Abstract
Hermansky-Pudlak syndrome (HPS) type is a rare disorder of oculocutaneous albinism, platelet dysfunction, and in some subtypes, fatal pulmonary fibrosis. There is no effective treatment for the pulmonary fibrosis except lung transplantation, but an initial trial using pirfenidone, an anti-fibrotic agent, showed promising results. The current, randomized, placebo-controlled, prospective, double-blind trial investigated the safety and efficacy of pirfenidone for mild to moderate HPS-1 and 4 pulmonary fibrosis. Subjects were evaluated every 4 months at the National Institutes of Health Clinical Center, and the primary outcome parameter was change in forced vital capacity using repeated measures analysis with random coefficients. Thirty-five subjects with HPS-1 pulmonary fibrosis were enrolled during a 4-year interval; 23 subjects received pirfenidone and 12 received placebo. Four subjects withdrew from the trial, 3 subjects died, and 10 serious adverse events were reported. Both groups experienced similar side effects, especially gastroesophageal reflux. Interim analysis of the primary outcome parameter, performed 12 months after 30 patients were enrolled, showed no statistical difference between the placebo and pirfenidone groups, and the study was stopped due to futility. There were no significant safety concerns. Other clinical trials are indicated to identify single or multiple drug regimens that may be effective in treatment for progressive HPS-1 pulmonary fibrosis.
Keywords: Hermansky-Pudlak syndrome, albinism, pulmonary function tests, pulmonary fibrosis, Puerto Rico, pirfenidone
1.0 Introduction
Hermansky-Pudlak syndrome (HPS) consists of 8 genetically distinct subtypes, which share the common features of oculocutaneous albinism and a platelet storage pool deficiency [1–4]. Approximately 15% of patients experience granulomatous colitis [2, 5], and people with HPS-1, HPS-2 and HPS-4 develop pulmonary fibrosis [6–8]. The cellular defect in HPS is abnormal biogenesis of lysosome-related organelles. Absence of dense bodies on platelet electron microscopy confirms the diagnosis of HPS [9]; the lack of these lysosome-related organelles causes the bleeding diathesis. In addition, defective melanosome formation in melanocytes results in hypopigmentation. The etiology of the granulomatous colitis and pulmonary fibrosis in HPS remains unknown.
Although rare worldwide, HPS is the most common recessively inherited form of albinism in Puerto Rico. HPS-1 is concentrated in the northwest section of Puerto Rico, where the frequency is 1 in 1800 [10] due to a founder mutation (i.e., a 16-bp duplication in exon 15 of HPS1) [11]. HPS-3 is primarily found in the center of the island due to a different founder mutation (i.e., a 3904-bp deletion in HPS3) [12].
Pulmonary fibrosis remains the most serious manifestation of HPS, and lung disease typically develops in the third to fifth decade of life [2, 7]. Patients present with progressive exertional dyspnea, fatigue, and chronic cough. Pulmonary function testing reveals a restrictive pattern with low diffusing capacity [6, 13] and hypoxemia with ambulation. High-resolution computed tomography (HRCT) scan imaging of the chest reveals ground-glass opacities, interstitial reticulations, and honeycombing [13]. The course of the lung disease varies among patients, but is universally progressive with an approximate two-year survival when forced vital capacity reaches 50% of predicted values [18]. There is no effective treatment except lung transplantation (14), which has been performed successfully in several patients.
The poor outcome associated with HPS pulmonary fibrosis prompted an initial clinical trial at the National Institutes of Health (NIH) Clinical Center using the anti-fibrotic agent, pirfenidone (5-methyl-1-phenyl-2-(1H)-pyridone). Pirfenidone, a small molecule that inhibits TGF-beta-mediated fibroblast proliferation and collagen synthesis in vitroameliorates cyclosporine- and bleomycin-induced pulmonary fibrosis in mice [15, 16]. The initial study demonstrated that pirfenidone was safe, and it showed modest benefit in treatment for HPS-1 pulmonary fibrosis with respect to the primary outcome parameter, rate of change in forced vital capacity [18]. This paper reports the results of a second study, which investigated pirfenidone in the treatment for mild to moderate HPS-1 pulmonary fibrosis.
2.0 Methods
2.1 Subjects and testing
Subjects were enrolled between 2005 and 2009 in protocol 97-HG-0085, which was approved by the National Human Genome Research Institute (NHGRI) Institutional Review Board. Primary inclusion criteria were a diagnosis of HPS-1 or -4 confirmed by molecular analysis [3, 7, 8] and a forced vital capacity between 51–85% of predicted, regardless of radiographic evidence of fibrosis on HRCT. Subjects were excluded if they had exposures or other medical conditions associated with pulmonary fibrosis. Subjects gave written, informed consent.
2.2 Study design
The study was a prospective, double-blind, randomized, placebo-controlled trial. Two patients were randomized to receive pirfenidone for every one randomized to placebo. Randomization was performed independently by the NIH Pharmaceutical Development Service, who had no knowledge of the subjects’ clinical status. In addition to being placed in treatment groups, subjects were stratified according to the severity of their lung disease; a mild designation was applied to patients with forced vital capacities of 68–85% of predicted, and a moderate designation to patients with forced vital capacities of 51–67% of predicted.
Evaluations were conducted at the NIH Clinical Research Center every 4 months for 3–4 days. Baseline and annual evaluations included a general medical assessment, echocardiogram, pulmonary function tests, and HRCT scan of the chest. Interim visits included a general medical evaluation and pulmonary function tests. Pulmonary function tests were performed in accordance with American Thoracic Society guidelines as previously described [19]. All pulmonary function tests and chest computed tomography scans were reviewed by a pulmonologist. In addition, HRCT scans were scored by a computer that used a scale of 0 (normal) to 100 (completely diseased lung) as previously described [20]. Criteria for termination included development of a serious adverse event (SAE) preventing further administration of pirfenidone, non-compliance with medication, pregnancy, two missed appointments within a 2-year period, use of an excluded therapy (e.g., steroids), or lung transplantation.
