Abstract
Purpose The Sauvé-Kapandji (S-K) procedure is now an established treatment option for symptomatic distal radioulnar joint (DRUJ) dysfunction. However, for patients with poor bone quality (frequently as a result of advanced-stage rheumatoid arthritis [RA]), the conventional S-K procedure is difficult to perform without reducing the radioulnar diameter of the wrist, which may result in a loss of grip strength and pain over the proximal ulnar stump. The purpose of this study was to review the radiographic outcomes of patients who underwent a modified S-K procedure that involves rotating the resected ulnar segment 90 degrees and using it to bridge the gap between the sigmoid notch and the ulnar head.
Methods The modified S-K procedure was performed in 29 wrists of 23 patients. Twenty-one patients had severe RA, while two had malunited radius fractures. The mean follow-up period was 43 months (range, 23 to 95). The radiographic evaluation included a measurement of the radioulnar width, the pseudarthrosis gap between the proximal and distal ulnar stump, the radioulnar distance, and the ulnar translation of the carpus.
Results The radioulnar width of the wrist, pseudarthrosis gap, and radioulnar distance were well maintained throughout the period. A postoperative loss in the radioulnar width of the wrists appeared to correlate with a postoperative additional ulnar translocation of the carpus.
Conclusion Narrowing of the radioulnar width of the wrist is a potential cause of progressive ulnar translocation of the carpus. The modified technique for the S-K procedure maintains the distal ulna in the proper position and provides sufficient ulnar support for the carpus. It is a useful reconstruction procedure in patients with severe RA with poor bone quality.
Keywords: modified Sauvé-Kapandji, radiographic evaluation, distal radioulnar joint
Severe arthritis or derangement of the distal radioulnar joint (DRUJ) leads to instability of the DRUJ, and the subluxation of the ulna causes pain on motion, loss of grip strength, and a restriction of forearm rotation.1 A variety of surgical procedures have been described to treat these.2 In 1912, Darrach described a resection of the ulnar head.3 Although this procedure could successfully restore forearm rotation, serious postoperative complications frequently occurred, such as a further loss of grip strength or pain over the proximal ulnar stump.4,5,6 As an alternative solution, Sauvé and Kapandji described a distal radioulnar arthrodesis combined with an intentional pseudarthrosis of the distal ulna.7 Some reports of this technique have shown superior results both clinically and radiographically,8,9,10,11 and hence the Sauvé-Kapandji (S-K) procedure has almost replaced Darrach's as the most common resection arthroplasty for the treatment of DRUJ dysfunction. The conventional S-K procedure is contraindicated, however, in patients with extremely poor bone quality, which is often seen in patients with advanced-stage rheumatoid arthritis (RA).
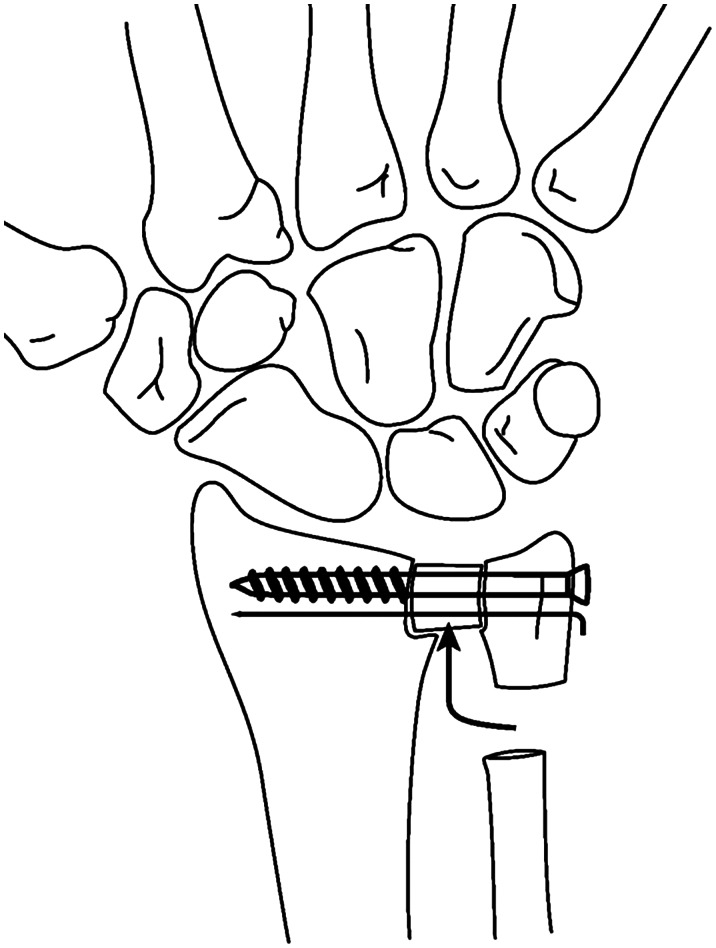
Since 1994, we have modified the S-K procedure for the treatment of patients with a severely damaged DRUJ. This modification involves rotating the resected ulnar segment 90° and inserting it into the DRUJ to form a bridge between the eroded ulnar head and the decorticated ulnar notch of the radius to provide ulnar support as well as to maintain the radioulnar width of the wrist (Fig. 1). The extensor carpi ulnaris (ECU) tendon sheath attachment into the ulnar head and shaft is preserved, providing a dynamic stabilizing effect on the proximal stump.
