Abstract
Objective
Personality change is emerging as an important predictor of health and well-being. Extending previous research, we examined whether two types of personality change, directional and absolute, are associated with both subjective and objective indicators of health.
Method
Utilizing the longitudinal Midlife in the United States Survey (MIDUS) data, we examined whether both types of change over 10 years were associated with psychological well-being, self-reported global health, and the presence of metabolic syndrome (MetS) components and diagnosis.
Results
Socially undesirable personality change (e.g., becoming less conscientious and more neurotic) and absolute personality change were independently associated with worse perceived health and well-being at Time 2. Notably, absolute personality change, regardless of the direction, was also associated with having a greater number of MetS components and a greater probability of diagnosis at Time 2.
Conclusions
In sum, too much personality change may be bad for one’s health: socially undesirable and absolute personality change were both associated with worse psychological health and worse metabolic profiles over 10 years. These findings suggest that personality change may contribute to psychological and physical health, and provide initial insight into potential intermediate links between personality change and distal outcomes such as mortality.
Keywords: Personality change, the metabolic syndrome, psychological well-being, self-reported health
Personality traits predict important health and life outcomes (Roberts, Kuncel, Shiner, Caspi, & Goldberg, 2007; Smith, 2006), and personality change is emerging as another important predictor of physical health (see Roberts & Mroczek, 2008). Although personality is generally quite stable, personality changes do occur throughout the life span (Caspi, Roberts, & Shiner, 2005). These changes can be a part of natural personality development, in response to life events, or perhaps due to a general tendency to be more labile. Although the bulk of normative, developmental change occurs in young adulthood, personality change continues to take place later in life (Roberts & DelVecchio, 2000) and there are individual differences in how much people change (Roberts & Mroczek, 2008); could such change have implications for health and well-being?
Recent research suggests that personality change, in addition to mean levels on personality traits, is indeed associated with physical health. For example, becoming less agreeable, conscientious, and extraverted is associated with lower self-reported health (Turiano et al., 2011).i Further, men who become more neurotic over time have a higher risk of mortality over 18 years (Mroczek & Spiro, 2007). However, no research to date has linked personality change to more proximal, objectively measured health indicators, which might provide insight into the biological mechanisms linking personality change and mortality. Thus, utilizing a national sample of adults from the Midlife in the United States Survey (MIDUS), the current study sought to fill this gap by examining whether personality change (on the Big 5 traits plus agency) over 10 years is associated with an objective, proximal indicator of midlife health problems, the metabolic syndrome (MetS), as well as subjective health and well-being indicators.
MetS is a prevalent syndrome, affecting an estimated 25 – 39% of Americans, reflecting a sedentary lifestyle and overnutrition (Cornier et al., 2008). Specifically, MetS involves a cluster of symptoms including abdominal adiposity, high blood pressure, problematic glucose control, and lipid dysregulation. It is an important health indicator to examine given that it is a precursor to multiple chronic diseases, including cardiovascular disease (Cornier et al., 2008). Furthermore, MetS is prospectively predicted by depression (e.g., Goldbacher, Bromberger, & Matthews, 2009) and general psychological distress (Puustinen, Koponen, Kautiainen, Mantyselka, & Vanhala, 2011), indicating that psychosocial factors may play a role in its development. Personality change may be one of these psychosocial factors. MetS is associated with a wide variety of personality traits, including hostility (Elovainio et al., 2011), neuroticism (Phillips et al., 2010; Sutin et al., 2010), low agreeableness and conscientiousness (Sutin et al., 2010), and low openness (van Reedt Dortland, Giltay, van Veen, Zitman, & Penninx, 2012). It is possible that changes to personality on a variety of traits might also be associated with MetS, potentially providing insight into why personality change is linked to mortality, as well as identifying an additional risk factor for this problematic syndrome.
Why might changes to personality be associated with psychological and physiological functioning? Given that personality traits are associated with a variety of health-relevant behaviors (Adler & Matthews, 1994; Bogg & Roberts, 2004; Hampson, Goldberg, Vogt, & Dubanoski, 2007), it is plausible that changes in personality could impact these behaviors, in turn putting individuals at risk for physical health problems (Siegler et al., 2003). For example, low conscientiousness is associated with drug use, poor diet, less exercise, and risky sexual behaviors (see Bogg & Roberts, 2004, for review). Similarly, becoming more hostile over time predicts engaging in less exercise and an unhealthy diet (Siegler et al., 2003). Further, the pessimism and anxiety that go along with neuroticism are associated with greater substance abuse and worse medical adherence (Friedman, 2000). Indeed, smoking behavior does partially explain the association between an increase in neuroticism and mortality (Mroczek, Spiro, & Turiano, 2009). Thus, based on these results it appears that change in a socially undesirable direction (e.g., becoming more neurotic, less conscientious, less agreeable, and possibly less extraverted, open, and agentic) could lead to increases in negative health-relevant behaviors, in turn impacting the cluster of components related to MetS, such as high blood pressure and central adiposity.
Socially undesirable personality change may also result in greater exposure and reactivity to social difficulties. For instance, greater anxiety and lower agreeableness could lead to more negative interpersonal interactions, enhancing exposure to social stressors. Indeed, increases in hostility are associated with increases social isolation and family life difficulties (Siegler et al., 2003). Further, socially undesirable changes on each of the Big 5 personality traits are associated with concurrent reductions in social well-being (Hill, Turiano, Mrozcek, & Roberts, 2011). Aspects of neuroticism and agreeableness (specifically, anxiety and hostility) are also associated with a chronically elevated stress response (Friedman, 2000). In turn, frequent exposure and strong reactivity to social stressors have negative implications for a variety of cardiovascular, endocrine, and immunologic processes relevant to MetS (Miller, Chen, & Cole, 2009). Thus, socially undesirable personality change could result in a risky pattern of managing acute stress, putting individuals who experience socially undesirable personality change on a negative trajectory for a variety of MetS processes.
It may be too simplistic, however, to say that change in a socially undesirable direction is uniformly bad (e.g., Kern & Friedman, 2011). For instance, despite the evidence that neuroticism predicts worse health behaviors and mortality, there is also evidence for a protective effect of neuroticism, particularly for men (e.g., Korten et al., 1999; Taga, Friedman & Martin, 2009). It is also possible that socially desirable change on some traits could have negative implications for health and well-being. For example, increased extraversion could lead one to be in more social situations involving alcohol and risky sexual behaviors (e.g., Vollrath, Knoch, & Cassano, 1999). Finally, although most traits do generally have a more and less socially desirable pole (Edwards, 1957; John & Robins, 1993), there may be exceptions depending social, gender, or cultural role. Thus, it remains an empirical question as to whether what might usually be considered undesirable change is indeed associated with poorer physical and psychological functioning.
