Abstract
Carrageenan, a sulfated polysaccharide that is widely used as a food additive, induces inflammatory responses in animal models and human cells. The carrageenan-induced inflammatory cascades involve TLR4- and BCL10-dependent activation of NF-κB, leading to increased IL-8 production. Translocations involving BCL10 in the mucosa-associated lymphoid tissue (MALT) lymphomas are associated with constitutive activation of NF-κB. This report presents a mechanism by which carrageenan exposure leads to prolonged activation of both BCL10 and NF-κB in human colonic epithelial cells. Study findings demonstrate that nuclear RelA and RelB bind to an NF-κB binding motif in the BCL10 promoter in human colonic epithelial NCM460 and HT-29 cells. In vitro oligonucleotide binding assay, non-radioactive gel shift assay, and chromatin immunoprecipitation (ChIP) indicate binding of RelA and RelB to the BCL10 promoter. Prolonged inflammation follows activation of the BCL10-NFκB inflammatory loop in response to carrageenan, shown by increased BCL10, RelA, and IL-8 for 36 to 48 hours and increased RelB for 24 hours following withdrawal of carrageenan after 12 hours. In contrast, exposure to dextran sulfate sodium, which does not cause inflammation through TLR4 and BCL10 in the colonic epithelial cells, did not provoke prolonged activation of inflammation. The carrageenan-enhanced BCL10 promoter activity was blocked by caffeic acid phenethyl ester (CAPE) and MB-132 which inhibit NF-κB activation. These results indicate that NF-κB binding to the BCL10 promoter can lead to prolonged activation of the carrageenan-induced inflammatory cascade by a transcriptional mechanism involving an NF-κB – BCL10 loop.
1. Introduction
1.1 Background about carrageenan exposure
Carrageenans are highly sulfated polysaccharides that are obtained from red seaweeds (Rhodophycae). They have been widely used for decades as a thickener, stabilizer, or emulsifying agent in many processed foods in the Western diet, including dairy products, processed meats, soymilk, and infant formula, and are also used in a variety of other products, such as cosmetics, toothpaste, room deodorizers, and pharmaceuticals. Current data suggest average consumption of 250 mg/day of carrageenan in the United States. Multiple studies in mammals have demonstrated that carrageenan exposure predictably causes inflammation, including development of ulcerations, polyps, colitis, and colorectal tumors, and carrageenan has been used in thousands of cell-based and animal experiments to cause inflammation, primarily to study mediators of inflammation and anti-inflammatory therapeutics [1-3].
1.2 Carrageenan stimulates TLR4 – BCL10 mediated pathway of inflammation
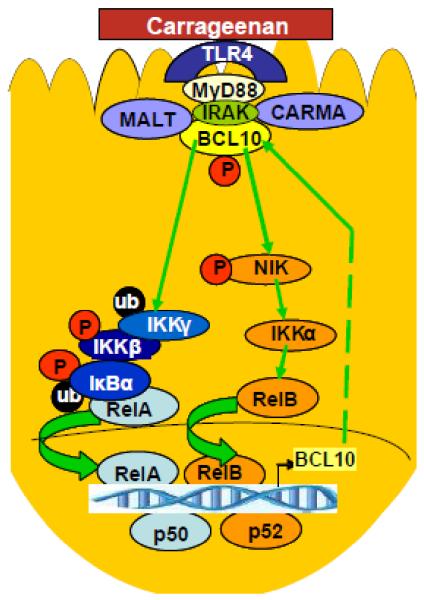
In human colonic epithelial cells and murine models, we have reported that carrageenan triggers innate immune pathways of inflammation in which TLR4 and BCL10 are critical [4-8]. The inflammatory response initiated by carrageenan exposure activated both canonical, involving RelA (p65) and p50, and non-canonical, involving RelB and p52, pathways of NF-κB activation. We have demonstrated that carrageenan induces inflammatory responses via three cascades: 1) a TLR4, BCL10, IkappaB kinase (IKK)γ, and phospho-IκBα-mediated activation of RelA; 2) a TLR4, BCL10, phospho-NF-κB-inducing kinase (NIK), IKKα-mediated activation of the non-canonical pathway leading to nuclear translocation of p52 and RelB; and 3) a reactive-oxygen species (ROS)-mediated pathway requiring Hsp27 and IKKβ (Fig. 1) [4-8]. Recent work also demonstrated that carrageenan-induced inflammation caused glucose intolerance, insulin resistance, and impaired insulin signaling in mouse and cell-based studies [9]. These effects are consistent with the role of TLR4-induced inflammation reported in diabetes and carrageenan stimulation of TLR4-mediated inflammatory cascades [10].
Figure 1. Schematic illustration of carrageenan-stimulated inflammatory signaling pathways in human colonocytes.
Schematic illustration indicates the presence of a signaling loop following exposure to carrageenan. Carrageenan through TLR4 and BCL10 leads to nuclear translocation/activation of NF-κB, both RelA and RelB. In turn, these nuclear factors bind to the putative NF-κB binding element in the BCL10 promoter, stimulating increased expression of BCL10, which again leads to increased nuclear translocation/activation of NF-κB through effects on the IKK signalosome.
1.3 BCL10 is associated with constitutive activation of NF-κB in the MALT lymphomas
BCL10, which encodes a cytosolic protein composed of 233 amino acids, has a pivotal role in the innate immune-mediated pathways of inflammation that require TLR4. The BCL10 gene (locus 1p22) was originally identified from a recurrent breakpoint t(1;14)(p22;q32) found in gastric mucosa-associated lymphoid tissue (MALT) lymphomas that was associated with constitutive activation of NF-κB [11,12]. BCL10 was shown to be an adaptor protein that mediated canonical NF-κB signaling in T and B lymphocytes. Subsequently, a critical role for BCL10 in non-myeloid cells was identified, including mediation of the inflammatory cascade in response to carrageenan, lipopolysaccharide, platelet-activating factor (PAF), lysophosphatidic acid, and angiotensin II [4, 13-17]. Experiments with BCL10 silencing and mutation in human colonic epithelial cells demonstrated a requirement for BCL10 in production of canonical and non-canonical activation of NF-κB, involving NF-κB components RelA and RelB, respectively [6,7,18]. In this report, we present a transcriptional mechanism by which carrageenan initiates an inflammatory loop, involving the up-regulation of BCL10 expression and prolonged activation of canonical and non-canonical NF-κB pathways of inflammation. This transcriptional effect is based on our previous identification of a putative NF-κB binding sequence in the BCL10 promoter that was activated following exposure to PAF [17].
2.0 Materials and Methods
2.1 Cell culture of colonic epithelial cells
NCM460 cells, a human colonic epithelial cell line derived from normal colonic mucosa, were grown in M3:10™ media (INCELL, San Antonio, TX) and maintained at 37°C in a humidified 5%CO2 environment with media changes at 2-day intervals [19]. The HT-29 (ATCC #HTB-38) cell line, a human colonic adenocarcinoma cell line, was grown in DMEM media with 10% FBS.