2.3 Statistical analysis
Power estimates were based upon an expected difference in rate of decline of forced vital capacity between pirfenidone and placebo-treated patients of 9 ± 6% per year; this rate was estimated from studies of HPS patients previously followed at the NIH. Based upon this estimate, the power to detect a significant difference at the 5% level would be 0.99 using 26 pirfenidone patients and 13 placebo patients. Recruitment of these 39 patients was intended to occur over the course of 12 months, with an interim analysis 12 months after enrollment was complete; demonstration of efficacy upon interim analysis would require a difference between the two treatment groups that was significant at p = 0.005.
The primary outcome parameter was rate of change in post-bronchodilator forced vital capacity, analyzed using repeated measures with a random coefficients model to account for the expected inter-patient variability. When patients dropped out of the study or died, a forced vital capacity 25% of predicted was assigned to them [18]. The statistical analysis plan for secondary outcome parameters was later modified by the investigators using the means of the differences between final and baseline results, and calculations of the rate of change in percent predicted forced vital capacity. For between group comparisons, an unequal variance version the Student’s two-sided t-test was employed.
2.4 Pirfenidone
Pirfenidone or placebo was dispensed by the NIH Pharmaceutical Development Service. Pirfenidone was obtained from InterMune (Brisbane, CA) under IND # 72,778 held by the principal investigator (W.A.G.). The placebo, also provided by InterMune, was composed of cellulose, starch, magnesium, and Bitrex, the latter ingredient being used to mimic the taste of pirfenidone. A dosage escalation schedule was employed to reach 801 mg t.i.d.; subjects took one 267 mg pill t.i.d. for the first week, two pills t.i.d. for the second week, and thereafter the full dose of three pills t.i.d.
2.5 Compliance
Compliance was assessed through regular phone contact and interim medical histories. Subjects were provided with pill boxes and written instructions to enhance compliance. Patients were given logs to record their medication usage and were closely followed by two bi-lingual staff.
2.6 Adverse events
Subjects were assessed for adverse events while on therapy. Adverse events were divided into expected complications of the disease and known side effects of pirfenidone, and serious adverse events. Known and minor side effects of pirfenidone were recorded and reported in aggregate, and serious adverse events were reported to the DSMB and IRB according to protocol guidelines.
3.0 Results
3.1 Baseline characteristics
Subjects in the placebo and pirfenidone groups were well matched for age, ethnicity, and severity of disease, as gauged by pulmonary function test results, 6-minute walk distance and partial pressure of oxygen, HRCT scores, and blood chemistries (Table 1). In particular, both groups showed similar degrees of impairment in forced vital capacity, total lung capacity, and diffusion capacity indicating pulmonary restriction and mild reduction of gas exchange. A total of 35 subjects enrolled in the study; 23 received pirfenidone and 12 received placebo. With the exception of 2 subjects, all participants were Puerto Rican. The pirfenidone group had a preponderance of females. In the pirfenidone group, 18 subjects had mild pulmonary fibrosis (forced vital capacity 68–85% of predicted) and 5 had moderate disease (forced vital capacity 51–67% of predicted). Four subjects in the pirfenidone group and 2 in the placebo group did not have radiographic evidence of fibrosis on HRCT scan.
Table 1.
Baseline characteristics of treatment groups
| Placebo (N=12) | Pirfenidone (N= 23) | P | |
|---|---|---|---|
| M/F | 6/6 | 8/15 | |
| Age (y) | 43.4 ± 7.7 | 39.2 ± 10.8 | 0.24 |
| Puerto Ricana | 11 | 22 | |
| Non-Puerto Rican | 1 | 1 | |
| Mildb | 9 (75%) | 18 (78%) | |
| Moderateb | 3 (25%) | 5 (22%) | |
| FVCc | 73.5 ± 9.7 | 72.9 ± 7.9 | 0.84 |
| FEV1/FVC | 111 ± 6.7 | 108 ± 11.3 | 0.41 |
| FEV1 c | 82.1 ± 10.9 | 80.7 ± 9.9 | 0.70 |
| TLCc | 73.3 ± 9.5 | 73.9 ± 11.7 | 0.88 |
| DLCOadjc | 66.8 ± 15.9 | 68.0 ± 16.6 | 0.84 |
| Baseline 6-min walk (m) | 525 ± 94 | 504 ± 120 | 0.60 |
| HRCT Score | 0.20 ± 0.16 | 0.19 ± 0.21 | 0.44 |
| PaO2 (mmHg) | 96.0 ± 5.3 | 93.4 ± 16.4 | 0.71 |
| Hemoglobin (g/dL) | 14.5 ± 1.3 | 13.6 ± 1.8 | 0.14 |
| Leucocyte count (106/L) | 6.5 ± 1.6 | 6.8 ± 1.8 | 0.63 |
| Alanine amino transferase (U/L) | 32 ± 22 | 27 ± 14 | 0.41 |
| Prothrombin time (s) | 13.0 ± 0.7 | 13.1 ± 0.5 | 0.77 |
| Potassium (mEq/L) | 4.0 ± 0.2 | 4.0 ± 0.8 | 0.93 |
| Total cholesterol (mg/dL) | 198 ± 29 | 192 ± 33 | 0.63 |
Results are means ± SD.
All Puerto Rican patients were homozygous for the 16-bp duplication in exon 15 of HPS1.