Fig. 1.
Surgical procedure of the modified Sauvé-Kapandji procedure. The resected ulnar segment is rotated 90° and inserted in the curetted distal radio-ulnar joint in existing form to bridge the thinned ulnar head and the sigmoid notch using a cancellous screw and a Kirschner wire.
The purpose of this study is to review the radiographic findings following the modified S-K procedure to assess its effectiveness at maintaining the radioulnar width of the wrist, controlling ulnar translocation, and maintaining the pseudarthrosis space.
Materials and Methods
A total of 29 wrists in 23 patients who had undergone the modified S-K procedure at our institute and related hospitals between 1994 and 2005 were evaluated (Table 1). There were 21 women and 2 men, and their mean age at the time of operation was 60 years (range, 25 to 77). Twenty-seven wrists in 21 patients had DRUJ dysfunction with severe RA as defined by the American Rheumatism Association.12 Eighteen of the 27 were preoperatively rated as Larsen's radiographic grade 5 (mutilating changes, where the original bony outlines have been destroyed), seven as grade 4 (severe erosions, where there is usually no joint space left and the original bony outlines are partly preserved), and two as grade 3 (marked erosions).13 Two wrists had a degenerative DRUJ due to dislocation of the ulnar head following a malunited radius fracture. The average follow-up period was 43 months (range, 23 to 95). The main indication for surgery was severe wrist pain combined with a limitation in forearm rotation that failed to respond to nonsurgical treatment.
Table 1. Individual patient data: Numbers and words in parentheses indicate the data of the surgery in the other wrist.
| Case | Age (years) | Sex | Side | Cause of arthrosis | Larsen grade | Tendon transfer | Follow-up (months) |
|---|---|---|---|---|---|---|---|
| 1 | 73 | F | R | RA | 3 | − | 26 |
| 2 | 32 | F | L | RA | 4 | + | 25 |
| 3 | 75 | F | R | OA | + | 48 | |
| 4 | 77 | F | R | RA | 5 | − | 24 |
| 5 | 51(53) | F | R(L) | RA | 5(5) | +(+) | 48(26) |
| 6 | 24 | F | L | RA | 5 | + | 25 |
| 7 | 59 | F | R | RA | 4 | + | 24 |
| 8 | 58 | F | R | RA | 5 | + | 25 |
| 9 | 76 | F | R | OA | − | 24 | |
| 10 | 33 | F | R | RA | 5 | + | 26 |
| 11 | 67(68) | F | R(L) | RA | 5(5) | +(+) | 35(24) |
| 12 | 64 | F | R | RA | 4 | + | 46 |
| 13 | 76(76) | F | R(L) | RA | 5(5) | +(+) | 27 |
| 14 | 70(71) | F | L(R) | RA | 4(5) | +(+) | 70(58) |
| 15 | 56 | F | R | RA | 5 | + | 71 |
| 16 | 63 | F | R | RA | 5 | + | 58 |
| 17 | 61(64) | F | R(L) | RA | 3(5) | +(+) | 95(46) |
| 18 | 42 | F | R | RA | 5 | + | 59 |
| 19 | 53 | M | R | RA | 5 | + | 33 |
| 20 | 59 | F | R | RA | 4 | + | 46 |
| 21 | 56 | F | L | RA | 4 | + | 61 |
| 22 | 56(59) | F | R(L) | RA | 5(4) | +(+) | 60(34) |
| 23 | 54 | M | R | RA | 5 | + | 91 |
Abbreviations: OA, osteoarthritis; RA, rheumatoid arthritis.
