Abstract
Context:
To improve selective infraspinatus muscle strength and endurance, researchers have recommended selective shoulder external-rotation exercise during rehabilitation or athletic conditioning programs. Although selective strengthening of the infraspinatus muscle is recommended for therapy and training, limited information is available to help clinicians design a selective strengthening program.
Objective:
To determine the most effective of 4 shoulder external-rotation exercises for selectively stimulating infraspinatus muscle activity while minimizing the use of the middle trapezius and posterior deltoid muscles.
Design:
Cross-sectional study.
Setting:
University research laboratory.
Patients or Other Participants:
A total of 30 healthy participants (24 men, 6 women; age = 22.6 ± 1.7 years, height = 176.2 ± 4.5 cm, mass = 65.6 ± 7.4 kg) from a university population.
Intervention(s):
The participants were instructed to perform 4 exercises: (1) prone horizontal abduction with external rotation (PER), (2) side-lying wiper exercise (SWE), (3) side-lying external rotation (SER), and (4) standing external-rotation exercise (STER).
Main Outcome Measure(s):
Surface electromyography signals were recorded from the infraspinatus, middle trapezius, and posterior deltoid muscles. Differences among the exercise positions were tested using a 1-way repeated-measures analysis of variance with Bonferroni adjustment.
Results:
The infraspinatus muscle activity was greater in the SWE (55.98% ± 18.79%) than in the PER (46.14% ± 15.65%), SER (43.38% ± 22.26%), and STER (26.11% ± 15.00%) (F3,87 = 19.97, P < .001). Furthermore, the SWE elicited the least amount of activity in the middle trapezius muscle (F3,87 = 20.15, P < .001). Posterior deltoid muscle activity was similar in the SWE and SER but less than that measured in the PER and STER (F3,87 = 25.10, P < .001).
Conclusions:
The SWE was superior to the PER, SER, and STER in maximizing infraspinatus activity with the least amount of middle trapezius and posterior deltoid activity. These findings may help clinicians design effective exercise programs.
Key Words: side-lying wiper exercise, selective strengthening, shoulder external-rotation exercises
Key Points.
The side-lying wiper exercise is a novel and effective exercise for selectively activating the infraspinatus muscle while minimizing the use of the posterior deltoid and middle trapezius muscles.
Clinicians may wish to consider adding the side-lying wiper exercise when designing a program to selectively strengthen the infraspinatus muscle.
Rotator cuff (RC) muscle activity is crucial for the normal performance of shoulder motion.1 The RC muscles, which comprise the infraspinatus, teres minor, subscapularis, and supraspinatus muscles,2 enable the humerus to pivot on its head within the glenoid fossa and produce rotational torque during shoulder motion.3 In particular, the infraspinatus muscle produces an approximation force to resist distraction during an overhead throwing motion.4 Furthermore, this muscle provides the primary external-rotation force.5 Given that the infraspinatus muscle plays a critical role in providing dynamic stability and producing external-rotation torque at the shoulder joint, infraspinatus-strengthening exercises have been recommended to enhance muscular strength and endurance of the RC in rehabilitation and athletic conditioning programs.2,6–11 A collective reduction in force of the RC muscle group or an isolated reduction in force of any RC muscle potentially increases humeral head translation and reduces the force required to sublux the humeral head.12 Lesions causing RC dysfunction are a common source of shoulder pain, impairment, and disability.13,14 Therefore, selective strengthening exercises to restore muscle function are an important aspect of nonoperative and postoperative treatment of RC injuries.15 Several researchers11,16,17 have recommended selective infraspinatus-strengthening exercises during rehabilitation or athletic conditioning programs to enhance muscular strength and endurance.
Among the infraspinatus muscle exercises are prone horizontal abduction with external rotation (PER),6,10,11 shoulder external rotation in the scapular plane,18 side-lying external rotation (SER),4,6,10 and standing external rotation (STER).4,10 In addition, we have developed the side-lying wiper exercise (SWE), which is performed with the shoulder flexed to 90° and supported with the opposite hand.
Researchers have reported varying results of selective infraspinatus muscle strengthening, depending on the exercise and shoulder-joint position.4,6,10,11,19 Furthermore, the optimal shoulder position to specifically strengthen the infraspinatus muscle is controversial. According to exercise position, Townsend et al11 and Blackburn et al6 reported that PER was more effective than SER in strengthening the infraspinatus muscle; however, other investigators have found that SER was the most effective exercise for activating the infraspinatus muscle.9,11 Ballantyne et al4 compared SER and external rotation in the prone position with the shoulder abducted to 90° and reported no difference in infraspinatus muscle activity between the exercises.
