Abstract
This article describes initial validation of the Structured Interview for Self-Destructive Behaviors (SI-SDB), a brief interview assessing suicidality, self-injury, substance abuse, disordered eating and risky sexual behaviors. Self-destructive behaviors present clinical and practical challenges for mental health treatment providers. Participants were 217 psychiatric inpatients with a wide variety of diagnoses who completed the SI-SDB and other measures of psychiatric symptoms, trauma exposure, and other childhood experiences. Internal validity analyses revealed an internally consistent measure with two major factors. External validity analyses indicated that Substance Abuse and Disordered Eating scales were predictive of related psychiatric diagnoses. All scales except Substance Abuse were significantly correlated with psychiatric symptoms and childhood abuse. These findings indicate that the SI-SDB is a valid means to assess five significant domains of dangerous behaviors in clinical and research settings. Further research on the reliability of reports over time, interrater consistency, and convergent validity with longer measures of the SI-SDB domains are needed.
Keywords: self-destructive behaviors, interview, self-harm, suicidality, sexual impulsiveness
Self-destructive behaviors (SDBs) such as suicidality, self-injury, substance abuse, disordered eating, and risky sexual behaviors can present clinical and practical challenges for mental health providers. Assessment of past and current SDBs in an initial clinical evaluation can help clinicians formulate hypotheses about the level and dynamics of clients’ psychopathology, the functions of the behaviors, and what treatment is most likely to be effective. A brief tool that allows rapid assessment of SDBs could be valuable to clinicians. Such a measure could also be used by researchers to quickly quantify SDBs so that they can be studied.
In clinical populations, the frequency and severity of SDBs can vary greatly – ranging from occasional, mildly dangerous behaviors to frequent and extreme behaviors that disrupt functioning and put individuals at risk of injury, illness, or death. SDBs occur in the context of a wide variety of psychological disorders, and the same behavior can have a different psychological purpose or meaning. These behaviors may reflect a desire to commit suicide, to express distress or self-loathing, to obtain social support or reduce social demands, or to reduce or avoid distressing cognitions or sensations (Briere & Spinazzola, 2005; Hayes, Wilson, Gifford, Follette, & Strosahl, 1996; Nock, 2010). SDBs are elements of the DSM-IV diagnostic criteria for various disorders, including substance abuse disorders, eating disorders, and borderline personality disorder (BPD). They are also often part of the clinical presentation for complex posttraumatic stress disorder (CPTSD) (Ford & Courtois, 2009; Herman, 1997; van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005).
Although the different domains of SDBs are phenomenologically distinct, the presence of one SDB raises the likelihood of the presence of another. In a study of hospitalized forensic patients, half of the individuals who self-mutilated had also attempted suicide (Hillbrand, Krystal, Sharpe, & Foster, 1994). Similarly, those with eating disorders are at elevated risk for suicide (Pompiii, Girardi, Tatarelli, Ruberto, & Tatarelli, 2006) and self-mutilation (Favazza & Conterio, 1989). Up to half of those with eating disorders abuse drugs and/or alcohol, and up to 35% of alcohol/drug abusers have eating disorders (National Center on Addictions and Substance Abuse at Columbia University, 2001). The relationship between alcoholism and suicidality is also well-established. One study of suicide rates in those with alcohol dependence found it to be six times that of the general population. (Cherpital, Borges, & Wilcox, 2004; Harris & Barraclough, 1997). In general, the presence of any SDBs increases the probability and need for assessment of all SDBs.
Explanations of the frequent co-occurrence of these behaviors have included that SDBs share common neurochemical (Straus, 1979) or psychosocial causes (Zlotnick, 1997). SDBs may reflect attempts at behavioral and emotional regulation (Lieb, Zanarini, Schmahl, Linehan, & Bohus, 2004). Genetic tendencies, early childhood experiences, and trauma exposure likely interact to cause intense and difficult to manage emotions, and individuals engage in SDBs in response to the strong emotions or in attempts to relieve their distress. In a study of individuals who engaged in self-mutilating behaviors, the primary reported reasons for the behaviors were to reduce dissociative symptoms of derealization and numbing, reduce stress and tension, and to block upsetting memories and reexperiencing (Briere & Gil, 1996). Thirty percent or more reported emotional states before the behavior of anger at others, hurt, emptiness, fear, anger at self, loneliness, and/or sadness, and 68% reported feeling relief after the behavior.