2.2 BCL10 promoter activity by luciferase assay
A 1310 bp promoter region of BCL10 gene (NM_003921) that was cloned previously into pGL2 plasmid (Promega, Fitchburg, WI) was transiently transfected into NCM460 cells using Lipofectamine 2000 (Invitrogen, Carlsbad, CA) [17]. Twenty-four hours post-transfection, cells were treated with λ-carrageenan (1 μg/ml; Sigma Chemical Company, St. Louis, MO) for 24 h. Promoter activity was measured utilizing firefly luciferase assay kit (Promega) as described previously and expressed as relative luciferase units (RLU)/mg protein [17]. Putative transcription factor binding sites in the promoter region where identified using TFSEARCH and Motif Search (http://motif.genome.jp/)., as previously described [17].
2.3 BCL10 and phospho-BCL10 by ELISA
A standardized BCL10 ELISA was used to determine the BCL10 content following stimulation by carrageenan, with or without caffeic acid phenethyl ester (CAPE), an inhibitor of NF-κB activation or MG-132, a proteasomal inhibitor [4,20,21]. Cells were pre-treated with CAPE (50 μM × 1 hr) or MG-132 (20 μM × 2 h), and then in combination with carrageenan (1 μg/ml × 24 h). Phospho-BCL10 was detected by cell-based ELISA using phospho(Ser138)-BCL10 antibody, as previously described [6,7].
2.4 RelA, RelB and c-Rel binding to BCL10 promoter by oligonucleotide-based ELISA
Nuclear extracts were prepared from control or carrageenan-treated NCM460 cells by a nuclear extraction kit (Active Motif, Carlsbad, CA). Sense and antisense oligonucleotides encompassing the putative NF-κB binding region in the BCL10 promoter and corresponding mutated constructs were commercially synthesized. After being annealed, the double-stranded oligonucleotides [NF-κB (NF) consensus oligonucleotide: 5′-GGGACTTTCC-3′; NF-κB Experimental binding site in BCL10 promoter (NFE): 5′-GGAAACGCCC-3′; NFE Mutated (NFEM): 5′-GTCCACGCCC-3′] were coated onto the wells of 96-well microtiter plates according to the reported procedure [22]. Treated and control nuclear extract samples were added to the coated wells and incubated for one hour. NF-κB components (RelA, RelB or c-Rel) bound to the coated oligonucleotides were captured by anti-RelA, anti-RelB or anti-c-Rel antibodies and detected by an anti-rabbit-HRP-conjugated IgG (Active Motif). Color development was performed with hydrogen peroxide/TMB chromogenic substrate, and intensity of the developed color proportionately represented the quantity of NF-κB component in each sample. The sample values were normalized with the total cell protein determined by protein assay kit (Pierce, ThermoFisher Scientific, Rockford, IL).
2.5 Detection of DNA-protein interactions by Digoxigenin (DIG)-non-radioactive gel shift assay
The binding of RelA (p65) to the putative NF-κB binding element was detected utilizing the nonradioactive DIG Gel Shift Kit (Roche, Indianapolis, IN). Nuclear extracts from control or carrageenan-treated cells were prepared using the nuclear extraction kit (Active Motif). Recombinant terminal transferase and digoxigenin (DIG)-11-ddUTP were used to label the 3′ end of the NF-κB oligonucleotide binding site in the BCL10 promoter (NFE) which differed from the consensus oligonucleotide for NFκB (NF) and the mutated NF-κB binding sequence in BCL10 promoter (NFEM). The labeled probe was incubated with the nuclear extracts with or without competition by unlabeled oligos, with or without specific RelA or p50 antibodies, for analysis of competition, as described previously [7]. Nuclear extracts and probes were run on a 4% polyacrylamide gel. An alkaline phosphatase conjugated anti-digoxigenin antibody bound to the DIG-labeled oligonucleotide-protein complex, and the immobilized alkaline phosphatase removed a phosphate group from the chemiluminescent substrate CSPD, thereby emitting a signal that was detected and proportionate to the amount of bound NFE.
2.6 Detection of DNA-protein interactions by chromatin immunoprecipitation (ChIP) assay
ChIP assay was performed utilizing a ChIP assay kit (Active Motif). Control and carrageenan-treated HT-29 cells were fixed with 1% formaldehyde for 10 min at room temperature, followed by shearing of chromatin by sonication. Sheared DNA was incubated with anti-RelA and anti-RelB antibodies (Active Motif) for 1 h. Protein-DNA complexes were precipitated by protein A-coupled agarose beads. After purification of the DNA from the immunoprecipitated complexes by reversal of cross-linking, followed by proteinase K treatment, real-time RT-PCR was performed using Brilliant SYBR Green QRT-PCR master mix (Stratagene, La Jolla, CA) and M×3000 (Stratagene) with the primer pair (forward: 5′-ACGGAAACGATGCCTTATGA-3′ and reverse: 5′-TCCTTCCCTCTAGGCTCAGG-3′) that encompassed the putative NF-κB binding element in the BCL10 promoter. Band intensity was compared between the carrageenan-treated and the control samples on a 1.5% agarose gel.
2.7 Carrageenan and Dextran Sulfate Sodium (DSS) withdrawal studies
NCM460 and HT-29 cells grown to 60% confluency in 24-well plates were treated with λ-carrageenan (1 μg/ml) or DSS (1 μg/ml; Sigma, St. Louis, MO) for 12 h. In selected wells, carrageenan or DSS treatment was continued for 60 h, with exchange of fresh, carrageenan or DSS-containing media every 12 h. In other wells, carrageenan or DSS was withdrawn after 12 h, and fresh media, without carrageenan or DSS was exchanged every 12 h. Samples (cells or spent media) from all preparations were collected at 12 h intervals. Spent media were stored at −80°C for subsequent IL-8 measurement; cells were washed with 1×PBS and stored at −80°C for later processing to measure RelA or RelB in the nuclear extracts.
2.8 Statistical analysis
Data are the mean ± Standard Deviation (S. D.) of three independent biological samples with two technical replicates of each determination, unless stated otherwise. Statistical significance was determined by one-way ANOVA followed by a post-hoc Tukey–Kramer test for multiple comparisons, unless stated otherwise in the Results or Figure Legends, using Prism or InStat software (GraphPad, Carlsbad, CA). Asterisks represent significant differences compared to control, with * for p≤0.05, ** for p≤0.01, and *** for p≤0.001.