Although selective strengthening of the infraspinatus muscle is recommended for therapy and training, limited information is available to help clinicians design an effective strengthening program. Thus, exercise programs currently are based on functional anatomy and biomechanics of the shoulder complex, previous electromyography (EMG) studies, and clinical experience. These protocols primarily are directed at (1) increasing the tension-generating capability in isolated muscles that demonstrate deficiency,4 (2) restoring the normal kinematics of the glenohumeral (GH) and scapulothoracic joint motion,4 (3) designing functional strengthening exercises that decrease the strain on the anterior capsule and replicate the muscle length–tension relationship,17 and (4) generating precise movement while maintaining optimal control of the path of instantaneous center of rotation.20 Several investigators4,6,10,11 have focused on muscles that generate GH joint motion. Sahrmann20 reported that compensatory scapular retraction may occur during shoulder external rotation. Unnecessary scapular movement during shoulder external rotation indicates abnormal muscle dominance of the middle trapezius and rhomboid muscles and poor control of GH external rotation.
Few researchers have measured activity in compensatory muscles (ie, middle trapezius and posterior deltoid) during shoulder external-rotation exercise. Selectively activating the infraspinatus muscle is difficult with minimal use of the posterior deltoid and scapular retractor muscles in the PER and STER.10,20 Townsend et al11 reported that SER activated the infraspinatus muscle; however, this is not a functional position. Therefore, the purpose of our study was to compare muscle activity of 4 shoulder external-rotation exercises (PER, SWE, SER, and STER) to determine the most effective exercise for activating the infraspinatus muscle with minimal activity in the middle trapezius and posterior deltoid muscles. Our results may provide insight into specific muscle activation and the optimal exercise program for people with infraspinatus dysfunction. We hypothesized that the SWE exercise would selectively activate the infraspinatus muscle.
METHODS
Participants
We performed a power analysis using Excel (version 2010; Microsoft Corporation, Redmond, WA) to determine the sample size. At least 20 participants were required to attain an α level of .05 and power of .8. The effect size was set at 10% maximal voluntary isometric contraction (MVIC) to be clinically relevant.10 A total of 30 healthy participants (24 men, 6 women; age = 22.6 ± 1.7 years, height = 176.2 ± 4.5 cm, mass = 65.6 ± 7.4 kg) with no neck or shoulder conditions were recruited from the Department of Physical Therapy at Yonsei University. Exclusion criteria were a history of shoulder pain, neurologic conditions, or musculoskeletal conditions that could interfere with external rotation of the shoulder in the testing positions. All participants provided written informed consent, and the study was approved by the Yonsei University Wonju Campus Human Studies Committee.
Electromyography
Surface EMG data were collected using TeleMyo 2400T (Noraxon USA Inc, Scottsdale, AZ) and analyzed using MyoResearch software (XP Master Edition 1.06; Noraxon USA Inc) (Figure 1). The electrode sites were shaved and cleaned with rubbing alcohol. We positioned surface electrode pairs at an interelectrode distance of 2 cm. The reference electrode was placed on the ipsilateral clavicle. We collected the EMG data for the following muscles: middle trapezius (midway on a horizontal line between the root of the spine of the scapula and the third thoracic spinous process), posterior deltoid (lateral border of the spine of the scapula and angled on an oblique angle toward the upper extremity running parallel to the muscle fiber), and infraspinatus (4 cm below the spine of the scapula on the lateral aspect over its infrascapular fossa).21 The sampling rate was 1000 Hz, the raw signal was full-wave rectified and filtered using a Lancosh finite impulse response digital filter (Noraxon USA Inc), and the bandpass-filter frequency was between 20 Hz and 300 Hz. We processed the EMG data into the root mean square (RMS) value, which we calculated from 50-millisecond windows of data points.
Figure 1.
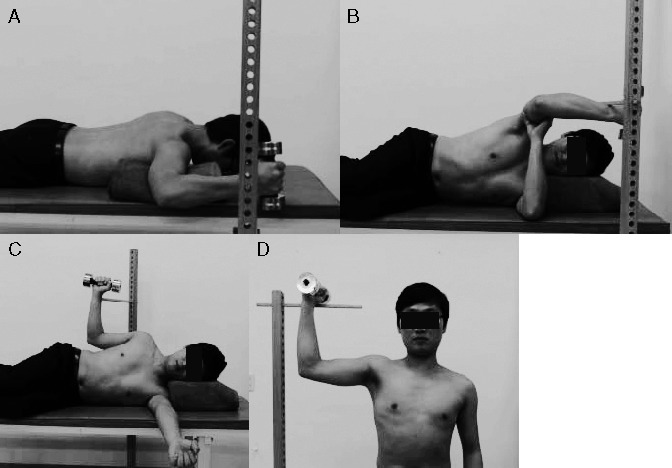
Four types of exercise. A, Prone external-rotation exercise. B, Side-lying wiper exercise. C, Side-lying external-rotation exercise. D, Standing external-rotation exercise.