Mild, ≥68% predicted FVC; Moderate, ≤67% predicted FVC.
% predicted
3.2 Compliance
Mean duration on study for the 35 subjects was 25.2 mo (26.8 ± 10.5 mo for the placebo group; 24.3 ± 13.8 mo for the pirfenidone group; p = 0.59). In total, 210 (93%) of 226 scheduled admissions were kept. Missed appointments (4 placebo; 12 pirfenidone) were due to medical illness or sudden changes in work schedules, except for two subjects who missed one or two visits prior to withdrawing from the trial. One subject in the placebo group and 3 in the pirfenidone group voluntarily withdrew from the study. One pirfenidone-treated subject was taken off drug due to the occurrence of a serious adverse event (SAE), but remained on the study on an intent-to-treat basis.
3.3 Safety
There were 10 SAEs and a variety of non-serious adverse events during the course of the trial (Table 2).
Table 2.
Serious and non-serious adverse events
| Placebo (N=12) | Pirfenidone (N=23) | |||
|---|---|---|---|---|
| Serious Adverse Events | N | % | N | % |
| Fatal | 1 | 8 | 2 | 9 |
| Nonfatal | 1 | 8 | 6 | 26 |
| Other Adverse Events | ||||
| Nausea | 1 | 8 | 4 | 17 |
| Vomiting | 2 | 17 | 0 | 0 |
| Heartburn | 6 | 50 | 12 | 52 |
| Transaminitis | 0 | 0 | 1 | 4 |
| Photosensitivity rash | 0 | 0 | 2 | 9 |
| Drug eruption rash | 0 | 0 | 1 | 4 |
| Urticaria | 1 | 8 | 0 | 0 |
| Rash (unspecified) | 2 | 17 | 2 | 9 |
| Dizziness/lightheadedness | 0 | 0 | 1 | 4 |
| Fatigue | 0 | 0 | 2 | 9 |
| Drowsiness | 0 | 0 | 2 | 9 |
| Palpitations | 0 | 0 | 2 | 9 |
| Chest pain | 1 | 8 | 2 | 9 |
| Joint pain | 0 | 0 | 1 | 4 |
| Abdominal pain | 2 | 17 | 1 | 4 |
| Muscle Aches | 1 | 8 | 0 | 0 |
3.3.1 Deaths
Three of the 10 SAEs involved deaths during the trial. Two in the pirfenidone group died at 74 and 45 years of age, which occurred 6 and 25 months after enrollment, respectively. One patient in the placebo group died at 56 years of age, which occurred 42 months after enrollment. The deaths were considered to reflect the natural course of the lung disease.
SAE #5 was a 74-year old Puerto Rican female randomized to pirfenidone. Her initial forced vital capacity was 68% of predicted and her diffusion capacity was 38% of predicted. Her HRCT showed a moderate degree of pulmonary fibrosis with some honeycombing in the lung bases. She desaturated to 64% on room air during her six-minute walk test. After 3 months on study, her oxygen saturation was 85% on 3 L/min oxygen. She missed her 4-month visit, remained compliant with study drug therapy, and continued to deteriorate. At 6 months, she was transitioned to hospice care on high-flow oxygen. The subject expired from respiratory failure seven months after enrollment.
SAE #7 was a 45 year-old Puerto Rican man randomized to pirfenidone. His forced vital capacity was 59% of predicted and his initial HRCT showed moderately severe pulmonary fibrosis with honeycombing in the lung bases. He desaturated to 88% on room air during his initial six-minute walk test. At his 16-month visit his forced vital capacity was 37% of predicted and his diffusion capacity was too low to calculate. Oxygen therapy was initiated, and lung transplantation was pursued. He missed his 20-month and 24-month admissions. At 25 months, he was hospitalized locally for dyspnea, improved, and was discharged on oxygen at 10 L/min. The subject expired two days after discharge.
SAE #9 was a 53 year-old Puerto Rican female randomized to the placebo group. Her initial forced vital capacity was 58% of predicted, and her baseline HRCT showed a moderate degree of pulmonary fibrosis. At her 36-month visit, she reported worsening exertional dyspnea, with a forced vital capacity of 30% of predicted and a diffusion capacity of 40% of predicted; oxygen therapy was initiated. She was unable to travel for her 40-month admission, and died of end-stage lung disease 42 months after enrollment.
3.3.2 Other serious adverse events
Six additional subjects experienced 7 nonfatal SAEs (6 in the pirfenidone group, 1 in the placebo group) (Table 3). Two subjects were hospitalized with severe chest pain; both had histories of recurrent chest pain, but their pre-enrollment cardiac evaluation showed no evidence of coronary ischemia. Subject #101 underwent coronary angiography, revealing a congenital malformation in the descending branch of the left coronary artery causing reversible ischemic defects in the myocardium. Other SAEs involved a deep vein thrombosis, elevated serum creatine phosphokinase values, hematochezia, dizziness, and vertigo. In every case, the study drug was stopped for a time; in all cases except SAE #1, it was restarted. Except for SAE #1, the SAE resolved spontaneously.
Table 3.
Non-fatal Serious Adverse Events
| SAE # | Age/Sex | Study Group | Event | Months after enrollment |
Resolution | Restart drug? |
|---|---|---|---|---|---|---|
| 1 | 44-M | Pirf-Moderate | Chest pain | 1 | No cardiac disease; chest pain recurred off drug | No |
| 2 | 38-Ma | Pirf-Mild | Deep vein thrombosis | 11 | Warfarin; restart rug | Yes |
| 3 | 34-F | Placebo-Mild | Elevated CPK | 21 | CPK normalized; | Yes |
| 4 | 39-Ma | Pirf-Mild | Elevated CPK | 22 | CPK normalized | Yes |
| 6 | 43-M | Pirf-Mild | Hematochezia | 4 | Resolved | |
| 8 | 56-M | Pirf-Mild | Chest pain, dizziness | 27 | Resolved | Yes |
| 10 | 43-F | Pirf-Mild | Otitis, vertigo | 46 | Resolved | Yes |
Same subject.