3.0 Results
3.1 Carrageenan exposure increased BCL10 promoter activity
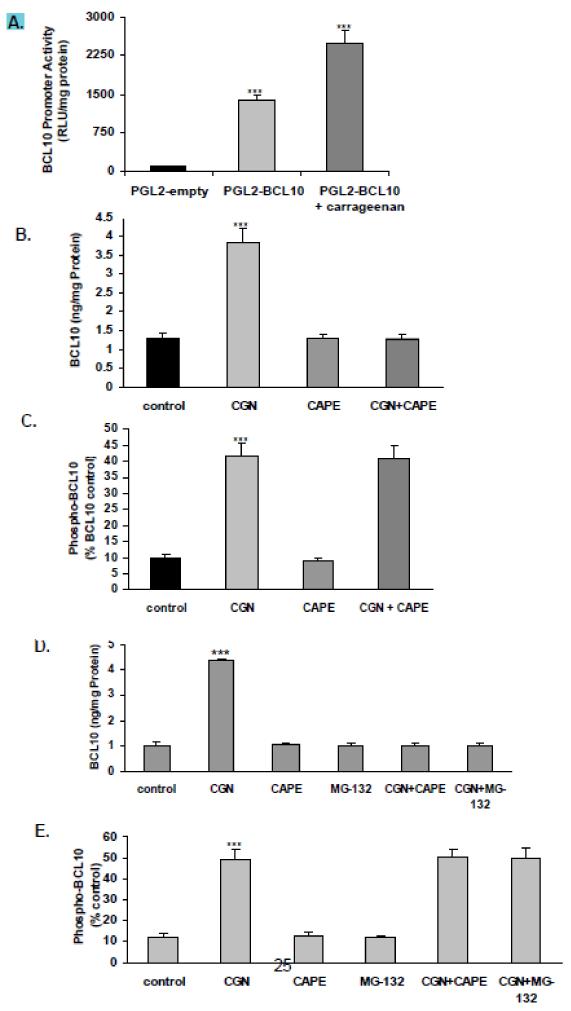
NCM460 cells, derived from normal colonic epithelial cells, were exposed to λ-carrageenan (carrageenan 1 μg/ml × 24 hr) to examine the effects on BCL10 promoter activity. A 1310 bp fragment of the 5′-untranslated region of the BCL10 gene that has cis elements for various transcription factors, including NF-κB, was cloned previously in the pGL2 reporter plasmid [17]. When transiently transfected into NCM460 cells, the cloned fragment showed 10-fold greater promoter activity, as compared to pGL2 empty vector control. Carrageenan treatment for 24 hours further increased the BCL10 promoter activity (~2-fold) (Fig. 2A), consistent with previously reported increases in BCL10 expression following carrageenan. The carrageenan-induced increase in BCL10 protein expression was completely inhibited when NCM460 cells were pre-incubated with caffeic acid phenethyl ester (CAPE 50 μM × 1 h, then in combination with carrageenan 1 μg/ml × 24 h), an inhibitor of NF-κB nuclear translocation (Fig. 2B). In contrast, the carrageenan-induced increase in phospho-BCL10 level was unaffected (Fig. 2C). In the colorectal adenocarcinoma cell line HT-29, similar decline in BCL10 protein expression and no change in phospho-BCL10 were demonstrated with CAPE and with the proteasomal inhibitor MG-132 (20 μM × 2 h, then in combination with λ-carrageenan × 24 h) (Fig. 2D, 2E), indicating that these effects are not cell-line specific. These findings demonstrate that the enhanced BCL10 expression following carrageenan is a transcriptional effect that requires the nuclear translocation of NF-κB.
Figure 2. Carrageenan enhances BCL10 promoter activity in NCM460 cells.
A. When NCM460 cells were transiently transfected with the BCL10 promoter construct in the pGL2 vector or with the empty vector and exposed to carrageenan (1 μg/ml × 24 hr), promoter activity increased significantly. Results are mean ± S.D. of five independent experiments (***p<0.001 vs. control).
B. NCM460 cells were pre-treated with CAPE (50 μM × 1 hr, then in combination with carrageenan 1 μg/ml × 24 h), and BCL10 protein was measured by ELISA in the cell lysate. The carrageenan-induced increase in BCL10 was inhibited in the presence of CAPE.
C. Phospho(Ser138)-BCL10 protein expression in NCM460 cells, as detected by cell-based ELISA, increased following carrageenan and was unaffected by CAPE.
D. In the HT-29 cells, both CAPE and MG-132 (20 μM for 2 hr, then in combination with carrageenan 1 μg/ml × 24 h) inhibited the carrageenan-induced increase in BCL10, as detected by ELISA.
E. In the HT-29 cells, neither CAPE nor MG-132 affected the carrageenan-induced increase in phospho(Ser138)-BCL10.