For normalization, we measured the RMS of a 5-second MVIC 3 times for each muscle. All muscles were tested with the participant lying prone. The infraspinatus muscle was tested by laterally rotating the shoulder joint while stabilizing the humerus in the glenoid cavity during movement. We applied manual resistance to the wrist joint at the end range of shoulder external rotation. To test the middle trapezius muscle, we abducted the shoulder to 90° and rotated it laterally with the elbow extended. For testing of the posterior deltoid muscle, the shoulder joint was abducted horizontally with a slight lateral rotation.22 Each contraction was held for 5 seconds with maximal effort. The first and last second of each MVIC trial was discarded, and the remaining 3 seconds of EMG data were used in the analysis.10 We used a metronome to control the duration of the contraction. Participants performed 3 repetitions of each test, resting for 2 minutes after each repetition to minimize muscle fatigue.23 We closely monitored participants during each isometric test to ensure that they did not elevate or protract their scapulae or perform compensatory movements of the trunk. If a participant was performing an exercise incorrectly, we stopped the exercise and instructed him or her to repeat it. The data for each trial were expressed as a percentage of the calculated mean RMS of the MVIC (%MVIC), and the mean %MVIC of the 3 trials was used in the analysis.
Procedures
The dominant arm, which was defined as the upper extremity used to eat and write, was tested for all participants.24 All participants were right-arm dominant. A target bar was placed so that the radial border of the participant's wrist touched it in each exercise position. Each participant was tested in the prone, side-lying, and standing positions (Figure 1). For PER, the participant lay prone with the extremity abducted to 90° and the elbow flexed to 90°. He or she moved the extremity from the neutral position to full lateral rotation of the GH joint until the wrist joint touched the target bar. For SWE, the participant lay in the side-lying position with the extremity flexed and internally rotated to 90° and the elbow flexed to 90°. The participant supported the distal humerus of the dominant arm with the palm of the opposite hand. From the starting position, the participant moved to a position of full lateral rotation until the wrist joint touched the target bar. We instructed the participant to use the opposite hand to support the dominant arm during the external-rotation exercise to maintain the center of rotation in the same position. For SER, the participant lay in the side-lying position with the humerus parallel to the trunk and the elbow flexed to 90°. From the starting position with the forearm resting on the abdomen, he or she moved the extremity to a position of full lateral rotation (45°) until the wrist joint touched the target bar. For STER, the participant stood with the dominant arm abducted and internally rotated to 90° and the elbow flexed to 90°. From the starting position, the participant moved the extremity to a position of full lateral rotation until the wrist joint touched the target bar.