3.3.3 Non-serious adverse events
The most commonly reported symptoms, dyspepsia and heartburn, were seen in approximately half of the subjects in each group. The majority of subjects reported symptoms due to gastroesophageal reflux prior to randomization and almost all required anti-acid therapy, irrespective of their treatment group. Proton pump inhibitors provided better symptom relief than histamine-2 antagonists.
Other adverse events were more common in the pirfenidone group. A photosensitivity rash occurred upon sun exposure in subject #204 as a red, mildly pruritic, and papular eruption on the forearms approximately three months after starting therapy. Subject #202 developed a similar rash on his forearms, neck and upper back after sun exposure. The subjects were given high-caliber sun block, study drug was continued, and the rashes resolved without recurrence. Another subject receiving pirfenidone developed a red, papular rash on her extremities after 4 months of therapy, but had also been started on thyroid replacement therapy at approximately that time. The study drug was stopped, and the subject withdrew from the study before the drug was re-started. A fourth subject in the pirfenidone group developed a pruritic, red papular rash after 5 months of treatment and was taken off the drug. The rash resolved with topical steroid cream, and re-appeared after re-starting therapy; skin biopsy was consistent with a drug eruption.
For both the pirfenidone and placebo groups, baseline and final laboratory values for hemoglobin, total leucocyte count, serum creatinine, alanine aminotransferase, potassium, and total cholesterol did not differ significantly (data not shown). For both the pirfenidone and placebo groups, the prothrombin time rose significantly during the study, but remained within the normal range. There was no evidence of bone marrow, cardiac, renal, or hepatic toxicity.
3.4 Efficacy
3.4.1 Primary outcome parameter; repeated measures analysis
An interim analysis was performed 12 months after 30 individuals were enrolled. Rate of decline in forced vital capacity, assessed by repeated measures analysis with random coefficients, was 0.7%/year less for the pirfenidone group compared with the placebo group. This occurred despite the two deaths and 3 dropouts in the pirfenidone group; nevertheless, it was far from significant, and the protocol was terminated due to futility.
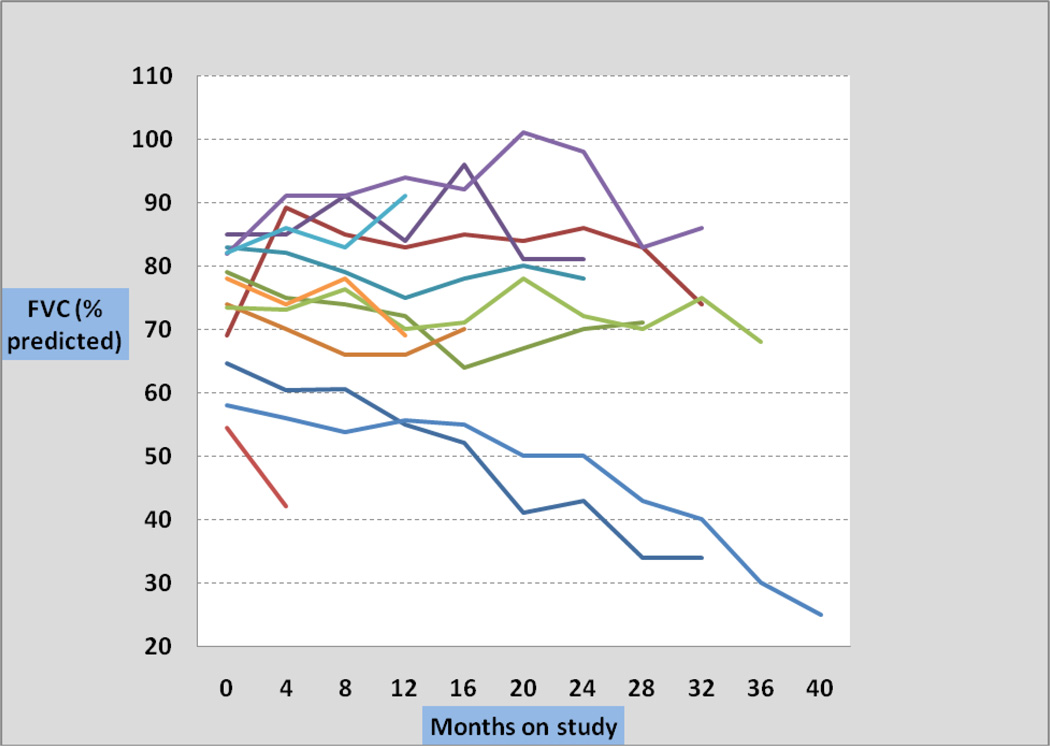
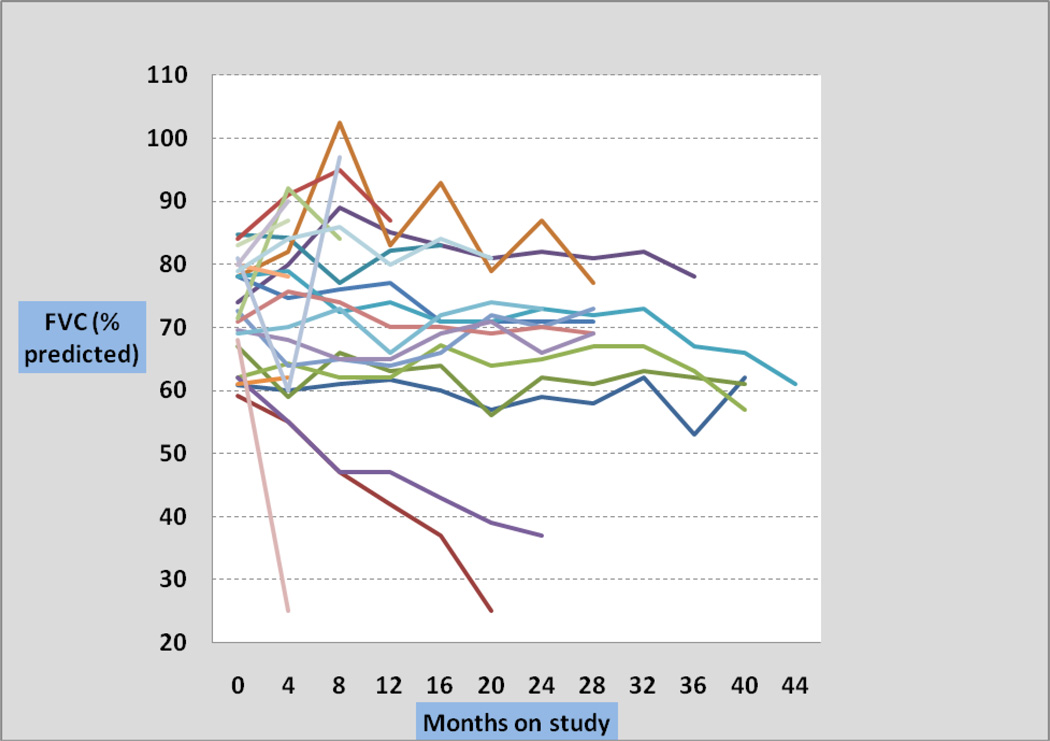
Individual plots of forced vital capacity against time are presented for the placebo group (Figure 1) and for the pirfenidone group (Figure 2). There was no difference between the two groups.
Figure 1. Forced vital capacity of placebo subjects plotted against time on study.
Percentage of predicted forced vital capacity for 12 subjects receiving placebo is shown. Interval measurements were made every 4 months on study.
Figure 2. Forced vital capacity of pirfenidone subjects plotted against time on study.
