = 61.6 ± 5.1 kg) was deemed adequate for this study. They did not have any lower extremity injuries and were excluded if they reported a history of lower extremity surgery within 2 years of the study, an injury to the lower extremity within 6 months of the study, ACL injury or surgery, or pregnancy. Participants wore tight-fitting clothing and used the team running shoes (Supernova; adidas AG, Herzogenaurach, Germany). All participants provided written informed consent, and the study was approved by the Institutional Review Board of Old Dominion University.
Experimental Procedures
Lower extremity 3-dimensional joint kinematic and ground reaction force data were recorded throughout the execution of unanticipated tasks. Before testing, we recorded each participant's mass and height and provided approximately 10 minutes to warm up (bicycling and stretching). After the warm-up, we used a VERTEC (Sports Import, Hilliard, OH) device as previously described to obtain maximal vertical jump.9
Participants performed 2 unanticipated tasks (stop jump, sidestep cutting).9,20,21 To create the anticipation factor, a light beam was placed across the area where the participants were running and 2 m before the force plates. When the light beam was interrupted, it triggered a custom-made software program to randomly generate the athletic task (stop jump or sidestep) and project it onto a screen in front of the participant.22 Two timing systems (Brower, Draper, UT) were used to control the approach speed. For the purpose of this study, only the sidestep-cutting task was analyzed, and the stop-jump task was discarded before analysis.
The sidestep-cutting task consisted of a running approach, stepping with the dominant foot on the force plate, cutting to the contralateral side of the dominant foot, and touching the force plate at an angle of approximately 45°.23 The dominant foot was defined as the foot a participant would use to kick a ball the farthest. Before data collection, participants practiced the task 3 times or until they were comfortable with it (average = 4 practice trials). Participants had to perform 2 successful trials of each task between fatigue sets. A trial was considered unsuccessful and repeated if the participant did not land completely on the force plate or could not execute the trial at a minimum speed of 3.5 m/s.20 A single experimenter (N.C.) determined if the trials were successful or unsuccessful.
Functional Agility Short-Term Fatigue Protocol
The functional agility short-term fatigue protocol (FAST-FP) consisted of a series of athletic exercises. Each set of the FAST-FP included 3 countermovement jumps at 90% of maximal vertical jump, step ups and step downs on a 30-cm box for 20 seconds, 3 squats to 90° of knee flexion, and a proagility shuttle run (5-10-5 agility run).24 The protocol started with the participant performing 3 consecutive countermovement jumps, followed by a series of step-up and step-down movements on a 30-cm box for 20 seconds with a metronome set at 200 beats per minute.6 Immediately after completing the step ups, the participant performed 3 squats to 90° of knee flexion. After completing the squats, the participant performed the 5-10-5 agility drill. Between fatigue sets, she had to successfully complete 4 unanticipated trials (2 stop jump, 2 sidestep). Within 5 seconds of successfully completing the 4 tasks, the participant began another set of the fatigue protocol. This was repeated until she achieved maximal fatigue. The criteria for maximal fatigue were (1) the participant did not attain 90% of her maximal jump on all 3 vertical jumps for 2 consecutive fatigue sets or (2) she achieved a heart rate plateau over 3 consecutive fatigue sets that was within 90% of her estimated maximal heart rate.25 We continuously monitored heart rate through a Polar system (model FS2C; Polar Electro, Lake Success, NY).
Biomechanical Analysis
We placed 40 reflective markers, 10 of which were calibration markers, on specific body landmarks.26 Before data collection, we obtained a standing trial and a dynamic trial to calculate hip joint center.27,28 For these trials, participants stood in a neutral position with their upper extremities across their chests. We removed the calibration markers before the fatigue protocol started. We secured pelvic tracking markers with surgical glue, prewrap, and Powerflex tape (Andover Healthcare, Inc, Salisbury, MA) and thigh and shank cluster markers with Powerflex tape. Cluster plates with 5 markers were made to attach to the participants' shoes and secured with athletic tape (Cramer Products Inc, Gardner, KS).