Participants were familiarized with the 4 external-rotation exercises during a 30-minute period before testing. A 1-kg dumbbell was provided for all exercise protocols. During the familiarization period, the principal investigator instructed the participants to move their dominant arms until the radial border of the wrists touched the target bar, which was located in a predetermined position for each exercise. The familiarization period was completed when the participants could maintain each exercise position for 5 seconds. All participants were comfortable after the familiarization period, and none reported fatigue. They rested for 15 minutes after the familiarization period and before data collection began.
The order of testing was randomized using the random number generator in Excel. The participants externally rotated their dominant arms from the starting position to the predetermined position and then sustained an isometric contraction for 5 seconds while touching the target bar. We collected the EMG data during the middle 3 seconds of the 5-second period.10 They performed 3 trials with a 1-minute rest between trials, and we used the mean value of the 3 trials in the data analysis. Participants rested for 3 minutes between exercises when changing from 1 exercise position to another, thus minimizing the chance of muscle fatigue.2,25
Statistical Analyses
We used the SPSS Statistical Package for Windows (version 18.0; IBM SPSS, Armonk, NY) to analyze differences in the infraspinatus, posterior deltoid, and midtrapezius muscles. A 1-way analysis of variance with repeated measures was used with the α level set at .05. When we found a difference, we used the Bonferroni adjustment (Padj) with the α level set at .013 (.05/4). The effect size (Cohen d) was calculated to determine the standardized mean difference among exercises for each muscle. Effect sizes were classified as small (d = 0.20), medium (d = 0.50), or large (d = 0.80).26
RESULTS
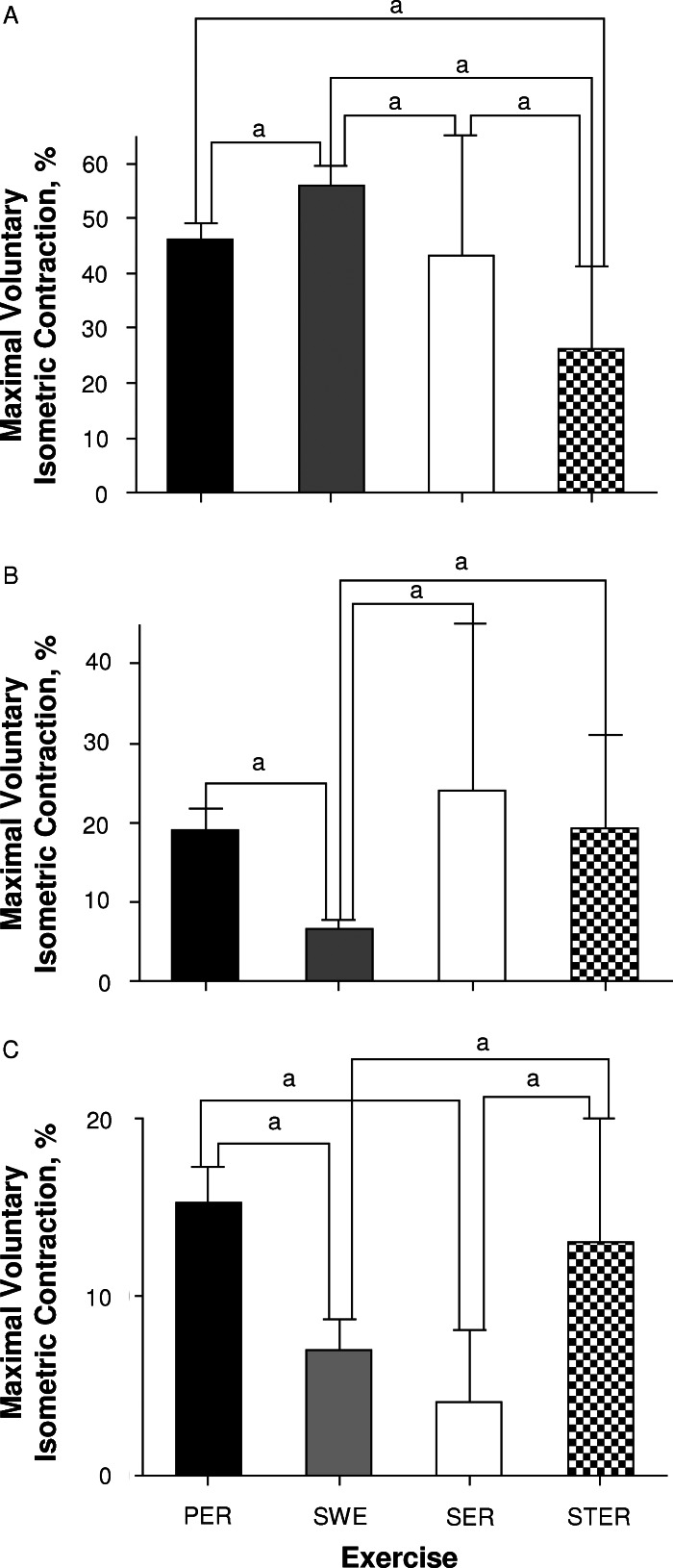
Infraspinatus EMG
The normalized EMG activity of the infraspinatus muscle is shown in Table 1 (F3,87 = 19.97, P < .001). We observed the largest increase in muscle activity during exercise in the SWE and the least activity in the STER (F3,87 = 19.97, Padj < .001 for PER versus SWE; F3,87 = 19.97, Padj = .004 for SER versus SWE; F3,87 = 19.97, Padj < .001 for STER versus SWE). Infraspinatus muscle EMG activity was not different between the PER and SER (Tables 1 and 2; Figure 2A). The calculated effect sizes of the infraspinatus muscle between exercises are shown in Table 2.
Table 1.
Electromyographic Activation for Each Exercise
| Muscle |
Exercise, % Maximal Voluntary Isometric Contraction (Mean ± SD) |
F3,87 |
P |
|||
| Prone Horizontal Abduction With External Rotation |
Side-Lying Wiper |
Side-Lying External Rotation |
Standing External Rotation |
|||
| Infraspinatus | 46.14 ± 15.65 | 55.98 ± 18.79 | 43.38 ± 22.26 | 26.11 ± 15.00 | 19.97 | <.001 |
| Middle trapezius | 19.14 ± 14.85 | 6.55 ± 6.87 | 24.14 ± 21.57 | 19.21 ± 11.90 | 20.15 | <.001 |
| Posterior deltoid | 15.31 ± 10.76 | 7.01 ± 9.26 | 4.11 ± 4.08 | 13.09 ± 12.91 | 25.10 | <.001 |
Table 2.