Results shown are mean ± S.D. of three independent experiments (***p<0.001 vs. control). [CGN=carrageenan; CAPE=caffeic phenethyl ester]
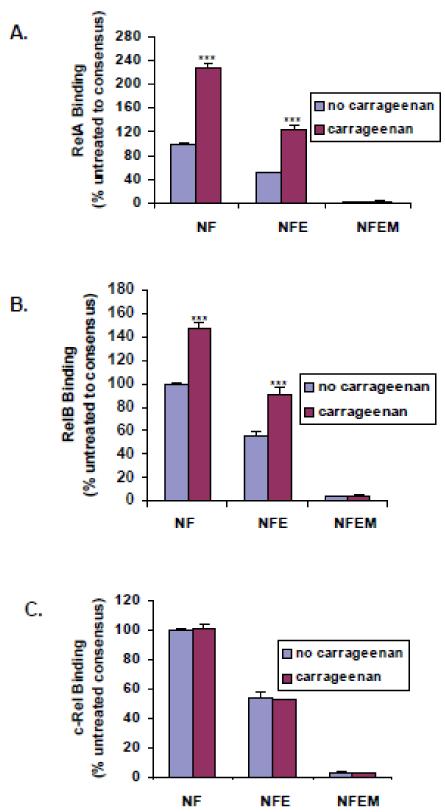
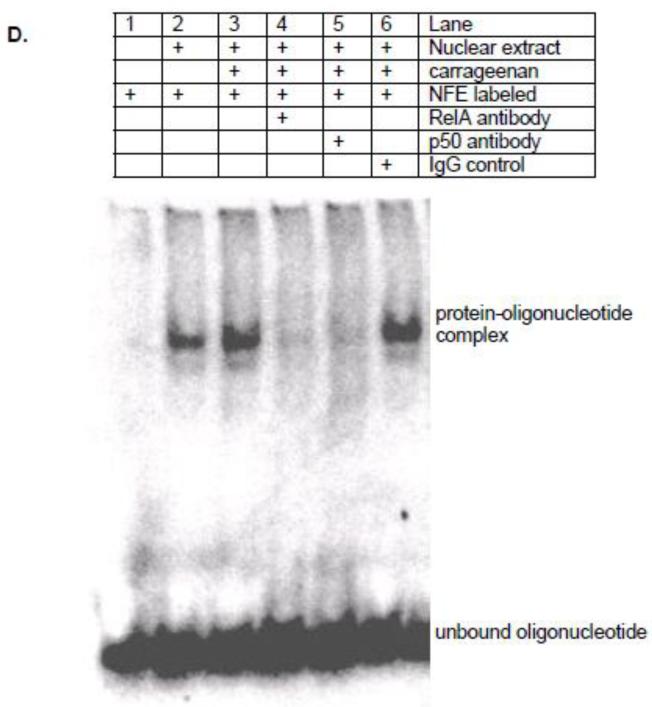
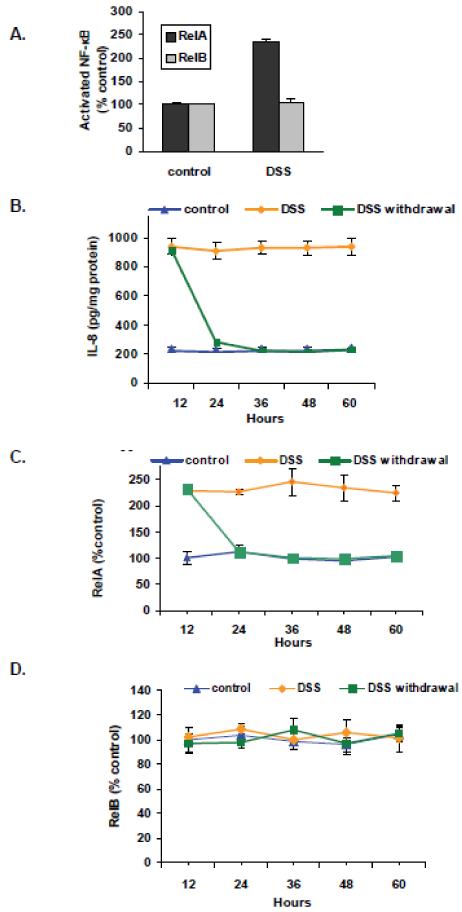
3.2 Carrageenan increased RelA and RelB binding to BCL10 promoter
3.2.1 Oligonucleotide-based ELISA
The BCL10 promoter construct contains a sequence with high homology to the established NF-κB consensus sequence that was identified as a putative NF-κB binding sequence [17]. By oligonucleotide-based ELISA, carrageenan exposure significantly increased binding of RelA to the NFE (experimental NF-κB binding site in BCL10 promoter), as well as to the established NF-κB consensus sequence (NF) (p<0.001), but not to the mutated sequence (NFEM) in the NCM460 cells (Fig. 3A). Carrageenan treatment also significantly increased binding of RelB to the NFE and NF (p<0.001), but not the NFEM (Fig. 3B). Carrageenan treatment did not induce c-Rel binding to NF, NFE or NFEM (Fig. 3C).
Figure 3. Oligonucleotide-protein assays demonstrate binding to the NF-κB binding element in the BCL10 promoter.
The double-stranded annealed nucleotides corresponding to the established NF-κB consensus sequence (NF), the putative, experimental NF-κB binding element in the BCL10 promoter (NFE), or its mutated version (NFEM) were coated onto the wells of microtiter plates.
A. In the NCM460 cells, binding of RelA to the NF-κB consensus sequence (NF) and NF-κB binding element in the BCL10 promoter (NFE) was increased following exposure to carrageenan, whereas binding to the mutated sequence (NFEM) was unaffected.
B. Similarly, binding of RelB to NF and NFE was increased after carrageenan, but binding to NFEM was unaffected.
C. No increase in binding of c-Rel to either NF, NFE or NFEM was detected following carrageenan.
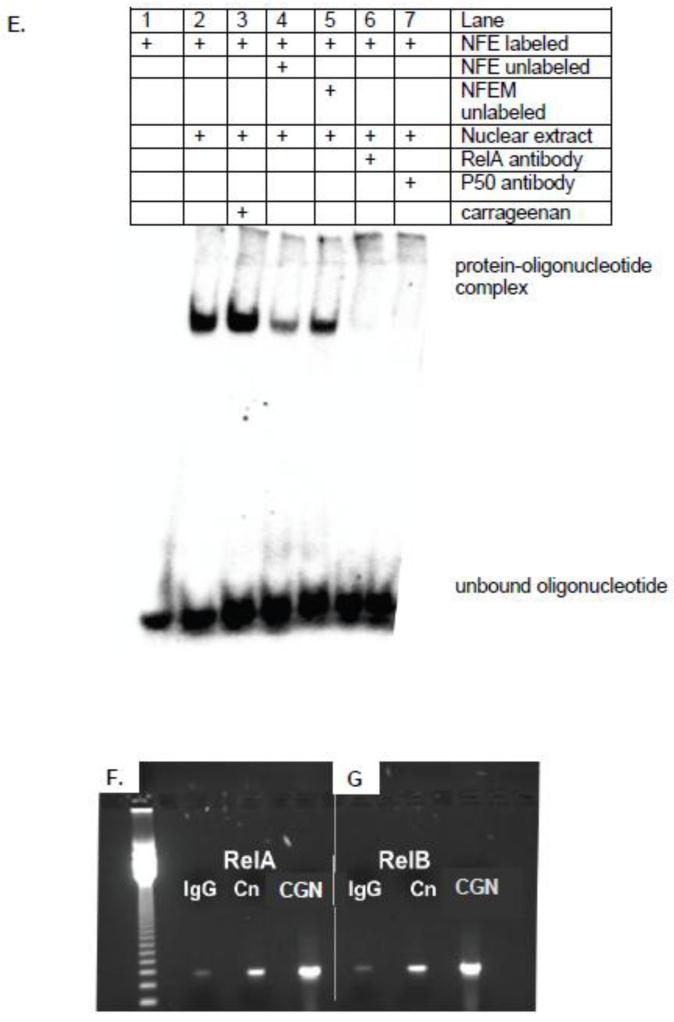
D. Digoxigenin (DIG)-non-radioactive gel shift assay was performed with untreated NCM460 cell nuclear extract and following exposure of the cells to carrageenan. Lane 1: No nuclear extract; Lane 2: nuclear extract and labeled NFE; Lane 3: carrageenan-treated nuclear extract and NFE; Lane 4: carrageenan-treated nuclear extract, NFE and RelA antibody; Lane 5; carrageenan-treated nuclear extract, NFE, and p50 antibody, and Lane 6: carrageenan-treated nuclear extract, NFE, and IgG control. Studies demonstrate increase in the oligonucleotide-protein band following carrageenan (Lane 3 vs. Lane 2). Exogenous RelA and p50 antibodies compete for binding between the endogenous RelA (Lane 4) or p50 (Lane 5) in the nuclear extract and the oligonucleotide binding site in the BCL10 promoter (NFE), eliminating the protein-oligonucleotide band. In contrast, IgG has no effect on the binding of the nuclear extract and the labeled NFE (Lane 6).
