Abstract
The major complications of distal ulna resection, the Darrach procedure, are radioulnar impingement and instability. High failure rates have been reported despite published modifications of the Darrach procedure. Several surgical techniques have been developed to treat this difficult problem and to mitigate the symptoms associated with painful convergence and impingement. No technique has demonstrated clinical superiority. Recently, implant arthroplasty of the distal ulna has been endorsed as an option for the management of the symptomatic patient with a failed distal ulna resection. However, there are concerns for implant longevity, especially in young, active adults. Resection interposition arthroplasty relies on interposition of an Achilles tendon allograft between the distal radius and the resected distal ulna. Although this technique does not restore normal mechanics of the distal radioulnar joint, it can prevent painful convergence of the radius on the ulna. Achilles allograft interposition arthroplasty is a safe and highly effective alternative for failed distal ulna resections, especially for young, active patients, in whom an implant or alternative procedure may not be appropriate.
Keywords: Achilles allograft, distal ulna, failed Darrach, radioulnar impingement
Distal ulna resection operations, such as the Darrach procedure and its modifications, have many known complications, including loss of ulnar support of the carpus and radioulnar convergence.1,2,3,4 Radioulnar convergence produces painful impingement of the ulnar stump against the radius, usually accompanied by instability.5,6,7,8,9,10 Distal radioulnar instability may manifest with crepitus, pain with forearm rotation, and grip weakness. Persistent painful instability of the distal ulna is a difficult clinical dilemma.
To overcome painful impingement and instability secondary to failed distal ulna resection, many surgical procedures have been described with varying success. The reported techniques include stabilizing soft tissue procedures, further shortening of the ulna, wide resection of the ulna, lengthening of the ulna, and other more complex procedures.11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27
Several soft tissue procedures using part of the flexor and/or extensor carpi ulnaris tendons to stabilize the ulnar stump have been described.11,12,13,14,15,16,17 These procedures are technically demanding, and their results are not reproducible. Furthermore, none of these procedures was found to reliably restore stability and painless forearm rotation. Wide resection of the ulna, as well as lengthening of the excessively shortened ulna, has been described, but it has not reliably resolved symptoms.18,19,20 Recently, distal ulna replacement has become a popular option.21,22,23,24,25,26,27,28 However, there are concerns for implant longevity, especially in young active adults.
In an effort to mitigate the symptoms associated with painful convergence and impingement and to avoid the complications of ulnar head replacement, particularly in young patients, the senior author (D. G. S.) developed an interposition technique using Achilles tendon allograft between the distal radius and the resected distal ulna.29,30
Etiology
Despite modifications to the Darrach procedure, the published failure rates have been high (7–40%).2,4,7,8,31,32,33,34 Possible causes of failure include excessive bony resection, inadequate bony resection, insufficient soft tissue stabilization of the ulna, ulnar impingment and instability, and ulnar translocation of the carpus.3,7,10,34
Stability of the distal radioulnar joint (DRUJ) depends on bony and ligamentous structures, including the intrinsic stabilizers of the triangular fibrocartilage complex (TFCC) and the extrinsic stabilizers of the distal forearm.9,10
Following distal ulna resection, all of the mechanical restraints preventing radioulnar impingement have been eliminated. Loss of linkage between the radius and the ulna results in radioulnar convergence, producing impingement of the ulnar stump against the radius, and is usually accompanied clinically by instability of the distal ulna.3,4,5,6,7 Loss of stability of the TFCC and the associated ulnocarpal soft tissue stabilizers of the triangular fibrocartilage allows accentuated translation of the distal ulna with forearm rotation.7,17
Diagnosis
The diagnosis of symptoms as secondary to a failed distal ulna resection and subsequent radio-ulnar impingement/ instability is clinical. History and physical exam findings are usually diagnostic and are supported by plain radiographs. It must be emphasized that while radioulnar convergence is common following excision of the distal ulna, not all patients are symptomatic.6,7
Typically, a symptomatic failed distal ulna resection will present with incapacitating pain over the distal stump of the ulna, aggravated by forearm rotation and grip; sensation of instability; and complaints of grip weakness. Painful grinding and mechanical limitations to forearm rotation lead to painful disuse of the upper extremity.
