Abstract
Context:
Therapeutic exercise programs that incorporate real-time feedback have been reported to enhance outcomes in patients with lower extremity joint injuries. The Wii Fit has been purported to improve balance, strength, flexibility, and fitness.
Objective:
To determine the effects of Wii Fit rehabilitation on postural control and self-reported function in patients with a history of lower limb injury.
Design:
Single-blinded, randomized controlled trial.
Setting:
Laboratory.
Patients or Other Participants:
Twenty-eight physically active participants with a history of lower limb injuries were randomly assigned to 1 of 3 groups (9 Wii Fit, 10 traditional, 9 control).
Intervention(s):
Intervention groups performed supervised rehabilitation 3 d/wk for a total of 12 sessions.
Main Outcome Measure(s):
Time to boundary (TTB) and the Star Excursion Balance Test (SEBT) were conducted at baseline, 2 weeks, and 4 weeks. Self-reported function was measured at baseline and 4-week follow-up. Between-groups differences were compared using repeated-measures multivariate analysis of variance.
Results:
With the eyes open, both intervention groups improved (P < .05) in the mean and the SD of the TTB anterior-posterior minima. In the eyes-closed condition, a time main effect (P < .05) for absolute TTB medial-lateral minima was observed. A time main effect was also noted in the posteromedial and posterolateral reach directions of the SEBT. When the scores for each group were pooled, improvement (P < .05) in self-reported function was demonstrated at 4-week follow-up.
Conclusions:
Rehabilitation using the Wii Fit and traditional exercises improved static postural control in patients with a history of lower extremity injury.
Key Words: balance, rehabilitation, time to boundary, virtual reality
Key Points.
Visual feedback during rehabilitation can improve static postural control in patients with a lower extremity injury.
The Wii Fit can be used in conjunction with traditional rehabilitation to heighten the patient's interest level and self-reported function.
Balance is essential for performance in both daily and athletic activities and is often compromised after an injury.1 Preprogrammed reactions, nerve conduction velocity, joint range of motion, and muscle strength all contribute to balance when attempting to maintain a specific state of posture while standing, sitting, and changing positions.2,3 Additionally, these mechanisms play important roles in sequencing movements4 and reacting to external disturbances such as a push or fall.5 Static balance is defined as the ability to hold a still posture while maintaining balance over a stable base, whereas dynamic balance is defined as an individual's ability to maintain balance while leaning or reaching in different directions.4,6
The recent literature discusses improving neuromuscular control and activation and strengthening of the musculature in the entire lower extremity in order to improve postural stability through balance rehabilitation.5,7 It has been well established that rehabilitation programs focused on improving neuromuscular control, strength, and range of motion improve postural control and self-reported function in patients with chronic ankle instability (CAI),8–10 acute ankle sprains,11 and patellofemoral pain.12,13 Although traditional therapeutic exercises have been effective in improving postural control after injury, a variety of treatment approaches can be used to improve balance after joint injury.14
Clinicians are beginning to introduce gaming consoles, computer vision technology, and virtual reality into rehabilitation protocols.5,15–18 The Wii Fit (Nintendo of America, Inc, Redmond, VA) is a relatively low-cost virtual reality–based product released by Nintendo. The Wii Fit has been purported to improve balance, strength, fitness, and weight loss.14 During participation, real-time feedback on control and accuracy is provided for most of the activities and overall competency is provided after the completion of the task or game. After 10 weeks of exergaming with the Wii Fit, improvements in unilateral balance and lower limb strength have been reported in healthy individuals.14 Greater improvements in balance have also been reported in patients using the Wii Fit when compared with patients performing a traditional balance rehabilitation protocol.19 Currently, there is a dearth of controlled clinical trials including injured adults that demonstrate the benefits of using Wii Fit during rehabilitation to improve postural control.
Therefore, the purpose of this study was to compare the effects of a 4-week supervised intervention using traditional and Wii Fit protocols on static and dynamic postural control and self-reported function in individuals with a history of lower limb injury. Our hypothesis was that after a 4-week intervention, individuals in the Wii Fit group would demonstrate greater improvements in postural control as assessed with static and dynamic measures than individuals in the control and traditional exercise groups at 1-, 2-, and 4-week follow-ups.
METHODS
Participants
A convenience sample of 28 participants (12 men, 16 women) between the ages of 18 and 25 years were randomized into 3 groups: Wii Fit, traditional balance, or control (Table 1). Participants (age = 21.6 ± 2.4 years, height = 173.1 ± 9.0 cm, weight = 73.3 ± 10.4 kg) were recruited from within the university. Participants were included in the study if they had a self-reported history of a lower limb joint injury or surgery, including ligamentous, capsular, or cartilaginous damage to the ankle or knee, within the past year. Participants had to have been cleared for full sports participation by their attending physician. Exclusion criteria were a lower limb injury within the past 6 weeks, participation in a lower limb rehabilitation program at the time of the study, concussion within the last 6 months, self-reported balance disorders, neuropathies, diabetes, or other conditions known to adversely affect balance or gait. All participants were functioning at a high level and were recreationally active. Before testing, all participants read and signed an informed consent form approved by the university's institutional review board.
Table 1.
Participant Demographics
| Group |
No. |
Mean ± SD |
Injured Limb, No. |
|||
| Age, y |
Height, cm |
Weight, kg |
Ankle |
Knee |
||
| Wii Fit | 9 | 21.3 ± 3.5 | 174.3 ± 11.1 | 73.3 ± 13.36 | 3 | 6 |
| Traditional | 10 | 21.7 ± 2.0 | 170.8 ± 9.1 | 73.5 ± 8.6 | 6 | 4 |
| Control | 9 | 21.8 ± 1.7 | 174.4 ± 7.0 | 73.0 ± 10.0 | 5 | 4 |
Study Design
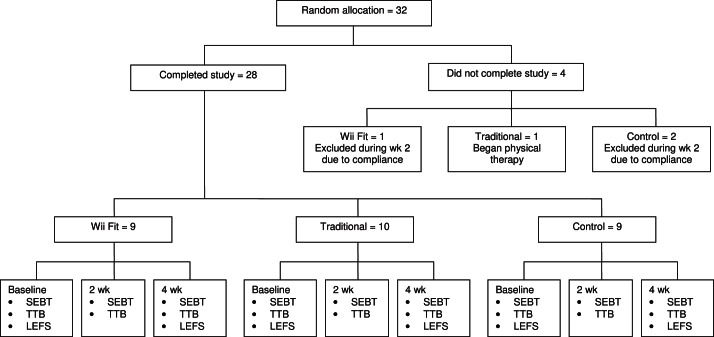
The study was a single-blinded randomized controlled trial (Figure 1). Participants were randomly assigned using a sealed envelope to one of the following intervention groups: Wii Fit group, traditional balance group, or control group. The Wii Fit and traditional balance groups underwent 12 supervised rehabilitation sessions during a 4-week period. The participants remained in the same allocation throughout the study. A computer-generated randomization list was compiled by one of the investigators and given to the clinician responsible for delivering the intervention. An independent assessor was blinded to group assignment and took measurements of static and dynamic postural control at baseline, 2 weeks, and 4 weeks. Measures of self-reported function were recorded at baseline and 4 weeks. All outcome measures were taken on the limb with a history of lower extremity injury.