We used 8 high-speed motion-analysis cameras (Vicon, Oxford, UK) sampling at 300 Hz to track marker trajectory and 2 force plates (Bertec Corporation, Columbus, OH) sampling at 1200 Hz to measure ground reaction forces. From the standing trial, a kinematic model (pelvis, thigh, shank, and foot) was created for each participant using Visual 3D software (C-Motion, Germantown, MD) with a least-squares optimization.29 The kinematic model was used to quantify the motion at the hip, knee, and ankle joints, and rotations were expressed relative to the standing trial. A fourth-order, zero-lag Butterworth filter with 7- and 25-Hz cutoff frequencies was used to filter trajectory data and ground reaction force data, respectively.30 To the kinematic and ground force data, we applied an inverse dynamic method with segment inertial characteristics estimated for each participant to calculate 3-dimensional joint forces and moments.31,32 Intersegmental joint moments were defined as internal moments and were expressed to the respective joint-coordinate system (eg, a knee internal-extension moment will resist a flexion load applied to the knee). All data were normalized to 100% of stance, and initial contact was the point at which vertical ground reaction force exceeded 10 N and ended with toe-off.
Statistical Analyses
Before statistical analyses, we normalized fatigue sets to percentage of fatigue. The first set was considered prefatigue (ie, 0%); the last set when maximal fatigue was achieved was considered 100% fatigue. The half point of the total number of sets was determined as 50% fatigue. For example, if 12 total fatigue sets were completed, the sixth set would be 50% fatigue. Independent variables included fatigue level with 3 levels (prefatigue, 50% fatigue, and 100% fatigue). A 1-way, repeated-measures analysis of variance was conducted for each dependent variable at each time instant. Dependent variables were hip- and knee-flexion and -abduction angles and moments, which were measured at initial contact and peak stance.6 Peak-stance dependent measures were obtained between 0% and 50% of stance phase.6 We reduced all data with Visual 3D and a custom-made MATLAB (The MathWorks, Natick, MA) program. Statistical procedures were conducted in PASW (version 18.0; IBM, Somers, NY). Tukey post hoc analysis was used for further evaluation when a main effect was present. The α level was set at .05.
RESULTS
Participants completed an average of 9.4 ± 2.7 sets to achieve maximal fatigue as determined by our criteria. We observed a reduction in approach speed (F2,34 = 5.781, P < .001). Specifically, participants had decreased speeds between prefatigue and 100% fatigue; however, they still met the requirement of at least 3.5 m/s. The Table presents descriptive statistics (means and standard deviations) with the associated statistical values for each dependent measure.
Table.
Dependent Variables at Different Fatigue Levels (Prefatigue, 50% Fatigue, and 100% Fatigue) at Initial Contact and Peak Stance During a Sidestep-Cutting Task (Mean ± SD)
| Variable |
Fatigue Level |
F2,34 |
P |
||
| Prefatigue |
50% |
100% |
|||
| Initial contact | |||||
| Knee flexion, ° | −17 ± 5 | −16 ± 6 | −14 ± 4a | 5.112 | .004 |
| Knee abduction, ° | 0.8 ± 1.9b | −0.3 ± 1.9 | 0.3 ± 2.1 | 3.784 | .03 |
| Knee-adduction moment, Nm/kgm | 0.11 ± 0.08 | 0.08 ± 0.07c | 0.05 ± 0.09c | 5.712 | .003 |
| Hip flexion, ° | 45.4 ± 10.9 | 46.2 ± 11.2 | 40.9 ± 11.3a | 6.542 | .004 |
| Hip abduction, ° | −13.8 ± 6.6 | −9.1 ± 6.5c | −7.8 ± 6.5c | 11.228 | <.001 |
| Hip-adduction moment, Nm/kgm | 0.14 ± 0.13 | 0.08 ± 0.13c | 0.06 ± 0.05c | 5.767 | .007 |
| Peak stance | |||||
| Knee flexion, ° | −52.9 ± 5.6b | −56.1 ± 7.2 | −50.5 ± 7.1b | 8.282 | .001 |
| Knee-adduction moment, Nm/kgm | 0.49 ± 0.23 | 0.55 ± 0.25 | 0.37 ± 0.24b | 3.755 | .03 |
| Hip flexion, ° | 49.8 ± 9.9 | 52.9 ± 12.1 | 46.3 ± 12.9c | 8.639 | .001 |
| Hip-adduction moment, Nm/kgm | 0.72 ± 0.31 | 0.59 ± 0.33 | 0.39 ± 0.29a | 9.483 | <.001 |
Indicates lower than at prefatigue and 50% fatigue.