Multiple Comparisons Between Exercises
| Muscle |
Exercise Comparison |
P |
Effect Size |
| Infraspinatus | PER versus SWE | <.001 | 0.27 |
| PER versus SER | >.99 | 0.07 | |
| PER versus STER | <.001 | 0.54 | |
| SWE versus SER | .004 | 0.29 | |
| SWE versus STER | <.001 | 0.66 | |
| SER versus STER | <.001 | 0.41 | |
| Middle trapezius | PER versus SWE | <.001 | 0.48 |
| PER versus SER | .38 | 0.13 | |
| PER versus STER | >.99 | <.001 | |
| SWE versus SER | <.001 | 0.48 | |
| SWE versus STER | <.001 | 0.54 | |
| SER versus STER | >.99 | 0.14 | |
| Posterior deltoid | PER versus SWE | <.001 | 0.38 |
| PER versus SER | <.001 | 0.57 | |
| PER versus STER | >.99 | 0.09 | |
| SWE versus SER | .11 | 0.20 | |
| SWE versus STER | .03 | 0.26 | |
| SER versus STER | <.001 | 0.43 |
Abbreviations: PER, prone horizontal abduction with external rotation; SER, side-lying external rotation; STER, standing external rotation; SWE, side-lying wiper exercise.
Figure 2.
Comparison of the muscle activity among 4 different exercises. A, Infraspinatus. B, Middle trapezius. C, Posterior deltoid. a Indicates difference between exercise positions. Abbreviations: PER, prone external-rotation exercise; SER, side-lying external-rotation exercise; STER, standing external-rotation exercise; SWE, side-lying wiper exercise.
Middle Trapezius EMG
The normalized EMG activity in the middle trapezius muscle was greater in the PER, SER, and STER than in the SWE (F3,87 = 20.15, Padj < .001 for each). The EMG activity did not differ among the PER, SER, and STER (Tables 1 and 2; Figure 2B). The calculated effect sizes of the middle trapezius muscle between exercises are shown in Table 2.
Posterior Deltoid EMG
The normalized EMG activity in the posterior deltoid muscle was less in the SWE than in the PER (F3,87 = 20.10, Padj < .001). Posterior deltoid EMG activity was less in the SER than the PER and STER (F3,87 = 20.10, Padj < .001 for each). The EMG activity did not differ between the SER and SWE. Posterior deltoid EMG activity was not different between the PER and STER (Tables 1 and 2; Figure 2C). The calculated effect sizes of the posterior deltoid muscle between exercises are shown in Table 2.
DISCUSSION
The importance of the infraspinatus muscle in the nonoperative and postoperative treatment of the RC is well known,9 and various exercises have been developed to strengthen the infraspinatus using EMG to measure muscle activity.6,11,27,28 The current trend in exercise programs is to focus on functional restoration by strengthening specific target muscles with minimal participation of the surrounding musculature.29 The purpose of our study was to investigate the most effective of 4 shoulder external-rotation exercises for selectively stimulating infraspinatus muscle activity while minimizing the use of the middle trapezius and posterior deltoid muscles.
Researchers have disagreed about which exercise position most effectively activates the infraspinatus with minimal stimulation of the surrounding muscles. Blackburn et al6 and Townsend et al11 found the highest level of infraspinatus muscle activity (80%–88%MVIC) when participants were in the prone position with the shoulder abducted to 90°. In contrast, Reinold et al10,29 reported that the side-lying exercise with the shoulder abducted to 0° was optimal for strengthening the infraspinatus muscle while minimizing posterior deltoid muscle activity. We found that normalized EMG activity in the middle trapezius, infraspinatus, and posterior deltoid muscles differed in the 4 external-rotation exercises. Infraspinatus muscle activity was greater in the SWE (55.98% ± 18.79%) than in the PER (46.14% ± 15.65%), SER (43.38% ± 22.26%), and STER (26.11% ± 15.00%). Although our results demonstrated differences among exercises, mean differences were smaller than the standard deviations in the infraspinatus muscle activity. To be clinically relevant, the mean difference in muscle activity must be at least 10%MVIC.10 In our study, the effect size for the infraspinatus muscle was 0.66 for SWE versus STER, 0.29 for SWE versus SER, and 0.27 for SWE versus PER.
