Abstract
Context:
Successful implementation of evidence-based practice (EBP) within athletic training is contingent upon understanding the attitudes and beliefs and perceived barriers toward EBP as well as the accessibility to EBP resources of athletic training educators, clinicians, and students.
Objective:
To assess the attitudes, beliefs, and perceived barriers toward EBP and accessibility to EBP resources among athletic training educators, clinicians, and students.
Design:
Cross-sectional study.
Setting:
Online survey instrument.
Patients or Other Participants:
A total of 1209 athletic trainers participated: professional athletic training education program directors (n = 132), clinical preceptors (n = 266), clinicians (n = 716), postprofessional athletic training educators (n = 24) and postprofessional students (n = 71).
Main Outcome Measure(s):
Likert-scale items (1 = strongly disagree, 4 = strongly agree) assessed attitudes and beliefs and perceived barriers, whereas multipart questions assessed accessibility to resources. Kruskal-Wallis H tests (P ≤ .05) and Mann-Whitney U tests with a Bonferroni adjustment (P ≤ .01) were used to determine differences among groups.
Results:
Athletic trainers agreed (3.27 ± 0.39 out of 4.0) that EBP has various benefits to clinical practice and disagreed (2.23 ± 0.42 out of 4.0) that negative perceptions are associated with EBP. Benefits to practice scores (P = .002) and negative perception scores (P < .001) differed among groups. With respect to perceived barriers, athletic trainers disagreed that personal skills and attributes (2.29 ± 0.52 out of 4.0) as well as support and accessibility to resources (2.40 ± 0.40 out of 4.0) were barriers to EBP implementation. Differences were found among groups for personal skills and attributes scores (P < .001) and support and accessibility to resources scores (P < .001). Time (76.6%) and availability of EBP mentors (69.6%) were the 2 most prevalent barriers reported. Of the resources assessed, participants were most unfamiliar with clinical prediction rules (37.6%) and Cochrane databases (52.5%); direct access to these 2 resources varied among participants.
Conclusions:
Athletic trainers had positive attitudes toward the implementation of EBP within didactic education and clinical practice. However, accessibility and resource use remained low for some EBP-related resources. Although the perceived barriers to implementation are minimal, effective integration of EBP within athletic training will present challenges until these barriers dissolve.
Key Words: athletic training education, evidence-based medicine, survey research
Key Points.
Athletic trainers' attitudes toward the implementation of evidence-based practice within clinical practice and didactic education were favorable, yet barriers exist.
Improving access to resources and eliminating barriers to implementation must be addressed.
Athletic trainers should be educated about evidence-based practice concepts and assisted with strategies for incorporating evidence into daily clinical practice.
In the spring of 2011, the National Athletic Trainers' Association (NATA) Executive Committee for Education released the fifth edition of the Athletic Training Education Competencies.1 These competencies, which must be fully implemented in Commission on Accreditation of Athletic Training Education (CAATE)–accredited professional athletic training education programs by the end of the 2012–2013 academic year, contain several changes. Of particular interest is the addition of an evidence-based practice (EBP) content area.1 This area contains new competencies pertaining to various aspects of EBP in which students must be proficient before they graduate and sit for the Board of Certification examination.
To effectively educate athletic training students, it is imperative that educators and clinicians be fully competent in the content areas of EBP as well.2 Overall, the goal of the athletic training profession is to provide efficient patient care3; therefore, we must produce clinicians who routinely search the evidence for optimal treatment methods and interventions for each patient or problem. However, without a full understanding of the various concepts of EBP, we may never achieve this goal. The infusion of EBP requires a multifaceted approach to educating the profession on the concepts associated with EBP as well as effective strategies for implementation within clinical practice.
Several challenges may restrict athletic trainers and athletic training students from accepting EBP and incorporating it in everyday clinical practice. The most prevalent barrier to implementing EBP is athletic trainers' perceived lack of knowledge of the EBP process and associated concepts.4,5 Other health care professions have also reported lack of knowledge as a barrier,6–9 but these professions have begun to incorporate strategies to educate their members about EBP.10–13 Additional commonly reported barriers include time4,5,7 and accessibility and use of resources.7,14,15 Although previous researchers7 studying nurses and physical therapists reported that most clinicians are aware that they have access to professional literature, one study15 revealed that only 20% of clinicians read professional literature on a regular basis.
As EBP becomes infused within athletic training education, it is important to have an understanding of athletic trainers' perceptions regarding EBP concepts. More specifically, it is critical to assess athletic trainers' knowledge of, attitudes and beliefs toward, accessibility to, and barriers to EBP resources within clinical practice and didactic education. Previous researchers have attempted to identify these factors. However, each investigation primarily focused on 1 subgroup of athletic trainers: educators,2,16 clinical preceptors,17 and professional athletic training students.18 Therefore, the purpose of our study was to assess the attitudes and beliefs, accessibility, and perceived barriers to EBP resources among athletic training educators, clinicians, and students. We hypothesized the following: (1) Individuals affiliated with athletic training education programs (ie, educators, clinical preceptors, students) would achieve higher composite scores on the benefits to practice items, indicating agreement that EBP provides various benefits to practice; (2) Clinicians would achieve lower negative perception composite scores regarding the implementation of EBP than all other athletic training groups; (3) Professional program directors, postprofessional educators, and postprofessional students would report using resources relating to EBP more frequently than did clinical preceptors and clinicians not affiliated with education programs; (4) Professional program directors, postprofessional educators, and postprofessional students would report higher rates of direct access to resources than did clinical preceptors and clinicians not affiliated with education programs; (5) Clinicians would achieve higher composite scores regarding perceived barriers relating to personal skills and attributes than all other athletic training groups; and (6) Clinicians would achieve higher composite scores regarding perceived barriers relating to support and accessibility to resources than all other athletic training groups.
METHODS
Participants
Professional athletic training education program directors, clinical preceptors, clinicians not affiliated with athletic training education programs, postprofessional educators, and postprofessional students (N = 6702) were solicited for participation during the spring of 2010. A total of 1209 individuals responded to the Evidence-Based Concepts Assessment (EBCA), for an overall response rate of 18.04%. Demographics of the participants are presented in Part 1 of this series.19 The Old Dominion University Institutional Review Board approved this study as exempt research, and consent was implied upon voluntary submission of the completed survey.