Figure.
Flow diagram of participants throughout the study. Abbreviations: SEBT, Star Excursion Balance Test in the anterior, posteromedial, and posterolateral directions; TTB, time-to-boundary measures in the eyes-open and eyes-closed positions; and LEFS, Lower Extremity Functional Scale.
Time to Boundary.
Participants completed balance testing using a force plate (model Accusway Plus; Advanced Mechanical Technology, Inc, Watertown, MA). The participants performed 3 trials of single-limb stance on the affected leg with their eyes open and then closed for 15 seconds each. Following a protocol from Hertel and Olmsted-Kramer,20 the stance foot was placed in the same position on the force plate for each individual trial. During the initial study visit, the foot width and length were measured to ensure accuracy of foot placement for each static balance trial. Participants were instructed to stand in the middle of the force plate, and the examiner measured and marked the location to ensure accuracy and reproducibility. Before the test began, the participants were instructed to begin the test with their hands across their chest and to hold the opposite limb in knee flexion.21 If the participant touched down with the opposite limb, made contact with the stance limb, or was unable to maintain standing posture during the 15-second trial, the trial was terminated and repeated.
Star Excursion Balance Test.
The Star Excursion Balance Test (SEBT) was used to measure dynamic balance. Each participant stood on a 3-point grid made of athletic tape, as described by Hertel et al.22 Participants maintained a single-limb stance with hands on hips while reaching as far as possible along the graduated line of direction with their opposite limb, lightly touched the line, and returned to starting position.22 The reach distances were measured in the anterior, posteromedial (PM), and posterolateral (PL) directions.22
Trials were excluded and rerun if the participant loaded excessive weight on the reaching limb, removed the stance foot from the center of the grid, touched down for an extended period of time, or lost balance completely.23 Three practice trials were permitted to minimize learning effect.23 Participants were then allowed a 5-minute rest period22 and completed 3 measured trials on the affected limb in each reach direction. Reach distances were normalized to the participant's leg length.23 Dynamic balance measures were taken with the affected limb as the stance leg; the mean of 3 trials for each direction was used for data analysis.
Self-Reported Function.
Self-reported function was measured using the Lower Extremity Functional Scale (LEFS).24 The LEFS was administered at baseline and at 4 weeks to capture changes in self-reported function. The reliability and minimally clinically important differences for the LEFS have been reported to be 0.94 and 9 points, respectively.24 The LEFS has 20 items, with each item being scored from 0 (extreme difficulty or unable to perform activity) to 4 (no difficulty), with a total point value of 80 points.24 Therefore, higher scores on the LEFS indicate better self-reported function.
Interventions
Participants randomly assigned to the 4-week Wii Fit group or traditional balance group participated in 12 supervised rehabilitation sessions, 3 sessions per week. Each rehabilitation session for both groups lasted approximately 15 minutes and focused on balance exercises. Rehabilitation for the Wii Fit and traditional balance groups was overseen and directed by a certified athletic trainer. Participants in the intervention groups were required to complete all 12 rehabilitation sessions; 3 participants were not able to attend all sessions and therefore were dropped from the study for noncompliance (Figure).
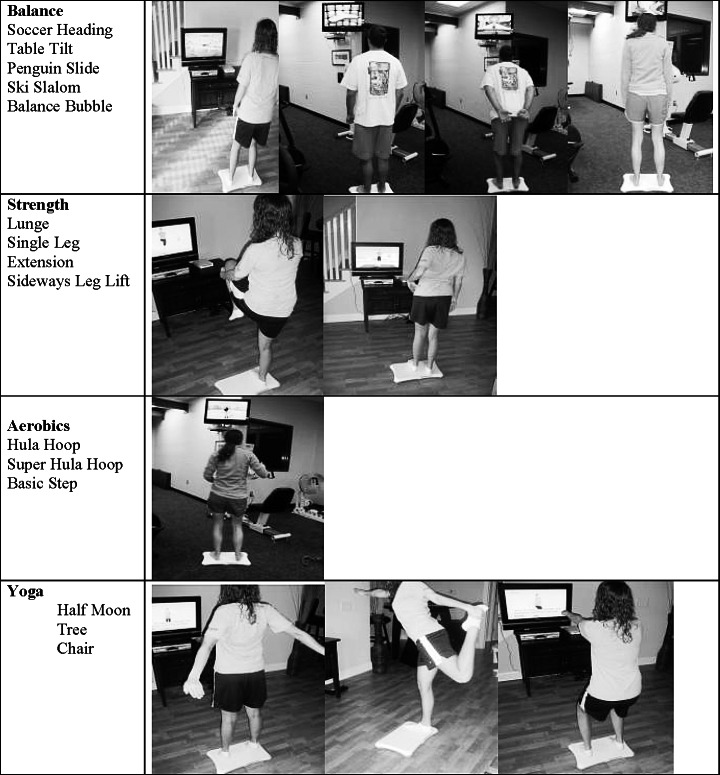
Wii Fit Group.
The 9 participants in the Wii Fit group began their first testing session by creating a “Mii” character and taking anthropometric measurements. The Wii Fit protocol consisted of strength, yoga, and aerobic programs that were performed on the Wii Fit balance board. Advancement in exercises and repetition increases were determined by the participant's performance on each Wii Fit program. The games were chosen to mimic weight shifting, double- to single-legged stance, and moving over the base of support. A certified athletic trainer who was responsible for overseeing the interventions was also responsible for demonstrating and making decisions on participant progressions (see Appendix A for exercises).