Percentage of predicted forced vital capacity for 23 subjects receiving pirfenidone is shown; interval measurements were made every 4 months on study.
3.4.2 Secondary outcome parameters and analyses
Additional outcome measures were analyzed by calculating means of the differences between final and baseline results, which were weighted for time on study, and calculations of the slope of change in percent predicted forced vital capacity, which was annualized. These means ± SD, determined for pulmonary function tests (i.e., forced vital capacity, total lung capacity, adjusted diffusion capacity) and expressed as percentage of predicted values, did not differ between the pirfenidone and placebo groups (Table 4). In addition, neither the baseline nor the final mean HRCT scores differed between the pirfenidone and placebo groups (Table 4). Representative computed tomography scan images demonstrate radiographic progression of pulmonary fibrosis in a subject from each group (Figure 3).
Table 4.
Secondary Outcome parameters
| Placebo (N= 12) | Pirfenidone (N =23) | ||
|---|---|---|---|
| FINAL-BASELINEa | Mean ± SD | Mean ± SD | P |
| FVC | −3.8 ± 9.0 | −2.0 ± 5.6 | 0.48 |
| FEV1 | −4.8 ± 10.1 | −2.5 ± 6.3 | 0.42 |
| TLC | −3.6 ± 9.4 | −4.0 ± 8.4 | 0.89 |
| DLCOadj | −2.4 ± 7.6 | −0.3 ± 5.9 | 0.39 |
| HRCT scoreb | |||
| Baseline | 0.20 ± 0.2 | 0.19 ± 0.2 | 0.45 |
| Final | 0.28 ± 0.2 | 0.21 ± 0.2 | 0.32 |
| RATE OF CHANGEC | |||
| FVC | −2.8 ± 5.0 | −2.0 ± 10.2 | 0.80 |
| TLC | −2.1 ± 6.0 | −2.5 ± 4.6 | 0.83 |
| DLCOadj | −2.0 ± 4.5 | 0.0 ± 6.2 | 0.38 |
Percent predicted, weighted for months on study.
N=11 for placebo; N=22 for pirfenidone.
Percent predicted. Rate of change in PFT data is calculated as the slope and is annualized.
Figure 3. Representative CT scan images from two HPS subjects.
A–C. CT scans of subject #104, a 54-year-old man, randomized to placebo, showing worsening fibrosis (arrows) with a subpleural predominance of disease. The patient’s baseline FVC fell from 65% to 34% of predicted after 32 months on study.
D–I. CT scans of subject #107, a 48-year-old woman randomized to pirfenidone. The conventional (D–F) and high-resolution (G–I) CT scans show bilateral progressive areas of fibrosis (arrows). Her baseline FVC fell from 62% to 37% of predicted after 24 months on study.
4.0 Discussion
Of the 8 HPS subtypes, only types 1, 2 and 4 manifest pulmonary fibrosis [2]. HPS-1 and HPS-4 resemble each other clinically because the protein products of the HPS1 and HPS4 genes interact together as Biogenesis of Lyososome-related Organelles Complex-3, i.e., BLOC-3 [21]. This complex is considered to function in the early stages of intracellular vesicle formation and trafficking [3]. HPS-2 is due to defects in the beta-3A subunit of adaptor protein complex-3 [22], which functions in the interactions of intracellular vesicle membranes [23]. Only recently has HPS-2 been associated with pulmonary fibrosis. The relationship between the development of pulmonary fibrosis and the basic defect in these HPS subtypes remains speculative.