Several existing measures assess self-injury and suicidal thoughts and behaviors (Briere, 1995; Firestone & Firestone, 1996; Jobes, 2006; Linehan, Comtois, Brown, Heard, & Wagner, 2006; Nock, Holmberg, Photos, & Michel, 2007), intentional self-harming behaviors (Gratz, 2001; Sansone, Wiederman, & Sansone, 1998), disordered eating (Garner, Olmstead, & Polivy, 1983; Hill, Reid, Morgan, & Lacey, 2009), and problematic sexual behaviors (Kalichman et al., 1994; Miner, Coleman, Center, Ross, & Simon Rosser, 2007), and numerous measures assess substance abuse and dependence. None of these measures, however, assess the full range of dangerous behaviors that may be clinically important, and administering all would be prohibitively time-consuming in most clinical settings.
The Self-Harm Inventory (SHI) (Gratz, 2001; Sansone et al., 1998) is a brief self-report measure that is a count of endorsement of 22 intentional self-destructive behaviors that were significantly correlated with scores on a diagnostic interview for Borderline Personality Disorder. While the items on the SHI cover the full content domain of SDBs, endorsement of dichotomous items yields a count of different behaviors, rather than an index of the severity of types of dangerous behaviors. In addition, SHI items emphasize that the behaviors are intentional. Because those engaging in self-destructive behaviors often do not experience them as intentional, inquiring about behaviors independently of intentionality seems preferable.
Assessing a range of SDBs in one measure has several advantages. First, it is simpler and less time-consuming to administer and score one measure. In many clinical settings, time constraints do not allow use of several longer measures. The availability of a single, brief measure to collect data on SDBs would make it possible to include this variable in more studies and reduce the burden of research participation. Secondly, assessing all these behaviors collectively will facilitate quantification of an individual’s total level of these dangerous behaviors. Similarly, if different dangerous behaviors are functionally equivalent, assessing the total level of dangerous behavior may be the most effective way to study them. The total amount of these behaviors may relate significantly to other variables, while the levels of individual behaviors do not.
An interview format was selected for multiple reasons. First, interview screening questions allow the clinician to skip or speed through sections of the interview that are not relevant to the respondent. An interviewer can determine the global severity of each type of behavior much more quickly than an individual can complete a detailed self-report measure. In addition, given the seriousness of certain behaviors such as suicidality, the interview format is ideal for immediate clinical response to such thoughts or behaviors. Clinicians can also gather additional information about clients during the interview through observation of specific verbal content of responses, affect associated with content reports, and nonverbal behaviors. This may be especially helpful in assessing minimization or dangerous behaviors that are not experienced by the individual as intentional. Finally, the use of an interview allows for clinicians and patients to begin to develop rapport, which is especially important when assessing SDBs, because clients may be reluctant to report them due to shame, anxiety, or other factors.
In the context of a study of multivariate prediction of posttraumatic symptoms in psychiatric inpatients (Carlson et al., 2001), we collected data that allows us to examine the internal and external validity of the Structured Interview for Self-Destructive Behaviors (SI-SDB), including concurrent, convergent, and discriminant validity. Specifically, we examined internal validity through descriptive statistics, domain intercorrelations, and structural analyses. To evaluate the external validity of the SI-SDB, we investigated concurrent validity by examining associations between scores for two domains of SDBs and related psychiatric diagnoses. Convergent and discriminant validity was also investigated by examining correlations between the scores on the domains of SDBs and measures of theoretically-related and unrelated psychological symptoms.
Methods
Procedure
The study was approved by ethics review boards of the institution where participants were hospitalized and the first author’s institution at the time of the research. Over a 3.5 year period, we contacted inpatient clinicians responsible for the care of any admitted patient between the ages of 30 and 45 and received permission to contact 87% of them. Of 591 patients who were available and invited to participate, 217 took part in the study, 180 declined participation, and 194 were discharged before taking part in or completing the study. After complete description of the study to the subjects, written informed consent was obtained for all participants. Patients first completed self-report measures and were then interviewed in private by trained clinical psychology graduate students. A timeline of major life events was constructed and used to improve the accuracy of patient retrospective recall. Additional detail on the methods used to collect the data reported here are provided in Carlson et al. (2001).