Examination
Physical examination may reveal pain with ballottement of the distal ulna in a dorsal-palmar direction, or with direct compression of the ulna into the radius. Crepitus and palpable “clicking” or “popping” over the ulnar stump and the distal radius during forearm rotation may be noted. Physical examination also reveals reduced grip strength in comparison with the contralateral side. Assessment for coexisting pathology of the proximal radioulnar joint and interosseous membrane is necessary, and other sources of wrist pain and dysfunction must be ruled out.
Relevant Imaging
Standard posteroanterior (PA) radiographs of the wrist in neutral forearm rotation often show the residual ulna converging toward or abutting against the distal radius (Fig. 1). Erosion of the medial cortex of the distal radius may be present, implying dynamic impingement between the ulnar stump and the radius, which may otherwise not be apparent on static images. Such radiographic findings of impingement, however, can be present in asymptomatic patients.
Fig. 1.

PA view depicting impingement between the ulnar stump and the distal radius after failed Darrach procedure.
A gripping “weight-bearing” PA view of the wrist will accentuate radioulnar convergence. This is a technique in which the patient holds a weight with the forearm in neutral rotation while the radiograph is taken in a “cross-table” direction (Fig. 2). Advanced imaging is seldom indicated.
Fig. 2.

Gripping “weight-bearing,” PA view, showing contact between distal radius and ulnar stump.
Nonsurgical Treatment
A variety of conservative measures have been suggested to eliminate the symptoms associated with failed distal ulna resection, of which none are uniformly successful. Patients with mild symptoms and minimal functional impairment can be managed with oral anti-inflammatory medications, activity modification, and adjuvant physiotherapy. Patients with low functional demands can be managed with a forearm brace carefully molded along the interosseous membrane to separate the radius and ulna. However, conservative measures seldom produce a complete and lasting resolution of symptoms.
Surgical Treatment and Technique
The Achilles tendon allograft interposition procedure for failed distal ulna resection can be performed under general or regional anesthesia with tourniquet control. The patient is positioned supine with the affected extremity on a hand-table extension. If possible, the previous surgical incisions are incorporated into the approach. A dorsal approach through the fifth dorsal compartment is made, providing access to the resected distal ulna and to the medial cortex of the radius. Care is taken to preserve the dorsal cutaneous branch of the ulnar nerve. Subperiosteal exposure of the distal ulna is performed ∼4–6 cm proximal to the distal stump. Frequently, the resected ulna develops reactive bone, which may impinge on the distal radius or cause mechanical limitations to motion. The prominent bone is removed, and a smooth surface of the ulnar stump is created. Then the medial cortex of the radius is exposed by retraction of the ulna volarly. Three or four mini, unicortical suture anchors (micro FT, Arthrex) are placed into the medial cortex of the radius, proximal to the ulnar notch at site of the impingement. It is necessary to create an anchor footprint 2–3 cm in length for later fixation of the allograft to the medial radius. This ensures that a large allograft buffer can be created between the two bones. Similarly, three or four drill holes are next made in a medial-to-lateral direction in the distal ulna along 2–3 cm length of bone, and sutures are passed through each of the holes (Fig. 3).
Fig. 3.