Our understanding of the pulmonary fibrosis of HPS derives largely from studies of HPS-1, because HPS-2 and HPS-4 are extremely rare disorders [2]. In particular, the genetic isolate of HPS-1 in Puerto Rico, which numbers approximately 650, has revealed that in HPS-1 pulmonary fibrosis, pulmonary function tests decline in concert [6, 7] and their rate of decline generally resembles that of severe IPF [18]. Death due to HPS-1 pulmonary fibrosis typically occurs between 40 to 50 years of age with a forced vital capacity approximating 25% of predicted [18]. Although its mechanisms of action remain incompletely defined, pirfenidone has been shown to have anti-fibrotic and anti-inflammatory effects. The drug inhibits TGF-beta stimulated collagen synthesis without impairing cell viability in cultured fibroblasts [24]. In hamster studies, oral pirfenidone that was administered after lung inflammation was initiated reduced bleomycin-induced lung fibrosis [25].
In human studies, pirfenidone has been investigated in treatment for idiopathic pulmonary fibrosis (IPF). In 2005, Azuma et al. published the results of a double-blind, placebo-controlled trial of pirfenidone in 107 IPF patients [26]. Secondary endpoints of this study, including change in vital capacity at 9 months and episodes of acute exacerbation, demonstrated the potential benefits of pirfenidone in individuals with IPF. A 52-week multi-center, randomized, double-blind Japanese study enrolled 275 IPF patients, who received high-dose (1800 mg/day) or low-dose (1200 mg/day) pirfenidone or placebo [27]. Before unblinding, the primary outcome parameter was revised, and the trial showed that change in vital capacity at 52 weeks was significantly worse in the placebo group compared to the high-dose pirfenidone group. Two large multi-national placebo-controlled clinical trials investigating pirfenidone for treatment of IPF have also been conducted (i.e., CAPACITY-1, CAPACITY-2). Subjects in these trials had mild to moderate IPF. The highest dose of pirfenidone in either trial was 801 mg t.i.d., i.e., equivalent to the dose used in our trial. The primary endpoint was change in percent of predicted forced vital capacity at week 72. In CAPACITY 2, but not CAPACITY 1, mean decline in percent predicted FVC from baseline in the highest dose group was significantly reduced compared with that of placebo, and significant differences in progression-free survival time were found between the two groups [28]. Pirfenidone is approved for treatment of IPF in Japan, and recently received approval in India, but not in the United States.
For HPS pulmonary fibrosis, pirfenidone has been studied in a single randomized, double-blind, placebo-controlled clinical trial involving 21 subjects [18]. This study showed that subjects with an initial forced vital capacity between 50% and 75% of predicted who received pirfenidone lost forced vital capacity at a significantly slower rate than those in the placebo group (p<0.022). However, using the entire data set, there was no significant difference between the pirfenidone and placebo groups.
To investigate pirfenidone in treatment for mild to moderate HPS pulmonary fibrosis, we conducted a trial that enrolled subjects with a forced vital capacity of 51–85% of predicted. The study was terminated due to futility at its first interim analysis, which was performed 12 months after enrollment of the first 30 subjects. There are several possible explanations for this outcome, but the main issue is that the placebo group did not progress as rapidly as anticipated. In this study, the placebo group lost forced vital capacity at a rate of 2.5% of predicted per year. Given this slow rate of decline, it would not have been possible to demonstrate a significant difference in rate of decline of forced vital capacity between the pirfenidone and placebo groups even if pirfenidone completely halted the progression of pulmonary fibrosis. Another issue in our study was the withdrawal of subjects due to death from progressive pulmonary fibrosis and personal circumstances.
Although it was not possible to determine whether or not pirfenidone is beneficial in treatment for HPS pulmonary fibrosis, this study provided information about the safety of pirfenidone and the natural history of mild to moderate HPS pulmonary fibrosis. Pirfenidone is associated with relatively few and mild side effects in patients with HPS pulmonary fibrosis. In this cohort, pirfenidone-specific side effects were limited to a photosensitivity rash and possibly an elevated creatine phosphokinase. The rash was treatable with high-caliber sun block or topical steroids. In addition, this study demonstrated that the natural history of mild to moderate HPS pulmonary fibrosis differs from that of severe HPS pulmonary fibrosis. The rate of decline in lung function of patients with HPS pulmonary fibrosis and forced vital capacity more than 70% of predicted is less than that of patients with a forced vital capacity less than 50% predicted, who generally die of end-stage lung disease in approximately two years unless they receive a lung transplant (18).
The results of this study also highlight important issues that are relevant to conducting clinical trials focusing on pulmonary fibrosis. There is a need to identify suitable primary endpoints, because changes in lung function only grossly assess the therapeutic response of individuals with pulmonary fibrosis, especially those with early stage disease. Identification of biomarkers that accurately measure molecular and cellular changes in the lung in pulmonary fibrosis is needed. Studying HPS-1 pulmonary fibrosis is advantageous, because it is a monogenic and etiologically homogeneous disorder. Specifically, HPS-1 can serve as a model for understanding the causes and treatments of other types of pulmonary fibrosis; the existence of animal models for HPS pulmonary fibrosis provides a system in which to investigate these topics [29, 30]. Finally, since multiple clinical trials investigating single-drug therapy for pulmonary fibrosis have been unsuccessful, it is possible that pulmonary fibrosis may need to be treated with a multidrug regimen to target multiple pathways that contribute to fibrosis [31]. Further studies addressing these issues are indicated.