Another possibility is that the direction of change may not always matter – instead, any personality change, both desirable and undesirable, may negatively impact one’s health and well-being. Given the central, organizing role that personality plays, a change in personality – even if it is ultimately positive – may be a subjectively and physiologically stressful experience. A coherent, strong sense of self is thought to be a psychological coping resource for dealing with stressors and life changes as people age (Brandtstädter & Greve, 1994). Thus, a change to one’s personality could weaken one’s sense of sense of self, and therefore have ramifications for one’s coping resources. Indeed, there is evidence that absolute personality change in neuroticism, conscientiousness, and openness are associated with greater cognitive decline (Graham & Lachman, 2012). Further, greater variability in the individual difference of perceived control over a short-term period predicts a higher risk of mortality five years later (Eizenman, Nesselroade, Featherman, & Rowe, 1997). Perceived control refers to believing that outcomes are contingent upon one’s own actions, as well as that one has the ability to bring about the desired outcomes (e.g., Eizenman et al., 1997). Such a tendency is likely to be related to the personality trait of agency, which reflects a sense of and striving towards mastery and power (Wiggins, 1991). That is, a person who generally experiences a sense of mastery or power in their social environment is likely to believe that they do and are able to bring about desired outcomes. In sum, it is possible that absolute change in the Big 5 personality traits plus agency also has implications for subjective and objective health.
Thus, both the direction and absolute amount of personality change may be associated with subjective and objective health indicators. We examined both types of change on average across all personality traits combined together (as a general index of broad personality change), as well as change on each personality trait separately. Examining personality change at a broad level, on average across all traits, is a more holistic, parsimonious, and reliable approach than looking at trait specific changes. Specifically, examining broad change is a person-centered approach that explores whether people who generally change more (in a given direction or at all) experience lower well-being and exhibit more symptoms of MetS. This provides more reliable estimates of change than the estimates of change for a given trait because it averages across a greater number of items than are available for any given trait. Nevertheless, this approach also loses the specificity of trait-specific change scores, which are also important to explore given that change on different traits may have differing associations with health and well-being indicators. As such, utilizing the longitudinal MIDUS sample, we examined how both directional and absolute change, broadly across traits as well as on each of the Big 5 traits plus agency, are associated with MetS components and diagnosis, as well as subjective global health and psychological well-being.
Method
Participants
The participants were drawn from the Midlife in the United States Survey (MIDUS). A total of 7108 adults completed the first wave of the MIDUS study in 1994–1995, with 4968 completing the second wave in 2004–2005, a response rate of 75% within the surviving sample. At enrollment, participants ranged in age from 20 to 75 (M = 46.46, SD = 12.51). A subset of these participants also participated in a biological assessment at Time 2 (N = 1044), done during an overnight visit to a General Clinical Research Center (GCRC). This subset had higher educational attainment than the overall MIDUS II sample, but was otherwise similar on demographic and biomedical characteristics (see Dienberg Love, Seeman, Weinstein, & Ryff, 2010). However, due to missing data on the Time 2 personality and subjective health or well-being measures, the number of participants that we were able to include in our analyses of self-reported health and well-being ranged from 3816 to 3853, while the total number of participants in our metabolic syndrome analyses was 996.ii
Personality
Personality traits at Time 1 and Time 2 were assessed with the Midlife Development Inventory (MIDI; Lachman & Weaver, 1997), which includes 30 adjectives that map on to each of the Big 5 personality traits, namely extraversion, neuroticism, conscientiousness, agreeableness, and openness, plus agency (Mean α at T1 = .74; Mean α at T2 = .73), all assessed on a 1 (a lot) – 4 (not at all) scale (for additional scale details see Graham & Lachman, 2012; Prenda & Lachman, 2001; Turiano et al., 2012; Zimprich, Allemand, & Lachman, 2011). Prior to analyses, all items were coded such that higher scores reflected higher endorsement on each item in what previous research would suggest is the more socially desirable direction (high extraversion, conscientiousness, agreeableness, openness, agency, and low neuroticism; John & Robins, 1983). However, neuroticism was not reversed scored for the trait-specific analyses.
As reported in Turiano et al., the test-retest reliabilities from Time 1 to Time 2 were quite high (range: .61 – .71), demonstrating considerable stability in personality over time at levels similar to those found in prior studies with similar age groups (e.g., Roberts & DelVecchio, 2000). The critical question, however, will be whether individual differences in change are associated with subjective health and well-being and the MetS.
Assessing Change
As there were only two time points (therefore making more sophisticated techniques for modeling change unfeasible), personality change was indexed with difference scores. Difference scores have recently regained popularity as an index of change when only two time points are available (e.g., Graham & Lachman, 2012; Turiano et al., 2012) because they are an easily interpretable and reliable method when individual differences in change are expected (see Rogosa & Willett, 1983). Change scores were calculated both holistically across all 30 personality items (to provide a broad, more reliable indicator of overall personality change) and for each trait separately (so that trait-specific effects could be examined). An overall directional personality change score was calculated by first subtracting each Time 1 personality item from its corresponding Time 2 personality item. Given that each item was coded such that higher scores reflected a more socially desirable standing on that item, a higher directional change score would therefore reflect increasing on a given item in a more socially desirable direction. We then calculated the overall directional personality change score by averaging these difference scores for each of the 30 personality items (M = −.04, SD = .28; Range: −1.38 – 1.30; α = .77). Thus, this change score takes direction into account such that positive values on this variable reflect an overall shift in the more socially desirable direction on average across items (e.g., becoming more conscientious and less neurotic), while negative values reflect change in the socially undesirable direction on average across items (e.g., becoming less conscientious and more neurotic). Note that if a person was to change in a more positive direction on some items (e.g., become much more conscientious), but simultaneously change in a more negative direction on other items (e.g., they also became much more neurotic), they would receive a low directional change score because, despite these changes, the average level of desirability of their personality profile has remained quite constant. Thus, this index of change captures the overall direction and therefore desirability of change, rather than the total amount of change. This procedure was then repeated for each trait to create trait-specific directional change scores (range αs = .33 – .62).
If it is the total amount of personality change, rather than the direction of change, that is associated with indicators of health and well-being, directional personality change will show a symmetric curvilinear association with outcome variables. Thus, we also examined whether directional change has nonlinear associations with these outcomes. However, to better capture total rather than directional change, we also examined absolute personality change by taking the mean absolute difference score across the 30 personality items (α = .69), as well as for each trait (range αs = .28 – .51), thereby disregarding the direction of change. Although this indicator of change is certainly related to quadratic directional change, they are not completely isomorphic. For example, a person could increase in conscientiousness and neuroticism by one unit each and therefore receive a directional change score of 0 (and therefore quadratic change would also be 0). However, absolute change scores would capture this change, with the person receiving a change score of 1, because on average across these two traits they changed by 1 unit.