Surgical Technique
All procedures were performed under general anesthesia with tourniquet control. The patient was positioned supine with the arm on a hand table. The DRUJ was exposed through a dorsal skin incision. Care was taken to avoid injury to the dorsal sensory branch of the ulnar nerve. The extensor retinaculum was entered between the fourth and fifth extensor compartments, and the capsule was incised and reflected to the radial side as a rectangular flap. A thorough synovectomy of the DRUJ was performed, and the ulnar notch of the radius and the ulnar head were decorticated. A subperiosteal dissection was used to expose the distal ulna, and an osteotomy of the ulna was performed at 10–20 mm and 20–30 mm proximal to the distal end with an oscillating saw, excising a 10-mm-long segment of the ulna. This resected bone segment was rotated 90°, inserted into the DRUJ to bridge the gap between the ulnar head and the ulnar notch of the radius, and fixed with a cancellous screw and a Kirschner wire (K-wire). If the ECU tendon was dislocated palmarly, the tendon sheath was reconstructed using a periosteal sleeve, which was also wrapped around and sutured to the proximal ulnar stump. The patient's arm was immobilized in a long-arm plaster cast in neutral forearm rotation for 3 to 4 weeks, followed by gentle active wrist motion. Tendon transfers were performed in 26 wrists of 20 patients who had ruptures of the extensor digitorum communis or the extensor digiti minimi. One patient underwent a concomitant carpal tunnel release.
Radiographic Evaluation
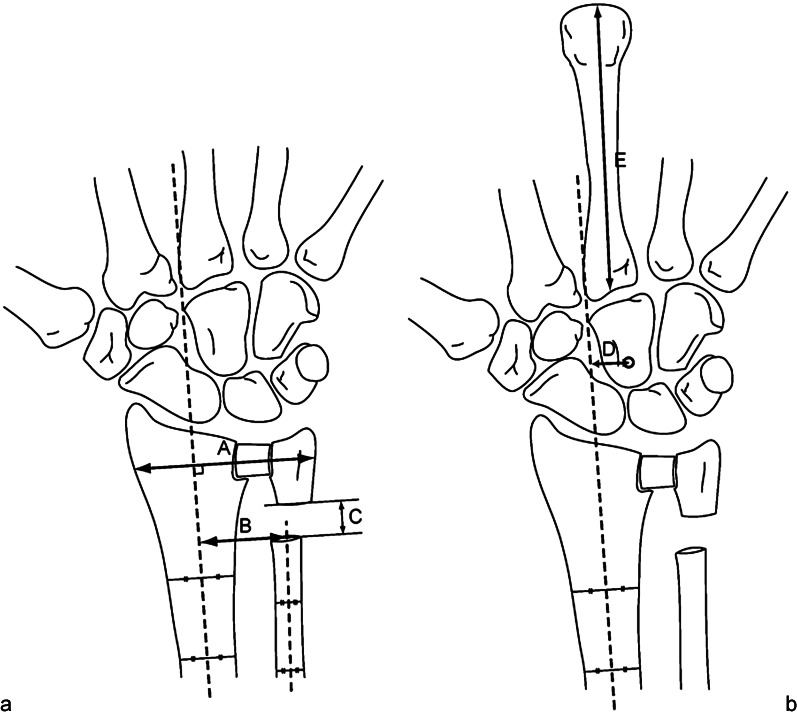
Static posteroanterior X-ray images of the wrists in neutral position were taken before and after the operation until the final follow-up. The radiographic evaluation included a measurement of the radioulnar width of the wrist 5 mm proximal to the distal edge of the ulnar head, the pseudarthrosis gap between the proximal and distal ulnar stump, the radioulnar distance between the radius and the proximal ulnar stump, and the ulnar translation of the carpus (Fig. 2). We measured the distance between the long axes of the radius and ulna to eliminate any influence of the shape of the proximal ulnar stump. The longitudinal axis of the radius was determined by bisecting the distance between the radial and ulnar cortices at 4 cm and 6 cm proximal to the tip of the radial styloid, and the ulnar axis was obtained by bisection of the ulnar shaft at 2 cm and 4 cm proximal to the ulnar stump. The preoperative radioulnar distance was measured at the same level of proximal stump to compare the distances between before and after the operation.
Fig. 2.
Radiographic parameters of posteroanterior view. (a) A, width of wrist at 5 mm proximal to distal end of ulnar head. B, radioulnar distance between the axis of radial and ulnar shaft at the level of ulnar stump. C, gap of ulnar stump measured along to the longitudinal axis of distal radius. (b) Ulnar translation index = D/E. D, distance between a longitudinal axis of the distal radius and the center of proximal capitate. E, length of the middle finger metacarpal. (This index normally measures 0.09 ± 0.02 according to DiBenedetto et al14).