Acknowledgments
We would like to acknowledge the efforts of the Clinical Center pharmacists Judy Starling and George Grimes of the Pharmaceutical Development Service. We thank the members of the Hermansky Pudlak syndrome network for their support, and most importantly, we thank our patients for their contributions to this research. This study was supported by the Intramural Research Programs of the National Human Genome Research Institute, the Eunice Kennedy Shriver National Institute of Child Health & Human Development, and the Clinical Center, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement
The authors have no conflict of interest regarding this work.
References
- 1.Hermansky F, Pudlak P P. Albinism associated with hemorrhagic diathesis and unusual pigmented reticular cells in the bone marrow: Report of two cases with histochemical studies. Blood. 1959;14:162–169. [PubMed] [Google Scholar]
- 2.Gahl WA. GeneReviews at GeneTests: Medical Genetics Information Resource [database online]. Copyright. Seattle: University of Washington; 1997–2007. Hermansky-Pudlak Syndrome. (updated 2010), Available at http://www.genetests.org. [Google Scholar]
- 3.Huizing M, Helip-Wooley A, Westbroek W, Gunay-Aygun M, Gahl WA. Disorders of lysosome-related organelle biogenesis: Clinical and molecular genetics. Ann. Rev. Genomics Hum. Genet. 2008;9:59–86. doi: 10.1146/annurev.genom.9.081307.164303. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei ML. Hermansky-Pudlak syndrome: a disease of protein trafficking and organelle function. Pigment Cell Res. 2006;19:19–42. doi: 10.1111/j.1600-0749.2005.00289.x. [DOI] [PubMed] [Google Scholar]
- 5.Hussain N, Quezado M, Huizing M, Geho D, White JG, Gahl W, Mannon P. Intestinal disease in Hermansky-Pudlak syndrome: occurrence of colitis and relation to genotype. Clin. Gastroenterol. Hepatol. 2006;4:73–80. doi: 10.1016/s1542-3565(05)00858-x. [DOI] [PubMed] [Google Scholar]
- 6.Brantly M, Avila NA, Shotelersuk V, Lucero C, Huizing M, Gahl WA. Pulmonary function and high-resolution CT findings in patients with an inherited form of pulmonary fibrosis, Hermansky-Pudlak syndrome, due to mutations in HPS-1 . Chest. 2000;117:129–136. doi: 10.1378/chest.117.1.129. [DOI] [PubMed] [Google Scholar]
- 7.Gahl WA, Brantly M, Kaiser-Kupfer MI, Iwata F, Hazelwood S, Shotelersuk V, Duffy LF, Kuehl EM, Bernardini I. Genetic defects and clinical characteristics of patients with a form of oculocutaneous albinism (Hermansky-Pudlak syndrome) N. Engl. J. Med. 1998;338:1258–1264. doi: 10.1056/NEJM199804303381803. [DOI] [PubMed] [Google Scholar]
- 8.Anderson PD, Huizing M, Claassen DA, White J, Gahl WA. Hermansky-Pudlak syndrome type 4 (HPS-4): clinical and molecular characteristics. Hum. Genet. 2003;113:10–17. doi: 10.1007/s00439-003-0933-5. [DOI] [PubMed] [Google Scholar]
- 9.Witkop CJ, Krumwiede M, Sedano H, White JG. Reliability of absent platelet dense bodies as a diagnostic criterion for Hermansky-Pudlak syndrome. Am. J. Hematol. 1987;26:305–311. doi: 10.1002/ajh.2830260403. [DOI] [PubMed] [Google Scholar]
- 10.Witkop CJ, Babcock MN, Rao GHR, Gaudier F, Summers CG, Shanahan F, Harmon KR, Townsend DW, Sedano HO, King RA, et al. Albinism and Hermansky-Pudlak syndrome in Puerto Rico. Bol. Aso.c Med. 1990;82:333–339. [PubMed] [Google Scholar]
- 11.Oh J, Bailin T, Fukai K, Feng GH, Ho L, Mao JI, Frenk E, Tamura N, Spritz RA. Positional cloning of a gene for Hermansky-Pudlak syndrome, a disorder of cytoplasmic organelles. Nature Genet. 1996;14:300–306. doi: 10.1038/ng1196-300. [DOI] [PubMed] [Google Scholar]
- 12.Anikster Y, Huizing M, White J, Shevchenko YO, Fitzpatrick DL, Touchman JW, Compton JG, Bale SJ, Swank RT, Gahl WA, Toro JR. Mutation of a new gene causes a unique form of Hermansky-Pudlak syndrome in a genetic isolate of central Puerto Rico. Nature Genet. 2001;28:376–380. doi: 10.1038/ng576. [DOI] [PubMed] [Google Scholar]
- 13.Avila NA, Brantly M, Premkumar A, Huizing M, Dwyer A, Gahl WA. Hermansky- Pudlak syndrome: radiography and CT of the chest compared with pulmonary function tests and genetic studies. Am. J. Roentgenol. 2002;179:887–892. doi: 10.2214/ajr.179.4.1790887. [DOI] [PubMed] [Google Scholar]
- 14.Lederer DJ, Kawut SM, Sonnet JR, Vakiani E, Seward SL, White JG, Wilt JS, Marboe CC, Gahl WA, Arcasoy SM. Successful bilateral lung transplantation for pulmonary fibrosis associated with the Hermansky-Pudlak syndrome. J. Heart Lung Transplant. 2005;24:1697–1699. doi: 10.1016/j.healun.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Iyer SN, Gurujeyalakshmi G, Giri SN. Effects of pirfenidone on procollagen gene expression at the transcriptional level in bleomycin hamster model of lung fibrosis. J. Pharmacol. Exp. Ther. 1999;289:211–218. [PubMed] [Google Scholar]