Indicates lower than at 50% fatigue.
Indicates lower than at prefatigue.
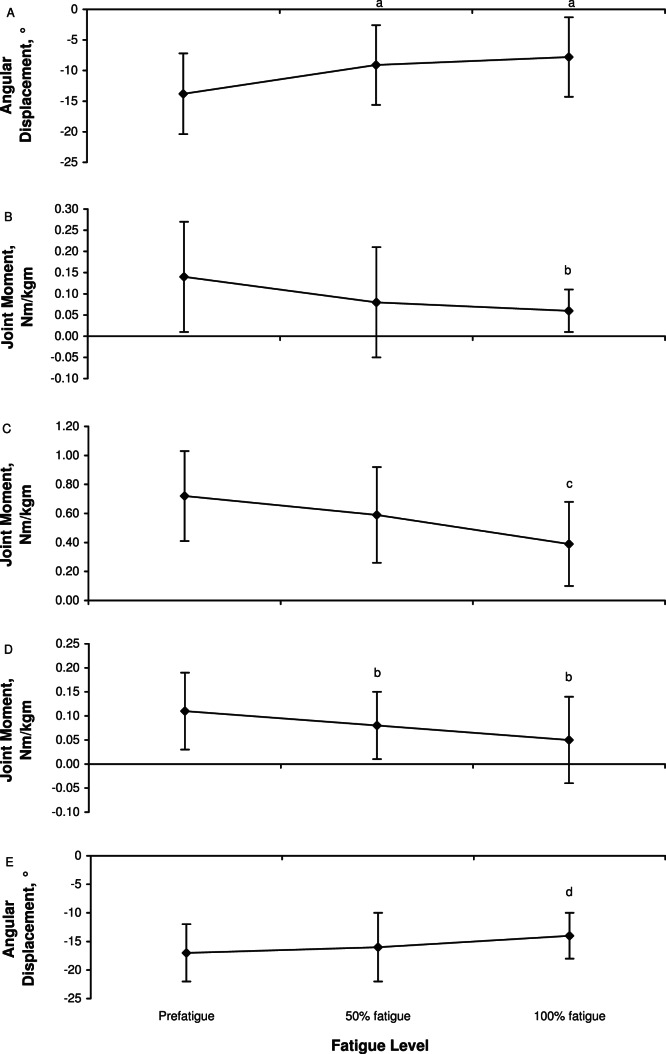
Fatigue influenced several kinematic variables at initial contact. Specifically, knee flexion was less at 100% fatigue than at prefatigue and 50% fatigue (F2,34 = 5.112, P = .004). Similarly, hip abduction at initial contact decreased from prefatigue to 50% and 100% fatigue (F2,34 = 11.228, P < .001). This was accompanied by a decrease in hip- adduction moment at initial contact from prefatigue to 50% and 100% fatigue (F2,34 = 5.767, P = .007). Similarly, at peak stance, internal hip-adduction moment was less at 100% fatigue than at prefatigue and 50% fatigue (F2,34 = 9.483, P < .001). Internal knee-adduction moment at initial contact also decreased throughout the protocol from prefatigue to 50% and 100% fatigue (F2,34 = 5.712, P = .003). Altered lower extremity biomechanics for knee-flexion and hip-abduction angles at initial contact and internal hip-abduction and knee-abduction moments during the fatigue protocol are represented in Figure 1.
