Abstract
Distal radioulnar joint (DRUJ) problems can occur as a result of joint instability, abutment, or incongruity. The DRUJ is a weight-bearing joint; the ulnar head is frequently excised either totally or partially, and in some cases it is fused, because of degenerative, rheumatoid, or posttraumatic arthritis. Articles about these procedures report the ability to pronate and supinate, but they rarely discuss grip strength, and even less do they address lifting capacity. We report the long term results of the first 35 patients who underwent total DRUJ arthroplasty with the Aptis DRUJ prosthesis after 5 years follow-up. Surgical indications were all causes of dysfunctional DRUJ (degenerative, posttraumatic, autoimmune, congenital). We recorded data for patient demographics, range of motion (ROM), strength, and lifting capacity of the operated and of the nonoperated extremity. Pain and functional assessments were also recorded. The Aptis DRUJ prosthesis, a bipolar self-stabilizing DRUJ endoprosthesis that restores forearm function, consists of a semiconstained and modular implant designed to replace the function of the ulnar head, the sigmoid notch of the radius, and the triangular fibrocartilage ligaments. The surgical technique is presented in detail. The majority of the patients regained adequate ROM and improved their strength and lifting capacity to the operated side. Pain and activities of daily living were improved. Twelve patients experienced complications, most commonly being extensor carpi ulnaris (ECU) tendinitis, ectopic bone formation, bone resorption with stem loosening, low-grade infection, and need for ball replacement. The Aptis total DRUJ replacement prosthesis is an alternative to salvage procedures that enables a full range of motion as well as the ability to grip and lift weights encountered in daily living activities.
Keywords: distal radioulnar joint, wrist prosthesis, wrist arthritis
The function of the forearm is well known, but this knowledge is seldom used when selecting a procedure to repair a dysfunctional distal radioulnar joint (DRUJ). The head of the ulna is frequently excised and not replaced.1,2,3
The two long bones of the forearm, the radius and the ulna, are connected through the radioulnar joint, a bicondylar pivot-type joint that is divided into a proximal and a distal half. The DRUJ is half of a bicondylar forearm joint, with its condyle, the head of the ulna, articulating with the sigmoid notch of the distal radius. Conversely, the proximal radioulnar joint has its condyle, the head of the radius, articulating with the lesser sigmoid notch in the proximal ulna.4 The DRUJ has a central role in lifting. Acting against gravity to lift an object, a transverse force runs from the hand/wrist to the radius and from there to the ulnar head. The ulna has the function of supporting the radius, which is connected to the ulna by the annular ligament and the triangular fibrocartilage complex (TFCC).5,6
The pathologies affecting the distal radioulnar joint include posttraumatic, degenerative, rheumatoid, and inflammatory arthritis; tumors; and congenital anomalies. Posttraumatic arthritis is most commonly the result of distal radius fractures, but it is also the result of untreated DRUJ instability. The patient with DRUJ pathology presents with pain on the ulnar side of the wrist, exacerbated by lifting even small objects. Those affected with Madelung deformity and with Ehlers-Danlos syndrome become symptomatic after puberty.
Historically, irreparable damage to the distal radioulnar joint has been treated by excision or fusion.1,2,3,7 The most common complication of these procedures is painful impingement between the radius and the remaining ulna, which may be much more symptomatic in active patients8,9,10 (Fig. 1).
Fig. 1.

Twenty-two-year-old female patient with painful impingement following Sauvé-Kapandji procedure.
Partial or complete excision of the ulnar head leads to dynamic impingement, which is painful in the majority of patients. It is important to reevaluate decisions to perform procedures that remove part or all of the ulnar head. Excision of the ulna should be avoided at any cost. There are three procedures that can help to restore function to the forearm: osteotomy of the radius or ulna, ligament reconstruction, and DRUJ implants, either partial- or total-replacement. This article discusses our experience with a semiconstrained implant, our technique, and results.