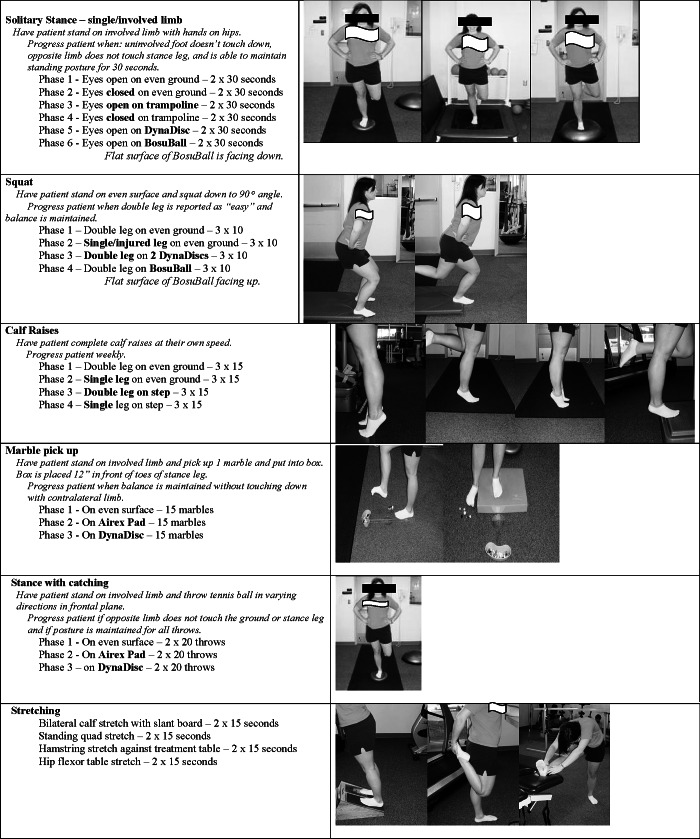
Traditional Balance Exercise Group.
The 10 individuals in the traditional balance exercise group completed a rehabilitation protocol derived from studies by Holme et al25 and Hale et al.8 The rehabilitation protocol consisted of progressions of the following exercises: single-limb stance, double- and single-limb squat, double- and single-limb calf raises, single-limb marble pick-up, single-limb stance with ball throwing, and lower extremity stretching. Progression was based on criteria set by the examiner to adjust the intensity of the program by varying surface type and eliminating visual stimuli; sets and repetitions remained the same throughout the entire 4 weeks of rehabilitation. The varying surface types included even ground and uneven ground, which were manipulated using various rehabilitation devices (see Appendix B for exercises). Exercise progression was based on an athletic trainer's assessment of success at each level. For example, the examiner tested whether the participant could stand in unilateral stance for 30 seconds. If that was achieved, then the participant was asked to perform the same task with his or her eyes closed. The progression included the use of rehabilitation equipment, such as a Bosu Ball (Power Systems, Inc, Nashville, TN) or Dyna Disc (Exertools, Petaluma, CA), to make the surface unstable and further challenge the participant. Every effort was made to keep the program consistent among participants but challenging to the individual at each exercise level.
Control Group.
The 9 individuals randomly assigned to the control group were instructed to continue normal activities of daily living. Each member of the control group recorded daily physical activities and was asked to not participate in any sort of balance rehabilitation training program. Only the control group completed a daily journal, which included descriptions of their cardiovascular and strength exercises, to ensure that they did not alter their activities of daily living.
Data Processing
All force-plate measurements were processed using a custom software program in MATLAB (The MathWorks, Inc, Natick, MA). Translational forces (Fx, Fy, Fz) and moments of force (Mx, My, Mz) were recorded at 50 Hz, and a time series of 750 center-of-pressure (COP) data points was calculated for each trial. Center-of-pressure data were filtered with a fourth-order, zero-lag, low-pass filter with a cutoff frequency of 5 Hz.
Time-to-boundary (TTB) measures have been described in detail in previous research reports.20,26 Briefly, TTB measures estimate the time it would take for the COP to reach the boundary of the base of support if the COP were to continue on its trajectory at its instantaneous velocity. A typical TTB series shows a sequence of peaks and valleys, with each valley, or minimum, representing a period of potential postural instability. The minima across each trial were sampled and the absolute minimum, mean of the minima, and SD of the minima were calculated as dependent variables. For each of these measures, higher values represented greater postural stability and lower measures indicated postural instability.
The percentage of COP range was calculated by dividing the COP range by the width or length of the foot in the mediolateral (ML) and anteroposterior (AP) directions, respectively. Postural-control measures that served as dependent variables were the percentage range, absolute minimum, mean of minima, and standard deviation of minima in the ML and AP directions. For each of these measures of postural control, higher measures represented greater postural stability and lower measures indicated postural instability.27,28
Statistical Analysis
We performed four 3 × 3 (group × time) mixed-model repeated-measures multivariate analyses of variance (MANOVAs) to assess changes in TTB in the eyes-open AP and ML directions and eyes-closed AP and ML directions, respectively. Three 3 × 3 (group × time) mixed-model repeated-measures analyses of variance (ANOVAs) were used to assess changes in excursion during the SEBT. To assess changes in the LEFS scores for self-reported function due to rehabilitation, we used a 3 × 2 (group × time) mixed-model repeated-measures ANOVA. In the event of a significant MANOVA, the individual ANOVAs were assessed for each dependent variable included. In the event of a significant interaction or main effect in an ANOVA, a Tukey post hoc test was used to identify specific significant differences among groups at each follow-up period. Before analysis, each dependent variable was assessed to assure normality of distribution using a Levene test. The α level was set a priori at P ≤ .05 for all analyses. All statistical comparisons were performed with SPSS (version 17.0; SPSS, Inc, Chicago, IL). Cohen d measures of effect size were determined by calculating the mean difference within groups (baseline, week 2, week 4) and dividing it by the reference SD (baseline). The strength of the effect size was determined as small (≤0.4), moderate (0.41–0.7), or large (≥0.71).
RESULTS
Time to Boundary
Eyes Open, Anterior to Posterior Direction.
When patients balanced with their eyes open, a group-by-time interaction was noted (Wilks λ = 0.289; df = 16, 36; P = .050), however, no time (Wilks λ = 0.52; df = 8, 18; P = .09) or group (Wilks λ = 0.63; df = 8, 44; P = .22) main effect was observed. During post hoc analysis, we found that participants in the Wii Fit and traditional rehabilitation groups had greater improvements in TTB during the eyes-open tasks when TTB was being assessed in the AP direction. These improvements were demonstrated for the mean of the TTB anterior-posterior (TTBAP) minima (F4,50 = 3.4, P = .015) (Table 2) and the SD of TTBAP minima (F4,50 = 2.7, P = .039) (Table 2). During the 4-week intervention, the Wii Fit group improved at each follow-up period, whereas the traditional group initially improved from baseline to 2 weeks but regressed toward baseline values at 4-week follow-up (Table 2).
Table 2.