Instrumentation
Within the past decade, several instruments have been developed to assess numerous aspects of EBP.2,7,10,14,18,20 However, each EBP instrument is different and may have been developed to target a specific population. Because of the lack of preexisting instruments to assess various concepts of EBP across several groups within athletic training, we created an online survey using Inquisite Corporate Survey Builder (version 8.0; Catapult Systems, Austin, TX). The EBCA consisted of 6 sections: (1) perceived importance of EBP concepts, (2) attitudes and beliefs toward EBP, (3) accessibility to EBP resources, (4) knowledge of EBP, (5) confidence in knowledge, and (6) perceived barriers to EBP implementation. Additionally, participants were asked to complete a demographic questionnaire at the end of the online instrument. Each section of the EBCA included 4-point Likert-scale items (4 = strongly agree, 3 = agree, 2 = disagree, 1 = strongly disagree), multiple choice questions, or multipart questions. With permission from the authors, we adopted some questions from previously established EBP instruments.7,14,18 Once the instrument was developed, a panel of 5 experts assessed the survey for content validity, and changes were made as necessary. The EBCA was deemed a valid and reliable instrument to assess perceived importance, knowledge, confidence in knowledge, attitudes and beliefs, accessibility, and perceived barriers among various groups of athletic trainers.19 The focus of this article is to discuss attitudes and beliefs, accessibility, and perceived barriers among the different athletic training groups; Part 1 of this series discusses perceived importance, knowledge, and confidence in knowledge.19
Attitudes and Beliefs
The attitudes and beliefs section included 15 items on a 4-point Likert scale assessing participants' perceptions of the various aspects of EBP. Principal component analysis revealed 2 distinct groups of questions. The first group, negative perceptions (α = .74), included 6 Likert-scale items that provided negative statements about EBP. The second group, benefits to practice (α = .73), included 5 Likert-scale items that consisted of statements that promoted the implementation of EBP within clinical practice. The remaining 4 Likert-scale items within the attitudes and beliefs section did not fit well with the rest of the items; therefore, these items were reported independently. The composite score for each group was averaged and normalized to the Likert scale; the maximum score was 4. Statements relating to negative perceptions are displayed in Table 1, whereas statements relating to benefits to practice are displayed in Table 2.
Table 1.
Negative Perceptions About Evidence-Based Practice Resources Among Athletic Training Groups, No. (%)
| Attitudes and Beliefs Negative Perception Items |
Professional Athletic Training Education Program Directors |
Clinical Preceptors |
Athletic Training Clinicians |
Postprofessional Athletic Training Educators |
Postprofessional Athletic Training Students |
|||||
| Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
|
| The adoption of evidence-based practice places unreasonable demands in my daily practice | 44 (33.4) | 88 (66.6) | 61 (23.0) | 205 (77.0) | 144 (20.1) | 572 (79.9) | 5 (20.9) | 19 (79.1) | 9 (12.7) | 62 (87.3) |
| Evidence-based practice does not take into account the limitations of my clinical practice setting | 72 (54.6) | 60 (45.4) | 163 (61.3) | 103 (38.7) | 417 (58.3) | 299 (41.7) | 14 (58.4) | 10 (41.6) | 33 (46.5) | 38 (53.5) |
| Evidence-based practice does not take into account patient preferences | 69 (52.3) | 63 (47.7) | 161 (60.5) | 105 (39.4) | 445 (62.1) | 271 (37.9) | 13 (54.1) | 11 (45.9) | 27 (38.0) | 44 (62.0) |
| Using evidence-based practice is a “cookbook” clinical practice | 24 (18.2) | 108 (81.8) | 78 (29.4) | 188 (70.6) | 191 (26.6) | 525 (73.4) | 1 (4.2) | 23 (95.8) | 13 (18.3) | 58 (81.7) |
| Using evidence-based practice will reduce my professional independence in clinical decision-making | 23 (17.4) | 109 (82.6) | 44 (16.5) | 222 (83.5) | 103 (14.4) | 613 (85.6) | 2 (8.3) | 22 (91.7) | 8 (11.3) | 63 (88.7) |
| The concept of evidence-based practice is a “fad” that will come and go | 19 (14.4) | 113 (85.6) | 16 (6.0) | 250 (94.0) | 72 (10.1) | 644 (89.9) | 1 (4.2) | 23 (95.8) | 5 (7.0) | 66 (93.0) |
Table 2.
Benefits to Practice Among Athletic Training Groups, No. (%)
| Attitudes and Beliefs Benefits to Practice Items |
Professional Athletic Training Education Program Directors |
Clinical Preceptors |
Athletic Training Clinicians |
Postprofessional Athletic Training Educators |
Postprofessional Athletic Training Students |
|||||
| Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
|
| Application of evidence-based practice is important to the credibility of the athletic training profession | 131 (99.2) | 1 (0.8) | 261 (98.1) | 5 (1.9) | 708 (98.9) | 8 (1.1) | 24 (100.0) | 0 (0.0) | 69 (97.2) | 2 (2.8) |
| Literature and research findings are useful in my day-to-day practice | 118 (89.4) | 14 (10.6) | 247 (92.9) | 19 (7.1) | 658 (91.9) | 58 (8.1) | 22 (91.7) | 2 (8.3) | 66 (93.0) | 5 (7.0) |
| Evidence-based practice improves the quality of patient care | 121 (91.7) | 11 (8.3) | 248 (93.2) | 18 (6.8) | 670 (93.6) | 46 (6.4) | 22 (91.7) | 2 (8.3) | 68 (95.8) | 3 (4.2) |
| Evidence-based practice is a process that helps me make decisions about patient care | 114 (86.3) | 18 (13.7) | 237 (89.0) | 29 (11.0) | 648 (90.5) | 68 (9.5) | 22 (91.7) | 2 (8.3) | 68 (95.8) | 3 (4.2) |
| Developing a clinical question helps direct my search for evidence | 118 (89.4) | 14 (10.6) | 236 (88.7) | 30 (11.3) | 649 (90.6) | 67 (9.4) | 23 (95.8) | 1 (4.2) | 51 (71.8) | 20 (28.2) |
Accessibility
The accessibility section included 2 multipart questions assessing participants' access to resources that enhance clinical decision making. The first question asked participants how often they used 10 common resources: systematic reviews and/or meta-analyses, peer-reviewed journal articles (eg, Journal of Athletic Training, Journal of Sport Rehabilitation, Journal of Strength and Conditioning Research), clinical prediction rules, professional literature (eg, NATA News, Training & Conditioning, BioMechanics), Cochrane databases, MEDLINE and PubMed databases (eg, MEDLINE, PubMed, OvidSP), NATA Think Tanks, textbooks, Web sites (eg, Google Scholar, Wikipedia, WebMD), and NATA position statements. The participant had 6 choices that ranged from never to more than once a week. A seventh choice was available if the participant was unfamiliar with the resource. The second multipart question asked participants to identify the resources to which they had direct access among the 10 listed. Direct access was defined as being able to access the resource and its content through work or home without assistance from other individuals.