E. Digoxigenin (DIG)-non-radioactive gel shift assay showed carrageenan enhancement of RelA binding to the NF-κB binding element in the BCL10 promoter. Competition studies with cold (unlabeled) NFE or cold (unlabeled) and mutated NFEM or with RelA and p50 antibodies were performed to confirm the specificity of the protein-DNA interaction between RelA or p50 with the NF-κB binding site in the BCL10 promoter. Lane 1: No nuclear extract; Lane 2: control nuclear extract and labeled NFE; Lane 3. carrageenan-treated nuclear extract and NFE; Lane 4: competition by cold NFE; Lane 5: competition by cold NFEM; Lane 6: competition by RelA antibody; Lane 7: competition by p50 antibody. A representative blot of 4 independent experiments with similar results is shown.
F, G. Increased binding of RelA and RelB to the BCL10 promoter by chromatin immunoprecipitation (ChIP) assay following carrageenan exposure. Control or carrageenan (1 μg/ml × 24 h) treated NCM460 cells were fixed with formaldehyde, and chromatin prepared from these cells was sheared, and then immunoprecipitated with anti-RelA, anti-RelB antibody or with control IgG. Specific primers were used to amplify the promoter region containing the NF-κB binding element in the human BCL10 promoter. Amplified products were resolved on 1.5% agarose gel and indicate marked increase following carrageenan vs. control.
[Cn=control; CGN=lambda-carrageenan; NF=NF-κB consensus sequence; NFE=experimental NF-κB binding element in the BCL10 promoter; NFEM=mutated NF-κB binding element in the BCL10 promoter]
3.2.2 Non-radioactive competitive oligonucleotide-protein gel shift assay
The carrageenan-induced enhancement of NF-κB binding to NFE was also shown by competitive oligonucleotide-protein gel shift assay in the NCM460 cells (Fig. 3D, 3E). Digoxigenin (DIG)-non-radioactive gel shift assay was performed with NCM460 cell nuclear extract alone and following exposure of the cells to carrageenan. The nuclear extract-NFE (protein-oligonucleotide) band intensity was increased in response to carrageenan treatment, compared to the untreated control (Lane 3 vs. Lane 2, Fig. 3D). The addition of RelA antibody or p50 antibody successfully competed for binding between the endogenous RelA (Lane 4) or p50 (Lane 5) in the nuclear extract and the labeled oligonucleotide binding site in the BCL10 promoter (NFE), and eliminated the protein-oligonucleotide band. In contrast, the IgG negative control had no effect (Lane 6).
Nuclear extract binding to labeled NFE was competed out by unlabeled NFE oligonucleotide (lane 4, Fig. 3E), but not by the mutated unlabeled oligonucleotide (NFEM) (lane 5). In the antibody competition assay, the RelA antibody (lane 6) and the p50 antibody (lane 7) competed out the binding of the endogenous Rel A or p50 in the nuclear extract to labeled NFE, as noted above.
3.2.3 Chromatin immunoprecipitation assay
Chromatin immunoprecipitation (ChIP) assay examined the in vivo interaction of RelA and RelB proteins with the BCL10 promoter following carrageenan exposure in the HT-29 cells. The BCL10 promoter had increased interaction with RelA (Fig. 3F) and RelB (Fig. 3G) in carrageenan-treated cells, compared to control. The specificity of the ChIP was verified using control IgG-precipitated chromatin, and no PCR-amplified product was visible.
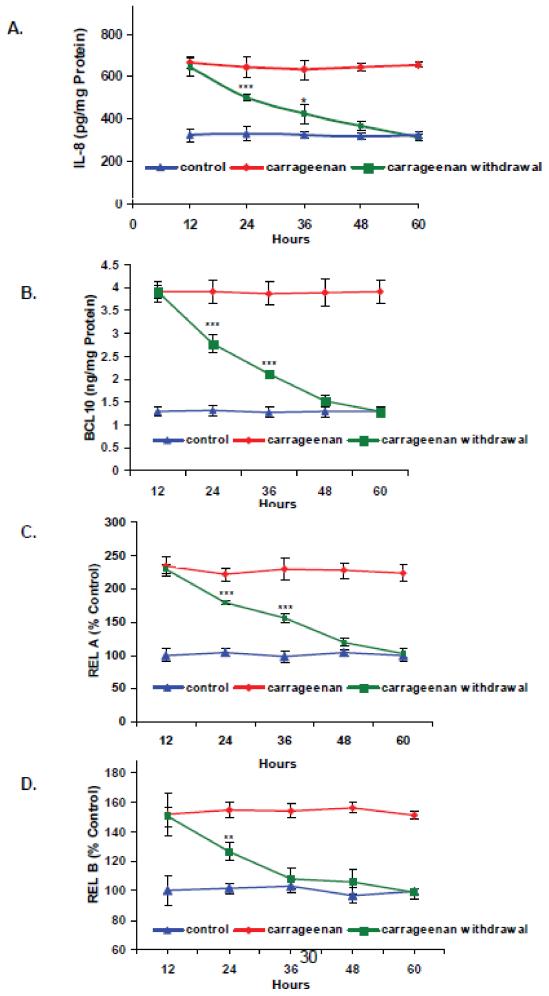
3.3 Carrageenan exposure caused prolonged NF-κB activation in NCM460 and HT-29 cells
Since the function of the NF-κB-BCL10 loop was anticipated to lead to a prolonged inflammatory response following carrageenan exposure, the duration of the effects of carrageenan stimulation were tested following carrageenan withdrawal. In the NCM460 cells, IL-8 secretion in the spent media (Fig. 4A), total cellular BCL10 protein content (Fig. 4B), and nuclear RelA (Fig. 4C) remained significantly elevated compared to control for 24 h after carrageenan withdrawal. Nuclear RelB (Fig. 4D) remained significantly elevated for 12 h after carrageenan withdrawal. Sustained increase in BCL10 was also demonstrated by Western blot at 36 hours which indicates significantly increased BCL10 protein, compared to untreated control (Fig. 4E), although less than with continuous carrageenan treatment. Phospho(Ser138)-BCL10 was markedly increased at 36 hours following continuous exposure to carrageenan, as demonstrated by Western blot (Fig. 4F). When carrageenan was withdrawn after 12 hours, the intensity of the band for phospho-BCL10 at 36 hours was much reduced. In the HT-29 cells, even larger sustained effects were observed following withdrawal of carrageenan than were evident in the NCM460 cells (Supplementary Figures 1A-1D).
Figure 4. Sustained increases in IL-8, BCL10, RelA, and RelB following carrageenan exposure in NCM460 and HT-29 cells.
NCM460 cells were either exposed to carrageenan continuously for 60 hours with media exchange and replenishment of carrageenan every 12 hours, exposed to carrageenan for only an initial 12 h period with media exchange every 12 hours, or not exposed to carrageenan at all with media exchange every 12 hours. Statistical significance was determined by one-way ANOVA with Tukey-Kramer post-test.