Patients and Methods
A retrospective analysis was conducted on all DRUJ prostheses implanted at our center from 2005 to 2011. The project was approved by the Institutional Review Board of the University of Louisville. During this period, 284 patients were treated with implantation of the DRUJ prosthesis. We followed, for a period of 5 years, the first 35 patients who underwent total DRUJ arthroplasty with the Aptis DRUJ prosthesis. These patients underwent surgery between March and December 2005. One patient received bilateral arthroplasties, totaling 36 DRUJ arthroplasties performed in 2005. Currently 260 patients are enrolled in the study and being evaluated for the long-term results of DRUJ implant.
Surgical indications were patients with mature skeletons who had rheumatoid, congenital, degenerative, or posttraumatic arthritis of the DRUJ and who may or may not have already had surgical treatment at the same wrist. All of these conditions caused decreased range of motion and painful/dysfunctional DRUJ.
Included in the study were 21 female and 14 male patients with a mean age of 44 years (range 23–74). 18 implants were inserted into the right wrist and 17 into the left. 19 patients had the operation in their dominant hands.
Preoperative patient assessment was performed with clinical examination and radiographic examination. Two specific tests are particularly important when addressing DRUJ congruity and stability. The best way to evaluate the integrity or the derailment of the DRUJ is to place the hands of the examiner at mid-forearm of the patient with the elbow flexed at 90° and ask the patient to resist downward forces exerted by the examiner, while the patient is pronating and supinating the forearm. The applied force is loaded against the radioulnar joint; by grinding the seat of the ulna against the sigmoid notch, this maneuver recreates the pain. When the distal radioulnar joint is involved in pathological conditions, the patient is unable to resist with the affected arm (Fig. 2).
Fig. 2.

The painful left DRUJ limits the patient's strength to resist the downward force applied by the examiner.
The second test assesses the stability of the DRUJ. The patient places the elbow on the examining table with the forearm in an upright position. The examiner applies a shear force between the radius and the ulna with the forearm in full pronation and full supination. The amount of displacement, if any, between the radius and the ulna shows the integrity of the palmar and dorsal radioulnar ligaments. Always compare the test results with the contralateral side to determine the accuracy of the tests.
Plain radiographs in anteroposterior (AP) and lateral views are useful in diagnosing DRUJ pathologies. On occasions there is need of a computed tomography (CT) scan to confirm the diagnosis.
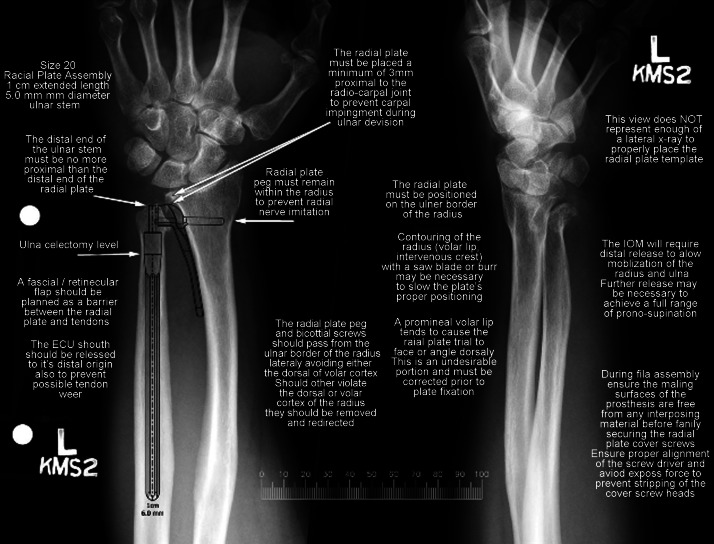
If prosthesis is contemplated, preoperative graded X-ray images of wrist and forearm are used to determine the size of the prosthesis that is required for each individual case (Fig. 3).
Fig. 3.
If a prosthesis is planned for the patient, a graded scale X-ray image is helpful in determining the position and size of the implant.