Participants
Participants were 217 psychiatric inpatients between the ages of 30 and 45 who were recently admitted to a large private, nonprofit psychiatric hospital serving both urban and suburban areas. The sample included 92 males and 125 females with an average age of 38. Participants were predominantly Caucasian (81%) and African American (16%). The marital status of the sample included 37% married, 33% single, 17% divorced, 12% separated and 1% widowed. Average socioeconomic status (SES), as measured by the Hollingshead Index (Hollingshead & Redlich, 1958), was 40 (SD = 17.6; range = 11 to 77), which falls in the middle class. Up to three psychiatric diagnoses per participant were obtained from patient medical records. At least one diagnosis was available for 90% (n = 195). Of those for whom diagnostic information was available, 68% had at least two diagnoses, and 11% had three. The majority (61%), were diagnosed with at least one mood disorder including 36% with major depressive disorder, 16% with bipolar disorder, and 11% with some other mood disorder. Other frequent disorders included substance use disorders (30%) and dissociative disorders (30%), and PTSD (26%). The high rate of the two latter diagnoses was due to a specialty treatment unit for trauma and dissociative disorders. Additional diagnoses included schizophrenia or other psychotic disorder (7%), eating disorder (4%), borderline personality disorder (3%), and an anxiety disorder other than PTSD (2%).
Measures
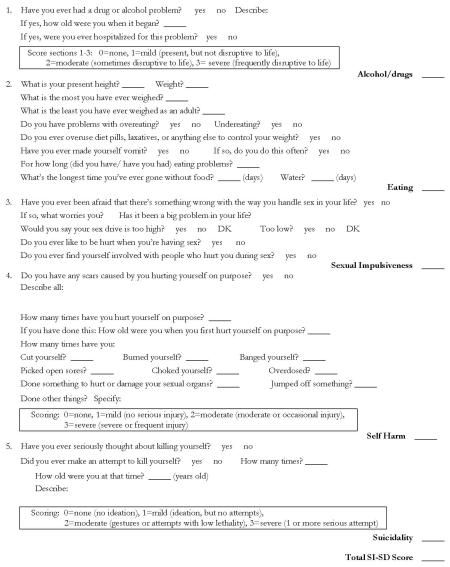
Structured Interview of Self-Destructive Behaviors (SI-SDB)
The SI-SDB consists of five sections in the domains of substance abuse, disordered eating, disordered sexual behavior, self-injury, and suicidality (see Appendix). In each section, a series of questions is asked to flesh out the domain and allow the interviewer to rate the severity of the problem. Items were designed to inquire about behaviors and injuries in a neutral way and do not assume intentionality, with the exception self-harm and suicidal behaviors. We elected not to investigate unintentional self-harming behaviors by asking about all injuries, to avoid lengthening the interview for most individuals. Rating levels are defined and anchored in terms of functioning, with 0 = none; 1 = mild = present, but not disruptive to life; 2 = moderate = sometimes disruptive to life; and 3 = severe = frequently disruptive to life. Ratings are assigned for lifetime level of each behavior and the domains can also be rated for current levels of behaviors. Total scores are the sum of domain scores and range from 0 to 15. The time required to conduct the interview varies depending on the extent of the behaviors endorsed. We estimate the interview will take from five to 12 minutes in research use and five to 20 minutes in clinical use.
Psychiatric Symptoms
Current psychiatric symptoms were assessed with the Symptom Checklist-90 – Revised (SCL-90-R), a well-validated, 90-item self-report questionnaire that measures overall distress (Global Severity Index) and psychiatric symptoms in nine domains (Depression, Interpersonal Sensitivity, Somatization, Anxiety, Hostility, OCD, Phobic Anxiety, Paranoid Ideation, and Psychoticism) (Derogatis, 1983). Response options range from 0 (not at all distressed by a symptom) to 4(extremely distressed by a symptom), and scale scores are the average of item scores.
