Abstract
A 35-year-old man developed progressive memory problems and personality changes over the course of 6 months. This amnesia culminated in overt functional impairment as he began getting lost in familiar places and paid his rent multiple times in one day. He then displayed increased aggression and was admitted to hospital after assaulting a family member.
A 35-year-old man developed progressive memory problems and personality changes over the course of 6 months. This amnesia culminated in overt functional impairment as he began getting lost in familiar places and paid his rent multiple times in one day. He then displayed increased aggression and was admitted to hospital after assaulting a family member.
At admission he was found to have right-sided 10th, 11th, and 12th cranial nerve palsies and left-sided supraclavicular lymphadenopathy. He was emotionally labile. His Montreal Cognitive Assessment (MoCA) score was 16/30.
Routine investigation showed a white blood cell (WBC) count of 12.7 × 109/L with neutrophil count of 9.37 × 109/L. The erythrocyte sedimentation rate was 65 mm/h and lactate dehydrogenase was 455 μ/L (208–378). CSF analysis found WBC count 12/mm3 (all mononuclear), no red cells, and elevated protein at 0.87 g/L (0.12–0.45 g/L) with a raised immunoglobulin G (IgG) index suggesting possible intrathecal synthesis of IgG. CSF Gram stain, culture, and cytology were negative and no oligoclonal bands were detected. All other tests for infectious and metabolic causes of encephalopathy were negative.
Antibodies to GAD, LGI1, and Caspr2 (VGKC) and paraneoplastic antibodies, including Hu, Ri, Yo, CRMP5, Ma2, and amphiphysin, were negative. CSF 14-3-3 protein was within normal limits.
Thoracic CT revealed mediastinal and right axillary lymphadenopathy. A brain MRI revealed increased T2 signal and postcontrast enhancement on T1-weighted sequences in the upper pons. An EEG showed intermittent bilateral cerebral dysfunction without asymmetry but no epileptiform abnormalities or periodic phenomena.
A cervical lymph node biopsy diagnosed nodular sclerosing Hodgkin lymphoma (HL), stage IIB. After 2 cycles of treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD), plus dexamethasone as an antiemetic, a repeat MRI showed complete resolution of the pontine lesion. In addition, the patient had substantial improvement of all neurologic symptoms, although he could not remember the majority of his initial hospitalization. At the time of discharge following 6 cycles of ABVD, his MoCA was 27/30. A body FDG-PET approximately 8 months after admission showed a complete radiologic remission of disease. At the time of writing, the patient was living independently in the community and working full-time.
After the recent publication of antibodies against metabotropic glutamate receptor 5 (mGluR5) in 2 patients with HL,1 we examined archived CSF obtained at the time of our patient's presentation (no serum was saved), which proved to be positive for these antibodies (figure).
Figure. Detection of mGluR5 antibodies in CSF.
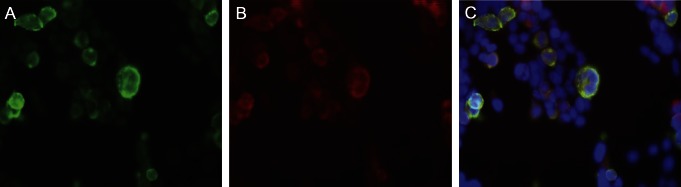
(A) Human embryonic kidney cells transfected with mGluR5 reacted with the patient's CSF antibodies (green reactivity), diluted 1:5. (B) Same cells reacted with a commercial antibody against mGluR5 (red reactivity). (C) Merged reactivities demonstrate that the cells expressing mGluR5 react with both human antibodies and a commercial antibody against mGluR5. The method and technique for antibody determination have been previously reported by Lancaster et al.1
Discussion.
Paraneoplastic encephalitis (PE) in association with HL was first reported in 1982 by Carr,2 who described an insidious neuropsychiatric degeneration in his 15-year-old daughter and how she was diagnosed with Hodgkin disease. This clinical entity is termed the Ophelia syndrome (OS), after Shakespeare's unfortunate Danish maiden.