Pre- and postoperative data were collected for the present study. Clinical data parameters related to DRUJ function were collected, including range of motion (ROM) in pronation and supination using a wrist goniometer, grip strength (Jamar II, Jamar Dynamometer), lifting capacity using 2.3-, 4.5-, 6.8-, and 9.1-kg weights (5, 10, 15, and 20 lbs) (elbow starting in extension and lifting weights, moving elbow into horizontal axis in neutral, pronated, and supinated positions). Hand surgeons, hand therapists, or hand surgery nurses obtained clinical measurements. Patients completed Disabilities of the Arm, Shoulder and Hand (DASH), Patient Rated Wrist Evaluation (PRWE), and Patient Satisfaction and Pain questionnaires preoperatively and postoperatively. Preoperative data were correlated with 5-year postoperative data. ROM, grip strength, and pain outcomes were compared with preoperative values, and load-bearing capacity of the prosthesis arm was compared with the contralateral arm. Comparisons were analyzed statistically using independent, one-tailed t test with unequal variance with a 95% confidence interval. Statistical significance was considered a P-value < 0.05.
Preoperative and the most recent available postoperative X-ray images (3 years or more postoperative, n = 24 prostheses, 23 patients) were reviewed and compared for signs of loosening and bone changes. Intraoperative complications and postoperative adverse events were also documented. Follow-up was at 2 weeks, 4 weeks, 2 months, 6 months, and yearly postoperatively.
Surgical Technique
The procedure is generally accomplished under axillary block. An iodine plastic wrap is used to avoid contact between the implant and the skin. A tourniquet is always applied for visualization. An 8-cm longitudinal incision in the shape of a hockey stick is made along the ulnar border of the distal forearm, in the interval between the fifth and sixth dorsal compartments. Care is taken to avoid damage to the sensory branch of the ulnar nerve. The skin and subcutaneous flap are elevated up to the radial wrist extensors. A rectangular, ulnar-based fascia flap is created with enough width to cover the head of the implant; it may include the most proximal part of the extensor retinaculum. This flap will be used later to create a buffering barrier between the prosthesis and the extensor carpi ulnaris (ECU) (Fig. 4). The dissection is continued between the extensor digiti minimi (EDM) and the ECU until the ulna is encountered, and the EDM is elevated from the ulna and the interosseous membrane for at least 8 cm. The sensory branch of the posterior interosseous nerve is divided to avoid avulsion of the nerve from the thumb extensors when placing an elevator between the extensor mass and the radius. The sheath of the ECU tendon is opened completely up to its insertion at the base of the fifth metacarpal to avoid pressure against the distal end of the implant. The remaining head of the ulna, if present, is then excised at a level just proximal to the cartilage or where the DRUJ would have been (Fig. 5).
Fig. 4.
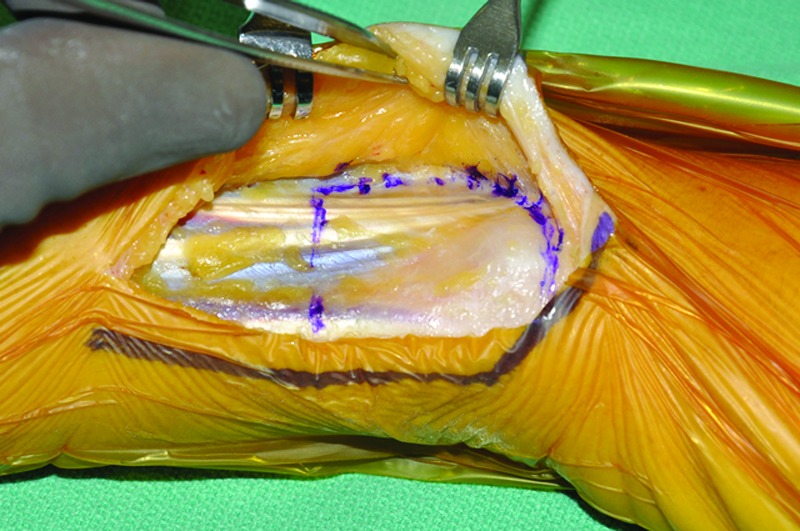
The ulnarly based fascioretinacular flap is raised as a first step in the procedure to create a buffer between the implant and the ECU.
Fig. 5.