PTSD symptoms were assessed using the Structured Interview for PTSD (SI-PTSD) (Davidson, Smith, & Kudler, 1989) when a positive response was given to the gate question about an extremely stressful event such as serious physical injury, combat, rape, assault, captivity, being kidnapped, being burned, seeing loss of life, one’s own life being threatened, destruction of property, or threat or harm to one’s family. Interviewers rate the severity of the 17 symptoms of PTSD in the DSM-IV on a scale of (absent or not affected) to 4 (very severe or strongly affected by a problem). The SI-PTSD has demonstrated good interrater and test-retest reliability and concurrent validity (Davidson, Kudler, & Smith, 1990; Davidson et al., 1989). The Screen for Posttraumatic Stress Symptoms (SPTSS) was added to the study mid-way to provide a means of quantifying PTSD symptoms in all participants, regardless of trauma exposure. The SPTSS is a 17-item, self-report questionnaire assessing the frequency of symptoms of PTSD that does not key symptoms to a single, specific traumatic stressor and has demonstrated good internal and concurrent validity (Carlson et al., 2001; Caspi, Carlson, & Klein, 2007). SPTSS items are rated on a 0 (never) to 10 (always) scale in reference to the past two weeks. Total scores are the mean of item scores.
Dissociative symptoms were assessed with the Dissociative Experiences Scale, a 28-item self-report questionnaire that assesses depersonalization, derealization, lack of recall, absorption, and imaginative involvement (Bernstein & Putnam, 1986; Briere). For each item, participants circle a multiple of 10 to indicate the percentage of time they have the experience (0%, 10%, 20% ... 100%). The total score is the average of all item scores. The DES has been used extensively and validated in a range of psychiatric and general population samples (Carlson, Dalenberg, & McDade-Montez, 2012; Carlson & Putnam, 1993).
Trauma Exposure
Childhood sexual and physical abuse were assessed with a modified versions of Jacobson’s structured interviews for interpersonal violence and nonconsensual sexual experiences (Jacobson & Richardson, 1987) that was based on the Conflict Tactics Scale (Straus, 1979). For physical abuse, participants were assessed for up to four possible abusers about being hit with an object, being kicked, bitten or hit with a fist, being burned, being beaten or being threatened with a gun or knife, having someone throw, smash or kick something; having someone threaten to hit you, or throw something at you; and being pushed, grabbed shoved, slapped or spanked hard. For sexual abuse, participants were assessed for attempted or completed oral, vaginal or anal penetration, unwanted kissing, hugging, or touching of body or sexual organs; or being made to touch someone’s sexual organs. Scores on these variables represent the number of experiences of these types of abuse, rather than specific occasions of abuse, so that multiple types of abuse on one occasion are counted. Additional description of the interview and evidence to support its reliability and are reported elsewhere (Carlson et al., 2001). Adult trauma frequency was assessed using the gate question to the SI-PTSD. Those responding positively were asked to describe the events. and coded into 5 categories of 0 traumas, 1 trauma, 2 or 3 traumas, 4 or 5 traumas, and 6 or more traumas.
Psychosocial Variables
Caretaker dysfunction was measured through a structured interview designed for this study that inquired about whether up to five primary caretakers 1) had difficulties with substance abuse, 2) had other mental health problems, 3) attempted suicide or 4) was violent toward others in the household. Each was scored 0 (no) or 1 (yes) for each caretaker, and the total score was the average score across caretakers. Neglect was measured with a series of items designed for this study that included getting sick because of neglect, being sick and having no one care for you, going without food or water for a day or more, living away from home for more than three months, and living in foster care. Neglect scores were the number of these experiences endorsed. Perceived social support as a child was measured with a structured interview designed for this study assessing self-esteem support, informational support, instrumental support, motivational support and listening support (e.g., “Was there anyone who would give you advice or would give you suggestions that helped you?”). Participants indicated when, who, and how much this helped. The extent this person helped was rated 0 (not at all), 1 (a little), 2 (somewhat), or 3 (very much), and total scores were the average of item scores.
Results
SI-SDB data were available for 207 of 217 participants as 10 participants chose to discontinue the interview or were unable to complete all measures of the study before being discharged. Unless otherwise noted, n = 207 for all analyses reported.
Internal/Structural Validity
SI-SDB Descriptive Statistics
Table 1 shows the means of the SI-SDB scales for men, women, and the total sample and results of t-tests comparing means across sex. All means were significantly different between men and women. Table 1 also shows the proportion of participants who endorsed a moderate or severe level for each of the five SI-SDB scales.