A. In the NCM460 cells, when compared to untreated controls, IL-8 remained significantly elevated at 24 (p<0.001) and 36 hours (p<0.05) in the spent media of the cells treated for only 12 hours.
B. Total cellular BCL10 remained significantly increased at 24 (p<0.001) and 36 (p<0.001) hours, following withdrawal of carrageenan after 12 hours.
C. RelA remained significantly increased in the nuclear lysates of the NCM460 cells at 24 (p<0.001) and 36 (p<0.001) hours, following 12 hours of carrageenan exposure.
D. RelB remained significantly increased at 24 (p<0.01) hours in the NCM460 cells following withdrawal of carrageenan after 12 hours.
E. Western blot demonstrates increase in BCL10 protein at 36 hours following withdrawal of carrageenan after 12 hours. Continued exposure to carrageenan leads to more intense staining. Densitometry confirms the visual impression. [CGN=carrageenan]
F. Western blot demonstrates marked increase in the band intensity of phospho-BCL10 at 36 hours upon continuous exposure to carrageenan, and a much smaller response when carrageenan was withdrawn after 12 hours.
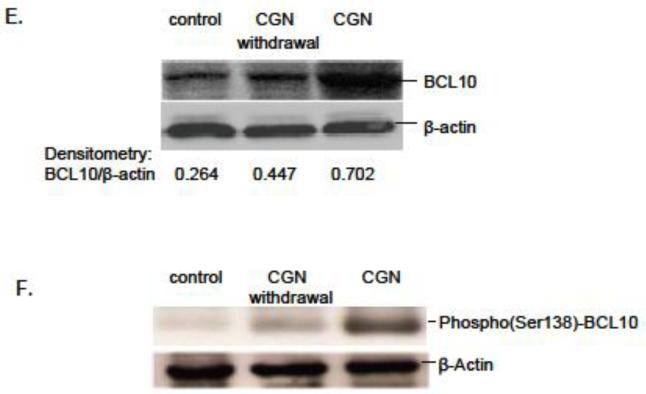
3.4 DSS treatment did not lead to sustained NF-κB activation
Effects of carrageenan differed from those obtained following exposure to dextran sodium sulfate (DSS), the sulfated polysaccharide that is very commonly used to cause inflammation in cell-based and animal experiments. DSS (1 μg/ml × 24 h) increased RelA, but not RelB in NCM460 cells (Fig. 5A). Withdrawal experiments using DSS in the NCM460 and HT-29 cells showed that DSS stimulation did not produce sustained increases in RelA or IL-8. Treatment with DSS (1 μg/ml) for 12 h significantly increased IL-8 secretion (Fig. 5B) and nuclear RelA (Fig. 5C), compared to control. However, upon DSS withdrawal, IL-8 and RelA levels declined to the control levels by 24 h, indicating that the inflammatory response was not sustained. RelB did not increase following exposure to DSS in the NCM460 cells (Fig. 5D). Similar lack of sustained increases in IL-8 and RelA was demonstrated in the HT-29 cells following exposure to DSS (Supplementary Figures 2A-2B).
Figure 5. DSS-induced increase in IL-8 and RelA (p65) are not sustained upon DSS withdrawal in NCM460 or HT-29 cells.
A. DSS exposure produced no increase in RelB in the NCM460 cells.
NCM460 cells were initially exposed to DSS (1 μg/ml) for 12 hr. This was followed by either replenishment with fresh DSS containing media every 12 h, or with media without DSS. Samples (spent media or cells) were harvested every 12 h.
B. IL-8 declined to untreated level by 24 hours in the NCM460 cells.
C. RelA declined to untreated level by 24 hours in the NCM460 cells. [DSS=dextran sulfate sodium]
D. RelB did not increase following exposure to DSS in the NCM460 cells.
4.0 Discussion
Previous reports have presented three pathways by which exposure to the common food additive carrageenan stimulates inflammation in human colonic epithelial cells (Fig. 1) [4-8]. These include pathways initiated by interaction of carrageenan with the toll-like receptor (TLR)-4, requiring MyD88, IRAK, and BCL10. The canonical pathway of NF-κB activation involves BCL10 interaction with IKKγ, the regulatory subunit of the IKK signalosome, leading to IKKγ ubiquitination, IKKβ phosphorylation of IκBα, and nuclear translocation of NF-κB RelA (p65) and p50. Alternatively, as in the non-canonical pathway of NF-κB activation, phospho-BCL10 interacts with NIK and NIK is phosphorylated, leading to the phosphorylation of IKKα and the nuclear translocation of RelB and p52. In addition to the TLR4-BCL10 mediated pathways, carrageenan exposure stimulates a reactive oxygen species (ROS)-mediated pathway, in which phospho-Hsp27 interacts with the IKK signalosome, leading to the phosphorylation of IκBα and the nuclear translocation of NF-κB. To these pathways, we now add a feedback loop, by which NF-κB binding to the BCL10 promoter leads to increased production of BCL10, which can thereby continue activation of the inflammatory process.
The caspase recruitment domain (CARD)-containing protein BCL10 has previously been implicated in sustained inflammatory processes in lymphocytes, since translocations involving BCL10 are of etiologic significance in development of mucosa-associated lymphoid tissue (MALT) lymphomas [11,12]. The MALT lymphomas, first described in 1983, are the third most common subtype of non-Hodgkin’s Lymphoma. They arise in a wide range of sites, including most commonly stomach (~70%), lung (~14%), then ocular adnexa, thyroid, and small intestine [23-25]. The majority of the gastric MALT lymphomas are attributable to Helicobacter pylori infections, and are amenable to cure by eradication of the infection. The association of reciprocal chromosomal translocations involving BCL10 [t(1;14)(p22;q32)] or MALT1 [t(11;18)(q21;q21) and t(14;18)(q32;q21)] with MALT lymphomas that are not attributable to H. pylori indicates an overlap between the molecular mechanisms that are manifestations of infection- and inflammation-associated malignancies.