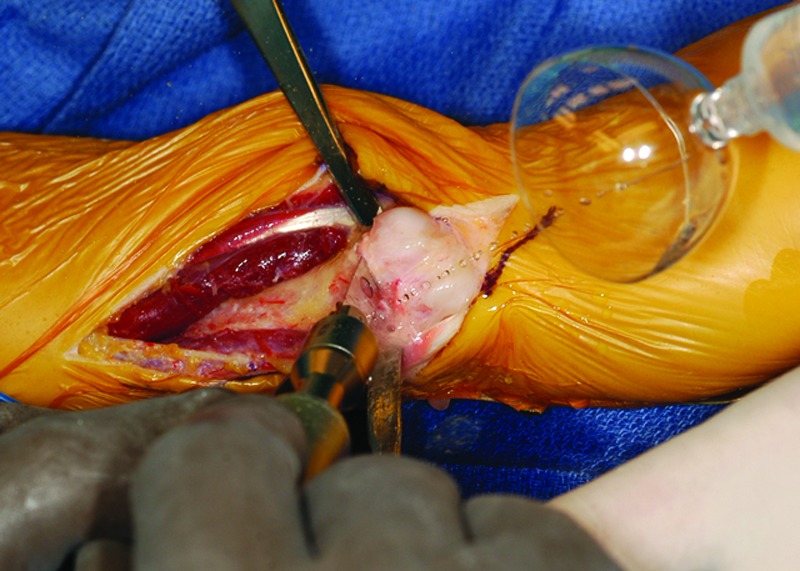
The ulnar head is excised proximal to the neck in order to depress the ulnar shaft volarly, expose the ulnar side of the radius, and create space for the trial plate.
At this stage, the radial attachment of the triangular fibrocartilage, if found intact, is left undisturbed. If left in situ, this structure can provide a barrier between the prosthesis and the carpal bones. The ulnar shaft is then retracted in a volar direction, thus ensuring access to the radius. The interosseous membrane is elevated from the radius along the distal 8 cm of the interosseous crest. The radial trial plate is then placed over the interosseous crest of the radius, and its volar border is aligned with the volar surface of the radius. Care is taken to ensure that at least 3 mm of the sigmoid notch lies distal to the end of the plate. Depending on the anatomy encountered, the distal radius may require contouring, including removal of the volar lip of the sigmoid notch with a saw blade or a medium-size burr ball. After the position of the trial plate has been deemed appropriate—meaning parallel to the volar shaft of the radius and at least 3 mm proximal to the end of the radius—a 1.4-mm (0.054-in.) Kirschner wire (K-wire) is inserted in one of the holes at the distal end of the trial plate as well as the most proximal hole.
An image intensifier is used to check the position of the trial plate in both AP and lateral views. If no adjustment is needed, a 2.5-mm drill bit is used with the provided guide to drill the screw hole at the oval opening, the proper screw length is gauged, the hole is tapped, and the appropriate length 3.5-mm screw is placed. The image intensifier is used again to confirm plate positioning and proper screw length. With confirmation of the length of the screw and good plate contact with the bone, the distal K-wire is removed, and the hole for the radial peg is drilled with the appropriate drill bit. When the surgeon is satisfied, the trial component is removed and replaced with the prosthesis radial component. If necessary, a soft mallet is used to achieve good contact between the radial plate and the ulnar border of the radius. After the last screw is placed in position, a final check of the radial plate to confirm screw length and position is performed with the image intensifier (Fig. 6).
Fig. 6.

Once the radial plate is completely secured, the image intensifier is used to assess the position and length of the screws. Screws that are too long can irritate the superficial radial nerve.
Attention is now turned to the ulna. With the forearm fully pronated, a measuring device with an appropriately colored ball (blue for a large implant and black for a small implant) fitting into the hemi-socket of the radial component is seated, and the ulna is juxtaposed against its shaft. This enables the surgeon to assess the exact amount of ulna to be resected (Fig. 7).
Fig. 7.

The reference guide is use to determine the final cut of the ulna. In general, if the patient has had no previous ulnar head excision, the chosen line is 1 centimeter for an extended stem. If the patient has had ulna resection, the cut is made to match an exact length of 1, 2, or 3 cm to have a perfect match between the radial plate and the ulna stem.
After final resection of the distal ulna, a 1.6-mm (0.062-inch) guide wire is inserted into the ulnar medullary canal to act as a centralizer for a cannulated drill bit. The cannulated drill bit is introduced for a length of 11 cm. Next, a medullary broach of appropriate size is inserted into the canal to bevel the distal ulna and plane its distal end.