- 16.Kehrer JP, Margolin SB. Pirfenidone diminishes cyclophosphamide-induced lung fibrosis in mice. Toxicol. Lett. 1997;90:125–132. doi: 10.1016/s0378-4274(96)03845-3. [DOI] [PubMed] [Google Scholar]
- 17.Raghu G, Johnson WC, Lockhart D, Mageto Y. Treatment of idiopathic pulmonary fibrosis with a new antifibrotic agent, pirfenidone: results of a prospective, open-label P hase II study. Am. J. Respir. Crit. Care Med. 1999;159:1061–1069. doi: 10.1164/ajrccm.159.4.9805017. [DOI] [PubMed] [Google Scholar]
- 18.Gahl WA, Brantly M, Troendle J, Avila NA, Padua A, Montalvo C, Cardona H, Calis KA, Gochuico B. Effect of pirfenidone on the pulmonary fibrosis of Hermansky-Pudlak syndrome. Mol. Genet. Metab. 2002;76:234–242. doi: 10.1016/s1096-7192(02)00044-6. [DOI] [PubMed] [Google Scholar]
- 19.Gochuico BR, Avila NA, Chow CK, Novero LJ, Wu HP, Ren P, MacDonald SD, Travis WD, Stylianou MP, Rosas IO. Progressive preclinical interstitial lung disease in rheumatoid arthritis. Arch. Intern. Med. 2008;168:159–166. doi: 10.1001/archinternmed.2007.59. [DOI] [PubMed] [Google Scholar]
- 20.Rosas IO, Yao J, Avila NA, Chow CK, Gahl WA, Gochuico BR. Quantification of HRCT scan findings in populations at risk for pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2010;181:A1115. [Google Scholar]
- 21.Chiang PW, Oiso N, Gautam R, Suzuki T, Swank RT, Spritz RA. The Hermansky- Pudlak syndrome 1 (HPS1) and HPS4 proteins are components of two complexes, BLOC-3 and BLOC-4, involved in the biogenesis of lysosome-related organelles. J. Biol. Chem. 2003;278:20332–20337. doi: 10.1074/jbc.M300090200. [DOI] [PubMed] [Google Scholar]
- 22.Dell'Angelica EC, Shotelersuk V, Aguilar RC, Gahl WA, Bonifacino JS. Altered trafficking of lysosomal proteins in Hermansky-Pudlak syndrome due to mutations in the beta 3A subunit of the AP-3 adaptor. Mol. Cell. 1999;3:11–21. doi: 10.1016/s1097-2765(00)80170-7. [DOI] [PubMed] [Google Scholar]
- 23.Dell'Angelica EC, Ooi CE, Bonifacino JS. Beta3A-adaptin, a subunit of the adaptor-like complex AP-3. J. Biol. Chem. 1997;272:15078–15084. doi: 10.1074/jbc.272.24.15078. [DOI] [PubMed] [Google Scholar]
- 24.Lurton JM, et al. Pirfenidone inhibits the stimulatory effects of pro-fibrotic cytokines on human lung fibroblasts in vitro. Am. J. Respir. Crit. Care Med. 1996;153:A403. [Google Scholar]
- 25.Iyer SN, Hyde DM, Giri SN. Anti-Inflammatory effect of pirfenidone in the bleomycinhamster model of lung inflammation. Inflammation. 2000;24:477–491. doi: 10.1023/a:1007068313370. [DOI] [PubMed] [Google Scholar]
- 26.Azuma A, Nukiwa T, Tsuboi E, Suga M, Abe S, Nakata K, Taguchi Y, Nagai S, Itoh H, Ohi M, Sato A, Kudoh S, for the members of the Research Group for Diffuse Lung Diseases in Japan. Raghu G. Double-blind, placebo-controlled trial of pirfenidone in patients with idiopathic pulmonary fibrosis. Am. J. Resp. Crit. Care Med. 2005;171:1040–1047. doi: 10.1164/rccm.200404-571OC. [DOI] [PubMed] [Google Scholar]
- 27.Taniguchi H, Ebina M, Kondoh Y, Ogura T, Azuma A, Suga M, Taguchi Y, Takahashi H, Nakata K, Sato A, Takeuchi M, Raghu G, Kudoh S, Nukiwa T. Pirfenidone Clinical Study Group in Japan. Pirfenidone in idiopathic pulmonary fibrosis. Eur. Respir. J. 2010;35:821–829. doi: 10.1183/09031936.00005209. [DOI] [PubMed] [Google Scholar]
- 28.Spagnolo P, Del Giovane C, Luppi F, Cerri S, Balduzzi S, Walters EH, D’Amico R, Richeldi L. Non-steroid agents for idiopathic pulmonary fibrosis. Cochrane Database Syst. Rev. 2010;9 doi: 10.1002/14651858.CD003134.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Swank RT, Novak EK, McGarry MP, Rusiniak ME, Feng L. Mouse models of Hermansky Pudlak syndrome: a review. Pigment Cell Res. 1998;11:60–80. doi: 10.1111/j.1600-0749.1998.tb00713.x. [DOI] [PubMed] [Google Scholar]
- 30.Mahavadi P, Korfei M, Henneke I, Liebisch G, Schmitz G, Gochuico BR, Markart P, Bellusci S, Seeger W, Ruppert C, Guenther A. Epithelial stress and apoptosis underlie Hermansky-Pudlak syndrome-associaged interstitial pneumonia. Am. J. Respir. Crit. Care Med. 2010;182:207–219. doi: 10.1164/rccm.200909-1414OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thannickal VJ, Flaherty KR, Martinez FJ, Lynch JP. Idiopathic pulmonary fibrosis: emerging concepts on pharmacotherapy. Expert Opin. Pharmacother. 2004;5:1671–1686. doi: 10.1517/14656566.5.8.1671. [DOI] [PubMed] [Google Scholar]