Carrageenan due to its unique chemical structure stimulates innate immune responses and evokes sustained activation of NF-κB and BCL10. Previously, we reported that NF-κB activation in response to DSS treatment was mediated via reactive oxygen species and Hsp27, and did not involve TLR4 or BCL10, since BCL10 silencing had no impact on the responses to DSS, DSS exposure did not increase BCL10, and MyD88 and TLR4 were not required for DSS effects [26]. In the current study, inflammatory responses are not prolonged following withdrawal of DSS, consistent with observed effects in animal models [27]. The difference in the inflammatory mechanisms between carrageenan and DSS, both of which are highly sulfated polysaccharides, but vary in their specific hexoses and in their glycosidic bonds, supports the essential role of the unique chemical structure of carrageenan, involving its unusual alpha-1,3-galactosidic bond, in activation of an innate immune response [28,29]. In contrast, DSS, which is not used as a food additive, but predictably causes inflammation, is composed of glucose residues, linked predominantly in alpha-1,6-bonds [30]
The post-translational modifications of BCL10 may modulate the effects of specific inflammatory signals, and BCL10 may serve a critical function in the downstream regulation of different inputs, such as those from carrageenan, lipopolysaccharide, platelet-activating factor, angiotensin II, and lysophosphatidic acid [6,7,13-18]. The phosphorylation of BCL10 Ser138 is required for phosphorylation of NIK in the non-canonical pathway of NF-κB activation, and was not affected by proteasomal inhibition by MG-132 or by CAPE, indicating that BCL10 phosphorylation occurs independently of NF-κB nuclear translocation, in contrast to BCL10 expression [6,7,18,21]. The study finding that the RelB activation is sustained for a shorter interval than the RelA activation suggests that another process, likely involving the phosphorylation of NIK, BCL10, or IKKα, is also required to prolong the activation of the non-canonical pathway.
Exposure of cells to inflammatory stimuli results in rapid phosphorylation and degradation of IκBα and subsequent translocation of NF-κB to the nucleus. These events enable prompt cellular response in the absence of de novo protein synthesis [31,32]. Given the central role of NF-κB in the pathogenesis and maintenance of chronic inflammatory states, examination of mechanisms that contribute to the prolonged activation of NF-κB is of considerable relevance to human disease. In the current report, carrageenan exposure for 12 hours caused sustained RelA activation, IL-8 production, and BCL10 protein level for 48 hours. Since upregulation of BCL10 expression results from NF-κB activation, and NF-κB activation following carrageenan exposure involves BCL10, a positive feedback loop involving BCL10 and NF-κB that causes prolonged activation of NF-κB in response to carrageenan may have clinical significance, leading to extended inflammation in intestinal epithelial cells. The relationship between infectious or inflammatory processes and malignancy, such as H. pylori and gastric cancer, human papillomavirus and cervical cancer, or ulcerative colitis and colorectal carcinoma, is also of interest, since therapeutic interventions with anti-microbial and anti-inflammatory agents that retard inflammation may impact upon neoplastic transformation. Identification of specific transcriptional regulatory mechanisms, such as this NF-κB-BCL10 loop that is set in motion by carrageenan exposure, may contribute to improved understanding of the origins of malignancy, as well as of chronic inflammation.
Supplementary Material
Supplementary Figure 1. In the HT-29 cells, effects were determined at 12, 24, 36, and 48 hour time points following withdrawal of carrageenan, in contrast to no treatment control and renewed treatment every 12 hours.
A. IL-8 remained significantly elevated at 24 (p<0.001), 36 (p<0.001), and 48 (p<0.01) hours following withdrawal of the carrageenan after 12 hours of treatment, suggesting a more prolonged effect in the HT-29 cells than in the NCM460 cells.
B. The BCL10 remained significantly increased at 24 (p<0.001) and 36 (p<0.001) hours following withdrawal at 12 hours.
C. The increase in RelA remained significant at 24( p<0.001), 36 (p<0.001), and 48 (p<0.05) hours.
D. RelB was significantly increased at 24 (p<0.01) hours, following withdrawal of the carrageenan at 12 hours.
Supplementary Figure 2. In the HT-29 cells, the effects of carrageenan were contrasted with those of DSS.
A. Similar to the findings in the NCM460 cells, in the HT-29 cells the increase in IL-8 was not sustained following withdrawal of DSS.
B. The RelA declined to the control level by 24 hours in the HT-29 cells.
Highlights.
Exposure to common food additive carrageenan initiates protracted inflammation
Presence of NF-κB binding site in the BCL10 promoter sets up inflammatory loop
Both RelA and RelB bind to the NF-κB binding site in the BCL10 promoter
In contrast to carrageenan, DSS exposure does not initiate prolonged inflammation
Acknowledgments
Supported by Department of Veterans Affairs and the NIDDK (R01-DK54016, R01-DK81858 and PO1-DK67887).
Abbreviations
- BCL10
B-cell leukemia/lymphoma 10
- CAPE
caffeic phenethyl ester
- CARMA
caspase recruitment domain membrane-associated guanylate kinase
- CBM
CARMA-BCL10-MALT complex
- CGN
carrageenan
- ChIP
chromatic immunoprecipitation
- DSS
dextran sulfate sodium
- Hsp
heat-shock protein
- MALT
mucosa-associated lymphoid tissue
- IκB
inhibitor of κB
- IKK
inhibitor of IκB kinase
- IL-8
Interleukin-8
- IRAK
Interleukin-β receptor associated kinase
- NF
NF-κB consensus oligonucleotide
- NF-κB
nuclear factor kappaB
- NFE
experimental NF-κB binding site in BCL10 promoter
- NFEM
mutated experimental NF-κB binding site in BCL10 promoter
- NIK
NF-κB inducing kinase
- PAF
platelet-activating factor
- ROS
reactive oxygen species
- TLR4
Toll-like receptor 4
- Ub
ubiquitin
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Tobacman JK. Environ. Health Perspect. 2001;109:983–94. doi: 10.1289/ehp.01109983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Encyclopædia Britannica . Encyclopædia Britannica. 2010. “algae” Encyclopædia Britannica Online. Web. 22 Jan 2011. http://search.eb.com/eb.article-31714. [Google Scholar]
- [3].West J, Miller KN. Agarophytes and carrageenophytes. California Department of Fish and Game; 2001. California’s living marine resources: a status report; pp. 286–287. [Google Scholar]