Each parameter was measured three times using ImageJ software (National Institutes of Health), and the averaged values were compared pre- and postoperatively. The degree of ulnar translation of the carpus was calculated according to the ulnar translation index (UTI) method of DiBenedetto et al.14 This is calculated as a ratio of the distance between the center of the proximal capitate and the long axis of the distal radius to the length of the middle metacarpal bone. The normal value is 0.09 ± 0.02.
Statistical Analysis
A statistical analysis was performed using Pearson's correlation coefficients, and a one-way analysis of variance (ANOVA) was applied to determine the significance of any difference between the means, with the cutoff for significance of p = 0.05.
Results
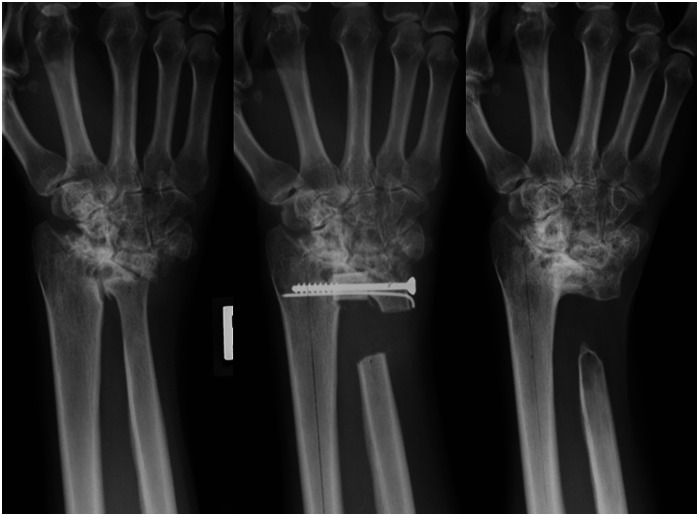
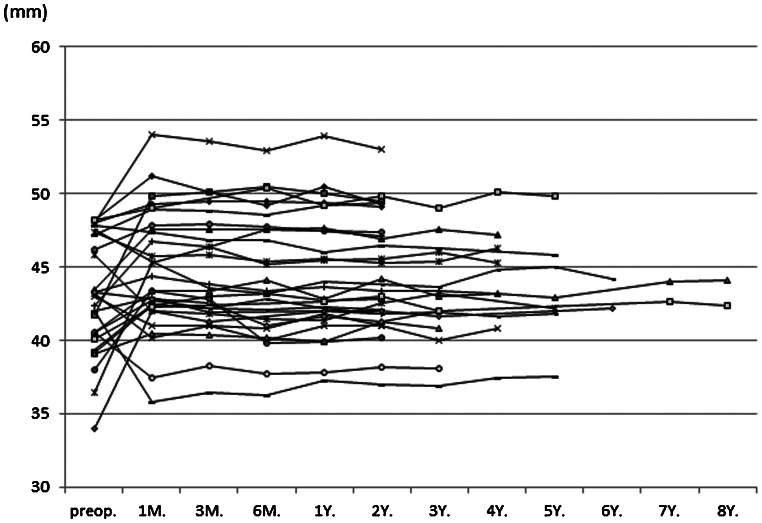
Bony union was achieved within 8 weeks after surgery for all patients. The DRUJ appeared stable radiographically at the final follow-up (Fig. 3). One of two wrists in Larsen grade 3 (marked erosions) and five of seven wrists rated as a Larsen grade 4 (severe erosions, where there is usually no joint space left and the original bony outlines are partly preserved), showed radiological progression to a Larsen grade 5 (mutilating changes, where the original bony outlines have been destroyed). The mean value of the width of the wrist was 43.0 ± 3.8 mm preoperatively, 44.6 ± 4.1 mm at 1 month after the operation, and 44.4 ± 3.8 mm at the time of the final radiographic follow-up. The radioulnar width of the wrist increased in 21 cases and decreased in 8 of 29 wrists (mean 1.6 ± 3.7 mm) compared with the preoperative width of the wrist. A reduction in the width by more than 3.0 mm was found in two wrists (cases 22-R and 19), possibly due to overtightening of the screws. Postoperatively, the width of the wrist was well maintained in all cases throughout the follow-up period (Fig. 4).
Fig. 3.
Serial radiographic images of a 51-year-old woman (case 5-R) before and after the modified Sauvé-Kapandji procedure. Left: Preoperative. Middle: 2 weeks after the operation. Right: 4 years after the operation.