Perceived Barriers
The perceived barriers section included 16 Likert-scale items assessing the participants' own barriers that prevented them from EBP implementation. Principal component analysis revealed 2 groups of questions. The first group, personal skills and attributes barriers (α = .83), included 8 Likert-scale items that assessed participants' perceived barriers relating to their own practices. The second group, support and accessibility to resources barriers (α = .71), included 6 Likert-scale items that assessed participants' perceived barriers relating to external resources. Similar to the attitudes and beliefs section, the remaining 2 Likert-scale items were reported independently. Again, the composite score for each group was averaged and then normalized to the Likert scale. Statements relating to each of these groups are displayed in Tables 3 and 4, respectively.
Table 3.
Personal Skills and Attributes Barriers Among Athletic Training Groups, No. (%)
| Barriers Personal Skills and Attributes Items |
Professional Athletic Training Education Program Directors |
Clinical Preceptors |
Athletic Training Clinicians |
Postprofessional Athletic Training Educators |
Postprofessional Athletic Training Students |
|||||
| Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
|
| Ability to critically appraise the literature | 43 (32.5) | 89 (67.5) | 98 (36.8) | 168 (63.2) | 299 (41.8) | 417 (58.2) | 2 (8.4) | 22 (91.6) | 17 (23.9) | 54 (76.1) |
| Personal confidence to implement changes in my clinical practice | 49 (37.1) | 83 (62.9) | 98 (36.8) | 168 (63.2) | 243 (33.9) | 473 (66.1) | 4 (16.7) | 20 (83.3) | 30 (42.3) | 41 (57.7) |
| Personal interest in evidence-based practice | 61 (46.2) | 71 (53.8) | 105 (39.4) | 161 (60.6) | 308 (43.0) | 408 (57.0) | 4 (16.7) | 20 (83.3) | 19 (26.8) | 52 (73.2) |
| Understanding of the evidence-based practice process | 62 (47.0) | 70 (53.0) | 136 (51.1) | 130 (48.9) | 334 (46.6) | 382 (53.4) | 2 (8.4) | 22 (91.6) | 15 (21.1) | 56 (78.9) |
| Understanding statistical analyses | 58 (43.9) | 74 (56.1) | 144 (54.2) | 122 (45.8) | 408 (57.0) | 308 (43.0) | 2 (8.4) | 22 (91.6) | 30 (42.3) | 41 (57.7) |
| Ability to make independent clinical decisions | 26 (19.7) | 106 (80.3) | 51 (19.2) | 215 (80.8) | 159 (22.2) | 557 (77.8) | 1 (4.2) | 23 (95.8) | 12 (16.9) | 59 (83.1) |
| Ability to develop an answerable clinical question | 38 (28.8) | 94 (71.2) | 86 (32.4) | 180 (67.6) | 230 (32.1) | 486 (67.9) | 2 (8.4) | 22 (91.6) | 22 (31.0) | 49 (69.0) |
| Familiarity with Internet databases and search engines | 40 (30.3) | 92 (69.7) | 75 (28.2) | 191 (71.8) | 274 (38.3) | 442 (61.7) | 1 (4.2) | 23 (95.8) | 10 (14.1) | 61 (85.9) |
Table 4.
Support and Accessibility of Resources Barriers Among Athletic Training Groups, No. (%)
| Barriers Support and Accessibility of Resources Items |
Professional Athletic Training Education Program Directors |
Clinical Preceptors |
Athletic Training Clinicians |
Postprofessional Athletic Training Educators |
Postprofessional Athletic Training Students |
|||||
| Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
Agree |
Disagree |
|
| Accessibility of information resources | 33 (25.0) | 99 (75.0) | 92 (34.6) | 174 (65.4) | 314 (43.8) | 402 (56.2) | 3 (12.5) | 21 (87.5) | 15 (21.1) | 56 (78.9) |
| Support from administration | 28 (21.2) | 104 (78.8) | 81 (30.4) | 185 (69.6) | 224 (31.3) | 492 (68.7) | 2 (8.4) | 22 (91.6) | 17 (23.9) | 54 (76.1) |
| Ability to find research literature that relates to my patient population | 56 (42.4) | 76 (57.6) | 119 (44.7) | 147 (55.3) | 356 (49.7) | 360 (50.3) | 13 (54.2) | 11 (45.8) | 29 (40.9) | 42 (59.1) |
| Accessibility of patient outcome assessments | 82 (62.1) | 50 (37.9) | 158 (59.4) | 108 (40.6) | 425 (59.7) | 291 (40.3) | 7 (29.1) | 17 (70.9) | 29 (40.9) | 42 (59.1) |
| Collective support among colleagues in my facility | 53 (40.1) | 79 (59.9) | 92 (34.5) | 174 (65.5) | 247 (34.5) | 469 (65.5) | 3 (12.5) | 21 (87.5) | 24 (33.8) | 47 (66.2) |
| Application of research findings to individual patients with unique characteristics | 74 (56.0) | 58 (44.0) | 158 (59.4) | 108 (40.6) | 405 (56.5) | 311 (43.5) | 14 (58.3) | 10 (41.7) | 36 (50.7) | 35 (49.3) |
Procedures
During the data-collection period, participants were sent an e-mail that included the purpose and importance of the study, the estimated time to complete the survey, a hyperlink to the survey Web page, the date when the survey should be completed, and a request for their participation. Participants were given 4 weeks to complete the EBCA. Reminder emails were sent biweekly to thank those individuals who completed the survey and remind those who had not yet responded. Although survey distribution was consistent, recruitment for each group of participants differed slightly. Part 1 of this series provides a detailed description of recruitment procedures for each of the 5 athletic training groups.19
Data Analysis
We used SPSS (version 16.0; SPSS Inc, Chicago, IL) to calculate the statistical components. Descriptive statistics were used to calculate the means, standard deviations, and frequencies of the data within each section. A Kruskal-Wallis H test was used to detect differences for the ordinal data in the attitudes and beliefs and perceived barriers sections among the 5 athletic training groups. A Mann-Whitney U test with a Bonferroni adjustment was used to correct for type I error, which is commonly associated with multiple comparisons. The significance level was set at P ≤ .05 for each Kruskal-Wallis H test; taking into consideration the Bonferroni adjustment for 5 comparison groups, the significance level for each Mann-Whitney U test was set at P ≤ .01.
RESULTS
Attitudes and Beliefs
Overall, 60.07% of participants reported they agreed and 24.1% reported they strongly agreed with the statement, “I need to increase the use of evidence in my daily practice.” A majority of participants (93.2%) were “interested in learning or improving the skills necessary to incorporate evidence-based practice into clinical practice.” Approximately 66% of clinical preceptors and 72.1% of clinicians indicated they disagreed or strongly disagreed with the statement, “Strong evidence is lacking to support most interventions I use with my patients,” whereas 60.5% of postprofessional students and 79.2% of postprofessional educators agreed or strongly agreed with the statement. Program directors were fairly evenly divided regarding this statement, with 54% reporting they disagreed or strongly disagreed.