Table 1.
Descriptive Statistics of SI-SDB
| Overall |
Means (SD) Men |
Women | t | Range | Proportion Endorsing High Level |
|
|---|---|---|---|---|---|---|
| SI-SDB Scale | ||||||
| Substance Abuse | 1.68 (1.35) | 2.31 (119) | 1.20 (1.27) | 6.41*** | 0-3 | 57% |
| Disordered Eating | 1.36 (108) | .96 (0.99) | 1.68 (106) | 4.98*** | 0-3 | 44% |
| Sexual Impulsiveness | .68 (100) | .51 (0.89) | .82 (107) | 2.22* | 0-3 | 22% |
| Self-Harm | 1.51 (1.27) | 1.16 (124) | 1.79 (122) | 3.66*** | 0-3 | 53% |
| Suicidality | 1.95 (1.17) | 1.59 (125) | 2.22 (103) | 3.97*** | 0-3 | 64% |
| Total | 7.17 (3.54) | 6.52 (3.44) | 7.69 (3.54) | 2.39* | 0-15 | |
Note. N = 117 women, 90 men. SI-SDB domains were rated on a scale of 0 (none) to 3 (severe, frequently disruptive problems). Male and female means compared with independent groups t-test, df = 205
= t significant at p ≤ .05
= t significant at p ≤ .001.
SI-SDB Domain Correlations
Table 2 shows correlations among the scales of the SI-SDB and with total score (not including the scale score). The domain scores were significantly correlated with one another with the exceptions that Sexual Impulsiveness was not significantly related to Suicidality and Substance Abuse was not significantly related to any other scale.
Table 2. Correlations among SI-SDB Scales.
| Scale | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Substance Abuse | — | ||||
| 2. Disordered Eating | −.05 | — | |||
| 3. Sexual Impulsiveness | .11 | .28*** | — | ||
| 4. Self-Harm | .01 | .40*** | 19** | — | |
| 5. Suicidality | .00 | .32*** | .13 | .68*** | — |
| 6. Total Score | .02 | .37*** | .27*** | 54*** | .47*** |
Note.
= p ≤ .01, two-tailed
= p ≤ .001, two-tailed.
SI-SDB Structural Analyses
To further examine the structure of the SI-SDB, principal components analyses with varimax rotation were conducted. Based on examination of the factor loadings for each scale and scree plots in one- and two-factor solutions, it was determined that a two-factor solution best described the data. Self-Harm, Suicidality, and Disordered Eating loaded on the first component (.87, .84 and .66 respectively) and Substance Abuse and Sexual Impulsiveness loaded on the second component (.81 and .66 respectively). All other loadings were below .4. The solution accounted for 62.6 percent of the variance.
External Validity
Criterion validity for each scale was examined through associations between the SI-SDB domains of Substance Abuse and Disordered Eating and the relevant diagnostic category. Table 3 shows results of logistic regressions calculating the probability of specific diagnoses based on SI-SDB scores. Convergent and discriminant validity were examined by correlating the SI-SDB total and domain scores with childhood physical abuse, childhood sexual abuse, caretaker dysfunction, neglect, childhood social support, adult trauma exposure, and psychiatric symptoms. Results are shown in Table 4. Substance Abuse scores were not significantly correlated with any variable. Sexual Impulsivity correlated most strongly with childhood sexual abuse (r = .25, p < .01). Disordered Eating, Self-Harm, and Suicidality scores were significantly correlated with all experience and symptom variables, with the exception of adult trauma exposure.
Table 3.
Logistic Regression Analyses Predicting Diagnosis from SI-SDB Scales
| SI-SDB Scale | B | SE | Wald | Odds Ratio | 95% CI |
|---|---|---|---|---|---|
| Substance Abuse | |||||
| Substance Use Disorder (n=58) | 1.46 | .26 | 30.56*** | 4.31 | 2.57-7.23 |
| Disordered Eating | |||||
| Any Eating Disorder (n=8) | 2.52 | .98 | 6.61* | 12.49 | 1.82-85.58 |
| Any Dissociative Disorder (n=57) | .68 | .16 | 16.61*** | 1.97 | 1.45-2.67 |
| Self-Harm | |||||
| Any Anxiety Disorder (n=49) | .73 | .16 | 21.07*** | 2.07 | 1.52-2.83 |
|
Any Dissociative Disorder or
Borderline Personality Disorder (n=62) |
.68 | .14 | 23.26*** | 1.99 | 1.50-2.59 |
Note. Diagnoses entered into analyses included any mood, anxiety, dissociative, substance use, psychotic, or eating disorders, borderline personality disorder, and “other” for any additional diagnoses; all significant associations are listed.