The medullary canal is now thoroughly irrigated, and the stem of the ulnar component is introduced. The ultrahigh-molecular-weight (UHMW) polyethylene ball is placed over the distal peg or pivot, and the ulnar component is positioned within the hemi-socket of the radial component. Finally, the other half of the radial socket or cover is positioned and secured with two small screws. The image intensifier is once again used to confirm adequacy of the overall position (Fig. 8). Full ROM is confirmed. The fascioretinacular flap is placed between the prosthesis and the ECU tendon and sutured to the radius (Fig. 9). This prevents tenosynovitis of the ECU and provides a cushion over the implant, especially for a patient with little subcutaneous adipose tissue.
Fig. 8.

The final check with the image intensifier demonstrates the proper position and the range of motion after the implant is completely assembled.
Fig. 9.
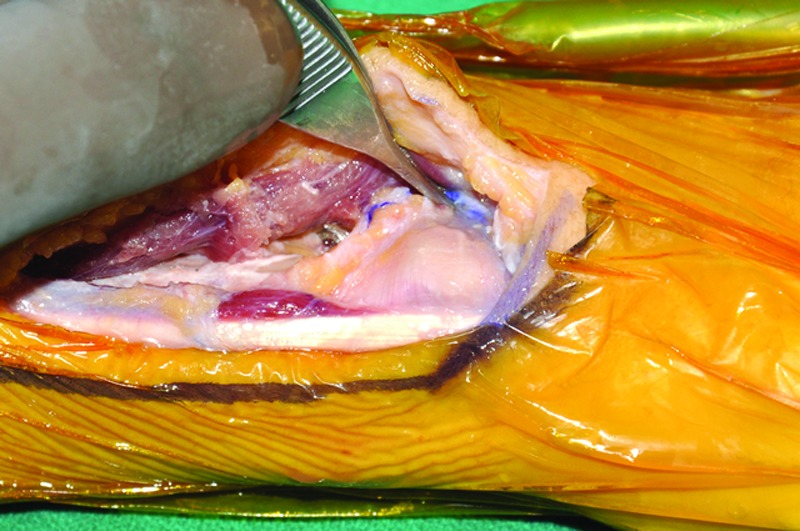
Placing the fascioretinacular flap between the implant and the ECU prevents tendinitis in cases with full range of wrist motion and adds cushion on top of the implant.
The tourniquet is released, and complete hemostasis is secured. The skin is then closed with interrupted sutures and a bulky soft dressing is applied. The soft bulky dressing is left in place to support the wound for 2 weeks and the patient is allowed to have full ROM. Gradual weight bearing is allowed immediately after surgery. Maximum weight bearing should be 10 kg.
Results
Osteoarthritis was the primary cause of dysfunctional DRUJs in our patients, occurring in 30 of 36 joints. Trauma causing DRUJ dysfunction and initiating osteoarthritis, with fractures to the radius or ulna, occurred in 16 DRUJs, and damage to the TFCC occurred in 6 DRUJs. Radioulnar impingement occurred in 8 forearms following Darrach, Bowers, or Sauvé-Kapandji procedures. Additional conditions such as Madelung deformity, Kienböck disease, Ehlers-Danlos syndrome, and gouty and rheumatoid arthritis contributed to DRUJ damage. Of the joints studied, 92% received the prosthesis as a salvage following previous DRUJ surgery. Prior to implantation of the index prosthesis, 32 patients (33 forearms) underwent 56 surgical procedures to damaged DRUJs. The most common previous procedures included 14 fixations of fractured distal radius and ulna, 8 ulnar shortenings, 1 radial shortening, and 8 ulnar head resections via the Darrach procedure. Patients also underwent the Sauvé-Kapandji and Bowers procedures, ligament reconstruction with tendon graft, tendon repair due to Vaughan-Jackson syndrome, cartilage realignment, radial and ulnar realignment osteotomy, and previous prostheses or an ulnar rod (Table 1). Twenty-seven of the 35 patients receiving DRUJ prostheses underwent follow-up at a mean 5 years postoperatively (range, 4.4 years– 6.2 years). Twenty-two patients returned to the clinic for follow-up, and five completed telephone questionnaires about activity level, pain, and satisfaction after surgery. The remaining eight patients did not undergo follow-up because the clinic was unable to contact them.