Absolute personality change is bounded at the lower end at zero and larger positive values reflect greater total change, in either a positive or negative direction (Mean = .46; SD = .18; Range: 0 – 1.53).iii Because directional change is a component of absolute change, we also controlled for the influence of directional change where applicable. Examining these two types of personality change gives us insight into the potentially differing associations of the direction of change versus total change with the metabolic syndrome and perceived health and well-being.
Self-Reported Health and Well-being
Self-reported health was assessed at both time points on a single item, “How would you rate your health these days”, on a 0 (worst possible health) to 10 (best possible health) scale (Time 2 Mean = 7.37; SD = 1.60). General well-being was assessed at Time 1 and Time 2 with a single overall satisfaction with life item (Prenda & Lachman, 2001), in which participants were asked, “How would you rate your life overall these days”, on a 0 (worst possible life overall) to 10 (best possible life overall) scale (Time 2 Mean = 7.76; SD = 1.25). Additional aspects of well-being were assessed at both time points with the short form of the Psychological Well-being Scale (Ryff & Keyes, 1995), with three items for each of the six positively correlated subscales: autonomy, personal growth, environmental mastery, purpose in life, positive relations with others, and self-acceptance. Ratings on each item were made on a 1 (agree strongly) to 7 (disagree strongly) scale. Given the direction of this rating scale, positive items were reversed coded so that higher scores indicate greater levels of well-being. Subscales were then calculated as the sum of each of the three corresponding items. Because of the low reliabilities of the individual subscales (range αs: .36 – .59), a composite psychological well-being indicator was examined (Time 2 Mean = 16.63; SD = 2.43; α = .80), in line with other empirical studies (e.g., Sherman, Nave, & Funder, 2012). The self-reported well-being and health measures showed moderate stability from Time 1 to Time 2, mean r = .56 (range: .51 – .62), all ps < .001.
The Metabolic Syndrome
The MetS was assessed at Time 2 as part of GCRC visits. Following the International Diabetes Federation (IDF) definition of MetS (Cornier et al., 2008), to be diagnosed an individual must first show central adiposity, defined by ethnic and gender-specific cutoffs for waist circumference, which are ≥ 94 and ≥ 80 cm for men and women, respectively, for those of European and African descent, who make up the majority of the MIDUS sample. iv An additional 2 of the following 4 components must also be present: 1) high blood pressure, defined as ≥ 130 systolic or ≥ 85 diastolic or treatment of previously diagnosed hypertension, 2) heightened triglycerides, defined as ≥ 150 mg/dl, or specific treatment for this lipid abnormality, 3) high fasting glucose, defined as ≥ 100 mg/dl, or previous diagnosis of diabetes and d) low high-density lipoprotein levels, defined as ≤ 40 and ≤ 50 mg/dl for men and women, respectively, or specific treatment for this lipid abnormality. Note that we did not have detailed medication use information, but participants did report whether they were on medication for hypertension, cholesterol, and diabetes, as well as whether they had been previously diagnosed with diabetes. In line with the IDF definition, this information was integrated into our definition such that being on medication for hypertension counted towards the criteria for high blood pressure, being on medication for cholesterol counted towards the criteria for heightened triglycerides and low high-density lipoprotein levels, and being on medication for diabetes or being diagnosed with diabetes counted towards the criteria for high fasting glucose. Because of the lack of specificity in the medication data, we also defined MetS based on lab-test criteria alone. This approach had no material impact on the results that follow.
Waist circumference was taken at the narrowest point between the ribs and iliac crest. Resting blood pressure was measured three times while seated, in between 30-second intervals. For the following analyses, the two most similar readings were averaged. A lipid panel and blood glucose were taken from fasting morning blood samples with automated instruments from Roche Diagnostics, Indianapolis, IN.
We examined two MetS variables: first, a MetS components variable, which was the overall number of the MetS components described above for which a participant met clinical cutoffs (range: 0 – 5). A MetS diagnosis variable was also created, which was a binary variable indicating whether the participant met the IDF definition for MetS as outlined above (0 = not diagnosed, 1 = diagnosed; see Miller et al., 2011).
Covariates
For all analyses, age at Time 2 (centered) and gender (effect coded: −1 for men, 1 for women) were controlled for. We also controlled for standing on Time 2 personality traits, because personality at Time 2 is a strong predictor of Time 2 subjective health and well-being (see Online Supplemental Table for associations among Time 1 and Time 2 personality traits and these variables). For the subjective health and well-being analyses, we also controlled for the corresponding Time 1 subjective health and well-being variable, thereby assessing change in subjective health and well-being since Time 1.v For all analyses involving the MetS outcome variables, additional demographic and biobehavioral variables were included as covariates, including race (coded as dummy variables reflecting European or African-American descent), current socioeconomic status at Time 2, indexed as a four-level education indicator ranging from “less than a high school diploma” to “a bachelor’s degree from a four-year institution (or more)”, and binary variables that reflected current smoking status and history of cardiovascular disease (CVD), both at Time 2.vi For MetS analyses, we also included Time 1 self-reported health as a covariate as an attempt to control for health at Time 1, given that Time 1 biological data were not available. Considering that self-reported health at Time 2 was significantly correlated with the number of MetS components at Time 2, r = −.22, p < .001, it seems likely that Time 1 self-reported health would at least partially capture one’s metabolic health at Time 1.
Results
Well-being & Self-reported Health
Overall Personality Change
To examine whether overall personality change was associated with changes in self-reports of health and well-being, we ran a series of multiple regressions predicting Time 2 satisfaction with life, psychological well-being, and self-reported health from overall personality change, controlling for the covariates outlined above.