Figure 1.
Changes in lower extremity biomechanics throughout the fatiguing protocol for hip-abduction angles at initial contact, A, hip-abduction moment at initial contact, B, hip-abduction moment at peak stance, C, knee-abduction moment at initial contact, D, and knee-flexion angle at initial contact, E. a Indicates less abducted than at prefatigue. b Indicates less than at prefatigue. c Indicates less than at prefatigue and 50% fatigue. d Indicates less knee flexion than at prefatigue and 50% fatigue. These variables presented a progressive deterioration from prefatigue to 100% fatigue.
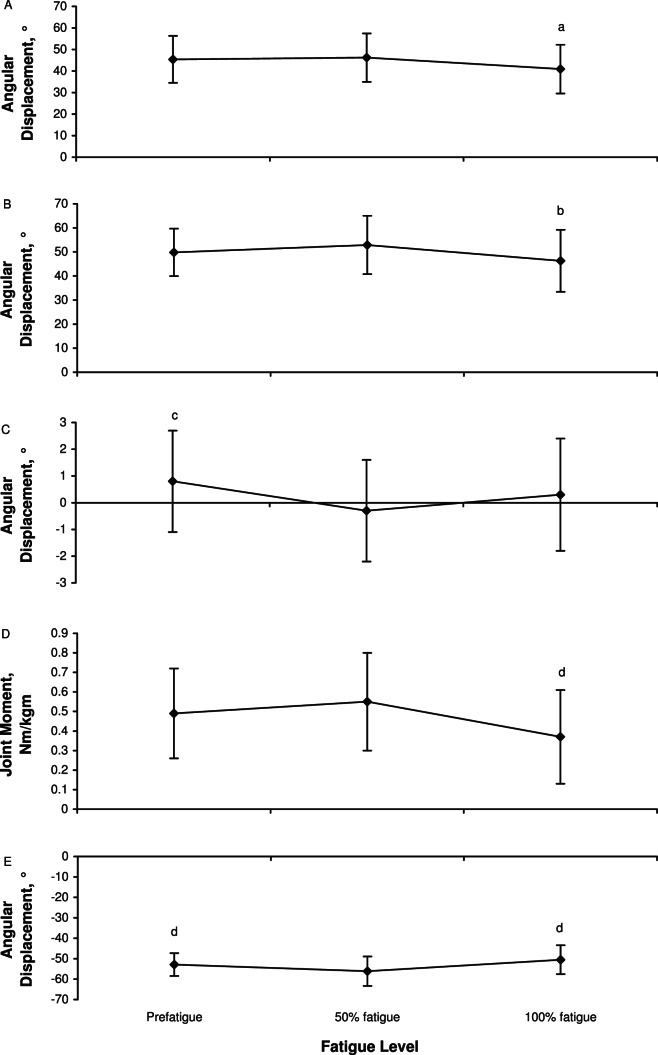
A noteworthy pattern was observed for certain remaining dependent measures. Hip flexion at initial contact (F2,34 = 6.542, P = .004) and peak stance (F2,34 = 8.639, P = .001), knee flexion at peak stance (F2,34 = 8.282, P = .001), knee abduction at initial contact (F2,34 = 3.784, P = .03), and knee-adduction moment at peak stance (F2,34 = 3.755, P = .03) increased from prefatigue to 50% fatigue, then decreased from 50% fatigue to 100% fatigue, which presented values less than prefatigue levels. This pattern is shown in Figure 2. Knee-abduction angle at peak stance was similar among fatigue conditions (prefatigue, 50% fatigue, and 100% fatigue) (F2,34 = 5.679, P > .05).
Figure 2.