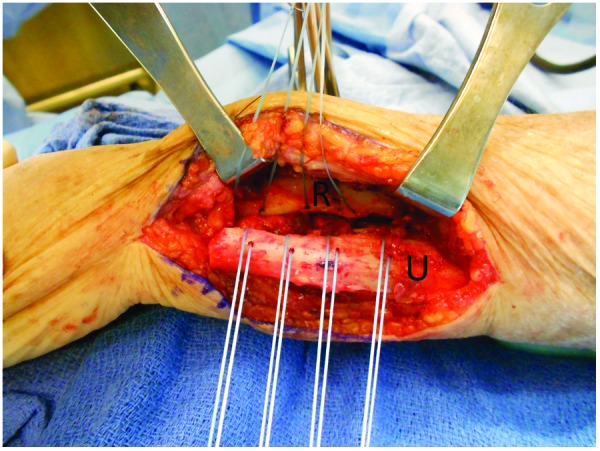
Intraoperative view. Suture anchors are placed into the medial cortex of the distal radius. Drill holes are made in the distal ulna, and sutures are passed through each of the holes. A large buffer is created between the distal ulna and the radius. R, radius; U, ulna.
An Achilles tendon allograft is prepared for implantation by removing the calcaneal remnant. The allograft is then rolled onto itself, creating a large interpositional “pillow” that will act as a soft tissue buffer between the radius and ulna (Fig. 4). The allograft is then sutured between the radius and ulna using the previous placed anchors and drill holes (Fig. 5). The size of the allograft pillow is determined by pronating and supinating the forearm with pressure applied to the ulnar aspect of the ulna. Generally, the entire soft tissue allograft is utilized. If crepitus is noted, the allograft size is increased until no further crepitus occurs with passive ulnar displacement of the ulna toward the radius or with forearm rotation. With final allograft placement, there should be padding between the radius and the ulna enough to prevent any palpable crepitus during forearm rotation under compression and to ensure that a smooth arc of motion occurs without impingement. No other tissues are used to stabilize the ulnar stump. Standard capsular and soft tissue closures are completed over the allograft, followed by routine retinaculum and skin closure.
Fig. 4.

The calcaneal remnant has been removed and the allograft is rolled onto itself, creating a large interposition “pillow.”
Fig. 5.
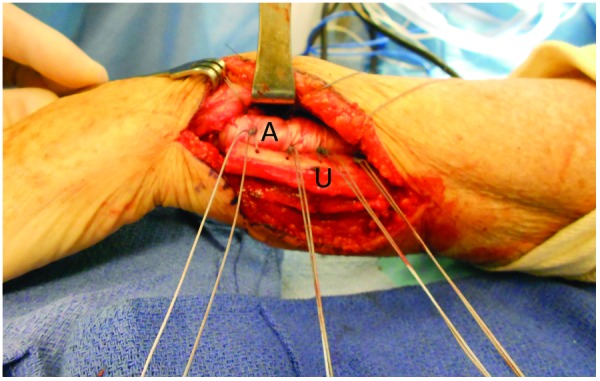
Intraoperative view. The allograft is placed and is sutured between the distal radius and ulnar stump using the placed anchors and drill holes. A, allograft; U, ulna.
Postoperative Rehabilitation
The wrist is placed in neutral rotation and flexion in a well-padded long arm splint. At the initial postoperative follow-up, usually in 10 days, the long arm splint is converted to a long arm cast. The cast is removed after 6 weeks, and a removable long arm splint is prescribed. At this time, the patient begins a rehabilitation program, initially consisting of active and active-assisted range of motion exercises with appropriate progression to strengthening exercises. Protected range of motion and interval splinting are continued until 12 weeks postoperatively.
Clinical Results
The combined clinical series includes 27 patients with failed distal ulna resection with a mean age of 44 years (range 37–68 years). The interposition arthroplasty with Achilles tendon allograft was performed at a mean time of 14 months after the Darrach procedure. Many patients had numerous procedures antecedent to the interposition arthroplasty.
At a mean follow-up of 72 months (range, 12–174 months), good (17/27 patients) to excellent (9/27 patients) results were demonstrated with marked alleviation of pain and improvement in forearm rotation. Grip strength improved an average of 72%, and the total arc of forearm rotation improved an average of 69 degrees. Pain persisted in 1 patient (worker's compensation), whose result was graded as a failure and attributed to insufficient graft bulk. No graft-related complications were encountered.