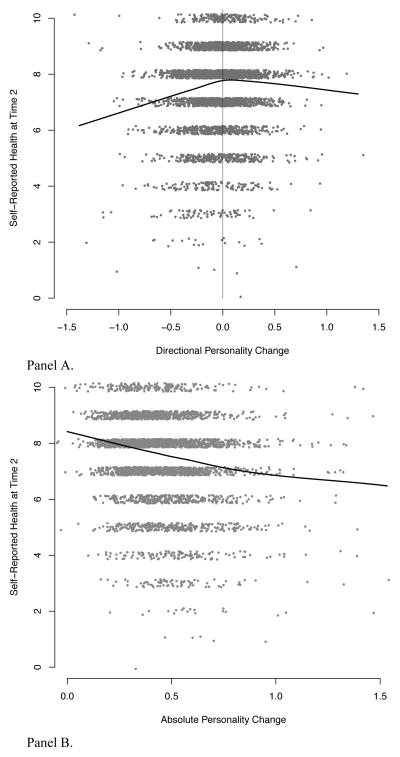
Directional Change
Overall directional personality change was significantly linearly associated with change on each of the Time 2 subjective health and well-being outcomes, all |ts| > 5.63 (see Table 1). However, there were also significantly negative quadratic associations with all of the self-reported well-being and health measures, all |ts| > 3.98. As illustrated in Figure 1A, which presents the simple bivariate relationship between directional personality change and self-reported health, the association between directional change is strongest for personality change in what would typically be considered the more undesirable direction. That is, individuals who report more negative personality change (e.g., increasing neuroticism, decreasing conscientiousness) also report worse health and well-being at Time 2, relative to Time 1. In contrast, personality change in a more positive direction (i.e., personality change scores above 0) does not appear to be associated with enhanced levels of well-being or self-reported health. That is, the associations between directional change and subjective health and well-being level off at the more desirable pole of personality change. Furthermore, there was a significant negative interaction between age and directional change predicting psychological well-being, such that change in the socially desirable direction was actually associated with lower well-being for older adults (see the Online Supplemental Appendix for details). There were no significant interactions with gender.
Table 1.
Overall and trait-specific personality change predicting self-reported well-being and health at Time 2.
| Personality Change | Satisfaction with Life | Psychological Well-Being | Self-Reported Health | |||
|---|---|---|---|---|---|---|
|
| ||||||
| b (SE) | β | b (SE) | β | b (SE) | β | |
| Overall | ||||||
| Directional | .41*** (.064) | .18 | 1.03*** (.115) | .23 | .48*** (.085) | .17 |
| Absolute | −.44*** (.090) | −.13 | −.90*** (.151) | −.14 | −.60*** (.121) | −.14 |
| Neuroticism | ||||||
| Directional | −.10*** (.032) | −.09 | −.23*** (.055) | −.10 | −.07 (.042) | −.05 |
| Absolute | .00 (.013) | .00 | −.09 (.071) | −.03 | −.06 (.056) | −.03 |
| Conscientiousness | ||||||
| Directional | .08† (.047) | .05 | .24** (.080) | .08 | .12* (.063) | .06 |
| Absolute | −.11† (.060) | −.05 | −.11 (.101) | −.03 | −.15† (.081) | −.05 |
| Agreeableness | ||||||
| Directional | .11** (.042) | .08 | .28*** (.072) | .10 | .10† (.057) | .05 |
| Absolute | −.04 (.055) | −.02 | −.25** (.093) | −.06 | .02 (.015) | .01 |
| Extraversion | ||||||
| Directional | .23*** (.040) | .16 | .54*** (.068) | .20 | .36*** (.053) | .20 |
| Absolute | −.30*** (.054) | −.14 | −.24** (.091) | −.06 | −.31*** (.073) | −.11 |
| Openness | ||||||
| Directional | .20*** (.042) | .13 | .37*** (.072) | .13 | .20*** (.057) | .10 |
| Absolute | −.21*** (.057) | −.09 | −.51*** (.096) | −.12 | −.30*** (.077) | −.11 |
| Agency | ||||||
| Directional | .13*** (.034) | .11 | .33*** (.057) | .14 | .19*** (.045) | .12 |
| Absolute | −.25*** (.047) | −.14 | −.33*** (.079) | −.09 | −.20** (.064) | −.08 |
Note. N Range: 3816 – 3853. SE = standard error. All analyses controlled for the corresponding Time 1 well-being and health scores, gender, age, and all T2 personality traits. Standardized regression coefficients, βs, were calculated as the predicted change in the dependent variable, in standard deviations, for a 2-SD change in the respective personality change score (see Gelman, 2008).
p < .10,
p < .05,
p < .01,
p <.001.
Figure 1.
Directional (Panel A) and absolute (Panel B) personality change predicting self-reported health at Time 2. Data are slightly jittered (randomly perturbed) to minimize overplotting and the nonparametric loess curve is plotted.
Absolute Change
Absolute personality change was also significantly associated with lower psychological well-being and perceived physical health for all indicators, all |ts| > 4.96 (see Table 2 and Figures 1B). Interestingly, this effect was not solely due to the socially desirable component of the absolute change score: when controlling for directional change, absolute change continued to significantly predict lower self-reported health and well-being, all |ts| > 2.70. Thus, experiencing greater personality change, even when it does not affect the overall desirability of one’s personality profile, is associated with worse perceived health and well-being. On the whole, these results demonstrate that, above and beyond mean personality trait levels, and controlling for age and gender, both socially undesirable change and greater absolute change are independently associated with negative changes in perceived health and well-being.
Table 2.
Overall personality change and covariates predicting MetS components at Time 2.
| Predictor | Descriptives | MetS Components | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean | SD | Directional Change | Absolute Change | |||
|
| ||||||
| b (SE) | β | b (SE) | β | |||
| Personality Change | See text | −.03 (.176) | −.01 | .66** (.255) | .17 | |
| Age | 55.43 | 12.45 | .01** (.004) | .20 | .01** (.004) | .23 |
| Education | 3.19 | .88 | −.24*** (.050) | −.30 | −.22*** (.050) | −.28 |
| T1 Self-reported Health | 7.66 | 1.41 | −.17*** (.031) | −.34 | −.16*** (.031) | −.32 |
| Female (%) | 57.36 | — | −.32*** (.044) | −.22 | −.32*** (.044) | −.23 |
| Black (%) | 2.59 | — | −.02 (.334) | −.01 | −.07 (.334) | −.01 |
| White (%) | 92.82 | — | −.05 (.205) | −.01 | −.07 (.204) | −.01 |
| Current Smoker (%) | 10.54 | — | .03 (.139) | .01 | −.06 (.139) | −.01 |
| History of CVD (%) | 14.75 | — | .13 (.123) | .00 | .11 (.123) | .03 |
| T2 Neuroticism | 2.07 | .63 | −.14† (.072) | −.13 | −.15* (.072) | −.13 |
| T2 Conscientiousness | 3.46 | .45 | −.25* (.104) | −.16 | −.23* (.104) | −.14 |
| T2 Agency | 2.61 | .66 | .22** (.083) | .21 | .22** (.082) | .22 |
| T2 Extraversion | 3.11 | .57 | −.28** (.106) | −.23 | −.25* (.106) | −.20 |
| T2 Agreeableness | 3.45 | .50 | .34** (.106) | .25 | .36*** (.104) | .26 |
| T2 Openness | 2.90 | .54 | −.02 (.103) | −.02 | .00 (.103) | −.00 |
Note. N = 996. SD = Standard deviation; SE = Standard error; MetS = Metabolic Syndrome; CVD = Cardiovascular disease. Standardized regression coefficients, βs, for continuous predictors were calculated as the predicted change in the dependent variable, in standard deviations, for a 2-SD change in the predictor variable (see Gelman, 2008).
p < .05,
p < .01,
p <.001.