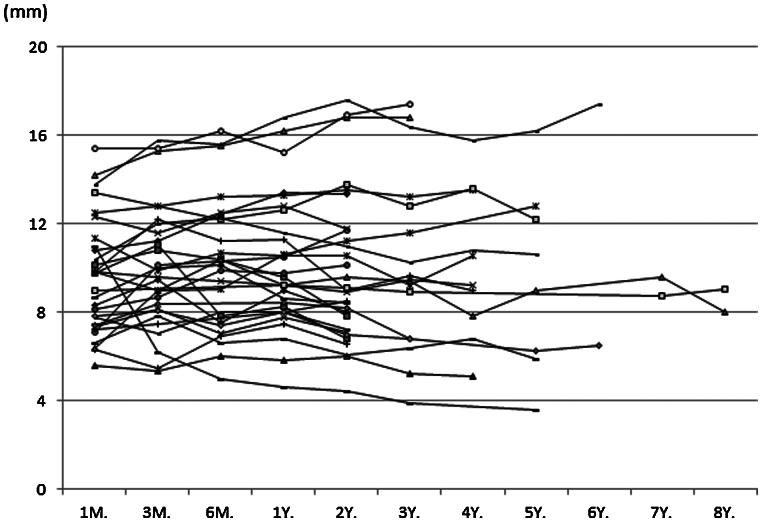
Fig. 4.
Temporal change of the width of the wrist. M, month; Y, year.
The mean ulnar gap was 9.6 ± 2.6 mm at 1 month after the operation and 9.7 ± 3.6 mm at the time of final follow-up (Fig. 5). In all except one case (case 14-L), the ulnar gap was well maintained until the final follow-up. In case 14-L, callus formation was observed at the tip of the proximal ulnar stump, but no bridging bone was noted.
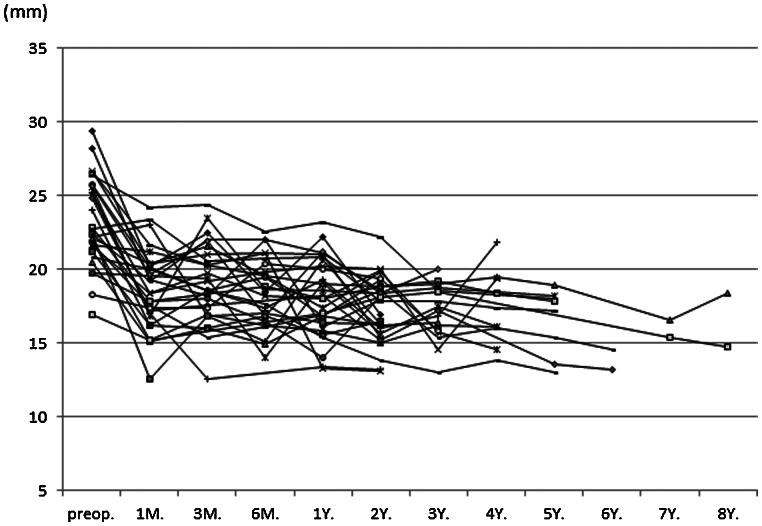
Fig. 5.
Temporal change of the gap between the proximal and distal ulnar stump. M, month; Y, year.
The mean radioulnar distance was 23.2 ± 3.0 mm preoperatively, 18.7 ± 2.7 mm 1 month after the surgery, and 16.8 ± 2.3 mm at the final follow-up (Fig. 6). This was a significant decrease between the pre- and postoperative values (p < 0.01), but the additional radial shift of the proximal ulnar stump was relatively small (1.9 ± 3.5 mm). Neither the immediate nor additional radial shift correlated significantly with the postoperative width of the wrists (immediate shift, r = –0.292, p = 0.12; additional shift, r = +0.037, p = 0.84). There was no obvious impingement or scalloping of the radius between the proximal stump and radial shaft on the static X-ray views, but stress views were not taken.
Fig. 6.
Temporal change of the distance between the axes of the radius and the ulna at the level of proximal ulnar stump. M, month; Y, year.
The mean UTI was 0.169 ± 0.070 preoperatively, 0.172 ± 0.064 at 1 month after the surgery, and 0.189 ± 0.067 at the final follow-up (Fig. 7), showing a slight but not significant increase (p = 0.99, p = 0.86). The postoperative change in the width of wrists and the carpal translation did not show any statistical correlation (r = –0.244, p = 0.20), and the postoperative width of wrists did not affect the additional carpal translation (r = –0.238, p = 0.21). However, the postoperative loss in the width compared with preoperative width of wrists had a possible correlation with the additional ulnar translation (r = –0.385, p = 0.03) (Fig. 8).