Table 1. Surgeries to DRUJ prior to DRUJ prosthesis.
| Fixation of distal radius/ulna | 15 |
| Ulna/radius shortening | 9 |
| Darrach procedure | 8 |
| Ligament reconstruction | 6 |
| TFCC repair | 5 |
| Radius/ulna osteotomy and realignment | 4 |
| Tendon repair | 3 |
| Previous prostheses | 2 |
| Sauvé-Kapandji procedure | 2 |
| Bowers procedure | 2 |
| Ulnar rod | 1 |
Comparison of pre- and postoperative data for patients who underwent long-term clinical follow-up showed significant improvements in all categories (Table 2). Mean ROM increased to American Medical Association normative ranges (forearm pronation ≥ 80° and supination ≥ 70° = 0% impairment) upon 5-year follow-up. Grip strength nearly doubled, increasing from 48% to 90% of the contralateral side. Pain at rest and upon activity both decreased significantly.
Table 2. Comparison of clinical measurements preoperatively and 5 years postoperatively in DRUJ implants.
| Pronation | Supination | Grip strength (% of contralateral side) |
Pain at rest (out of 10) |
Pain with activity (out of 10) |
|
|---|---|---|---|---|---|
| Preoperative | 66° (SD 30.6, n = 15) |
52° (SD 29.1, n = 16) |
48% (SD 29.5, n = 13) |
5.11 (SD 3.3, n = 9) |
8.25 (SD 1.2, n = 8) |
| Postoperative | 81° (SD 11.2, n = 20) |
75° (SD 17.9, n = 20) |
90% (SD 57.1, n = 22) |
1.02 (SD 1.5, n = 27) |
2.71 (SD 2.7, n = 24) |
| P-value | .039 | .007 | .004 | .002 | .000 |
Upon 5-year follow-up, single-arm load bearing in neutral position was an average 7.5 kg (16.4 pounds) in the DRUJ prosthesis arm versus 7.7 kg (16.9 pounds) in the contralateral arm (Table 3). There was no significant difference between the lifting capacities of the prosthesis arm and those of the other arm in either the neutral, pronated, or supinated lifting positions.
Table 3. Comparison of prosthesis arm versus contralateral arm: single-arm load-bearing capacities (maximum tested weight lifting 20 lbs [9 kg]).
| Neutral lifting position (lbs) [kg] | Pronated lifting position (lbs) [kg] | Supinated lifting position (lbs) [kg] | |
|---|---|---|---|
| Prosthesis arm | 16.4 (SD 5.5, n = 21) [7.5 kg (SD 2.5, n = 21)] |
15.5 (SD 6.2, n = 19) [7.1 kg (SD 1.3, n = 19)] |
15.8 (SD 5.6, n = 19) [7.2 kg (SD 2.6, n = 19)] |
| Other arm | 16.9 (SD 4.9, n = 18) [7.7 kg (SD 2.2, n = 18)] |
16.7 (SD 5.4, n = 18) [7.6 kg (SD 2.5, n = 18)] |
16.7 (SD 5.4, n = 18) 7.6 kg (SD 2.5, n = 18)] |
| P-value | .379 | .278 | .316 |
Patients expressed an average satisfaction of 9.8 out of 10 (10 = completely satisfied) with their prostheses (n = 26, SD = 0.49). Five-year postoperative mean DASH score was 16 out of 100 (n = 20), and mean PRWE score was 24 out of 100 (n = 19), indicating that patients had minimal pain and difficulty with activities of daily living 5 years postoperatively. Preoperative DASH and PRWE scores were not available for comparison.
Among the 27 patients who underwent 5-year follow-up, the prosthesis had a 100% 5-year survival rate. Two minor soft tissue infections occurred in immediate postoperative course and were resolved with antibiotics; no prostheses were infected; both of these patients had had multiple previous operations are the same site. Of the 36 prostheses implanted, 69% (25) were complication-free, while 31% (11) of the prostheses had 12 symptomatic complications: six cases of ECU tendinitis, five cases of ectopic bone formation, and one screw/cap loosening. All complications were resolved surgically with good clinical course and patient satisfaction. One patient suffered from ECU hypersensitivity 4 years postimplantation, which was attributed to failed tendon repairs prior to prosthesis implantation. Her issue was resolved with injections. One ulnar stem replacement was performed 4 years postoperatively when a larger ulnar stem became available; upon the patient's request, his original stem was implanted in 2005 although it was too small for his medullary cavity.