Trait-Specific Personality Change
Is change on individual traits also associated with self-reported health and well-being? Yes, in general, linear directional personality change and absolute personality change on each individual trait were also associated with lower self-reported health and well-being (see Table 1), although the effects were the strongest and most consistent for extraversion, openness, and agency. Overall, it appears that general personality change, rather than change on a specific trait, is associated with changes in subjective health and well-being. Further, the consistency of the direction of these directional change effects lends support to our categorization of the social desirability of each trait: in each case, greater change in the proposed undesirable direction was indeed more strongly associated with worse self-reported health and well-being.
Metabolic Syndrome
Overall Personality Change
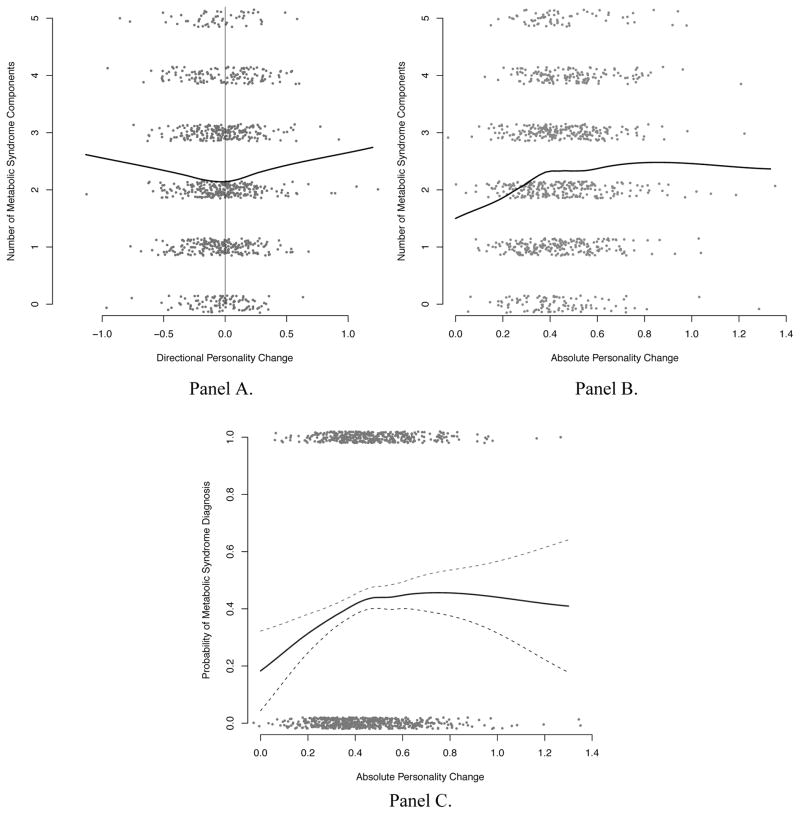
MetS Components
On average, participants in the biological assessment sample met the clinical cut-off for at least two MetS components (M = 2.29, SD = 1.40). To examine whether overall personality change was associated with meeting the cut-offs for a greater number of MetS components, we first regressed the number of MetS components a person exhibited on directional change and the set of covariates. Directional personality change was not significantly linearly associated with MetS components, b = −.03, β = −.01, t(980) = −.17, p = .86. However, this nonsignificant linear relationship masks a significant curvilinear association between directional change and MetS components (see Figure 2A), quadratic effect b = .76, t(979) = 2.29, p < .05. Indeed, as would be expected based on this quadratic effect, absolute personality change was significantly associated with having more MetS components, b = .66, β = .17, t(980) = 2.59, p < .01 (see Table 2; Figure 2B). vii Thus, personality change in any direction was associated with meeting the clinical cut-offs for more MetS components. Of note, this effect was unchanged after controlling for the socially desirable component of the absolute change score, b = .61, β = .16, t(979) = 2.43, p < .05. Further, these effects held controlling for personality trait levels and a range of covariates, nor were there any significant interactions with any of the covariates, all |ts| < 1.39. As can be seen in Table 2, there were interesting associations between Time 2 personality trait levels and MetS components; see the Online Supplemental Appendix for greater discussion.
Figure 2.
Directional (Panel A) and absolute (Panel B) personality change predicting metabolic syndrome components, and absolute personality change predicting the probability of metabolic syndrome diagnosis (Panel C). Not diagnosed = 0, Diagnosed = 1. Dashed lines represent the 95% confidence interval around the nonparametric loess curve. Data are slightly jittered (randomly perturbed) to minimize overplotting.
MetS Diagnosis
A total of 41.57% of participants met the criteria for a MetS diagnosis. Is absolute personality change also associated with the likelihood of receiving a diagnosis of MetS? To examine this we conducted a logistic regression predicting the binary MetS diagnosis variable from absolute personality change and the set of covariates. Absolute personality change was significantly associated with the log-odds of MetS prevalence, odds ratio = 2.31, t(987) = 1.96, p = .05.viii Further, there was a significant nonlinear relationship (see Figure 2C), such that small levels of absolute personality change were strongly related to greater MetS prevalence, odds ratio = 3.88, t(986) = 2.50, p < .05, but the association weakened with very high levels of personality change, with significant quadratic curvature, t(986) = −2.73, p < .05. The decline in MetS prevalence associated with large amounts of personality change is driven by a relatively small number of participants (3% of the sample) with absolute levels of change greater than .80.ix The loess curve, which provides a nonparametric estimate of the relationship, presented in Figure 2C illustrates the decline in MetS prevalence associated with high levels of personality change. Note, however, that the wide 95% confidence intervals around this estimate illustrates how imprecise this relationship is given the paucity of data available for very high levels of personality change. Additional research with samples that have more individuals at the highest levels of personality change would be needed to definitively establish the nature of the relationship at the tail end of the distribution. Note that there were no significant interactions with any of the covariates in predicting MetS diagnosis, all |ts| < 1.20. In sum, absolute personality change is associated with meeting the criteria for a greater number of MetS components and, especially for those with low to moderate levels of personality change, with whether one is actually diagnosed with MetS.