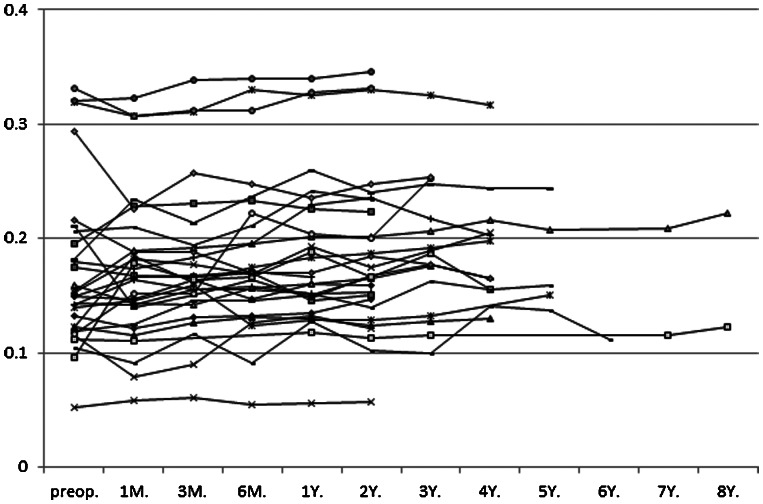
Fig. 7.
Temporal change of ulnar translation index. M, month; Y, year.
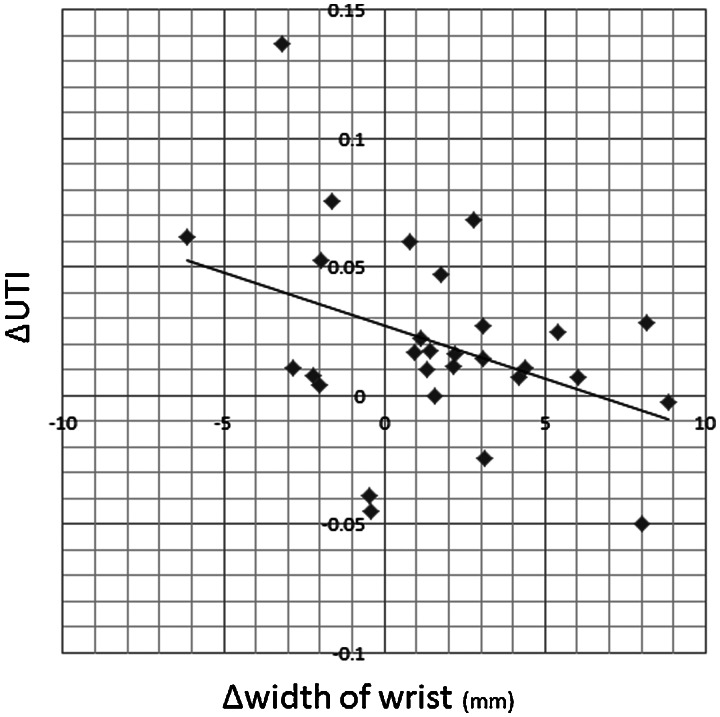
Fig. 8.
Correlation between the loss of the width of the wrist and the postoperative ulnar translation of the carpus. ΔUTI, preoperative value – final follow-up value; Δwidth of wrist, preoperative value – value at 1 month after the operation.
Discussion
The Darrach procedure is one of the most established treatment options for symptomatic DRUJ dysfunction. However, because of poor results reported in the young and in active patients, the procedure is now mostly limited to low-demand elderly patients.15,16,17,18,19,20 The major drawback of the Darrach procedure is the loss of grip strength, which Minami et al reported to be decreased by 25% postoperatively.21
The advantage of the S-K procedure compared with the Darrach procedure is that it can preserve the ulnocarpal joint. The distal end of the ulna is a key structural constituent in the stability of the wrist. It provides the osseous support for the ulnar carpus, which transmitted up to 34% of the axial load in one cadaver study.22 The ulnar head also provides an attachment point for the ligamentous stabilizers of the ulnocarpal joint and DRUJ, which include the ulnocarpal ligaments and the triangular fibrocartilage complex.23 Furthermore, the ulnar head behaves as a pulley for the ECU tendon, which is the most important dynamic stabilizer of the wrist.24 Releasing the ECU subsheath from its attachment on the distal ulna increases the excursion of the ECU tendon and can decrease the grip strength.25 Thus, the ulnar head must be maintained in the proper position to preserve a physiologic pattern of force transmission from the hand to the forearm. This may be a contributing factor in the superior improvements in grip strength following an S-K procedure as compared with a Darrach procedure in rheumatoid wrists.20,26 Poor bone quality, such as bony erosion of the ulnar notch of the radius in RA patients, results in a narrowing of the radioulnar width of the wrist with insufficient ulnocarpal wrist support, which is commonly considered a contraindication to the S-K procedure.27
In 2006, Fujita et al reported satisfactory results28 with a modification of the S-K procedure in which the distal part of the ulna, including the ulnar head, were resected and rotated 90°, then mounted on the ulnar notch of the radius as an artificial radial shelf. The shelf provided sufficient osseous support for the ulnar carpus and successfully prevented additional ulnar translation, even in patients with poor bone stock. The ECU sheath was resected in their modification; thus, no stabilizing effect by the ECU was expected. In our modification, we used the resected ulnar shaft to bridge a gap in the DRUJ and were able to maintain the width of the wrist in most cases, even in the RA patients who were preoperatively rated as Larsen grade 5 (mutilating changes, where the original bony outlines have been destroyed on plain radiograph).