Long-term follow-up radiographs of 24 DRUJ prostheses were available for review (mean 4.8 years postoperative). Radiographs were compared with images obtained in 2005 following implantation. Bone regrowth in former screw holes and/or around screws was observed in 20 prostheses. Bone growth was observed on the proximal edge of the radial plate in 19 cases. Twenty-one prostheses showed no signs of loosening. Two prostheses showed slight evidence of stem loosening. One of these prostheses also had asymptomatic loosening of a screw on the prosthesis cap, as well as ectopic bone growth over about one-third of the proximal part of the radial plate. One patient had ectopic bone growth at the top of the ulnar stem, and the patient who underwent stem replacement at 4 years postoperatively showed signs of shock around the screws and radial peg, attributed to his formerly malpositioned ulnar stem. All patients showing radiographic evidence of loosening or bone growth were asymptomatic and had minimal pain and utmost satisfaction with their prostheses.
Discussion
Procedures that excise or replace only a portion of the DRUJ do not take into account all the required functions of the joint and can potentially cause an active patient to require additional procedures. Patients without an ulnar head have impingement of the radius on the ulna in neutral position while the radius rides on top of the ulna and gravity pulls it down.8 In full pronation and full supination, the ulnar stump moves up as it is fixed and the radius falls, producing in some cases ulnar neuritis as the ulna pushes against the ulnar nerve.
The Aptis DRUJ prosthesis is indicated for patients with mature skeletons who have rheumatoid, degenerative, or posttraumatic arthritis of the DRUJ and who may or may not have already had surgical treatment.10,11,12,13 It is especially useful for a failed and painful Darrach, Sauvé-Kapandji, match resection, or similar types of bone excision or for failed and unstable unipolar ulna head replacement. The prosthesis has proven of great use for individuals who need distal ulna resection for tumors and for patients with congenital abnormalities such as Madelung deformity and Ehlers-Danlos syndrome.
The device can be used in patients with at least 14 cm of proximal ulna remaining, allowing the stem to be implanted properly. Elongated ulnar stems can be used in those individuals who have lost large segments of the ulna. In general, patients with more ulna available and those in whom the DRUJ replacement is the initial DRUJ procedure have better function. Patients with excessive ulna excision (> 4 cm) will require a customized, lengthened stem. For patients with Essex Lopresti injury and subsequent DRUJ instability, the DRUJ implant is a good salvage procedure for their wrist pain (Fig. 10a,b). Also, patients with single-bone forearm after multiple surgeries had favorable outcome after DRUJ implant (Fig. 11a,b). The use of the implant is contraindicated when bone, musculature, tendons, or adjacent soft tissue is compromised by systemic disease or recent infection. The implant should not be used in patients who have not reached skeletal maturity.
Fig. 10 .

(a) Ulnar plus as a result of radial head excision in an Essex-Lopresti fracture. (b) The total DRUJ implant has stabilized the joint, allowing the axial load to pass through the ulna without pain.
Fig. 11 .

(a) Patient complaining of severe right shoulder pain due to overuse as a result of radiocarpal and radioulnar fusion. (b) Pain in the shoulder subsided immediately after the pronation and supination of the patient's right forearm were reestablished.
Some complications that we had during the first procedures were ECU tendinitis, ectopic bone formation, and difficulty with the radial plate alignment. Our experience shows that these can be overcomed with careful surgical maneuvers.
To avoid ECU tendinitis, a rectangular ulnar based fascia flap is created with enough width to cover the head of the implant; it may include the most proximal part of the extensor retinaculum. This flap will be used later to create a buffering barrier between the prosthesis and the ECU.
All the patients with ectopic bone formation around the distal ulna were treated successfully with surgical excision. This ectopic calcification was caused by the periosteum not being resected as the head of the ulna was excised in a subperiosteal manner. This can be avoided by careful resection of the entire ulnar head primarily.