Postoperative radiographic evaluation at final follow-up demonstrated maintenance of a wide space between the distal ulna and radius (Fig. 6). Radiographic evaluation revealed asymptomatic ulnar scalloping in 2 patients at 2 and 3 years postoperatively.
Fig. 6.

Two-years postoperative PA view demonstrates maintenance of a wide space between the distal ulna and radius. Note no impingement between the two forearm bones.
Radial shaft fracture is a potential complication that may be avoided with the use of micro suture anchors for graft fixation.
Literature Review
Distal ulna resections, even when carefully executed, have a substantial incidence of persistent pain and radioulnar dysfunction. To mitigate the symptoms associated with painful convergence and impingement, a variety of alternative procedures, including stabilizing soft tissue techniques, wide resection, and lengthening of the distal ulna, have been developed. Varying degrees of success have been reported, and no technique has demonstrated clinical superiority.11,12,13,14,15,16,17,18,19,20
Implant replacement of the distal ulna is an effective treatment for the symptomatic patient after Darrach distal ulna resection. Reports by many investigators are encouraging.21,22,23,24,25,26,27,28,35,36 Nevertheless, there are concerns for implant longevity, especially in young active adults. Implant-associated complications, such as loosening, infection, bone resorption, dislocation, and implant instability, are concerns for this patient population. In a recent study, authors reported favorable long-term results of an ulnar head prosthesis following ulnar head resection.28 However, more studies with long-term results will be necessary to determine true clinical outcomes and the frequency of implant-associated complications.
The Achilles tendon allograft interposition arthroplasty is a straightforward technique that does not compromise existing tendons or muscles and allows custom tailoring of the graft's bulk and position. The size of the allograft must be given great attention. When insufficient allograft bulk is used, the radioulnar space may not be maintained. The allograft should prevent the ulnar stump from contacting the radius during pronation and supination under compression. Disadvantages of all allografts include cost, availability, and immunologic reaction. Nonetheless, they are currently widely used in orthopedic surgery. So far, there have been no reports of unfavorable immune reactions or infections with this technique.
The clinical outcomes herein showed that Achilles tendon allograft interposition arthroplasty is highly effective for the treatment of painful convergence and impingement after distal ulna resection. Although this technique does not restore normal biomechanics of the DRUJ, it can prevent impingement, crepitus, and painful convergence of the ulna on the radius. Interposition arthroplasty with the Achilles tendon allograft is an attractive alternative, especially for high-demand patients, in which an implant or alternative procedure may not be appropriate.
Footnotes
Conflict of Interest None
References
- 1.Darrach W. Anterior dislocation at the head of the ulna. Ann Surg. 1912;56:802–803. [Google Scholar]
- 2.Field J, Majkowski R J, Leslie I J. Poor results of Darrach's procedure after wrist injuries. J Bone Joint Surg Br. 1993;75(1):53–57. doi: 10.1302/0301-620X.75B1.8421034. [DOI] [PubMed] [Google Scholar]
- 3.McKee M D, Richards R R. Dynamic radio-ulnar convergence after the Darrach procedure. J Bone Joint Surg Br. 1996;78(3):413–418. [PubMed] [Google Scholar]