Negative Perceptions.
The composite score for negative perceptions toward EBP was 2.23 (disagree). We noted a difference in negative perceptions composite scores among the different athletic training groups (H = 31.26, P < .001). Negative perceptions composite scores reported by postprofessional students were lower than those of program directors (U = 3446, z = −3.13, P = .002), clinical preceptors (U = 6371, z = −4.25, P < .001), and clinicians (U = 16 606, z = −4.87, P < .001). Furthermore, postprofessional educators also had lower scores than clinicians (U = 5456, z = −3.08, P = .002) and clinical preceptors (U = 2061, z = −2.90, P = .004). Although statistically significant differences occurred among groups, group means ranged from 1.93 to 2.26, indicating that all 5 athletic training groups reported they disagreed on the negative perceptions toward EBP (Table 1).
Although all groups' composite scores indicated they disagreed that negative perceptions were associated with EBP, percentage differences were noted for particular statements. Program directors (54.6%), postprofessional educators (58.4%), clinical preceptors (61.3%), and clinicians (58.3%) reported they agreed with the statement, “Evidence-based practice does not take into account the limitation of [their] clinical practice setting.” These 4 groups also agreed (52.3%–62.1%) with the statement, “Evidence-based practice does not take into account patient preferences.”
Benefits to Practice.
Overall, participants reported they agreed (3.27 out of 4.0) that EBP had benefits to clinical practice. A difference was found between groups with regard to benefits to practice composite scores (H = 16.56, P = .002). Benefits to practice composite scores reported by postprofessional educators were higher than those of postprofessional students (U = 519, z = −2.91, P = .004), program directors (U = 1001, z = −2.90, P = .004), clinical preceptors (U = 1736, z = −3.76, P < .001), and clinicians (U = 5025, z = −3.51, P < .001) (Table 2). No other differences were found among groups. It is important to note, however, that regardless of the differences between postprofessional athletic training educators and the other 4 groups, all groups reported they agreed that EBP offered benefits to clinical practice (3.23–3.53 out of 4.0).
Accessibility
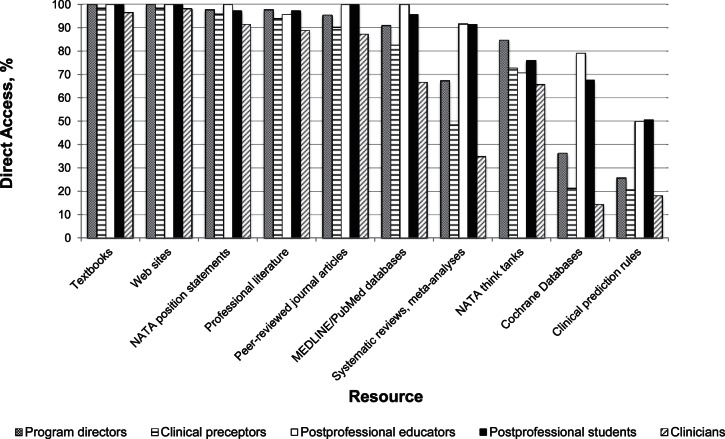
Direct Access to Resources.
Nearly all participants had direct access to textbooks (97.7%) and Web sites (98.5%) (Figure 1). More than 90% of the respondents had direct access to NATA position statements. More than 90% of program directors, postprofessional educators, and postprofessional students had direct access to MEDLINE or PubMed databases; however, only 82.7% of clinical preceptors and 66.8% of clinicians had direct access to this resource. Direct access to NATA Think Tanks remained moderate, with a range of 65.8% to 84.8% access among the groups. Direct access to professional literature was above 89% for all groups, whereas access to peer-reviewed journal articles averaged 87.3%. Approximately 92% of postprofessional educators and postprofessional students had direct access to systematic reviews or meta-analyses; only 34.9% of clinicians reported such access. Direct access to Cochrane databases varied greatly: 79.2% of postprofessional athletic training educators had access, but only 14.5% of clinicians did. Finally, direct access to clinical prediction rules was the lowest overall, with a range from 18.2% to 50.7% among the athletic training groups.
Figure 1.
Direct access to resources for athletic training groups.
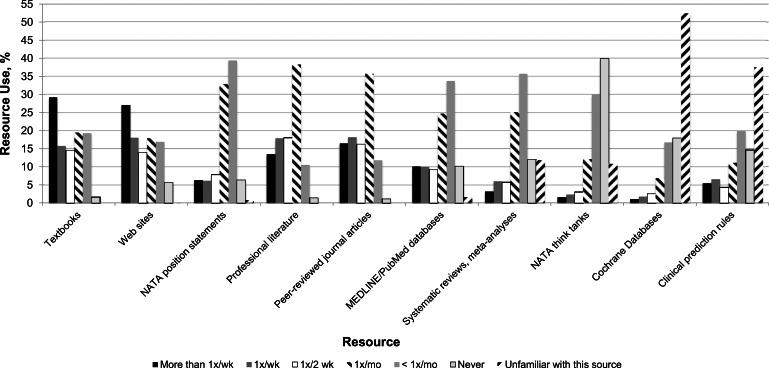
Resource Use.
Participants varied greatly in their use of several EBP-related resources (Figure 2). Textbooks (29.2%) and Web sites (27.1%) were the most frequently used resources at more than once per week. Professional literature (38.3%) and peer-reviewed journal articles (35.7%) were most often used once a month, whereas NATA position statements (39.4%), MEDLINE or PubMed databases (33.7%), and systematic reviews or meta-analyses (35.7%) were typically used less than once per month. Approximately 40% of participants never used NATA Think Tanks within their clinical practice or didactic education. Interestingly, Cochrane databases and clinical prediction rules were the 2 least familiar EBP-related resources; 37.6% of respondents were unfamiliar with clinical prediction rules, and 52.5% of respondents were unfamiliar with Cochrane databases.
Figure 2.
Resource use by all participants (n = 1209).
Perceived Barriers
Participants' responses to statements regarding barriers to implementing EBP within clinical practice were diverse. Postprofessional athletic training students (81.6%), clinical preceptors (83.0%), program directors (78.1%), and clinicians (74.4%) reported they agreed or strongly agreed that time was a barrier preventing EBP implementation within clinical practice or didactic education. Contrary to these results, 58.4% of postprofessional educators disagreed or strongly disagreed that time was a barrier for EBP implementation. With regard to the “availability of evidence-based practice mentors” as a barrier for EBP implementation, 78.0% of program directors, 70.8% of clinicians, and 70.3% of clinical preceptors agreed or strongly agreed. Thirty-eight percent of postprofessional educators and 50.7% of postprofessional students reported they disagreed or strongly disagreed.