Time-to-Boundary Measures of Postural Control for the Eyes-Open Condition (Mean ± SD)
| Direction |
Wii Fit |
Traditional |
Control |
||||||
| Baseline |
2 wk |
4 wk |
Baseline |
2 wk |
4 wk |
Baseline |
2 wk |
4 wk |
|
| Anteroposterior | |||||||||
| Absolute minimum TTBAP, s | 3.21 ± 0.66 | 4.01 ± 0.64 | 3.91 ± 0.61 | 3.26 ± 0.97 | 3.64 ± 1.37 | 3.25 ± 1.49 | 3.26 ± 0.83 | 3.68 ± 1.01 | 3.30 ± 0.76 |
| Mean minimum TTBAP, s | 11.70 ± 3.44 | 14.24 ± 1.92a | 16.72 ± 3.44b | 10.77 ± 3.59 | 12.89 ± 6.44a | 11.16 ± 5.31 | 13.69 ± 4.25 | 12.99 ± 2.34 | 12.44 ± 2.70 |
| SD minimum TTBAP, s | 7.43 ± 2.53 | 8.75 ± 1.00a | 11.63 ± 5.11b | 6.73 ± 2.78 | 8.15 ± 5.32a | 6.63 ± 3.34 | 8.41 ± 2.33 | 8.47 ± 1.66 | 7.97 ± 2.52 |
| Range COPAP, % | 5.45 ± 0.67 | 5.50 ± 0.77 | 4.76 ± 1.16 | 5.15 ± 0.98 | 5.44 ± 1.43 | 7.74 ± 8.69 | 5.87 ± 1.89 | 5.40 ± 1.08 | 5.83 ± 0.80 |
| Mediolateral | |||||||||
| Absolute minimum TTBML, s | 0.99 ± 0.24 | 0.91 ± 0.44 | 1.27 ± 0.33 | 0.87 ± 0.45 | 0.93 ± 0.40 | 1.05 ± 0.48 | 0.91 ± 0.60 | 0.95 ± 0.51 | 1.07 ± 0.49 |
| Mean minimum TTBML, s | 3.77 ± 0.74 | 3.72 ± 0.98 | 5.42 ± 1.16 | 3.57 ± 1.61 | 3.78 ± 1.46 | 3.98 ± 2.11 | 4.34 ± 1.97 | 4.11 ± 1.42 | 4.64 ± 2.02 |
| SD minimum TTBML, s | 3.24 ± 1.76 | 2.92 ± 0.50 | 4.15 ± 1.21 | 2.85 ± 1.37 | 2.83 ± 1.21 | 3.17 ± 1.94 | 3.87 ± 1.51 | 3.48 ± 1.02 | 4.18 ± 3.12 |
| Range COPML, % | 10.28 ± 0.71 | 11.13 ± 1.63 | 8.46 ± 1.09 | 10.18 ± 2.12 | 10.52 ± 2.61 | 13.48 ± 12.61 | 10.86 ± 2.38 | 10.75 ± 1.92 | 9.87 ± 1.46 |
Abbreviations: COPAP, center of pressure anterior-posterior; COPML, center of pressure medial-lateral; TTBAP, time to boundary anterior-posterior; TTBML, time to boundary medial-lateral.
Improvement in time to boundary from baseline to 2 wk (P > .05).
Improvement in time to boundary from baseline to 4 wk (P > .05).
Eyes Closed, Anterior to Posterior Direction.
In the AP eyes-closed position, no time main effect (Wilks λ = 0.726; df = 8, 18; P = .57), group main effect (Wilks λ = 0.681; df = 8,44; P = .34), or group-by-time interaction (Wilks λ = 0.362; df = 16,36; P = .16) occurred; see Table 3 for means and standard deviations.
Table 3.
Time-to-Boundary Measures of Postural Control for the Eyes-Closed Condition (Mean ± SD)
| Direction |
Wii Fit |
Traditional |
Control |
||||||
| Baseline |
2 wk |
4 wk |
Baseline |
2 wk |
4 wk |
Baseline |
2 wk |
4 wk |
|
| Anteroposterior | |||||||||
| Absolute minimum TTBAP, s | 1.05 ± 0.45 | 1.32 ± 0.28 | 1.62 ± 0.56 | 1.15 ± 0.41 | 1.39 ± 0.62 | 1.42 ± 0.63 | 1.48 ± 0.46 | 1.33 ± 0.35 | 1.25 ± 0.32 |
| Mean minimum TTBAP, s | 4.42 ± 1.42 | 5.17 ± 0.70 | 5.91 ± 1.93 | 4.49 ± 1.91 | 5.20 ± 2.41 | 4.54 ± 1.71 | 5.34 ± 1.27 | 5.00 ± 1.05 | 5.16 ± 1.25 |
| SD minimum TTBAP, s | 2.80 ± 0.95 | 3.08 ± 0.47 | 3.77 ± 1.28 | 3.13 ± 1.77 | 3.48 ± 2.10 | 2.66 ± 0.94 | 3.26 ± 0.94 | 3.39 ± 1.07 | 3.41 ± 1.22 |
| Range COPAP, % | 11.98 ± 2.11 | 9.84 ± 2.48 | 9.40 ± 2.48 | 11.93 ± 3.24 | 10.37 ± 3.67 | 13.13 ± 11.64 | 10.54 ± 2.02 | 10.57 ± 2.59 | 11.11 ± 1.96 |
| Mediolateral | |||||||||
| Absolute minimum TTBML, s | 0.47 ± 0.08 | 0.38 ± 0.18 | 0.54 ± 0.11a | 0.40 ± 0.21 | 0.41 ± 0.20 | 0.48 ± 0.19a | 0.35 ± 0.20 | 0.39 ± 0.20 | 0.47 ± 0.20a |
| Mean minimum TTBML, s | 1.75 ± 0.29 | 1.62 ± 0.42 | 1.96 ± 0.41 | 1.62 ± 0.55 | 1.74 ± 0.55 | 1.72 ± 0.59 | 1.64 ± 0.64 | 1.92 ± 0.55 | 1.86 ± 0.75 |
| SD minimum TTBML, s | 1.49 ± 0.54 | 1.47 ± 0.23 | 1.62 ± 0.49 | 1.34 ± 0.39 | 1.50 ± 0.53 | 1.48 ± 0.59 | 1.55 ± 0.65 | 1.90 ± 0.59 | 1.70 ± 0.71 |
| Range COPML, % | 17.19 ± 2.20 | 16.97 ± 2.11 | 16.68 ± 2.35 | 19.25 ± 5.28 | 18.56 ± 3.46 | 22.02 ± 15.45 | 18.46 ± 2.63 | 17.57 ± 2.12 | 18.08 ± 2.63 |
Abbreviations: COPAP, center of pressure anterior-posterior; COPML, center of pressure medial-lateral; TTBAP, time to boundary anterior-posterior; TTBML, time to boundary medial-lateral.
Improvements in time to boundary from 2 wk to 4 wk for the Wii Fit, traditional rehabilitation, and control groups (P > .05).
Eyes Open, Medial to Lateral Direction.
In the eyes-open ML direction, no time main effect (Wilks λ = 0.624; df = 8, 18; P = .28), group main effect (Wilks λ = 0.814; df = 8, 44; P = .77), or group-by-time interaction (Wilks λ = 0.388; df = 16, 36; P = .22) was observed.
Eyes Closed, Medial to Lateral Direction.