- [4].Borthakur A, Bhattacharyya S, Dudeja PK, Tobacman JK. Am. J. Physiol. Gastrointest. Liver Physiol. 2007;292:G829–G838. doi: 10.1152/ajpgi.00380.2006. [DOI] [PubMed] [Google Scholar]
- [5].Bhattacharyya S, Gill R, Chen ML, Zhang F, Linhardt RJ, Dudeja PK, Tobacman JK. J. Biol. Chem. 2008;283:10550–10558. doi: 10.1074/jbc.M708833200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Bhattacharyya S, Borthakur A, Anbazhagan AN, Katyal S, Dudeja PK, Tobacman JK. Am J. Physiol Gastrointest. Liver Physiol. 2011;301:G475–86. doi: 10.1152/ajpgi.00071.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bhattacharyya S, Borthakur A, Tyagi S, Gill R, Chen ML, Dudeja PK, Tobacman JK. J. Biol. Chem. 2010;285:522–530. doi: 10.1074/jbc.M109.050815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bhattacharyya S, Dudeja PK, Tobacman JK. Biochim. Biophys. Acta. 2008;1780:973–982. doi: 10.1016/j.bbagen.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bhattacharyya S, O-Sullivan I, Katyal S, Unterman T, Tobacman JK. Diabetologia. 2012;55:194–203. doi: 10.1007/s00125-011-2333-z. [DOI] [PubMed] [Google Scholar]
- [10].Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. J. Clin. Invest. 2006;116:3015–3025. doi: 10.1172/JCI28898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Willis TG, Jadayel DM, Du MQ, Peng H, Perry AR, Abdul-Rauf M, Price H, Karran L, Majekodunmi O, Wlodarska I, Pan L, Crook T, Hamoudi R, Isaacson PG, Dyer JF. Cell. 1999;96:35–45. doi: 10.1016/s0092-8674(00)80957-5. [DOI] [PubMed] [Google Scholar]
- [12].Zhang Q, Siebert R, Yan M, Hinzmann B, Cui X, Xue L, Rakestraw KM, Naeve CW, Beckmann G, Weisenburger DD, Sanger WG, Nowotny H, Vesely M, Callet-Bauchu E, Salles G, Dixit V,M, Rosenthal A, Schlegelberger B, Morris SW. Nat. Genet. 1999;22:63–68. doi: 10.1038/8767. [DOI] [PubMed] [Google Scholar]
- [13].Bhattacharyya S, Borthakur A, Pant N, Dudeja PK, Tobacman JK. Am. J. Physiol. Gastrointest. Liver Physiol. 2007;293:G429–G437. doi: 10.1152/ajpgi.00149.2007. [DOI] [PubMed] [Google Scholar]
- [14].Wang D, You Y, Lin PC, Xue L, Morris SW, Zeng H, Wen R, Lin X. Proc. Natl. Acad. Sci. U.S.A. 2007;104:145–150. doi: 10.1073/pnas.0601894104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].McAllister-Lucas LM, Ruland J, Siu K, Jin X, Gu S, Kim DS, Kuffa P, Kohrt D, Mak TW, Nuñez G, Lucas PC. Proc. Natl. Acad. Sci. U.S.A. 2007;104:139–144. doi: 10.1073/pnas.0601947103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Klemm S, Zimmermann S, Peschel C, Mak TW, Ruland J. Proc. Natl. Acad. Sci. U.S.A. 2007;104:134–138. doi: 10.1073/pnas.0608388103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Borthakur A, Bhattacharyya S, Alrefai W, Tobacman JK, Ramaswamy K, Dudeja PK. Inflamm. Bowel Dis. 2010;16:594–603. doi: 10.1002/ibd.21092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bhattacharyya S, Borthakur A, Dudeja PK, Tobacman JK. Exp. Cell Res. 2010;316:3317–3327. doi: 10.1016/j.yexcr.2010.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Moyer MP, Manzano LA, Merriman RL, Stauffer JS, Tanzer LR, R L. Vitro Cell. Dev. Biol. Anim. 1996;32:315–317. doi: 10.1007/BF02722955. [DOI] [PubMed] [Google Scholar]
- [20].Bhattacharyya S, Pant N, Dudeja PK, Tobacman JK. J. Immunoassay Immunochem. 2007;28:173–188. doi: 10.1080/15321810701454573. [DOI] [PubMed] [Google Scholar]
- [21].Bhattacharyya S, Dudeja PK, Tobacman JK. Am. J. Phys. Gastrointest. Liver Physiol. 2007;293(2):G429–37. doi: 10.1152/ajpgi.00149.2007. [DOI] [PubMed] [Google Scholar]
- [22].Zafiropoulos A, Hatzidakis G, Mavrogiannis L, Klinakis A, Kandilogiannaki M, Krambovitis E. Biotechniques. 1997;23:1104–1109. doi: 10.2144/97236rr02. [DOI] [PubMed] [Google Scholar]
- [23].Isaacson P, Wright DH. Cancer. 1983;52:1410–1416. doi: 10.1002/1097-0142(19831015)52:8<1410::aid-cncr2820520813>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- [24].Sagaert X, Van Cutsem E, De Hertogh G, Geboes K, Tousseyn T. Nat. Rev. Gastroenterol. Hepatol. 2010;7:336–346. doi: 10.1038/nrgastro.2010.58. [DOI] [PubMed] [Google Scholar]
- [25].http://www.cancer.gov/cancertopics/factsheet/Risk/h-pylori-cancer
- [26].Bhattacharyya S, Dudeja PK, Tobacman JK. Inflamm. Bowel Dis. 2009;15:673–683. doi: 10.1002/ibd.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Yan Y, Kolachala V, Dalmasso G, Nguyen H, Laroui H, Sitaraman SV, Merlin D. PLoS One. 2009;4:e6073. doi: 10.1371/journal.pone.0006073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bhattacharyya S, Liu H, Zhang Z, Jam M, Dudeja PK, Michel G, Linhardt RJ, Tobacman JK. J. Nutr. Biochem. 2009;21:906–913. doi: 10.1016/j.jnutbio.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Macher BA, Galili U. Biochim. Biophys. Acta. 2008;1780:75–88. doi: 10.1016/j.bbagen.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].http://www.gelifesciences.com/aptrix/upp00919.nsf/Content/A7BB06EF3C4EEE8EC1257628001CEC60/$file/18115175AA.pdf
- [31].Bierhaus A, Schiekofer S, Schwaninger M, Andrassy M, Humpert PM, Chen J, Hong M, Luther T, Henle T, Klöting I, Morcos M, Hofmann M, Tritschler H, Weigle B, Kasper M, Smith M, Perry G, Schmidt AM, Stern DM, Häring HU, Schleicher E, Nawroth PP. Diabetes. 2001;50:2792–2808. doi: 10.2337/diabetes.50.12.2792. [DOI] [PubMed] [Google Scholar]
- [32].Barnes PJ, Karin M. N. Engl. J. Med. 1997;336:1066–1071. doi: 10.1056/NEJM199704103361506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. In the HT-29 cells, effects were determined at 12, 24, 36, and 48 hour time points following withdrawal of carrageenan, in contrast to no treatment control and renewed treatment every 12 hours.
A. IL-8 remained significantly elevated at 24 (p<0.001), 36 (p<0.001), and 48 (p<0.01) hours following withdrawal of the carrageenan after 12 hours of treatment, suggesting a more prolonged effect in the HT-29 cells than in the NCM460 cells.
B. The BCL10 remained significantly increased at 24 (p<0.001) and 36 (p<0.001) hours following withdrawal at 12 hours.
C. The increase in RelA remained significant at 24( p<0.001), 36 (p<0.001), and 48 (p<0.05) hours.
D. RelB was significantly increased at 24 (p<0.01) hours, following withdrawal of the carrageenan at 12 hours.
Supplementary Figure 2. In the HT-29 cells, the effects of carrageenan were contrasted with those of DSS.
A. Similar to the findings in the NCM460 cells, in the HT-29 cells the increase in IL-8 was not sustained following withdrawal of DSS.
B. The RelA declined to the control level by 24 hours in the HT-29 cells.