Personal Skills and Attributes.
The composite score for personal skills and attribute barriers was 2.29 out of 4.0, indicating that participants reported they disagreed with the perceived barriers. A difference was found between groups in personal skills and attributes composite scores (H = 53.29, P < .001). Composite scores reported by postprofessional educators were lower than those of program directors (U = 717, z = −4.27, P < .001), clinical preceptors (U = 1072, z = −5.41, P < .001), clinicians (U = 2583, z = −5.85, P < .001), and postprofessional students (U = 389, z = −3.98, P < .001). Furthermore, postprofessional students had lower scores than did clinicians (U = 17 703, z = −4.24, P < .001) and clinical preceptors (U = 7263, z = −3.00, P = .003). Although program directors, clinical preceptors, postprofessional students, and clinicians disagreed that personal skills and attributes were barriers preventing EBP implementation, postprofessional educators strongly disagreed. The composite means and percentages for the personal skills and attributes items are shown in Table 3.
Individual group frequency analyses revealed that responses varied for 2 perceived barriers associated with personal skills and attributes. A total of 51% of clinical preceptors agreed that “understanding of the evidence-based practice process” was a barrier, whereas all other groups disagreed. Furthermore, both clinical preceptors (54.2%) and clinicians (57.0%) reported they agreed that understanding statistical analyses was a barrier to EBP implementation.
Support and Accessibility to Resources.
Overall, participants disagreed (2.40 out of 4.0) that support and accessibility to resources were barriers to EBP implementation. The groups differed with regard to support and accessibility to resources composite scores (H = 27.33, P < .001). Postprofessional educators' composite scores were lower than those of clinical preceptors (U = 1974, z = −3.12, P = .002) and clinicians (U = 5064, z = −3.45, P = .001). Additionally, postprofessional students also had lower scores than did clinicians (U = 18 954, z = −3.56, P < .001) and clinical preceptors (U = 7304, z = −2.95, P = .003). Composite means and percentages for the items associated with support and accessibility to resources barriers are provided in Table 4.
A few group frequency differences were noted for the support and accessibility to resources barriers. Postprofessional educators (54.2%) agreed or strongly agreed that the “ability to find research literature that related to my patient population” was a barrier, whereas program directors (57.6%), clinical preceptors (55.3%), and postprofessional students (59.1%) disagreed or strongly disagreed. Clinicians' responses to this barrier were even, with 50.3% of participants indicating they disagreed or strongly disagreed. For the “accessibility of patient outcome assessments” barrier, 70.9% of postprofessional educators and 59.1% of postprofessional students disagreed or strongly disagreed. Meanwhile, program directors (62.1%), clinical preceptors (59.4%), and clinicians (59.7%) agreed or strongly agreed that accessibility to patient outcome assessments was a barrier to EBP implementation.
DISCUSSION
The foundations of EBP have become recognized across various health care professions over the past decade. As EBP begins to transform athletic training education at the professional and postprofessional levels, it is also important to focus on the incorporation of EBP within clinical practice. If clinicians are unable to routinely administer effective patient care by balancing the best available evidence, clinician expertise, and patient values, the athletic training profession may continue to struggle to justify state legislation and third-party reimbursement. Identifying factors such as accessibility and perceived barriers to resources will allow administrators and facilitators to understand common concerns prohibiting athletic trainers from smoothly transitioning into evidence-based clinicians.
Attitudes and Beliefs
Our results indicate that athletic trainers have a relatively positive attitude toward the implementation of EBP and recognize that it provides benefits to clinical practice. Most of the participants in this investigation (98%) believed that applying EBP was important to the credibility of the profession. Furthermore, they agreed that EBP improves the quality of and helps clinicians make decisions about patient care. Similar results have been found in numerous investigations among physical therapists,7,21,22 dietitians,21 occupational therapists,21 nurses,23,24 and physicians.25–27 Our findings also indicate that 93.2% of participants believed they needed to increase their use of evidence within their daily clinical practices. These results are similar to those reported by Jette et al,7 in which 84% of physical therapists indicated they needed to increase their daily use of evidence.
Although athletic trainers believe EBP will improve patient care, some negative perceptions associated with implementation still remain. Similarly to those of Heiwe et al,21 our findings suggest that a majority of participants believed EBP did not take into account the limitations of their clinical practice settings. However, all groups disagreed that EBP placed unrealistic demands on daily practices. Contrary to our findings, Jette et al7 reported that 61% of physical therapists stated that EBP placed unrealistic demands on their clinical practices. Yet the literature is sparse regarding the patient populations for whom athletic trainers provide care. Therefore, athletic trainers may not perceive that EBP places unrealistic demands on daily practices because they believe no available evidence relates to their specific patient populations.
Bridges et al28 suggested that taking individual attitudes into consideration is crucial when intending to adopt EBP. Although the athletic training profession has already begun to implement EBP within didactic curricula and clinical practices, it is important to ensure that educators, students, and clinicians alike support these changes and are prepared with the appropriate tools and strategies for effective implementation. The results from this investigation match those performed on other health care professionals; athletic trainers support EBP and have positive attitudes regarding its implementation. Now that attitudes and beliefs toward EBP have been identified, it is essential to enhance athletic trainers' knowledge of EBP concepts, provide resources and tools for successful application, and eliminate barriers that prevent implementation.
Accessibility
Efficient access to resources and the skills to retrieve evidence are thought to be necessary for clinicians to appropriately implement EBP.7 The accessibility to EBP- related resources and use of these resources among athletic trainers varies greatly. Our results indicated that textbooks and Web sites (eg, Google Scholar, Wikipedia, WebMD) were the resources most frequently used on a weekly basis. Simultaneously, nearly all participants (98%) had direct access to textbooks and Web sites. Access to textbooks and Web sites may have been highest among the 10 resources assessed simply because they were the 2 types of resources with which the participants were most familiar. Sigouin and Jadad29 noted that 100% of oncologists used the Internet to access health information. Furthermore, 72% of nurses and 64% of physicians also retrieved health information via the Internet.29 However, our instrument only asked participants to identify if they were unfamiliar with a particular resource; therefore, we cannot make a conclusive statement regarding the familiarity of textbooks and Web sites.