- 4.Sauerbier M, Berger R A, Fujita M, Hahn M E. Radioulnar convergence after distal ulnar resection: mechanical performance of two commonly used soft tissue stabilizing procedures. Acta Orthop Scand. 2003;74(4):420–428. doi: 10.1080/00016470310017721. [DOI] [PubMed] [Google Scholar]
- 5.Kleinman W B, Graham T J. New York, NY: McGraw-Hill; 1996. Distal ulnar injury and dysfunction; pp. 667–709. [Google Scholar]
- 6.Bell M J, Hill R J, McMurtry R Y. Ulnar impingement syndrome. J Bone Joint Surg Br. 1985;67(1):126–129. doi: 10.1302/0301-620X.67B1.3968131. [DOI] [PubMed] [Google Scholar]
- 7.Bieber E J, Linscheid R L, Dobyns J H, Beckenbaugh R D. Failed distal ulna resections. J Hand Surg Am. 1988;13(2):193–200. doi: 10.1016/s0363-5023(88)80047-9. [DOI] [PubMed] [Google Scholar]
- 8.Noble J, Arafa M. Stabilisation of distal ulna after excessive Darrach's procedure. Hand. 1983;15(1):70–72. doi: 10.1016/s0072-968x(83)80038-2. [DOI] [PubMed] [Google Scholar]
- 9.Greenberg J A. Reconstruction of the distal ulna: instability, impaction, impingement, and arthrosis. J Hand Surg Am. 2009;34(2):351–356. doi: 10.1016/j.jhsa.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Elias M. Failed ulnar head resection: prevention and treatment. J Hand Surg [Br] 2002;27(5):470–480. doi: 10.1054/jhsb.2002.0815. [DOI] [PubMed] [Google Scholar]
- 11.Jupiter J B. Tendon stabilization of the distal ulna. J Hand Surg Am. 2008;33(7):1196–1200. doi: 10.1016/j.jhsa.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Sotereanos D G, Leit M E. A modified Darrach procedure for treatment of the painful distal radioulnar joint. Clin Orthop Relat Res. 1996;325(325):140–147. doi: 10.1097/00003086-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Syed A A, Lam W L, Agarwal M, Boome R. Stabilization of the ulna stump after Darrach's procedure at the wrist. Int Orthop. 2003;27(4):235–239. doi: 10.1007/s00264-003-0462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chu P J, Lee H M, Hung S T, Shih J T. Stabilization of the proximal ulnar stump after the Darrach or Sauvé-Kapandji procedure by using the extensor carpi ulnaris tendon. Hand (NY) 2008;3(4):346–351. doi: 10.1007/s11552-008-9113-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minami A, Iwasaki N, Ishikawa J, Suenaga N, Kato H. Stabilization of the proximal ulnar stump in the Sauvé-Kapandji procedure by using the extensor carpi ulnaris tendon: long-term follow-up studies. J Hand Surg Am. 2006;31(3):440–444. doi: 10.1016/j.jhsa.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Johnson R K. Stabilization of the distal ulna by transfer of the pronator quadratus origin. Clin Orthop Relat Res. 1992;275(275):130–132. [PubMed] [Google Scholar]
- 17.Kleinman W B, Greenberg J A. Salvage of the failed Darrach procedure. J Hand Surg Am. 1995;20(6):951–958. doi: 10.1016/S0363-5023(05)80142-X. [DOI] [PubMed] [Google Scholar]
- 18.Wolfe S W, Mih A D, Hotchkiss R N, Culp R W, Keifhaber T R, Nagle D J. Wide excision of the distal ulna: a multicenter case study. J Hand Surg Am. 1998;23(2):222–228. doi: 10.1016/s0363-5023(98)80117-2. [DOI] [PubMed] [Google Scholar]
- 19.Greenberg J A, Yanagida H, Werner F W, Short W H. Wide excision of the distal ulna: biomechanical testing of a salvage procedure. J Hand Surg Am. 2003;28(1):105–110. doi: 10.1053/jhsu.2003.50006. [DOI] [PubMed] [Google Scholar]
- 20.Watson H K, Brown R E. Ulnar impingement syndrome after Darrach procedure: treatment by advancement lengthening osteotomy of the ulna. J Hand Surg Am. 1989;14(2 Pt 1):302–306. doi: 10.1016/0363-5023(89)90026-9. [DOI] [PubMed] [Google Scholar]
- 21.van Schoonhoven J, Fernandez D L, Bowers W H, Herbert T J. Salvage of failed resection arthroplasties of the distal radioulnar joint using a new ulnar head prosthesis. J Hand Surg Am. 2000;25(3):438–446. doi: 10.1053/jhsu.2000.6006. [DOI] [PubMed] [Google Scholar]