A remarkable pattern was observed for some of the dependent measures, hip flexion at initial contact, A, hip flexion at peak stance, B, knee abduction at initial contact, C, knee-adduction moment at peak stance, D, and knee flexion at peak stance, E. These variables describe improved performance from prefatigue to 50% fatigue and a sudden decline from 50% to 100% fatigue. a Indicates less than at prefatigue and 50% fatigue. b Indicates less than at prefatigue. c Indicates less abducted than at 50% fatigue. d Indicates less than at 50% fatigue.
DISCUSSION
We evaluated the effects of a FAST-FP on lower extremity biomechanics during a sidestep-cutting task. Our results partially supported our hypothesis that sequential fatigue would alter lower extremity biomechanics. Overall, we observed a progressive change in the lower extremity mechanics for knee-flexion and hip-abduction angles and for internal hip-adduction moment. The changes observed for these variables have been reported to increase the risk of injury particularly at initial contact, with decreased knee-flexion angle noted to result in augmented shear force on the ACL.12,17,18,33
Unexpectedly, an interesting pattern was observed for hip flexion at initial contact and peak stance and knee flexion at peak stance. These dependent measures had a subtle altered pattern from prefatigue to 50% fatigue followed by a sudden change at 100% fatigue. Whereas the altered biomechanical patterns is in accordance with previous descriptions2,9,19,21 of the effects of fatigue on lower extremity biomechanics, the nonprogressive changes at 50% fatigue are novel findings of this study.
Investigators have used different fatigue strategies, such as isolated muscle fatigue,34 and prefatigue–postfatigue protocols9,19,21 to evaluate the effect of fatigue on lower extremity biomechanics. Whereas other researchers1,2 have used a similar approach to ours, they included fewer multiple athletic activities that could elicit different muscle groups and mimic actual sport situations, instead focusing on controlled movements, such as squats, vertical forward jumps, or vertical jumps.1,2,6,9,19 By including a multitude of activities that elicited different muscle groups, we expected to have a more accurate representation of what may happen during sport participation (eg, soccer, basketball). Quammen et al26 used a prefatigue–postfatigue assessment, and whereas they gained a better understanding of 2 distinct fatigue protocols, they observed a weakening of the effects of fatigue between preassessment and postassessment. For this study, we adopted a volitional strategy for our protocol to determine when participants would have achieved their maximal fatigue as previously reported.2,6
We noted that the demands placed upon the lower limb have been shown to be task dependent.23 Hence, comparing our results of fatigue using a sidestep task with the results of other researchers who used distinctly different tasks could yield contradictory findings. Our results were partially analogous to those reported by researchers21 investigating a sidestep task. Specifically, we saw a progressive degradation of lower extremity mechanics throughout the protocol. These variables included knee flexion, knee-adduction moment, hip-adduction moment, hip abduction at initial contact, and hip-adduction moment at peak stance. Our findings are similar to those reported in previous work and add to the concept of detrimental effects of fatigue on biomechanics during high-demand activities.2
On secondary analyses, additional variables presented yet another pattern worth noting. As our participants progressed from prefatigue to 50% fatigue, they adopted a posture during hip flexion at initial and peak stance and knee flexion at peak stance that may better protect the knee structures. Essentially, as they progressed toward fatigue, the participants went into a more-flexed position, which may place an increased tensile load on the ACL rather than a shear force.33 The adoption of this posture at 50% fatigue that may place lower loads on the ACL contradicts most fatigue studies in which researchers have shown a continuous decline as fatigue progresses.1,2,9,19 A plausible explanation for this observation is that our protocol used activities commonly performed during practices and games, which might have provided an initial central and muscular adaptation to the fatigue protocol, as typically occurs during practices and games. Although we cannot discern differences between these 2 mechanisms of fatigue, we believe that the observed changes probably are due to degradation of both central and muscular fatigue. Still, as the protocol progressively solicited the neuromechanical demands, we observed a natural deterioration in lower extremity mechanics.