Trait-Specific Personality Change
How is change on each trait associated with MetS components and diagnosis? In line with the overall directional change indicator, directional change on each trait was generally not significantly associated with greater MetS components or diagnosis, |ts| < 1.38. However, the quadratic term for agency was positive and significant, t(288) = 2.30, p < .05, indicating that both positive and negative changes in agency may be associated with greater MetS components. There were no significant quadratic associations for directional change on any of the other personality traits, |ts| < 1.17.
Greater absolute change on agency was significantly associated with meeting the criteria for a greater number of MetS components, b = .35, β = .16, t(989) = 2.68, p < .01, while neuroticism was marginally significantly associated, b = .20, β = .11, t(989) = 1.81, p < .10. Absolute change on agency and neuroticism were also marginally associated with a higher probability of receiving a diagnosis of MetS: Agency odds ratio = 2.27, t(996) = 1.88, p < .10; Neuroticism odds ratio = 2.26, t(996) = 1.85, p < .10. In sum, only agency, and to a lesser extent neuroticism, were individually associated with MetS. It is unclear whether these less consistent trait-specific results are a function of the lowered reliability of the trait-specific change scores or if this indicates that changes on agency and neuroticism are more critical to MetS than other traits.
Discussion
Overall, individuals who demonstrated greater personality change over 10 years also reported worsening subjective health and well-being and exhibited more risky metabolic profiles. These results extend previous findings in a number of ways. First, by examining and comparing multiple types (directional and absolute) of broad and trait-specific personality change it became apparent that both types of change are important, as both predict subjective and objective indicators of health. Second, this is the first paper to demonstrate that personality change is associated with an objective indicator of health in midlife, perhaps lending insight into one pathway through which personality change may be linked to the more distal outcome of mortality. Finally, by simultaneously examining both psychological and objective indicators of health, we are able to identify both commonalities and discrepancies in their associations with personality change, which will be discussed below.
Directional Change
For both subjective and objective indicators of health and well-being, change in what would usually be considered a more negative or undesirable direction (e.g., becoming less conscientiousness and more neurotic) was associated with declining health and well-being over the 10 year period. Thus, it seems plausible that negative changes to one’s personality may promote negative health-relevant behaviors and greater exposure and reactivity to social difficulties (e.g., Friedman, 2000). Interestingly, this effect was not linear, such that change in a positive direction was generally not associated with enhanced health and well-being, and was actually associated with worse psychological well-being for older adults (i.e., those above age 65; see Online Supplemental Appendix) and on the metabolic syndrome indicators. It is unclear why positive change was not as detrimental for self-reported health and satisfaction with life; perhaps there are some subjective benefits to socially desirable change that partially counteract the negative impact of absolute personality change, psychologically if not physiologically. Again, this potential benefit of positive change may not always hold for older adults, possibly because change is generally less frequent and therefore more detrimental in this age group, regardless of direction.
In sum, these results are at least partially in line with the health process model (Adler & Matthews, 1994), supporting the idea that general personality change in a socially undesirable direction may negatively influence one’s lifestyle, behaviors, and reactivity, thereby negatively impacting subjective well-being and physical health. Of course, it is also possible that changes to one’s health behaviors and reactivity, or well-being and health, could have changed personality, or that personality is a marker of other underlying problems that are causing these effects. With only two time points, and personality change being measured concurrently with these health and well-being measures, we are unable to establish causality with these data.
Absolute Personality Change
Although direction-based explanations provide some insight into why change in the undesirable direction may impact health and well-being, clearly there is more at play given that absolute change was also negatively associated with perceived health and well-being, as well as greater MetS components and prevalence. That is, what could be considered positive changes in personality (e.g., becoming more agentic and less neurotic) are also negatively associated with indicators of health and well-being. Why would this be the case? One possibility is that personality change, whether ultimately positive or negative, is itself a stressor. That is, a restructuring of one’s personality and corresponding patterns of behaviors and reactivity may take a strong psychological and physiological toll on an individual. Alternatively, absolute personality change may be an indicator of an internally driven general tendency to vary, indicating a less coherent sense of self and poorer coping abilities (Brandtstädter & Greve, 1994).
One alternative explanation is that greater absolute change is more reflective of variable responding to personality questionnaires or measurement error than of fundamental personality change. Nevertheless, to the extent that variable responding is driven by a psychologically meaningful phenomenon (e.g., a weaker sense of self), this remains an interesting finding. Indeed, the fact that absolute change was associated with meaningful psychological and physiological indicators suggests that this indicator of change must be meaningful (as opposed to just measurement error, for example). Nevertheless, the meaning of absolute personality change, and its causes, requires further examination.
Another alternative explanation is that developing health difficulties drove both personality change and also Time 2 metabolic outcomes. Although these results hold controlling for self-reported health at Time 1, it would of course be preferable to be able to control for more objective indicators of metabolic health at Time 1, and to avoid the concurrent assessments of personality and health indicators. Thus, personality change may be an effect of or perhaps a marker of psychological and health difficulties, as opposed to a cause. As such, all of the causal, mechanistic explanations discussed here must be made with caution. Ultimately, future research with prospective metabolic data and additional time points are needed to better understand the causal relationships among personality change, metabolic outcomes, and perceived health and well-being.
These findings also raise questions about the definition of the desirability of personality traits – if change in what is perceived to be a socially desirable direction is associated with declining health, should such change really be considered desirable? There appears to be a disconnect between what is perceived to be desirable and what may actually be desirable for health and well-being in midlife, a topic that deserves future research attention.
Trait-Specific Effects
The effects of change on subjective health and well-being indicators were generally consistent across each Big 5 trait and agency. These results suggest that change on any trait is negatively associated with one’s subjective health and well-being. In contrast, the associations among trait-specific change and the metabolic syndrome were much less consistent. Only absolute change in agency and neuroticism were significantly and marginally associated, respectively, with meeting the criteria for a greater number of MetS components, while absolute change on both traits was also marginally associated with a greater likelihood of being diagnosed with MetS. These effects were in line with the overall absolute personality change index.
It is possible that the lowered reliability of the trait-specific change scores may have contributed to the null and less consistent findings. On the other hand, change in agency and neuroticism may in fact be more strongly related to physical health than change on other traits. Indeed, there is initial empirical evidence supporting the findings that changes in agency and neuroticism have stronger associations with physical health indicators. For instance, Eizenman et al. (1997) found that short-term variability in perceived control, a construct very similar to agency, predicts mortality. Further, change in neuroticism has also been previously linked to higher mortality risk (Mroczek & Spiro, 2007). However, in contrast to Mroczek and Spiro’s finding that increases in neuroticism were important, here we found indications that any change, even decreases, in neuroticism was associated with worse metabolic profiles at Time 2.