In this study, bony union was observed within 8 weeks with our modified S-K procedure. Radiographic evaluation indicated that the width of the wrist was unchanged throughout the follow-up period. The pseudarthrosis was well maintained, with only one case of callus formation in the gap. The radioulnar distance, however, decreased from 23.2 ± 3.0 mm preoperatively to 18.7 ± 2.7 mm 1 month after the surgery, and 16.8 ± 2.3 mm at the final follow-up. Although there was no radiographically obvious radioulnar impingement between the proximal stump and the radial shaft, this finding may change with longer-term follow-up. The ulnar translation of the carpus was increased slightly. We found that postoperative loss in the width of wrists with respect to the preoperative width in the S-K procedure had a possible correlation with increased ulnar translation. This finding suggests that the surgeon must be careful to keep the original width of the wrist to avoid progressive ulnar translation of the carpus.
In conclusion, this modified technique of the S-K procedure could provide sufficient ulnar support for the carpus, and it was a useful reconstruction procedure even in patients with poor bone quality in the DRUJ.
Acknowledgments
The authors thank Yoshihiko Morikawa and Mari Sasaki, MD, Tokyo Metropolitan Children's Medical Center, Tokyo, Japan, for their constant interest and guidance in this investigation.
Footnotes
Conflict of Interest None
References
- 1.Backdähl M. The caput ulnae syndrome in rheumatoid arthritis. A study of the morphology, abnormal anatomv and clinical picture. Acta Rheumatol Scand Suppl. 1963;5:1–75. [PubMed] [Google Scholar]
- 2.Vesely D G. The distal radio-ulnar joint. Clin Orthop Relat Res. 1967;51:75–91. [PubMed] [Google Scholar]
- 3.Darrach W. Anterior dislocation of the head of the ulna. Ann Surg. 1912;56:802–803. [Google Scholar]
- 4.Rana N A, Taylor A R. Excision of the distal end of the ulna in rheumatoid arthritis. J Bone Joint Surg Br. 1973;55(1):96–105. [PubMed] [Google Scholar]
- 5.Newman R J. Excision of the distal ulna in patients with rheumatoid arthritis. J Bone Joint Surg Br. 1987;69(2):203–206. doi: 10.1302/0301-620X.69B2.3818749. [DOI] [PubMed] [Google Scholar]
- 6.Van Gemert A ML, Spauwen P HM. Radiological evaluation of the long-term effects of resection of the distal ulna in rheumatoid arthritis. J Hand Surg [Br] 1994;19(3):330–333. doi: 10.1016/0266-7681(94)90082-5. [DOI] [PubMed] [Google Scholar]
- 7.Sauvé L, Kapandji M. Nouvelle technique de traitement chirurgical des luxations recidivantes isolees de l'extremite inferieure du cubitus. J Chir (Paris) 1936;47:589–594. [Google Scholar]
- 8.Gonçalves D. Correction of disorders of the distal radio-ulnar joint by artificial pseudarthrosis of the ulna. J Bone Joint Surg Br. 1974;56B(3):462–464. [PubMed] [Google Scholar]
- 9.Kapandji I A. The Kapandji-Sauvé operation. Its techniques and indications in non rheumatoid diseases. Ann Chir Main. 1986;5(3):181–193. doi: 10.1016/s0753-9053(86)80057-6. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura R, Tsunoda K, Watanabe K, Horii E, Miura T. The Sauvé-Kapandji procedure for chronic dislocation of the distal radio-ulnar joint with destruction of the articular surface. J Hand Surg [Br] 1992;17(2):127–132. doi: 10.1016/0266-7681(92)90071-9. [DOI] [PubMed] [Google Scholar]
- 11.Minami A, Suzuki K, Suenaga N, Ishikawa J. The Sauvé-Kapandji procedure for osteoarthritis of the distal radioulnar joint. J Hand Surg Am. 1995;20(4):602–608. doi: 10.1016/s0363-5023(05)80276-x. [DOI] [PubMed] [Google Scholar]