These altered joint mechanics typically are characterized by decreased hip and knee flexion and knee-adduction moment and by increased knee-abduction and internal rotation.8,14,17,18,35–38 In our study, this pattern was attained at the moment of volitional exhaustion (ie, 100% fatigue) for knee- and hip-flexion angles but was not attained for all the dependent measures. Nevertheless, the decline in the biomechanical variables might not have reached the position that is believed to create excessive ACL strain and potentially cause its rupture.35,39 Although presented as showing a difference between prefatigue and 100% fatigue, the knee-abduction and knee-adduction moments do not seem to be sufficient to increasingly strain and potentially rupture the ACL.35,39
An extended position at landing, which was demonstrated by the decreased hip and knee flexion, has been associated with increased risk of ACL injury.12,14,17,18,40 Throughout the fatigue protocol, our participants always presented decreased knee flexion specifically at initial contact, which has been associated with higher anterior tibial shear force.36,37 This augmented force increases the load on the ACL and thus the probability of rupture. In a cadaveric study,36,37,41 investigators noted that anterior tibial displacement is augmented between 15° and 45° of knee flexion, with its peak occurring at 30°. Perhaps the hamstrings muscles cannot cocontract at smaller angles to minimize anterior displacement of the tibia.39 Throughout the fatigue protocol, our participants were within the range that is thought to increase anterior tibial displacement and consequently place greater stress on the ACL. In our study, the change from prefatigue to postfatigue was smaller than in previous studies,9 probably because of the earlier noted difference in the tasks performed. Different tasks may produce different outcomes based on the neuromuscular solicitations specific to each task.42 The participants' backgrounds also may have contributed to this difference. As highly trained NCAA Division I athletes, our participants may experience similar loads during practices and games, whereas participants in the other study were recreational athletes who might not be able to adapt appropriately to such neuromechanical and physiologic demands.
CONCLUSIONS
Distinct patterns exist in the biomechanical variables during fatigue. Some biomechanical variables had a protective adaptation between prefatigue and 50% fatigue and then showed a sudden deterioration from 50% to 100% fatigue. A few variables presented a progressive decline in performance from prefatigue to 100% fatigue. Highly trained NCAA Division I collegiate athletes appear to be able to sustain certain neuromechanical adaptations within the first 50% of a fatigue protocol. This information may be useful in developing future ACL injury-prevention programs. Reinforcement of proper mechanics needs to occur from the early stages and throughout the practice. This reinforcement exemplifies the training specificity principle that the desired mechanics learned during training will transfer to game situations and optimal performance.42 Therefore, developers of ACL injury-prevention programs should consider the effect of fatigue throughout practices and games rather than primarily during warm-ups. This recommendation applies to highly trained individuals in whom the detrimental effects of fatigue seem to be steadily present between 50% and 100% fatigue.
ACKNOWLEDGMENTS
This study was supported by grant SFRH/BD/28046/2006 from the Portuguese Foundation for Science and Technology and grant 1R03AR054031-01 from the National Institutes of Health.