- 22.Berger R A Cooney W P III Use of an ulnar head endoprosthesis for treatment of an unstable distal ulnar resection: review of mechanics, indications, and surgical technique Hand Clin 2005214603–620., vii [DOI] [PubMed] [Google Scholar]
- 23.Fernandez D L, Joneschild E S, Abella D M. Treatment of failed Sauvé-Kapandji procedures with a spherical ulnar head prosthesis. Clin Orthop Relat Res. 2006;445:100–107. doi: 10.1097/01.blo.0000205901.13609.70. [DOI] [PubMed] [Google Scholar]
- 24.Willis A A, Berger R A, Cooney W P III. Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. J Hand Surg Am. 2007;32(2):177–189. doi: 10.1016/j.jhsa.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 25.Herbert T J, van Schoonhoven J. Ulnar head replacement. Tech Hand Up Extrem Surg. 2007;11(1):98–108. doi: 10.1097/bth.0b013e318033738a. [DOI] [PubMed] [Google Scholar]
- 26.Scheker L R. Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(9):1639–1644. doi: 10.1016/j.jhsa.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 27.Herzberg G. Periprosthetic bone resorption and sigmoid notch erosion around ulnar head implants: a concern? Hand Clin. 2010;26(4):573–577. doi: 10.1016/j.hcl.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 28.van Schoonhoven J, Mühldorfer-Fodor M, Fernandez D L, Herbert T J. Salvage of failed resection arthroplasties of the distal radioulnar joint using an ulnar head prosthesis: long-term results. J Hand Surg Am. 2012;37(7):1372–1380. doi: 10.1016/j.jhsa.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 29.Sotereanos D G, Göbel F, Vardakas D G, Sarris I. An allograft salvage technique for failure of the Darrach procedure: a report of four cases. J Hand Surg [Br] 2002;27(4):317–321. doi: 10.1054/jhsb.2001.0737. [DOI] [PubMed] [Google Scholar]
- 30.Greenberg J A, Sotereanos D. Achilles allograft interposition for failed Darrach distal ulna resections. Tech Hand Up Extrem Surg. 2008;12(2):121–125. doi: 10.1097/BTH.0b013e3181640346. [DOI] [PubMed] [Google Scholar]
- 31.Hartz C R, Beckenbaugh R D. Long-term results of resection of the distal ulna for post-traumatic conditions. J Trauma. 1979;19(4):219–226. doi: 10.1097/00005373-197904000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Minami A Iwasaki N Ishikawa J Suenaga N Yasuda K Kato H Treatments of osteoarthritis of the distal radioulnar joint: long-term results of three procedures Hand Surg 2005102-3243–248.16568521 [Google Scholar]
- 33.Glowacki K A. Hemiresection arthroplasty of the distal radioulnar joint. Hand Clin. 2005;21(4):591–601. doi: 10.1016/j.hcl.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 34.Daecke W, Martini A K, Schneider S, Streich N A. Amount of ulnar resection is a predictive factor for ulnar instability problems after the Sauvé-Kapandji procedure: a retrospective study of 44 patients followed for 1–13 years. Acta Orthop. 2006;77(2):290–297. doi: 10.1080/17453670610046055. [DOI] [PubMed] [Google Scholar]
- 35.Sauerbier M, Hahn M E, Berglund L J, An K N, Berger R A. Biomechanical evaluation of the dynamic radioulnar convergence after ulnar head resection, two soft tissue stabilization methods of the distal ulna and ulnar head prosthesis implantation. Arch Orthop Trauma Surg. 2011;131(1):15–26. doi: 10.1007/s00402-010-1089-0. [DOI] [PubMed] [Google Scholar]
- 36.Sauerbier M, Hahn M E, Fujita M, Neale P G, Berglund L J, Berger R A. Analysis of dynamic distal radioulnar convergence after ulnar head resection and endoprosthesis implantation. J Hand Surg Am. 2002;27(3):425–434. doi: 10.1053/jhsu.2002.31734. [DOI] [PubMed] [Google Scholar]