- 12.Arnett F C, Edworthy S M, Bloch D A. et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 13.Larsen A. Radiological grading of rheumatoid arthritis. An interobserver study. Scand J Rheumatol. 1973;2(3):136–138. doi: 10.3109/03009747309098833. [DOI] [PubMed] [Google Scholar]
- 14.DiBenedetto M R, Lubbers L M, Coleman C R. A standardized measurement of ulnar carpal translocation. J Hand Surg Am. 1990;15(6):1009–1010. doi: 10.1016/0363-5023(90)90035-p. [DOI] [PubMed] [Google Scholar]
- 15.Bell M J, Hill R J, McMurtry R Y. Ulnar impingement syndrome. J Bone Joint Surg Br. 1985;67(1):126–129. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 16.Bieber E J, Linscheid R L, Dobyns J H, Beckenbaugh R D. Failed distal ulna resections. J Hand Surg Am. 1988;13(2):193–200. doi: 10.1016/s0363-5023(88)80047-9. [DOI] [PubMed] [Google Scholar]
- 17.Lichtman D M, Ganocy T K, Kim D C. The indications for and techniques and outcomes of ablative procedures of the distal ulna. The Darrach resection, hemiresection, matched resection, and Sauvé-Kapandji procedure. Hand Clin. 1998;14(2):265–277. [PubMed] [Google Scholar]
- 18.Fraser K E, Diao E, Peimer C A, Sherwin F S. Comparative results of resection of the distal ulna in rheumatoid arthritis and post-traumatic conditions. J Hand Surg [Br] 1999;24(6):667–670. doi: 10.1054/jhsb.1999.0288. [DOI] [PubMed] [Google Scholar]
- 19.Lee S K, Hausman M R. Management of the distal radioulnar joint in rheumatoid arthritis. Hand Clin. 2005;21(4):577–589. doi: 10.1016/j.hcl.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Rizzo M, Cooney W P III. Current concepts and treatment for the rheumatoid wrist. Hand Clin. 2011;27(1):57–72. doi: 10.1016/j.hcl.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Minami A, Iwasaki N, Ishikawa J, Suenaga N, Yasuda K, Kato H. Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures. Hand Surg. 2005;10(2-3):243–248. doi: 10.1142/S0218810405002942. [DOI] [PubMed] [Google Scholar]
- 22.Shaaban H, Giakas G, Bolton M, Williams R, Scheker L R, Lees V C. The distal radioulnar joint as a load-bearing mechanism—a biomechanical study. J Hand Surg Am. 2004;29(1):85–95. doi: 10.1016/j.jhsa.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 23.Nakamura T, Yabe Y, Horiuchi Y. Functional anatomy of the triangular fibrocartilage complex. J Hand Surg [Br] 1996;21(5):581–586. doi: 10.1016/s0266-7681(96)80135-5. [DOI] [PubMed] [Google Scholar]
- 24.Spinner M, Kaplan E B. Extensor carpi ulnaris. Its relationship to the stability of the distal radio-ulnar joint. Clin Orthop Relat Res. 1970;68:124–129. [PubMed] [Google Scholar]
- 25.Tang J B, Ryu J, Kish V. The triangular fibrocartilage complex: an important component of the pulley for the ulnar wrist extensor. J Hand Surg Am. 1998;23(6):986–991. doi: 10.1016/S0363-5023(98)80004-X. [DOI] [PubMed] [Google Scholar]
- 26.Nakagawa N, Abe S, Kimura H, Imura S, Nishibayashi Y, Yoshiya S. Comparison of the Sauvé-Kapandji procedure and the Darrach procedure for the treatment of rheumatoid wrists. Mod Rheumatol. 2003;13:239–242. doi: 10.3109/s10165-003-0229-6. [DOI] [PubMed] [Google Scholar]
- 27.Slater R R. The Sauve-Kapandji procedure. J Hand Surg Am. 2008;33:1632–1638. doi: 10.1016/j.jhsa.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 28.Fujita S Masada K Takeuchi E Yasuda M Komatsubara Y Hashimoto H Modified Sauve-Kapandji procedure for disorders of the distal radioulnar joint in patients with rheumatoid arthritis. Surgical technique J Bone Joint Surg Am 200688(Suppl 1 Pt 1):24–28. [DOI] [PubMed] [Google Scholar]