A total of 92% of participants also had direct access to professional literature, which was most frequently used once a month. Heiwe et al21 used an EBP instrument developed by Jette et al7 and found that 93% of physical therapists, dietitians, and occupational therapists had access to professional literature in paper or Internet form. Similarly, Jette et al7 noted that 96% of physical therapists had access to professional journals; yet 74% of participants read fewer than 5 articles per month. Other authors30,31 investigating physical therapists' use of resources found that approximately 75% of respondents read their professional journal once or less than once per month. Although athletic trainers reported a high percentage of direct access to professional literature, they may not be using this resource frequently within their daily practices.
Direct access to NATA Think Tanks was available to 77% of athletic trainers, but 40% never used this resource. Our data do not provide us with further information as to why this resource is rarely used within clinical practice. The NATA Think Tanks were developed in 2008 and replaced the former athletic training listserves. This resource was conceived concurrently with the technological updates and changes made to the NATA Web site in 2008. The NATA Think Tanks are online discussion forums available to all NATA members. They are categorized by topic and setting to promote idea exchanges and peer-to-peer collaboration (forum.nata.org/thinktanks). By June 2011, only 2800 members had registered for the NATA Think Tanks. Even though this resource provides an excellent mechanism for collaborating with peers and mentors to share clinical experiences, NATA members underuse it. A balance among the best available research evidence, clinician expertise, and patient values is required for EBP,32 and the NATA Think Tanks may be an effective way to infuse clinician expertise into the EBP process.
Direct access to clinical prediction rules remained low across all 5 athletic training groups. Interestingly, 37.6% of participants were unfamiliar with this resource, which may have influenced the low level of response regarding direct access. Clinical prediction rules are decision-making tools that identify predictor variables (eg, patient history, physical examination, diagnostic tests) that assist clinicians in making a specific diagnosis, predicting a particular outcome, or determining an appropriate management strategy.33 Several clinical prediction rules have been developed to enhance clinicians' decision-making processes for a multitude of conditions (eg, diagnosis of deep vein thrombosis, strep throat, low back pain patients who will benefit from spinal manipulation). Other than through Internet searching, no central mechanism currently allows athletic trainers to access the clinical prediction rules that are published in various journals. Glynn and Weisbach34 have published Clinical Prediction Rules: A Physical Therapy Reference Manual, which includes several clinical prediction rules relevant to clinical practice.
Along with clinical prediction rules, athletic trainers also had limited access to Cochrane databases. More than half of the participants (52.5%) indicated they were unfamiliar with this resource. Similarly, McColl et al25 noted that fewer than 28% of physicians used resources such as the Cochrane databases. These databases, which are a part of the Cochrane Collaboration (www.thecochranelibrary.com), were developed in 1993 to emphasize the importance of current research and assist health care providers during the clinical decision-making process.35 To date, the Cochrane Collaboration36 contains more than 190 000 randomized controlled trials and 4500 systematic reviews. The Cochrane Collaboration is proclaimed to be the best and most thorough source for obtaining evidence for clinical practice.37 Currently, brief summaries are available for free on the Cochrane Library Web site; however, full access requires the purchase of a license. Institutions such as colleges and universities often purchase several licenses for faculty, administrators, and students to access the Cochrane Library. Free online access to the Cochrane databases may also be available through funded provisions.36 For example, all Wyoming residents can access the Cochrane Library for free via that state's public library databases. Yet smaller work settings, such as clinics, secondary schools, and athletic training facilities not affiliated with a college or university, may not have access to this resource unless a license is purchased.
Educating athletic trainers on the various mechanisms and search engines available to access high-quality research is an important step toward enhancing the use of EBP within daily clinical practice. As educators, students, and clinicians become more knowledgeable and familiar with the types of resources available to them, the level of resource use may increase as well. Increasing familiarity must be accompanied by improved access to such resources. Individuals who are not affiliated with academic institutions may not have the same access to resources such as the Cochrane Library, CINAHL, or MEDLINE. Therefore, policymakers and administrators should be encouraged to provide adequate access to resources that will promote current evidence and enhance clinical decision making.5,38
Barriers to Implementation
Interestingly, although athletic trainers had limited access to some EBP-related resources (eg, Cochrane databases, clinical prediction rules, systematic reviews and meta-analyses), not all groups perceived the accessibility of information resources as a barrier to implementation. These results are similar to those cited by Heiwe et al21: fewer than 15% of physical therapists, dietitians, and occupational therapists perceived lack of information resources as a barrier to implementation. Physicians often seek information from personal contacts rather than from the research literature that must be read and appraised.39 However, our data do not provide a reason as to why participants did not see accessibility of resources as a barrier to EBP implementation.
As we had expected, 76.6% of participants reported insufficient time as a barrier to implementation. Insufficient time has been reported as a barrier to EBP implementation across numerous research investigations.4,5,7,24,25,39 Although participants in this investigation reported time as a barrier, we are currently unaware of the specific factors that lead individuals to believe they do not have time to implement the EBP process. Each athletic training role carries different responsibilities; whether an individual is a student, educator, or clinician, athletic trainers are often asked to juggle multiple tasks simultaneously. Salbach et al22 observed that although 80% of physical therapists had Internet access, only 8% were provided time during working hours to search the literature for current evidence.
Even though time is most often cited as a perceived barrier among clinicians in various health care professions,4,5,7,24,25,39 insufficient time as a barrier to EBP implementation may be inflated because of other perceived barriers. The lack of time as a constraint may be more complex; clinicians often misinterpret mental time for physical time.40 Thompson et al40 suggested that mental time accounts for the cognitive processes necessary to understand, interpret, and apply research in clinical practice and that mental time may more accurately reflect clinicians' perceptions of insufficient time. Along with time constraints, other commonly reported barriers include lack of knowledge,4,5,7,9,24,25,39 confidence,7 generalizability of findings to a specific patient or population,7 and ability to interpret or appraise the research literature.7,25,39 Fairhurst and Huby39 found that physicians acknowledged the lack of skills necessary for critical appraisal. In a more recent investigation, Heiwe et al21 revealed lack of knowledge in statistics, lack of research skills, and poor ability to appraise research literature as major barriers to EBP implementation.
Most personal skills and attributes were not perceived as barriers in this investigation. However, clinicians and clinical preceptors reported understanding statistical analyses as a barrier. Furthermore, clinical preceptors also reported understanding of the EBP process as a barrier. Hankemeier and Van Lunen5 demonstrated similar findings in a qualitative investigation assessing perceived barriers clinical preceptors have to EBP. To overcome barriers relating to personal skills, it is imperative to acknowledge athletic trainers' knowledge levels of the foundational components relating to EBP.5 With an appreciation for this level of knowledge, future steps to educate athletic trainers on EBP concepts can be initiated.