Why would positive as well as negative changes in neuroticism and agency be associated with the metabolic syndrome? Is it a function of greater variability, rather than stable change, or can stable positive changes in these traits even have a negative impact? There is evidence for a protective effect of high neuroticism, perhaps because of enhanced vigilance to potential health problems (Taga & Friedman, 2009). Thus, perhaps stable decreases in neuroticism could have harmful effects if compensatory health-enhancing behaviors are not successfully employed. Similarly, increases in agency may lead individuals to reject previously successful coping strategies (e.g., seeking instrumental social support) without developing compensatory strategies when faced with stressors. Future research that examines these competing explanations and potential mechanisms is needed. For example, longitudinal studies coupled with experience sampling methods would help to address to the question of whether this is a function of stable change or general variability. Similarly, assessing appraisal processes, coping behaviors, and physiological reactivity may provide some insight into the mechanisms underlying these associations.
Conclusion
In sum, both absolute and socially undesirable personality change over 10 years are associated with lower perceived health and well-being. Further, these data provide the first evidence that absolute personality change (particularly on agency and neuroticism) is associated with an objective, proximal health indicator, the metabolic syndrome, potentially providing insight into the intermediate links between personality change and mortality risk. Although the precursors of personality change and the causal links between personality change, well-being, and metabolic dysfunction remain to be determined, these data suggest that long-term personality changes in midlife may contribute to both psychological and physical health.
Supplementary Material
Acknowledgments
Support for MIDUS came from the National Institute on Aging (RO1 AG-032271, P01 AG-020166). Preparation of this article was supported by a Social Sciences and Humanities Research Council of Canada grant to Jeremy C. Biesanz (410-2008-2643).
Footnotes
The study reported by Turiano et al. (2012) also utilized the MIDUS sample, but our study differs in several important respects by: 1) examining an alternative index of subjective health from the self-report questionnaire rather than phone interview, 2) also examining psychological well-being, 3) examining nonlinear and absolute change in addition to linear directional change, and 4) examining an objectively measured indicator of health, the metabolic syndrome.
All reported results are based on available data only. However, it is possible that the missing data may have biased our results so we re-ran all analyses using multiple imputation to account for missingness. The results of these analyses were essentially identical. Further, the MIDUS sample includes twin and non-twin siblings (Total N at Time 1 = 1907). To account for potential nonindependence in the dataset, all analyses were re-run as multilevel models, with family ID as a random effect predicting the intercept. All results held when accounting for this data clustering.
Older adults did show slightly but significantly less change than younger adults, b = −.002, β = −.09, t(3893) = −6.11, p < .001, in line with previous findings that personality becomes increasingly consistent, if not fixed, over time (Roberts & DelVecchio, 2000).
Note that these are the most recent IDF guidelines for waist circumference cut-points (see http://www.idf.org/webdata/docs/MetS_def_update2006.pdf).
Note that personality change also predicts levels of subjective health and well-being at Time 2, rather than change in health and well-being (see Online Supplemental Appendix).
The full set of covariates were not included in the subjective health and well-being analyses because they were not were all available for the full set of participants and inclusion therefore reduced the sample size substantially. To ensure that the results with the subjective indicators also hold adjusting for the full set of covariates, all analyses were also run and did hold within the biological assessment subsample.
Comparable and indeed slightly stronger results were obtained analyzing the probability of the presence of a metabolic syndrome component as a multilevel logistic regression where each component was considered a repeated measure with different intercepts for each component and random intercepts for participant and family. For a parsimonious presentation of results we report the standard regression analysis predicting number of components in the manuscript. Another important issue to consider is that dichotomizing the MetS components (based on the clinical cut-offs) to create the composite measure results in a loss of data, which could obscure the results. Thus, we also examined whether these effects held using a continuous indicator of MetS components, following the procedures of van Reed Dortland et al. (2012, Progress in Neuro-Psychopharmacology). The main finding of absolute personality change significantly predicting greater MetS did hold using the continuous measure, b = .22, t(980) = 2.11, p < .05.
Following the argument outlined by Gelman (2008), we calculated the odds ratio based on a 2 standard deviation change in the predictor (e.g., absolute personality change), which provides a conceptual equivalency between dichotomous and continuous predictors.
Participants with very high levels of personality change did not differ significantly from the rest of the sample in terms of gender, but they were significantly younger and less educated, all ps < .05, perhaps indicating that personality change is less detrimental for younger individuals, for whom personality change is more common (see Online Supplemental Appendix for further consideration of the role of age). Absolute personality change significantly predicted MetS diagnosis when these participants were excluded, odds ratio = 3.34, t(957) = 2.24, p < .05.
The Online Supplemental Appendix can be found at: http://www.socialaccuracy.com/publications.html.
References
- Adler N, Matthews K. Health psychology: Why do some people get sick and some stay well? Annual Review of Psychology. 1994;45:229–259. doi: 10.1146/annurev.ps.45.020194.001305. [DOI] [PubMed] [Google Scholar]
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Brandtstädter J, Greve W. The aging self: Stabilizing and protective processes. Developmental Review. 1994;14:52–80. doi: 10.1006/drev.1994.1003. [DOI] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, Eckel RH. The metabolic syndrome. Endocrine Reviews. 2008;29:777–822. doi: 10.1210/er.2008-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dienberg Love G, Seeman TE, Weinstein M, Ryff CD. Bioindicators in the MIDUS national study: Protocol, measures, sample, and comparative context. Journal of Aging and Health. 2010;22:1059–1080. doi: 10.1177/0898264310374355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards AL. The social desirability variable in personality assessment and research. New York: Dryden; 1957. [Google Scholar]
- Eizenman DR, Nesselroade JR, Featherman DL, Rowe JW. Intraindividual variability in perceived control in a older sample: The MacArthur successful aging studies. Psychology and Aging. 1997;12:489–502. doi: 10.1037/0882-7974.12.3.489. [DOI] [PubMed] [Google Scholar]
- Elovainio M, Merjonen P, Pulkki-Råback L, Kivimäki M, Jokela M, Mattson N, Keltikangas-Järvinen L. Hostility, metabolic syndrome, inflammation and cardiac control in young adults: The young finns study. Biological Psychology. 2011;87:234–240. doi: 10.1016/j.biopsycho.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Friedman HS. Long-Term relations of personality and health: Dynamisms, mechanisms, tropisms. Journal of Personality. 2000;68:1089–1107. doi: 10.1111/1467-6494.00127. [DOI] [PubMed] [Google Scholar]
- Gelman A. Scaling regression inputs by dividing by two standard deviations. Statistics in Medicine. 2008;27:2865–2873. doi: 10.1002/sim.3107. [DOI] [PubMed] [Google Scholar]
- Goldbacher EM, Bromberger J, Matthews KA. Lifetime history of major depression predicts the development of the metabolic syndrome in middle-aged women. Psychosomatic Medicine. 2009;71:266–272. doi: 10.1097/PSY.0b013e318197a4d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson SE, Goldberg LR, Vogt TM, Dubanoski JP. Mechanisms by which childhood personality traits influence adult health status: Educational attainment and healthy behaviors. Health Psychology. 2007;26:121–125. doi: 10.1037/0278-6133.26.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PL, Turiano NA, Mroczek DK, Roberts BW. Examining concurrent and longitudinal relations between personality traits and social well-being in adulthood. Social Psychological and Personality Science. 2012 doi: 10.1177/1948550611433888. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham EK, Lachman ME. Personality stability is associated with better cognitive performance in adulthood: Are the stable more able? Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2012 doi: 10.1093/geronb/gbr149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John OP, Robins RW. Determinants of interjudge agreement on personality traits: The Big Five domains, observability, evaluativeness, and the unique perspective of the self. Journal of Personality. 1993;61:521–551. doi: 10.1111/j.1467-6494.1993.tb00781.x. [Special Issue] [DOI] [PubMed] [Google Scholar]
- Kern ML, Friedman HS. Personality and pathways of influence on physical health. Social and Personality Psychology Compass. 2011;5:76–87. doi: 10.1111/j.1751-9004.2010.00331.x. [DOI] [Google Scholar]
- Korten AE, Jorm AF, Jiao Z, Letenneur L, Jacomb PA, Henderson AS, Rodgers B. Health, cognitive, and psychosocial factors as predictors of mortality in an elderly community sample. Journal of Epidemiology and Community Health. 1999;53:83–88. doi: 10.1136/jech.53.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The midlife development inventory (MIDI) personality scales: Scale construction and scoring. 1997 Retrieved from http://www.brandeis.edu/departments/psych/lachman/pdfs/midi-personality-scales.pdf.