Several possible explanations exist for our results. First, infraspinatus muscle activity is related to the GH position. McMahon et al30 suggested that infraspinatus activity progressively increased from 0° to 90° in planar motion and reported that the highest level of infraspinatus muscle activity occurred during shoulder forward flexion at 90°. In our study, the SWE was performed with the shoulder flexed to 90°, whereas the other exercises were performed with the shoulder abducted to 90° or 0°.4,6,10,29
Second, SWE elicited less muscle activity in the middle trapezius muscle than the other exercises. In the SWE, the participant supported the weight of the exercise extremity with the palm of the opposite hand. This may explain why EMG activity in the middle trapezius and posterior deltoid muscles was less in the SWE.31 Researchers have reported that SER is the optimal exercise for activating the infraspinatus muscle while minimizing activity in the posterior deltoid muscle.9–11,29 However, SER with the shoulder abducted to 0° is limited in simulating functional activity, such as overhead motions, and maintaining normal scapula movement.20,29 Anatomically, the risk of subacromial impingement progressively increases over the 60° of shoulder flexion or abduction. Therefore, humeral external rotation is necessary over the 60° of shoulder flexion or abduction to prevent subacromial impingement during functional activity.32 Although the extremity is supported by abducting the humerus on the side in the SER, middle trapezius muscle activity elicited by scapular adduction was greater than that in the other exercises (Padj < .013). Our results were consistent with previous findings20; we showed that posterior deltoid muscle activity was lower in the SWE than the PER. Reinold et al10,29 reported that shoulder abduction to 90° produced moderate activity in the infraspinatus muscle in the prone position and increased activity in the posterior deltoid muscle because the deltoids actively assist in external rotation of the shoulder. Decreased muscle activity in the middle trapezius and posterior deltoid muscles may elicit increased infraspinatus muscle activity in the SWE. Our findings indicated that the SWE can selectively activate the infraspinatus muscle.
Third, both muscle length and length of the lever arm influence isometric tension generation.33 We measured muscle activity at the end position to control the effect of different muscle lengths among 4 external-rotation exercises on isometric tension generation. However, we did not control the length of the lever arm among the 4 external-rotation exercises. In PER and SWE, the long lever arm would have necessitated greater EMG activity than in SER and STER, when the forearm is almost parallel to the gravity line and approaching a zero-length lever arm. Therefore, further study is needed to compare muscle activity of the infraspinatus at the same lever-arm length among 4 different external-rotation exercises.
Generally, the position chosen for infraspinatus muscle-strengthening exercise is based on the objectives of the exercise and the patient's condition. Exercise performed with the shoulder abducted to 90° and the participant in the standing or prone position replicates the shoulder position, capsular strain, and muscle fiber length–tension relationship observed in sporting activities, making strength gains in this position advantageous.1,34–36 However, the combination of 90° of abduction and external rotation places strain on the shoulder capsule, particularly the anterior band of the inferior GH ligament,36,37 because the PER and STER can activate the posterior deltoid muscle, which causes anterior humeral head translation.38 Although exercise with the shoulder abducted to 90° may have a functional advantage because it replicates daily and sport-specific upper extremity function, the clinician must consider carefully the potential adverse effects when designing a program for a patient with anterior instability or passive structure dysfunction.29
The SER exercise performed with the shoulder abducted to 0° places less strain on the GH joint capsule and coracoacromial ligament than the PER and STER exercises with the shoulder abducted to 90°.29 Although muscle activity was low to moderate in this position, it can be used as a safe exercise. However, our results indicated that external-rotation exercise with the shoulder abducted to 0° increased middle trapezius muscle activity. Middle trapezius muscle compensatory activity may decrease the effectiveness of selective infraspinatus muscle contraction and alter the movement pattern. That is, if the middle trapezius contracts dominantly over the infraspinatus during shoulder external rotation, subsequent scapular adduction will occur and may reduce the participation of the infraspinatus muscle.20 Thus, the SWE exercise is a good candidate for the selective and functional strengthening of the infraspinatus muscle.
Two experimental methods of this study need further discussion. First, all participants, regardless of their mass, used a 1-kg dumbbell in each exercise because participants in a pilot study were comfortable with a 1-kg dumbbell. In a previous study,10 the amount of resistance was selected according to participants' body mass. In a preliminary study, we applied a 1-kg or 2-kg dumbbell during shoulder external-rotation exercises; however, some participants could not complete external rotation and reported discomfort when a 2-kg dumbbell was applied. Furthermore, the standard deviation of mass was not highly variable (±7.4 kg) in our study. Therefore, we applied a 1-kg weight for all participants. Second, speed of movement affected muscle activity in an EMG study.39 Therefore, we measured muscle activity during isometric contraction at the end position. Further research is necessary to assess the muscle activity throughout the range of motion during shoulder external-rotation exercises with speed controlled.
Our investigation had several limitations. First, our results are not widely generalizable because all participants were healthy students. Thus, additional research is needed to establish whether our findings apply to participants with shoulder pain. Second, we did not obtain kinematic measurements of humeral and scapular movements, and further studies are necessary to assess them. Third, our study was cross sectional, so longitudinal follow-up is warranted to determine the long-term effects of selective training for patients who have shoulder pain and infraspinatus weakness. Fourth, we did not measure the activity of the teres minor muscle, which plays an important role as an external rotator, due to the limitation of surface EMG for measuring activity of that muscle. Further study using wire EMG is needed to determine the role of the teres minor muscle during shoulder external-rotation exercise.