Another commonly reported barrier involves personal support. Our participants disagreed that support from administration and colleagues in their facility was a barrier to implementing EBP. These findings are similar to those of previous researchers. Jette et al7 found that 67% of physical therapists felt that their facility supported the use of EBP, whereas Heiwe et al21 noted that fewer than 15% of participants indicated lack of support as a barrier to EBP implementation. In the past, physical therapists were shown to look to colleagues rather than the research literature as information resources.30,31,41,42 Additionally, Fairhurst and Huby39 suggested that physicians generally implement research only after a consensus that the evidence fits within the practice. Thus, the support from colleagues and administration may be important for athletic trainers as we shift toward EBP.
Finally, the relevance and applicability of research literature to patient populations has been reported as a barrier to EBP implementation. Postprofessional athletic training educators agreed that the ability to find research literature relevant to a specific population was a barrier, whereas professional athletic training program directors, clinicians, and clinical preceptors agreed that the accessibility of patient outcome assessments was a barrier. All 5 athletic training groups also perceived the application of research findings to individual patients with unique characteristics as a barrier. Other health care professionals have also reported these barriers.7,21,24,26 In addition, Young and Ward27 found that patient demands for a particular intervention, regardless of the evidence, were a barrier to implementation. Our results, similar to those of Heiwe et al,21 indicate that athletic trainers did not believe EBP takes into account patient preferences. However, the third tier of EBP is, in fact, patient preferences.32 In time, as the research literature continues to flourish and clinicians become more familiar with balancing evidence, clinician expertise, and patient preferences, this barrier may dissolve.
Limitations
Certain limitations may have affected the results of this investigation. Different sampling procedures were used while targeting the various groups within the athletic training profession. These methods may have automatically excluded some athletic trainers from participating. For example, although clinicians not affiliated with athletic training education programs were solicited for participation, those individuals working in a college, university, or secondary school setting were excluded to prevent potential crossover with the clinical preceptors solicited using different sampling procedures. Therefore, clinicians working in the college, university, or high school setting who were not affiliated with education programs may not be appropriately represented in this study. In particular, athletic trainers working in the secondary school setting may not have access to various EBP-related resources; data for this group of individuals will be important to gather in the future to ensure that effective EBP implementation strategies are developed.
Because of the lack of a gold standard for comparison, the validity of the EBCA may be questioned. To combat this issue, a panel of EBP and survey research experts who had several years each of experience as an athletic trainer assessed the instrument.19 However, without a gold standard for comparison, it is difficult to assess the true validity of the instrument.
CONCLUSIONS
Overall, athletic trainers had generally positive attitudes toward the implementation of EBP within clinical practices and didactic education. However, enhancing the accessibility of resources and eliminating the barriers to the implementation of EBP will take both time and patience. As the athletic training profession embraces EBP processes in clinical practice and didactic education, it will be important for individuals to be conscious of the personal barriers that prevent them from implementing EBP. Collaborative efforts and support among all members of the profession will be vital to the successful installation of modern-day EBP. Furthermore, it is important to develop and provide effective educational methods to enhance athletic trainers' and athletic training students' knowledge of the various components involved in EBP.
Athletic trainers have positive attitudes toward the implementation of EBP, so future researchers should identify mechanisms (eg, workshops, online modules, other educational resources) to enhance knowledge levels of the various EBP concepts as well as promote strategies for incorporating evidence into daily clinical practices. Although it is important for athletic trainers to have a solid understanding of the concepts associated with EBP, it is also critical to educate these individuals on the best ways to locate, appraise, and apply research literature in the clinical setting.
REFERENCES
- 1.National Athletic Trainers' Association. Athletic Training Education Competencies. 5th ed. Dallas, TX: NATA; 2011. pp. 1–32. [Google Scholar]
- 2.Welch CE, Van Lunen BL, Walker SE, et al. Athletic training educators' knowledge, comfort, and perceived importance of evidence-based practice. Athl Train Educ J. 2011;6(1):5–14. [Google Scholar]
- 3.Snyder AR. Valovich McLeod TC, Sauers E. Defining, valuing, and teaching clinical outcomes assessment in professional and post-professional athletic training education programs. Athl Train Educ J. 2007;2(2):31–41. [Google Scholar]
- 4.Manspeaker S, Van Lunen B. Overcoming barriers to implementation of evidence-based practice concepts in athletic training education: perceptions of select educators. J Athl Train. 2011;46(5):514–522. doi: 10.4085/1062-6050-46.5.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hankemeier DA, Van Lunen BL. Perceptions of approved clinical instructors: barriers in the implementation of evidence-based practice. J Athl Train. 2013;48(3):382–393. doi: 10.4085/1062-6050-48.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bidwell SR. Finding the evidence: resources and skills for locating information on clinical effectiveness. Singapore Med J. 2004;45(12):567–572. [PubMed] [Google Scholar]
- 7.Jette DU, Bacon K, Batty C et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003;83(9):786–805. [PubMed] [Google Scholar]
- 8.O'Donnell CA. Attitudes and knowledge of primary care professional towards evidence-based practice: a postal survey. J Eval Clin Pract. 2004;10(2):197–205. doi: 10.1111/j.1365-2753.2003.00458.x. [DOI] [PubMed] [Google Scholar]
- 9.Brown CE, Wickline MA, Ecoff L, Glaser D. Nursing practice, knowledge, attitudes and perceived barriers to evidence-based practice at an academic medical center. J Adv Nurs. 2009;65(2):371–381. doi: 10.1111/j.1365-2648.2008.04878.x. [DOI] [PubMed] [Google Scholar]
- 10.Fritsche L. Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002;325(7376):1338–1341. doi: 10.1136/bmj.325.7376.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nicholson LJ, Warde CM, Boker JR. Faculty training in evidence-based medicine: improving evidence acquisition and critical appraisal. J Contin Educ Health Prof. 2007;27(1):28–33. doi: 10.1002/chp.90. [DOI] [PubMed] [Google Scholar]