In the ML eyes-closed condition, no group main effect (Wilks λ = 0.605; df = 8, 44; P = .16) or group-by-time interaction (Wilks λ = 0.632; df = 16, 36; P = .87) were seen; however, a time main effect (Wilks λ = 0.400; df = 8, 18; P = .02) was noted. When the scores from all groups were pooled, an improvement in the absolute minimum TTBML (F2,50 = 3.7, P = .031) from baseline to 4 weeks and from 2 weeks to 4 weeks was found for the 3 intervention groups (Table 3).
Star Excursion Balance Test
After 4 weeks of rehabilitation, all groups experienced an increase in reach distance in the PL (F2,50 = 8.7, P = .001) and PM (F2,50 = 15.3, P < .001) directions from baseline to 2 weeks and baseline to 4 weeks. No group main effect or group-by-time interactions were demonstrated for the SEBT; however, a time main effect for the SEBT in the PL and PM directions (Table 4) was observed. No significant findings were noted from 2 weeks to 4 weeks in any direction. No group (Wii Fit, traditional, or control) improved in the anterior reach direction over time.
Table 4.
Star Excursion Balance Test Condition (Mean ± SD)
| Reach Direction |
Wii Fit |
Traditional |
Control |
P Value |
||||||||
| Baseline |
2 wk |
4 wk |
Baseline |
2 wk |
4 wk |
Baseline |
2 wk |
4 wk |
Time |
Group |
Time by Group |
|
| ANT | 59.5 ± 6.8 | 59.4 ± 6.9 | 59.4 ± 6.3 | 61.9 ± 8.7 | 61.9 ± 8.7 | 64.2 ± 8.0 | 62.5 ± 5.7 | 65.6 ± 7.0 | 64.4 ± 5.7 | .60 | .33 | .32 |
| PM | 81.5 ± 7.9 | 85.2 ± 9.0 | 84.7 ± 10.1 | 84.9 ± 11.1 | 90.7 ± 11.4 | 90.6 ± 7.7 | 84.0 ± 8.2 | 88.7 ± 11.8 | 85.8 ± 12.2 | .001a | .53 | .67 |
| PL | 72.2 ± 9.3 | 80.7 ± 10.2 | 80.9 ± 9.1 | 79.8 ± 15.3 | 87.5 ± 11.8 | 84.1 ± 11.1 | 81.5 ± 8.1 | 83.5 ± 10.5 | 86.9 ± 9.2 | <.001a | .36 | .11 |
Abbreviations: ANT, anterior; PL, posterolateral; PM, posteromedial.
Significant variables at P = .05.
Self-Reported Function
No group main effect (F2,25 = 0.640, P = .54) or group-by-time interaction (F2,25 = 0.968, P = .39) occurred when self-reported function was assessed at 4-week follow-up. However, when scores from the 3 groups were pooled, a main time effect was observed (F1,25 = 8.04, P = .009) indicating a 3-point improvement in the LEFS score from baseline to 4 weeks. Means, standard deviations, and effect sizes for the LEFS are listed in Table 5.
Table 5.
Self-Reported Function Scores on the Lower Extremity Functional Scale (LEFS) (Mean ± SD)
| Group |
LEFS Pretest |
LEFS Posttest |
Effect Size |
| Wii Fit | 72.6 ± 8.9 | 77.7 ± 3.5a | 0.57 (−0.37 to 1.51) |
| Traditional | 69.7 ± 12.2 | 73.2 ± 7.97a | 0.29 (−0.59 to 1.17) |
| Control | 74.2 ± 7.0 | 75.8 ± 5.63a | 0.22 (−0.70 to 1.15) |
Increase in LEFS scores from baseline to 4-wk follow-up when the 3 groups were pooled (P > .05).
DISCUSSION
Improvements observed during static balance with the eyes open in patients with a previous history of lower limb injuries contrasts with the findings of other investigators28 who incorporated organized balance programs and observed changes in TTB in the eyes-closed condition. These conflicting results could reflect the types of exercises incorporated into each of the rehabilitation programs. During our study, exercises were more static in nature, and all but one of the exercises (static balance, eyes closed) required the patients to keep their eyes open during the task. McKeon et al,28 on the other hand, incorporated more dynamic tasks through the course of their rehabilitation program. Time-to-boundary measures improved for the Wii Fit group when compared with the traditional and control groups in the AP direction with the eyes open. These findings might be explained by the use of the Wii Fit and its abundance of eyes-open activities. Dynamically, all groups increased in reach distances in the PL and PM directions. To our knowledge, this is the first study to show significant findings with eyes-open TTB measures after a rehabilitation intervention.
Time to Boundary, Eyes Open
Postural stance is typically measured during a period of quiet standing and often fails to indicate deficiencies, because this task is easy for normally functioning individuals.29 Time-to-boundary calculations were developed from force-plate data to help identify subtle changes in static postural control by examining the rate of change in COP, particularly as the COP changes direction. In the present study, measures of static postural control improved in both intervention groups compared with the control group after 4 weeks of supervised exercise. Changes in TTB have been measured after rehabilitation programs designed for subacute CAI patients with the eyes closed,28 but no researchers thus far have identified an intervention resulting in changes in these measures with the eyes open. Overall, the Wii Fit group had greater improvements in TTB when participants balanced with their eyes open. These findings are similar to those of a study conducted by Nitz et al,14 who also reported greater changes in static postural control and strength in healthy participants involved in a 10-week Wii Fit intervention program compared with a control group.
The mean of the TTB minima is the time it would take for the sensorimotor system to make a postural correction before reaching either the AP or ML boundaries of the foot.26 Increases in the magnitude of this measure would imply that the patient has a greater amount of time to make a postural correction before reaching his or her limits of stability.26 After 4 weeks of balance rehabilitation, the mean of the TTB minima in the AP direction in the eyes-open position increased for the Wii Fit group compared with the traditional and control groups. These findings are supported by the large effect size (1.17) observed for the Wii Fit group compared with the control (−.0.29) and traditional (0.11) rehabilitation groups from baseline at 4-week follow-up. We believe that rehabilitation focused on balance training enhanced the sensorimotor system; in particular, it may have improved afferent feedback from the muscles, ligaments, and tendons surrounding the joint, thus increasing the number of strategies available to control single-limb balance in this group of patients with a lower extremity injury and contributing to the improvement in the mean of the TTB minima in the AP direction when patients in the Wii Fit and traditional rehabilitation groups balanced with their eyes open. Possibly the most clinically relevant potential benefit is the idea that a patient has more time to make a postural correction, affording more time before reaching the limits of stability. If a patient is given more time to make a postural correction, this may reduce the number of injuries sustained. However, future research is needed to determine whether increases in the magnitude of the mean of the TTB correlate with a decrease in injury rate after rehabilitation.