CONCLUSIONS
We investigated activation of the infraspinatus, middle trapezius, and posterior deltoid muscles during 4 external-rotation exercises. More infraspinatus muscle activity was observed with SWE than the other exercises. The SWE elicited less activity in the middle trapezius muscle than the other exercises and less activity in the posterior deltoid muscle than the PER and STER. Our results suggest that the SWE is a novel and effective exercise because it selectively activates the infraspinatus muscle while minimizing the use of the posterior deltoid and middle trapezius muscles. These findings may help clinicians design effective exercise programs.
REFERENCES
- 1.Wilk KE, Arrigo C. Current concepts in the rehabilitation of the athletic shoulder. J Orthop Sports Phys Ther. 1993;18(1):365–378. doi: 10.2519/jospt.1993.18.1.365. [DOI] [PubMed] [Google Scholar]
- 2.Brewster C, Schwab DR. Rehabilitation of the shoulder following rotator cuff injury or surgery. J Orthop Sports Phys Ther. 1993;18(2):422–426. doi: 10.2519/jospt.1993.18.2.422. [DOI] [PubMed] [Google Scholar]
- 3.Lippitt S, Matsen F. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res. 1993;291:20–28. [PubMed] [Google Scholar]
- 4.Ballantyne BT, O'Hare SJ, Paschall JL et al. Electromyographic activity of selected shoulder muscle in commonly used therapeutic exercises. Phys Ther. 1993;73(10):668–677. doi: 10.1093/ptj/73.10.668. [DOI] [PubMed] [Google Scholar]
- 5.Terry GC, Chopp TM. Functional anatomy of the shoulder. J Athl Train. 2000;35(3):248–255. [PMC free article] [PubMed] [Google Scholar]
- 6.Blackburn TA, McLeod WD, White B, Wofford L. EMG analysis of posterior rotator cuff exercises. Athl Train J Natl Athl Train Assoc. 1990;25(1):40–45. [Google Scholar]
- 7.Ellenbecker TS, Mattalino AJ. Concentric isokinetic shoulder internal and external rotation strength in professional baseball pitchers. J Orthop Sports Phys Ther. 1997;25(5):323–328. doi: 10.2519/jospt.1997.25.5.323. [DOI] [PubMed] [Google Scholar]
- 8.Hess SA. Functional stability of the glenohumeral joint. Man Ther. 2000;5(2):63–71. doi: 10.1054/math.2000.0241. [DOI] [PubMed] [Google Scholar]
- 9.Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med. 1982;10(6):336–339. doi: 10.1177/036354658201000602. [DOI] [PubMed] [Google Scholar]
- 10.Reinold MM, Wilk KE, Fleisig GS et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004;34(7):385–394. doi: 10.2519/jospt.2004.34.7.385. [DOI] [PubMed] [Google Scholar]
- 11.Townsend H, Jobe FW, Pink M, Perry J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med. 1991;19(3):264–272. doi: 10.1177/036354659101900309. [DOI] [PubMed] [Google Scholar]
- 12.Wuelker N, Wirth CJ, Plitz W, Roetman B. A dynamic shoulder model: reliability testing and muscle force study. J Biomech. 1995;28(5):489–499. doi: 10.1016/0021-9290(94)e0006-o. [DOI] [PubMed] [Google Scholar]
- 13.Murrell GA, Walton JR. Diagnosis of rotator cuff tears. Lancet. 2001;357(9258):769–770. doi: 10.1016/S0140-6736(00)04161-1. [DOI] [PubMed] [Google Scholar]
- 14.Norwood LA, Barrack R, Jacobson KE. Clinical presentation of complete tears of the rotator cuff. J Bone Joint Surg Am. 1989;71(4):499–505. [PubMed] [Google Scholar]
- 15.Malanga GA, Jenp YN, Growney ES, An KN. EMG analysis of shoulder positioning in testing and strengthening the supraspinatus. Med Sci Sports Exerc. 1996;28(6):661–664. doi: 10.1097/00005768-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30(1):136–151. doi: 10.1177/03635465020300011201. [DOI] [PubMed] [Google Scholar]
- 17.Wilk KE, Reinold MM, Andrews JR. Postoperative treatment principles in the throwing athlete. Sports Med Arthrosc Rev. 2001;9(1):69–95. [Google Scholar]
- 18.David G, Magarey ME, Jones MA et al. and strength correlates of selected shoulder muscles during rotations of the glenohumeral joint. Clin Biomech (Bristol, Avon) 2000;15(2):95–102. doi: 10.1016/s0268-0033(99)00052-2. [DOI] [PubMed] [Google Scholar]
- 19.Greenfield BH, Donatelli R, Wooden MJ, Wilkes J. Isokinetic evaluation of shoulder rotational strength between the plane of scapula and the frontal plane. Am J Sports Med. 1990;18(2):124–128. doi: 10.1177/036354659001800202. [DOI] [PubMed] [Google Scholar]