This case highlights the typical difficulties in diagnosing PE.3 Notably, the initial screen for well-recognized antineuronal antibodies was negative, although the screen for the recently reported anti-mGluR5 was positive. This case, the first detection of anti-mGluR5 antibodies in CSF, supports the accumulating evidence that anti-mGluR5 is implicated in the pathophysiology of PE and could be a useful marker in identifying the syndrome. Given the eminently curable nature of this condition, we would recommend that anti-mGluR5 antibodies are tested for in the serum, CSF, or both in suspected cases of PE.
Glutamate modulates a variety of synaptic responses by activating the metabotropic glutamate receptors. It has been established that mGluR5, expressed primarily in the hippocampus and amygdala, plays a role in behavioral learning and memory.4 The detection of antibodies to mGluR5 in PE cases could explain the typical behavioral and memory problems displayed by these patients.
Our report also demonstrated pontine abnormalities on MRI. According to the most commonly used diagnostic criteria, only mesial temporal lobe lesions on MRI can be considered diagnostic of PE.3 However, this disorder often occurs in association with involvement of other areas of the brain and a variety of nonspecific MRI lesions have been reported in cases of OS.1,5 Given that our patient's brainstem lesion resolved following chemotherapy, it is highly likely that it was directly related to his paraneoplastic syndrome.
While it is theoretically possible for this presentation to have been caused by direct involvement of the CNS by the patient's lymphoma, such metastases are exceedingly rare occurrences and would be unlikely to present in such a fashion. The presentation is more consistent with OS.
OS frequently resolves following treatment of the underlying lymphoma (a much higher cure rate than seen in PE caused by other malignancies) and responds to immunotherapy,1 suggesting that these antibodies are pathogenic and that reduction in tumor burden leads to reduction in the level of circulating autoantibodies. Future studies should focus on determining if this is indeed the case.
Footnotes
Author contributions: Drs. Adler, Mat, and Merwick drafted the manuscript. Drs. Chadwick, Gullo, and Tubridy were involved in critical revision of the manuscript. All the aforementioned authors were involved in the diagnosis and treatment of the patient. Dr. Dalmau performed the CSF analysis for mGluR5 antibodies, and was involved in critical revision of the manuscript.
Study funding: No targeted funding reported.
Disclosure: A. Mat reports no disclosures. H. Adler has received travel grants from Biogen Idec. A. Merwick reports unrestricted educational grants toward travel/accommodation costs for attendance at conferences from Boehringer Ingelheim, Pfizer Healthcare, Lunbeck, and Biogen Idec. G. Chadwick and G. Gullo report no disclosures. J. Dalmau is Professor at Institució Catalana de Recerca i Estudis Avançats (ICREA) in IDIBAPS/Hospital Clínic, Barcelona; has filed a patent application for the use of LGI1 as a diagnostic test; has received royalties from Athena Diagnostics, Inc., for a patent re: Ma2 autoantibody test and has patents pending re: NMDA and GABAB receptor autoantibody tests (license fee payments received from EUROIMMUN AG); and receives research support from funding from EUROIMMUN AG, the NIH/NCI, and a McKnight Neuroscience of Brain Disorders award. N. Tubridy is an advisory board member for Novartis and has received travel grants from Bayer Schering, Novartis, and Sanofi. Go to Neurology.org for full disclosures.
This paper was presented at the Irish Neurology Association annual meeting in Cork in May 2012, winning the award for best poster, and at the Association of British Neurologists annual meeting in Brighton in May 2012, winning the award for best case presentation.
References
- 1.Lancaster E, Martinez-Hernandez E, Titulaer MJ, et al. Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology 2011;77:1698–1701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carr I. The Ophelia syndrome: memory loss in Hodgkin’s disease. Lancet 1982;1:844–845 [DOI] [PubMed] [Google Scholar]
- 3.Gultekin SH, Rosenfeld MR, Voltz R, et al. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain 2000;123:1481–1494 [DOI] [PubMed] [Google Scholar]
- 4.Lu YM, Jia Z, Janus C, et al. Mice lacking metabotropic glutamate receptor 5 show impaired learning and reduced CA1 long-term potentiation (LTP) but normal CA3 LTP. J Neurosci 1997;17:5196–5205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epaulard O, Courby S, Pavese P, et al. Paraneoplastic acute diffuse encephalitis revealing Hodgkin's disease. Leuk Lymphoma 2004;45:2509–2512 [DOI] [PubMed] [Google Scholar]