The SD of the TTB minima represents the level of constraints placed on the sensorimotor system.30 A higher SD indicates a less constrained sensorimotor system, and a lower SD indicates a more constrained sensorimotor system. Healthy individuals typically have more degrees of freedom, or a less constrained system, and are capable of using more strategies to maintain stance.28,31 It has also been suggested that an injury to the lower limb may place greater constraints on the sensorimotor system, and consequently, a decreased number of strategies is available to maintain postural control.28 Participants in the Wii Fit and traditional groups experienced increases in the SD of the TTBAP minima compared with the control group over the 4-week intervention, indicating that the sensorimotor system in these individuals was no longer constrained to the same degree. The effect size for the Wii Fit group from baseline to 4 weeks was large and the 95% CI did not cross zero; by comparison, the effect sizes for the traditional and control group were small, with the 95% CI crossing zero (Tables 6 and 7). These findings are consistent with previous research that reported improvements in the SD of TTB in patients with CAI after 4 weeks of balance rehabilitation.28
Table 6.
Within-Group Effect Sizes and 95% Confidence Intervals for Eyes-Open, Static Balance
| Variable |
Wii Fit |
Traditional |
Control |
|||
| Time 1 |
Time 2 |
Time 1 |
Time 2 |
Time 1 |
Time 2 |
|
| Absolute minimum TTBML, s | −0.33 (−1.26 to 0.60) | 1.17 (0.17 to 2.17) | 0.13 (−0.74 to 1.01) | 0.40 (−0.49 to 1.29) | 0.07 (−0.86 to 0.99) | 1.77 (0.68 to 2.86) |
| Absolute minimum TTBAP, s | 1.21 (0.21 to 2.22) | 1.06 (0.07 to 2.05) | 0.39 (−0.49 to 1.28) | −0.01 (−0.89 to 0.87) | 0.51 (−0.43 to 1.44) | 0.05 (−0.88 to 0.97) |
| Mean minimum TTBML, s | −0.07 (−0.99 to 0.86) | 2.23 (1.05 −3.41) | 0.13 (−0.75 to 1.01) | 0.25 (−0.63 to 1.13) | −0.12 (−1.04 to 0.81) | 0.15 (−0.77 to 1.08) |
| Mean minimum TTBAP, s | 0.74 (−0.22 to 1.69) | 1.46 (0.42 to 2.50) | 0.59 (−0.30 to 1.49) | 0.11 (−0.77 to 0.99) | −0.16 (−1.09 to 0.76) | −0.29 (−1.22 to 0.63) |
| SD minimum TTBML, s | −0.18 (−1.11 to 0.74) | 0.52 (−0.42 to 1.46) | −0.01 (−0.89 to 0.86) | 0.23 (−0.65 to 1.11) | −0.26 (−1.19 to 0.67) | −0.21 (−0.72 to 1.13) |
| SD minimum TTBAP, s | 0.52 (−0.42 to 1.46) | 1.66 (0.59 to 2.73) | 0.51 (−0.38 to 1.40) | −0.04 (−0.91 to 0.84) | −0.03 (−0.90 to 0.95) | −0.19 (−1.11 to 0.74) |
| Range COPML, % | 1.20 (0.19 to 2.20) | −2.56 (−3.81 to 1.32) | 0.16 (−0.72 to 1.02) | 1.56 (0.56 to 2.56) | −0.05 (−0.97 to 0.88) | −0.42 (−1.35 to 0.52) |
| Range COPAP, % | 0.07 (−0.85 to 1.00) | −1.03 (−2.01 to 0.05) | 0.20 (−0.68 to 1.08) | 1.81 (0.77 to 2.85) | −0.25 (−1.18 to 0.68) | −0.02 (−0.95 to 0.90) |
Abbreviations: COPAP, center of pressure anterior-posterior; COPML, center of pressure medial-lateral; Time 1, effect size for baseline–week 2; Time 2, effect size for baseline–week 4; TTBAP, time to boundary anterior-posterior; TTBML, time to boundary medial-lateral.
Table 7.
Within-Group Effect Sizes and 95% Confidence Intervals for Eyes-Closed, Static Balance
| Variable |
Wii Fit |
Traditional |
Control |
|||
| Time 1 |
Time 2 |
Time 1 |
Time 2 |
Time 1 |
Time 2 |
|
| Absolute minimum TTBML, s | −1.13 (−2.12 to −0.13) | 0.88 (−0.09 to 1.84) | 0.05 (−0.83 to 0.92) | 0.38 (−0.50 to 1.27) | 0.20 (−0.73 to 1.13) | 0.60 (−0.34 to 1.54) |
| Absolute minimum TTBAP, s | 0.60 (−0.34 to 1.54) | 1.07 (0.25 to 2.28) | 0.59 (−0.31 to 1.48) | 0.66 (−0.24 to 1.56) | −0.33 (−1.26 to 0.60) | −0.50 (−1.44 to 0.44) |
| Mean minimum TTBML, s | −0.45 (−1.38 to 0.49) | 0.72 (−0.23 to 1.68) | 0.22 (−0.66 to 1.11) | 0.18 (−0.70 to 1.06) | 0.44 (−0.50 to 1.37) | 0.34 (−0.59 to 1.27) |
| Mean minimum TTBAP, s | 0.53 (−0.41 to 1.47) | 1.05 (0.06 to 2.03) | 0.37 (−0.51 to 1.26) | 0.03 (−0.85 to 0.90) | −0.27 (−1.20 to 0.66) | −0.14 (−1.07 to 0.78) |
| SD minimum TTBML, s | −0.04 (−0.96 to 0.89) | 0.24 (−0.69 to 1.17) | 0.41 (−0.48 to 1.30) | 0.36 (−0.52 to 1.24) | 0.54 (−0.40 to 1.48) | 0.23 (−0.70 to 1.16) |
| SD minimum TTBAP, s | 0.29 ( −0.63 to 1.22) | 1.02 (0.04 to 2.00) | 0.20 (−0.68 to 1.08) | −0.27 (−1.15 to 0.61) | 0.14 (−0.79 to 1.06) | 0.16 (−0.77 to 1.08) |
| Range COPML, % | 23.22 (15.58 to 30.86) | −0.23 (−1.16 to 0.70) | 3.43 (2.05 to 4.81) | 0.52 (−0.37 to 1.42) | 0.31 (−0.62 to 1.24) | −0.14 (−1.07 to 0.78) |
| Range COPAP, % | 1.54 (0.45 to 2.54) | −1.22 (−2.23 to −0.22) | 0.02 (−0.85 to 0.90) | 0.37 (−0.51 to 1.25) | 0 (−0.92 to 0.92) | −0.18 (−1.10 to 0.75) |
Abbreviations: COPAP, center of pressure anterior-posterior; COPML, center of pressure medial-lateral; Time 1, effect size for baseline–week 2; Time 2, effect size for baseline–week 4; TTBAP, time to boundary anterior-posterior; TTBML, time to boundary medial-lateral.