REFERENCES
- 1.Borotikar BS, Newcomer R, Koppes R, McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clin Biomech (Bristol, Avon) 2008;23(1):81–92. doi: 10.1016/j.clinbiomech.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 2.McLean SG, Samorezov JE. Fatigue-induced ACL injury risk stems from a degradation in central control. Med Sci Sports Exerc. 2009;41(8):1661–1672. doi: 10.1249/MSS.0b013e31819ca07b. [DOI] [PubMed] [Google Scholar]
- 3.Giza E, Mithofer K, Farrell L, Zarins B, Gill T. Injuries in women's professional soccer. Br J Sports Med. 2005;39(4):212–216. doi: 10.1136/bjsm.2004.011973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35(1):43–47. doi: 10.1136/bjsm.35.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Gall F, Carling C, Reilly T. Injuries in young elite female soccer players: an 8-season prospective study. Am J Sports Med. 2008;36(2):276–284. doi: 10.1177/0363546507307866. [DOI] [PubMed] [Google Scholar]
- 6.McLean SG, Felin RE, Suedekum N, Calabrese G, Passerallo A, Joy S. Impact of fatigue on gender-based high-risk landing strategies. Med Sci Sports Exerc. 2007;39(3):502–514. doi: 10.1249/mss.0b013e3180d47f0. [DOI] [PubMed] [Google Scholar]
- 7.Chappell JD, Limpisvasti O. Effect of a neuromuscular training program on the kinetics and kinematics of jumping tasks. Am J Sports Med. 2008;36(6):1081–1086. doi: 10.1177/0363546508314425. [DOI] [PubMed] [Google Scholar]
- 8.Hewett TE, Myer G, Gregory D et al. Neuromuscular control and valgus loading of the knee predict ACL injury risk in female athletes. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 9.Chappell JD, Herman DC, Knight BS, Kirkendall DT, Garrett WE, Yu B. Effect of fatigue on knee kinetics and kinematics in stop-jump tasks. Am J Sports Med. 2005;33(7):1022–1029. doi: 10.1177/0363546504273047. [DOI] [PubMed] [Google Scholar]
- 10.Griffin LY, Albohm MJ, Arendt EA et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 11.Shultz SJ, Schmitz RJ, Nguyen AD et al. ACL Research Retreat V: an update on ACL injury risk and prevention, March 25–27, 2010, Greensboro, NC. J Athl Train. 2010;45(5):499–508. doi: 10.4085/1062-6050-45.5.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 13.Boden BP, Breit I, Sheehan FT. Tibiofemoral alignment: contributing factors to noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2009;91(10):2381–2389. doi: 10.2106/JBJS.H.01721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 16.Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41((suppl 1)):i47–i51. doi: 10.1136/bjsm.2007.037192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koga H, Nakamae A, Shima Y et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218–2225. doi: 10.1177/0363546510373570. [DOI] [PubMed] [Google Scholar]
- 18.Krosshaug T, Nakamae A, Boden BP et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 19.Kernozek TW, Torry MR, Iwasaki M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am J Sports Med. 2008;36(3):554–565. doi: 10.1177/0363546507308934. [DOI] [PubMed] [Google Scholar]
- 20.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Neuromuscular and lower limb biomechanical differences exist between male and female elite adolescent soccer players during an unanticipated side-cut maneuver. Am J Sports Med. 2007;35(11):1888–1900. doi: 10.1177/0363546507300823. [DOI] [PubMed] [Google Scholar]
- 21.Sanna G, O'Connor KM. Fatigue-related changes in stance leg mechanics during sidestep cutting maneuvers. Clin Biomech (Bristol, Avon) 2008;23(7):946–954. doi: 10.1016/j.clinbiomech.2008.03.065. [DOI] [PubMed] [Google Scholar]
- 22.Cortes N, Blount E, Ringleb S, Onate J. Soccer-specific video simulation for improving movement assessment. Sports Biomech. 2011;10(1):22–34. doi: 10.1080/14763141.2010.547591. [DOI] [PubMed] [Google Scholar]
- 23.Cortes N, Onate J, Van Lunen B. Pivot task increases knee frontal plane loading compared with sidestep and drop-jump. J Sports Sci. 2011;29(1):83–92. doi: 10.1080/02640414.2010.523087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones MT, Matthews TD, Murray M, Van Raalte J, Jensen BE. Psychological correlates of performance in female athletes during a 12-week off-season strength and conditioning program. J Strength Cond Res. 2010;24(3):619–628. doi: 10.1519/JSC.0b013e3181cc23c3. [DOI] [PubMed] [Google Scholar]