- Miller GE, Chen E, Cole SW. Health psychology: Developing biologically plausible models linking the social world and physical health. Annual Review of Psychology. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AS, Seeman TE. Pathways to resilience: Maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychological Science. 2011;22:1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A. Personality change influences mortality in older men. Psychological Science. 2007;18:371–376. doi: 10.1111/j.1467-9280.2007.01907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A, Turiano N. Do health behaviors explain the effect of neuroticism on mortality? Longitudinal findings from the VA normative aging study. Journal of Research in Personality. 2009;43:653–659. doi: 10.1016/j.jrp.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips AC, Batty GD, Weiss A, Deary I, Gale CR, Thomas GN, Carroll D. Neuroticism, cognitive ability, and the metabolic syndrome: The vietnam experience study. Journal of Psychosomatic Research. 2010;69:193–201. doi: 10.1016/j.jpsychores.2010.01.016. [DOI] [PubMed] [Google Scholar]
- Prenda KM, Lachman ME. Planning for the future: A life management strategy for increasing control and life satisfaction in adulthood. Psychology and Aging. 2001;16:206–216. doi: 10.1037//0882-7974.16.2.206. [DOI] [PubMed] [Google Scholar]
- Puustinen PJ, Koponen H, Kautiainen H, Mäntyselkä P, Vanhala M. Psychological distress predicts the development of the metabolic syndrome: A prospective population-based study. Psychosomatic Medicine. 2011;73:158–165. doi: 10.1097/PSY.0b013e3182037315. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The power of personality: The comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspectives on Psychological Science. 2007;2:313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Mroczek D. Personality trait change in adulthood. Current Directions in Psychological Science. 2008;17:31–35. doi: 10.1111/j.1467-8721.2008.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin. 2000;126:3–25. doi: 10.1037//0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Rogosa DR, Willett JB. Demonstrating the reliability the difference score in the measurement of change. Journal of Educational Measurement. 1983;20:335–343. doi: 10.1111/j.1745-3984.1983.tb00211.x. [DOI] [Google Scholar]
- Ryff CD, Keyes CL. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. doi: 10.1037/0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Sherman RA, Nave CS, Funder DC. Properties of persons and situations relate to overall and distinctive congruence. Journal of Research in Personality. 2012;46:87–101. doi: 10.1016/j.jrp.2011.12.006. [DOI] [Google Scholar]
- Siegler IC, Costa PT, Brummett BH, Helms MJ, Barefoot JC, Williams RB, Rimer BK. Patterns of change in hostility from college to midlife in the UNC alumni heart study predict high-risk status. Psychosomatic Medicine. 2003;65:738–745. doi: 10.1097/01.PSY.0000088583.25140.9C. [DOI] [PubMed] [Google Scholar]
- Smith TW. Personality as risk and resilience in physical health. Current Directions in Psychological Science. 2006;15:227–231. doi: 10.1111/j.1467-8721.2006.00441.x. [DOI] [Google Scholar]
- Sutin AR, Costa PT, Uda M, Ferrucci L, Schlessinger D, Terracciano A. Personality and metabolic syndrome. Age (Dordrecht, Netherlands) 2010;32:513–519. doi: 10.1007/s11357-010-9153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taga KA, Friedman HS, Martin LR. Early personality traits as predictors of mortality risk following conjugal bereavement. Journal of Personality. 2009;77:669–690. doi: 10.1111/j.1467-6494.2009.00561.. [DOI] [PubMed] [Google Scholar]
- Turiano NA, Pitzer LM, Armour C, Karlamangla A, Ryff CD, Mroczek DK. Personality trait level and change as predictors of health outcomes: Findings from a national study of Americans (MIDUS) The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2012 doi: 10.1093/geronb/gbr072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Reedt Dortland AK, Giltay EJ, van Veen T, Zitman FG, Penninx BW. Personality traits and childhood trauma as correlates of metabolic risk factors: The netherlands study of depression and anxiety (NESDA) Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2012;36:85–91. doi: 10.1016/j.pnpbp.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Vollrath M, Knoch D, Cassana L. Personality, risky health behavior, and perceived susceptibility to health risks. European Journal of Personality. 1999;13:39–50. doi: 10.1002/(SICI)1099-0984(199901/02)13:1<39::AID-PER328>3.0.CO;2-J. [DOI] [Google Scholar]
- Wiggins J. Agency and communion as conceptual coordinates for the understanding and measurement of interpersonal behavior. In: Cicchetti D, Grove W, editors. Thinking clearly about psychology: Essays in honor of Paul Everett Meehl. Minneapolis: University of Minnesota Press; 1991. pp. 89–115. [Google Scholar]
- Zimprich D, Allemand M, Lachman ME. Factorial structure and age-related psychometrics of the MIDUS personality adjective items across the life span. Psychological Assessment. 2011 doi: 10.1037/a0025265. Advance Online Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.