Time to Boundary, Eyes Closed
The absolute minimum TTB represents the lowest single TTB data point and represents the closest an individual comes in time to losing balance.20 An increase in this measure indicates an improved balance strategy. All 3 groups showed increases in the absolute minimum TTBML, suggesting an increased ability to incorporate strategies to avoid a loss of balance. The increase in the absolute minimum TTBML after 4 weeks of balance rehabilitation demonstrates that whereas participants with a history of lower limb injuries were controlling their balance, they did so in a manner that increased the time available to make a postural correction. Although the absolute minimum TTBML value decreased, it should be noted that the mean of these minima did not. These results suggest that a balance training program wherein environmental constraints can be manipulated might be successful at overcoming the constraints that may have been placed on the sensorimotor system after lower limb injury.
It should be noted that participants in this study were physically active, and at least 50% were simultaneously involved in regular sport activities including aerobic conditioning and weight lifting. The concurrent level of activity coupled with the continued natural injury-healing process could explain improvements in these measures across all groups. The inherent nature of a repeated-measures design is that participants were performing the same task at each follow-up period, and the improvement observed in the absolute minimum TTBML across all groups could also be attributed to a learning effect.
Star Excursion Balance Test
At 4-week follow-up, participants in all 3 groups had improvements in excursions when reaching in the PM and PL reach directions; however, no differences among the groups were observed. These results contrast with those of previous researchers8,28 who reported increases in the PM and PL reach directions after 4 weeks of balance rehabilitation in patients with CAI when compared with a control group. The contrasting findings between the studies may be due to the type of patients. In the current study, the injury demographic was heterogeneous, compared with the McKeon et al28 study, which examined a homogeneous subset of patients with CAI. Overall, participants in each group performed approximately 18 trials in each reach direction at the completion of the study; therefore, improvements in dynamic postural control across the 3 groups may be attributed to a learning effect. We did not find a change in the anterior reach direction, however; this is consistent with research conducted by McKeon et al,28 who reported no changes in the anterior reach direction in patients with CAI after 4 weeks of balance training when compared with a control group. It has also been thought that the anterior direction may be related to arthrokinematic impairments such as reduced posterior talar glide28 or decreased dorsiflexion range of motion,32 which were not measured in this study.
Self-Reported Function
The Wii Fit, traditional, and control groups all reported improved function when they returned for their 4-week follow-up. However, the changes in the LEFS scores were below the minimal clinically important change score of 9.24 Effect sizes from baseline to 4-week follow-up for the Wii Fit, traditional, and control groups ranged from small to moderate (0.22, 0.29, and 0.57, respectively; Table 5). Binkley et al24 assessed the reliability, construct validity, and sensitivity to change of the LEFS and reported the following means for individuals with lower extremity injury at baseline and 1-, 2-, and 4-week follow-up: 24, 42, 45, and 49, respectively. The means in the Binkley et al24 study were higher at each follow-up period than those for the patients in our study (see Table 2). We believe that our functional-outcome scores may have been affected by our convenience sample of active individuals with a history of lower limb joint injuries, particularly because 50% of the participants were Division 1 collegiate athletes who were still active.
Our study was not without limitations. One limitation was the relatively small sample size. Our sample consisted of highly functioning athletes and recreationally active individuals with a history of lower extremity injury; therefore, generalizability of our findings to other injured populations cannot be made without future investigation. Our goal was to include participants who might have balance deficits but were not presently requiring a rehabilitation program, because the Wii Fit and control groups would not receive a standard of care that would include comprehensive strengthening and functional progressions. Second, the intervention groups did not have to complete a daily journal; therefore, we do not know if participating in the Wii Fit or traditional exercise groups motivated or encouraged patients to increase video game use or the amount of exercise outside of supervised rehabilitation. Last, we chose to include individuals with different types of lower extremity injuries, making our sample nonhomogeneous in nature. Therefore, the generalization of our results to patients with lower extremity joint injuries must be made vigilantly.
Clinical Implications
We chose to examine the effects of the Wii Fit on lower limb joint injuries, because this is the first trial to our knowledge to use the Wii Fit as a rehabilitation tool in patients with a self-reported musculoskeletal injury. After 4 weeks of balance training, participants in the Wii Fit and traditional rehabilitation groups experienced a less constrained sensorimotor system and had more time available to make a postural correction. Improvements in the magnitude of the TTB in the eyes-open positions were not observed until the second week of rehabilitation; therefore, we would not expect to observe immediate clinical changes when using this device in a rehabilitation setting. Based on our results, we would recommend using the Wii Fit as an adjunctive rehabilitation tool to complement therapeutic exercise for patients with a self-reported history of lower limb injury. Because the Wii Fit is an interactive gaming device, it allows rehabilitation to be completed without the aid of a clinician. More importantly, the Wii Fit can be used to heighten patient interest and compliance and can possibly be used as a part of a home exercise program.33
Future researchers should focus on using the Wii Fit and other exergames in a homogeneous population of patients during the typical postoperative or postinjury time period. The improvements demonstrated in this study justify the need for continued examination of exergaming in musculoskeletal rehabilitation. Future investigators should also focus on changes in postural control after Wii Fit intervention in healthy individuals. A major finding of the current research study was that patients with a history of lower limb injury had improvements in the magnitude of the mean of the TTB minima; however, we currently do not know what the relationship is between an improvement in this TTB measure and injury risk. Future authors should examine the relationship between increased TTB values after a balance training program and the reinjury rate.
CONCLUSIONS
Although TTB measures improved, detriments in postural control were seen at 2 weeks for the absolute minimum TTBAP, indicating the potential need for rehabilitation with the Wii Fit to last longer than 2 weeks to obtain the full benefits. Both Wii Fit and traditional balance exercise rehabilitation interventions appear to be effective in decreasing the amount of restraints placed on the sensorimotor system and increasing the amount of time an individual has available to make a postural correction while balancing with eyes open. Rehabilitation mechanisms that allow exploration of COP may reduce these restraints and may be the reason we observed increases in the eyes-open TTB measures for the 2 rehabilitation groups over time. When comparing the Wii Fit, traditional, and control interventions, the Wii Fit intervention seems to address static postural control, specifically with the eyes open. Rehabilitation using the Wii Fit and traditional exercises has positive benefits for improving static postural control in patients with a lower extremity injury. Each approach has advantages, and the protocols may be beneficial to the patient if used in combination.
Appendix A.
Wii Fit rehabilitation protocol. Rehabilitation should be 3×/wk for no more than 15 minutes. Participants began the first session with a 15-minute assessment of body composition and current balance. Each participant began with soccer heading each time he or she began the Wii Fit program. The Wii Fit program was set up to provide additional activities and levels based on the individual's accumulated time. Participants could move on to the advanced levels when 3 stars were achieved in the basic level.
Appendix B.