- 12.Cullen L, Titler MG, Rempel G. An advanced educational program promoting evidence-based practice. West J Nurs Res. 2011;33(3):345–364. doi: 10.1177/0193945910379218. [DOI] [PubMed] [Google Scholar]
- 13.Davis J, Chryssafidou E, Zamora J, Davies D, Khan K, Coomarasamy A. Computer-based teaching is as good as face to face lecture-based teaching of evidence based medicine: a randomised controlled trial. BMC Med Educ. 2007;7(23):1–6. doi: 10.1186/1472-6920-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitto S, Villanueva EV, Chesters J, Petrovic A, Waxman BP, Smither JA. Surgeons' attitudes towards and usage of evidence-based medicine in surgical practice: a pilot study. ANZ J Surg. 2007;77(4):231–236. doi: 10.1111/j.1445-2197.2007.04022.x. [DOI] [PubMed] [Google Scholar]
- 15.Mensik JS. Understanding research and evidence-based practice: from knowledge generation to translation. J Infus Nurs. 2011;34(3):174–178. doi: 10.1097/NAN.0b013e3182134f44. [DOI] [PubMed] [Google Scholar]
- 16.Manspeaker SA, Van Lunen BL. Implementation of evidence-based practice concepts in undergraduate athletic training education: experiences of select educators. Athl Train Educ J. 2010;5(2):51–60. doi: 10.4085/1062-6050-46.5.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hankemeier DA, Van Lunen BL. Approved clinical instructors' perspectives on evidence-based practice implementation strategies for students. J Athl Train. 2011;46(6):655–664. doi: 10.4085/1062-6050-46.6.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manspeaker SA, Van Lunen BL, Turocy P, Pribesh S, Hankemeier DA. Student knowledge, attitudes and use of evidence-based concepts following an educational intervention. Athl Train Educ J. 2011;6(2):88–98. [Google Scholar]
- 19.Hankemeier DA, Walter JM, McCarty CW, Newton EJ, Walker SE, Pribesh SL, Jamali BE, Manspeaker SA, Van Lunen BL. Use of evidence-based practice among athletic training educators, clinicians, and students, part 1: perceived importance, knowledge, and confidence. J Athl Train. 2013;48(3):394–404. doi: 10.4085/1062-6050-48.2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramos K. Validation of the Fresno test of competence in evidence based medicine. BMJ. 2003;326(7384):319–321. doi: 10.1136/bmj.326.7384.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heiwe S, Kajermo KN, Tyni-Lenne R et al. Evidence-based practice: attitudes, knowledge and behavior among allied health care professionals. Int J Qual Health Care. 2011;23(2):198–209. doi: 10.1093/intqhc/mzq083. [DOI] [PubMed] [Google Scholar]
- 22.Salbach NM, Jaglal SB, Korner-Bitensky N, Rappolt S, Practitioner Davis D. and organizational barriers to evidence-based practice of physical therapists for people with stroke. Phys Ther. 2007;87(10):1284–1303. doi: 10.2522/ptj.20070040. [DOI] [PubMed] [Google Scholar]
- 23.Waters D, Crisp J, Rychetnik L, Barratt A. The Australian experience of nurses' preparedness for evidence-based practice. J Nurs Manag. 2009;17(4):510–518. doi: 10.1111/j.1365-2834.2009.00997.x. [DOI] [PubMed] [Google Scholar]
- 24.Retsas A. Barriers to using research evidence in nursing practice. J Adv Nurs. 2000;31(3):599–606. doi: 10.1046/j.1365-2648.2000.01315.x. [DOI] [PubMed] [Google Scholar]
- 25.McColl A, Smith H, White P, Field J. General practitioner's perceptions of the route to evidence based medicine: a questionnaire survey. BMJ. 1998;316(7128):361–365. doi: 10.1136/bmj.316.7128.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flores G, Lee M, Bauchner H, Kastner B. Pediatricians' attitudes, beliefs, and practices regarding clinical practice guidelines: a national survey. Pediatrics. 2000;105((3 pt 1)):496–501. doi: 10.1542/peds.105.3.496. [DOI] [PubMed] [Google Scholar]
- 27.Young JM, Ward JE. Evidence-based medicine in general practice: beliefs and barriers among Australian GPs. J Eval Clin Pract. 2001;7(2):201–210. doi: 10.1046/j.1365-2753.2001.00294.x. [DOI] [PubMed] [Google Scholar]
- 28.Bridges PH, Bierema LL, Valentine T. The propensity to adopt evidence-based practice among physical therapists. BMC Health Serv Res. 2007;7:103. doi: 10.1186/1472-6963-7-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sigouin C, Jadad AR. Awareness of sources of peer-reviewed research evidence on the Internet. JAMA. 2002;287(21):2867–2869. doi: 10.1001/jama.287.21.2867. [DOI] [PubMed] [Google Scholar]
- 30.Turner PA, Whitfield TWA. Journal readership amongst Australian physiotherapists: a cross-national replication. Aust J Physiother. 1997;43(3):197–202. doi: 10.1016/s0004-9514(14)60410-4. [DOI] [PubMed] [Google Scholar]
- 31.Turner PA, Whitfield TWA. A multivariate analysis of physiotherapy clinicians' journal readership. Physiother Theory Pract. 1996;12(4):221–230. [Google Scholar]
- 32.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Childs JD, Cleland JA. Development and application of clinical prediction rules to improve decision making in physical therapist practice. Phys Ther. 2006;86(1):122–131. doi: 10.1093/ptj/86.1.122. [DOI] [PubMed] [Google Scholar]
- 34.Glynn PE, Weisbach PC. Clinical Prediction Rules: A Physical Therapy Reference Manual. Sudbury, MA: Jones and Bartlett;; 2011. [Google Scholar]
- 35.Fineoutoverholt E, Melnyk B, Schultz A. Transforming health care from the inside out: advancing evidence-based practice in the 21st century. J Prof Nurs. 2005;21(6):335–344. doi: 10.1016/j.profnurs.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 36.The Cochrane Collaboration Web site. http://www.cochrane.org/. Published 2010. Accessed May 17, 2011. [Google Scholar]
- 37.Bigby M. Evidence-based medicine in a nutshell: a guide to finding and using the best evidence in caring for patients. Arch Dermatol. 1998;134(12):1609–1618. doi: 10.1001/archderm.134.12.1609. [DOI] [PubMed] [Google Scholar]
- 38.Farmer J, Richardson A. Information for trained nurses in remote areas: do electronically networked systems provide the answer? Health Libr Rev. 1997;14(2):97–103. [PubMed] [Google Scholar]
- 39.Fairhurst K, Huby G. From trial data to practice knowledge: qualitative study of how general practitioners have accessed and used evidence about statin drugs in their management of hypercholesterolaemia. BMJ. 1998;317(7166):1130–1134. doi: 10.1136/bmj.317.7166.1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson DS, O'Leary K, Jensen E, Scott-Findlay S, O'Brien-Pallas L, Estabrooks CA. The relationship between busyness and research utilization: it is about time. J Clin Nurs. 2008;17(4):539–548. doi: 10.1111/j.1365-2702.2007.01981.x. [DOI] [PubMed] [Google Scholar]
- 41.Carr JH, Mungovan SF, Shepard RB et al. Physiotherapy in stroke rehabilitation: bases for Australian physiotherapists' choice of treatment. Physiother Theory Pract. 1994;10(4):201–209. [Google Scholar]
- 42.Bohannon RW. Information accessing behavior of physical therapists. Physiother Theory Pract. 1990;6(4):215–225. [Google Scholar]