- 20.Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO: Mosby;; 2002. pp. 205–207. [Google Scholar]
- 21.Cram JR, Kasman GS, Holtz J. Introduction to Surface Electromyography. Gaithersburg, MD: Aspen;; 1998. pp. 276pp. 288–293. [Google Scholar]
- 22.Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles: Testing and Function With Posture and Pain. 5th ed. Baltimore, MD: Williams & Wilkins;; 2005. [Google Scholar]
- 23.Vera-Garcia FJ, Moreside JM, McGill SM. MVC techniques to normalize trunk muscle EMG in healthy women. J Electromyogr Kinesiol. 2010;20(1):10–16. doi: 10.1016/j.jelekin.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 24.Yoshizaki K, Hamada J, Tamai K et al. Analysis of the scapulohumeral rhythm and electromyography of the shoulder muscles during elevation and lowering: comparison of dominant and nondominant shoulders. J Shoulder Elbow Surg. 2009;18(5):756–763. doi: 10.1016/j.jse.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 25.Dankaerts W, O'Sullivan PB, Burnett AF, Straker LM, Danneels LA. Reliability of EMG measurements for trunk muscles during maximal and sub-maximal voluntary isometric contractions in healthy controls and CLBP patients. J Electromyogr Kinesiol. 2004;14(3):333–342. doi: 10.1016/j.jelekin.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, NJ: Pearson Education;; 2009. [Google Scholar]
- 27.Glousman R, Jobe F, Tibone J et al. Dynamic electromyography analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70(2):220–226. [PubMed] [Google Scholar]
- 28.Kronberg M, Nerneth G, Brostrom LM. Muscle activity and coordination in the normal shoulder. Clin Orthop Relat Res. 1990;257:76–85. [PubMed] [Google Scholar]
- 29.Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39(2):105–117. doi: 10.2519/jospt.2009.2835. [DOI] [PubMed] [Google Scholar]
- 30.McMahon PJ, Debski RE, Thompson WO et al. Shoulder muscle forces and tendon excursions during glenohumeral abduction in the scapular plane. J Shoulder Elbow Surg. 1995;4(3):199–208. doi: 10.1016/s1058-2746(05)80052-7. [DOI] [PubMed] [Google Scholar]
- 31.Wise MB, Uhl TL, Mattacola CG, Nitz AJ, Kibler WB. The effect of limb support on muscle activation during shoulder exercises. J Shoulder Elbow Surg. 2004;13(6):614–620. doi: 10.1016/j.jse.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Brossmann J, Preidler KW, Pedowitz RA et al. Shoulder impingement syndrome: influence of shoulder position on rotator cuff impingement. An anatomic study. AJR Am J Roentgenol. 1996;167(6):1511–1515. doi: 10.2214/ajr.167.6.8956588. [DOI] [PubMed] [Google Scholar]
- 33.Lunnen JD, Yack J, LeVeau BF. Relationship between muscle length, muscle activity, and torque of the hamstring muscles. Phys Ther. 1981;61(2):190–195. doi: 10.1093/ptj/61.2.190. [DOI] [PubMed] [Google Scholar]
- 34.Fleisig GS, Barrentine SW, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21(6):421–437. doi: 10.2165/00007256-199621060-00004. [DOI] [PubMed] [Google Scholar]
- 35.Fleisig GS, Escamilla RF, Andrews JR et al. Kinematic and kinetic comparison between baseball pitching and football passing. J Appl Biomech. 1996;12(2):207–224. [Google Scholar]
- 36.Wilk KE, Arrigo CA, Andrews JR. Current concepts: the stabilizing structures of the glenohumeral joint. J Orthop Sports Phys Ther. 1997;25(6):364–379. doi: 10.2519/jospt.1997.25.6.364. [DOI] [PubMed] [Google Scholar]
- 37.O'Brien SJ, Neves MC, Arnoczky SP et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18(5):449–456. doi: 10.1177/036354659001800501. [DOI] [PubMed] [Google Scholar]
- 38.Lee SB, An KN. Dynamic glenohumeral stability provided by three head of the deltoid muscle. Clin Orthop Relat Res. 2002;400:40–47. doi: 10.1097/00003086-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Heckathorne CW, Childress DS. Relationships of the surface electromyogram to the force, length, velocity, and conduction rate of the cineplastic human biceps. Am J Phys Med. 1981;60(1):1–19. [PubMed] [Google Scholar]