Traditional rehabilitation protocol. Rehabilitation should be 3×/wk for no more than 15 minutes. Changes are in bold. Start at a challenging level. When proficient in activity, advancement can be made. A phase from each category must be done in each session.
REFERENCES
- 1.Mattacola CG, Dwyer MK. Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train. 2002;37(4):413–429. [PMC free article] [PubMed] [Google Scholar]
- 2.Blanchard Y, Carey S, Coffey J et al. The influence of concurrent cognitive tasks on postural sway in children. Pediatr Phys Ther. 2005;17(3):189–193. doi: 10.1097/01.pep.0000176578.57147.5d. [DOI] [PubMed] [Google Scholar]
- 3.Wikstrom EA, Tillman MD, Smith AN, Borsa PA. A new force-plate technology measure of dynamic postural stability: the dynamic postural stability index. J Athl Train. 2005;40(4):305–309. [PMC free article] [PubMed] [Google Scholar]
- 4.Docherty CL. Valovich McLeod TC, Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the Balance Error Scoring System. Clin J Sport Med. 2006;16(3):203–208. doi: 10.1097/00042752-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Deutsch JE, Borbely M, Filler J, Huhn K, Guarrera-Bowlby P. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys Ther. 2008;88(10):1196–1207. doi: 10.2522/ptj.20080062. [DOI] [PubMed] [Google Scholar]
- 6.Hertel J, Gay MR, Denegar CR. Differences in postural control during single-leg stance among healthy individuals with different foot types. J Athl Train. 2002;37(2):129–132. [PMC free article] [PubMed] [Google Scholar]
- 7.DeBolt LS, McCubbin JA. The effects of home-based resistance exercise on balance, power, and mobility in adults with multiple sclerosis. Arch Phys Med Rehabil. 2004;85(2):290–297. doi: 10.1016/j.apmr.2003.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2007;37(6):303–311. doi: 10.2519/jospt.2007.2322. [DOI] [PubMed] [Google Scholar]
- 9.Michell TB, Ross SE, Blackburn JT, Hirth CJ, Guskiewicz KM. Functional balance training, with or without exercise sandals, for subjects with stable or unstable ankles. J Athl Train. 2006;41(4):393–398. [PMC free article] [PubMed] [Google Scholar]
- 10.Kidgell DJ, Horvath DM, Jackson BM, Seymour PJ. Effect of six weeks of dura disc and mini-trampoline balance training on postural sway in athletes with functional ankle instability. J Strength Cond Res. 2007;21(2):466–469. doi: 10.1519/R-18945.1. [DOI] [PubMed] [Google Scholar]
- 11.Verhagen E, Bobbert M, Inklaar M et al. The effect of a balance training programme on centre of pressure excursion in one-leg stance. Clin Biomech (Bristol, Avon) 2005;20(10):1094–1100. doi: 10.1016/j.clinbiomech.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med. 1998;25(3):149–155. doi: 10.2165/00007256-199825030-00002. [DOI] [PubMed] [Google Scholar]
- 13.Henriksson M, Ledin T, Good L. Postural control after anterior cruciate ligament reconstruction and functional rehabilitation. Am J Sports Med. 2001;29(3):359–366. doi: 10.1177/03635465010290031801. [DOI] [PubMed] [Google Scholar]
- 14.Nitz JC, Kuys S, Isles R, Fu S. Is the Wii Fit a new-generation tool for improving balance, health and well-being? A pilot study. Climacteric. 2010;13(5):487–491. doi: 10.3109/13697130903395193. [DOI] [PubMed] [Google Scholar]
- 15.Graves LE, Ridgers ND, Stratton G. The contribution of upper limb and total body movement to adolescents' energy expenditure whilst playing Nintendo Wii. Eur J Appl Physiol. 2008;104(4):617–623. doi: 10.1007/s00421-008-0813-8. [DOI] [PubMed] [Google Scholar]
- 16.Martin-Moreno J, Ruiz-Fernandez D, Soriano-Paya A. Jesus Berenguer-Miralles V. Monitoring 3D movements for the rehabilitation of joints in physiotherapy. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:4836–4839. doi: 10.1109/IEMBS.2008.4650296. [DOI] [PubMed] [Google Scholar]
- 17.Harrison M. No Wii cause for concern. Emerg Med J. 2009;26(2):150. doi: 10.1136/emj.2008.058958. [DOI] [PubMed] [Google Scholar]
- 18.Lanningham-Foster L, Foster RC, McCrady SK, Jensen TB, Mitre N, Levine JA. Activity-promoting video games and increased energy expenditure. J Pediatr. 2009;154(6):819–823. doi: 10.1016/j.jpeds.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deutsch J, Robbins D, Morrison J, Bowlby PG. Virtual Rehabilitation International Conference. Haifa, Israel: 2009. Wii-based compared to standard of care balance and mobility rehabilitation for two individuals post-stroke. Paper presented at. June 29–July 2. 117–120. [Google Scholar]
- 20.Hertel J, Olmsted-Kramer LC. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25(1):33–39. doi: 10.1016/j.gaitpost.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Susco TM, McLeod TCV, Gansneder BM, Shultz SJ. Balance recovers within 20 minutes after exertion as measured by the Balance Error Scoring System. J Athl Train. 2004;39(3):241–246. [PMC free article] [PubMed] [Google Scholar]
- 22.Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- 23.Gribble PA, Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003;7(2):89–100. [Google Scholar]
- 24.Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 25.Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9(2):104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 26.Hertel J, Olmsted-Kramer L, Challis J. Time-to-boundary measures of postural control during single leg quiet standing. J Appl Biomech. 2006;22(1):67–73. doi: 10.1123/jab.22.1.67. [DOI] [PubMed] [Google Scholar]
- 27.McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. doi: 10.1186/1471-2474-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 29.Riemann BL, Guskiewicz KM, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8(2):71–82. [Google Scholar]
- 30.Haibach PS, Slobounov SM, Slobounova ES, Newell KM. Virtual time-to-contact of postural stability boundaries as a function of support surface compliance. Exp Brain Res. 2007;177(4):471–482. doi: 10.1007/s00221-006-0703-4. [DOI] [PubMed] [Google Scholar]
- 31.Davids K, Glazier P, Araujo D, Bartlett R. Movement systems as dynamical systems: the functional role of variability and its implications for sports medicine. Sports Med. 2003;33(4):245–260. doi: 10.2165/00007256-200333040-00001. [DOI] [PubMed] [Google Scholar]
- 32.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. doi: 10.2519/jospt.2006.2265. [DOI] [PubMed] [Google Scholar]
- 33.Betker AL, Szturm T, Moussavi ZK, Nett C. Video game-based exercises for balance rehabilitation: a single-subject design. Arch Phys Med Rehabil. 2006;87(8):1141–1149. doi: 10.1016/j.apmr.2006.04.010. [DOI] [PubMed] [Google Scholar]