- 25.Gellish RL, Goslin BR, Olson RE, McDonald A, Russi GD, Moudgil VK. Longitudinal modeling of the relationship between age and maximal heart rate. Med Sci Sports Exerc. 2007;39(5):822–829. doi: 10.1097/mss.0b013e31803349c6. [DOI] [PubMed] [Google Scholar]
- 26.Quammen D, Cortes N, Van Lunen BL, Lucci S, Ringleb SI, Onate J. Two different fatigue protocols and lower extremity motion patterns during a stop-jump task. J Athl Train. 2012;47(1):32–41. doi: 10.4085/1062-6050-47.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Begon M, Monnet T, Lacouture P. Effects of movement for estimating the hip joint centre. Gait Posture. 2007;25(3):353–359. doi: 10.1016/j.gaitpost.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz MH, Rozumalski A. A new method for estimating joint parameters from motion data. J Biomech. 2005;38(1):107–116. doi: 10.1016/j.jbiomech.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Lu TW, O'Connor JJ. Bone position estimation from skin marker co-ordinates using global optimisation with joint constraints. J Biomech. 1999;32(2):129–134. doi: 10.1016/s0021-9290(98)00158-4. [DOI] [PubMed] [Google Scholar]
- 30.Yu B, Gabriel D, Noble L, An K-N. Estimate of the optimum cutoff frequency for the Butterworth low-pass digital filter. J Appl Biomech. 1999;15(3):318–329. [Google Scholar]
- 31.Dempster WT. Wright Air Development Center. Wright Air Development Center Technical Report 55–159. Wright-Patterson Air Force Base, OH: 1955. Space Requirements of the Seated Operator: Geometrical, Kinematic, and Mechanical Aspects of the Body, With Special Reference to the Limbs. [Google Scholar]
- 32.Winter DA. Biomechanics and Motor Control of Human Movement. 3rd ed. Hoboken, NJ: John Wiley & Sons Inc;; 2005. pp. 75–102. [Google Scholar]
- 33.Blackburn JT, Padua DA. Influence of trunk flexion on hip and knee joint kinematics during a controlled drop landing. Clin Biomech (Bristol, Avon) 2008;23(3):313–319. doi: 10.1016/j.clinbiomech.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 34.Nyland JA, Shapiro R, Caborn DN, Nitz AJ, Malone TR. The effect of quadriceps femoris, hamstring, and placebo eccentric fatigue on knee and ankle dynamics during crossover cutting. J Orthop Sports Phys Ther. 1997;25(3):171–184. doi: 10.2519/jospt.1997.25.3.171. [DOI] [PubMed] [Google Scholar]
- 35.Cerulli G, Benoit DL, Lamontagne M, Caraffa A, Liti A. In vivo anterior cruciate ligament strain behaviour during a rapid deceleration movement: case report. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):307–311. doi: 10.1007/s00167-003-0403-6. [DOI] [PubMed] [Google Scholar]
- 36.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 37.Markolf KL, Gorek JF, Kabo JM, Shapiro MS. Direct measurement of resultant forces in the anterior cruciate ligament: an in vitro study performed with a new experimental technique. J Bone Joint Surg Am. 1990;72(4):557–567. [PubMed] [Google Scholar]
- 38.Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520–527. doi: 10.5435/00124635-201009000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pandy MG, Shelburne KB. Dependence of cruciate-ligament loading on muscle forces and external load. J Biomech. 1997;30(10):1015–1024. doi: 10.1016/s0021-9290(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 40.Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop-jump task. Clin Biomech (Bristol, Avon) 2006;21(3):297–305. doi: 10.1016/j.clinbiomech.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Hirokawa S, Solomonow M, Lu Y, Lou ZP, D'Ambrosia R. Anterior-posterior and rotational displacement of the tibia elicited by quadriceps contraction. Am J Sports Med. 1992;20(3):299–306. doi: 10.1177/036354659202000311. [DOI] [PubMed] [Google Scholar]
- 42.Magill RA. Knowledge is more than we can talk about: implicit learning in motor skill acquisition. Res Q Exerc Sport. 1998;69(2):104–110. doi: 10.1080/02701367.1998.10607676. [DOI] [PubMed] [Google Scholar]