For correct radial plate alignment, we had to perform removal of the volar lip of the sigmoid notch with a saw blade or a medium-size burr ball. We perform this maneuver more often now when we have some difficulty placing the radial plate to the best-fitting position.
Our study has some limitations. The lack of preoperative DASH and PRWE scores that were not available for comparison in this group of patients was corrected in the following cases. Hopefully we will be able to present the long-term follow-up results of a larger series in the future.
If all else fails, rather than a partial replacement (meaning replacement of the ulnar head), a total distal radioulnar joint replacement such as presented here is necessary—one that will reproduce the function of the sigmoid notch, the ulnar head, and the TFCC.12,14 The majority of the patients we treated have had between 2 and 14 procedures on the distal radioulnar joint, from partial excision of the distal radioulnar joint to wide excision of the ulna, passing through all the techniques of soft tissue stabilization available. Once the total replacement has taken place, the patient has been able to get off pain medications and return to a productive life.
Disclaimer
The second author was a paid researcher for Aptis Medical Inc. The fifth author is part owner of Aptis Medical Inc.
References
- 1.Darrach W. Partial excision of lower shaft of ulna for deformity following Colles's fracture. Ann Surg. 1913;57:764–765. [PubMed] [Google Scholar]
- 2.Sauvé L, Kapandji M. Nouvelle technique de traitement chirurgical des luxations récidivantes isolées de l'extrémité inférieure du cubitus. J Chir (Paris) 1936;47:589–594. [Google Scholar]
- 3.Watson H K, Ryu J Y, Burgess R C. Matched distal ulnar resection. J Hand Surg Am. 1986;11(6):812–817. doi: 10.1016/s0363-5023(86)80228-3. [DOI] [PubMed] [Google Scholar]
- 4.Markolf K L, Lamey D, Yang S, Meals R, Hotchkiss R. Radioulnar load-sharing in the forearm. A study in cadavera. J Bone Joint Surg Am. 1998;80(6):879–888. doi: 10.2106/00004623-199806000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Shaaban H, Giakas G, Bolton M, Williams R, Scheker L R, Lees V C. The distal radioulnar joint as a load-bearing mechanism—a biomechanical study. J Hand Surg Am. 2004;29(1):85–95. doi: 10.1016/j.jhsa.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 6.Shaaban H, Giakas G, Bolton M. et al. The load-bearing characteristics of the forearm: pattern of axial and bending force transmitted through ulna and radius. J Hand Surg [Br] 2006;31(3):274–279. doi: 10.1016/j.jhsb.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 7.Bowers W H. Distal radioulnar joint arthroplasty: the hemiresection-interposition technique. J Hand Surg Am. 1985;10(2):169–178. doi: 10.1016/s0363-5023(85)80100-3. [DOI] [PubMed] [Google Scholar]
- 8.Bell M J, Hill R J, McMurtry R Y. Ulnar impingement syndrome. J Bone Joint Surg Br. 1985;67(1):126–129. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 9.Lees V C, Scheker L R. The radiological demonstration of dynamic ulnar impingement. J Hand Surg [Br] 1997;22B:448–450. [Google Scholar]
- 10.Swanson A B. Implant arthroplasty for disabilities of the distal radioulnar joint. Use of a silicone rubber capping implant following resection of the ulnar head. Orthop Clin North Am. 1973;4(2):373–382. [PubMed] [Google Scholar]
- 11.Herbert T J, van Schoonhoven J. London, England: Martin Dunitz; 2000. Ulnar head prostheses: a new solution for problems at the distal radioulnar joint; pp. 145–149. [Google Scholar]
- 12.Scheker L R, Babb B A, Killion P E. Distal ulnar prosthetic replacement. Orthop Clin North Am. 2001;32(2):365–376. doi: 10.1016/s0030-5898(05)70256-x. [DOI] [PubMed] [Google Scholar]
- 13.Willis A A, Berger R A, Cooney W P III. Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. J Hand Surg Am. 2007;32(2):177–189. doi: 10.1016/j.jhsa.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Scheker L R. Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(9):1639–1644. doi: 10.1016/j.jhsa.2008.08.014. [DOI] [PubMed] [Google Scholar]