= p < .05
= p < .001.
Table 4.
External Validity Correlations
| SI-SDB Scale: | Total | Sub. Abu. | Dis. Eating | Sexual Imp. | Self-Harm | Suic. |
|---|---|---|---|---|---|---|
| Child Phys. Abuse1 | 28*** | .04 | .18** | .13 | .26*** | 25*** |
| Child Sex. Abuse1 | 42*** | −.13 | 42*** | .25** | 44*** | .34*** |
| Caretaker Dys. | 25*** | −.03 | 19** | .13 | .26*** | .22** |
| Neglect | .13 | −.05 | .15* | .13 | .12 | .09 |
| Child Soc. Supp. | − 28*** | .07 | −.21** | −.12 | −.34*** | −25*** |
| Adult Trauma | .07 | .08 | .03 | .00 | .07 | .02 |
| SCL-90-R Scale: | ||||||
| Depression | .39*** | −.02 | .30*** | .16* | .39*** | .36*** |
| Interpersonal Sens. | .34*** | −.08 | .30*** | .18** | .36*** | .30*** |
| Somatization | .27*** | .11 | .21** | .14* | .17* | .17* |
| Anxiety | 44*** | .02 | .29*** | .17* | 44*** | .39*** |
| Hostility | .37*** | .13 | 24*** | .08 | .18* | .17* |
| OCD | .33*** | .04 | .27*** | .12 | .29*** | .28*** |
| Phobic Anxiety | .39*** | .03 | 35*** | .12 | .36*** | 31*** |
| Paranoid Ideation | .29*** | .08 | .23*** | .15* | 19** | .22** |
| Psychoticism | .34*** | .06 | .26*** | .16* | .29*** | .27*** |
| GSI | .43*** | .05 | .33*** | .18** | .38*** | .35*** |
| Past PTSD interview | .48*** | −.12 | .35*** | .19* | 53*** | .50*** |
| Present PTSD intrvw. | 42*** | −.12 | .30*** | .15 | .49*** | .46*** |
| Self-Reported PTSD | .41*** | .02 | .21* | .14 | 42*** | .43*** |
| Dissociation | .40*** | .01 | 31*** | .16* | .40*** | .33*** |
= Given the skewness and kurtosis of responses to these items, common logarithm transformations were conducted to create normal distributions for both the physical and sexual abuse scores.
indicates significant at p ≤ .05
= p ≤ .01
= p ≤ .001, two-tailed.
“Past PTSD interview” and “Present PTSD intrvw.” are both rated from the SI-PTSD; “Self-Reported PTSD” is the SPTSS. For correlations with SPTSS, n = 136 patients. “Dissociation” is measured with the DES. Correlations in bold are the highest for each SI-SDB scale.
DISCUSSION
The goal of the current study was the development and initial validation of a brief interview assessing five domains of SDBs. Given the clinical significance of substance abuse, disordered eating, sexual impulsivity, self-harm and suicidality, we sought to create a simple interview to quickly assess for these behaviors in clinical and research settings.
Descriptive results indicated a range of endorsement for each of the five behaviors as well as significant gender differences. Men were more likely to endorse Substance Abuse whereas women were more likely to endorse Disordered Eating, Sexual Impulsivity, Self-Harm, and Suicidality. Structural analyses indicated that the interview had a two-factor structure, with Suicidality, Self-Harm, and Disordered Eating loading on the first factor and Substance Abuse and Sexual Impulsivity loading on the second factor.
Criterion validity analyses indicated that the probability of receiving a SUD diagnosis was significantly higher for those with high scores on the Substance Abuse scale (OR = 4.31, p < .001), the probability of receiving an eating disorder diagnosis was significantly higher for those with high scores on the Disordered Eating scale score, and the probability of receiving a diagnosis of an anxiety disorder, a dissociative disorder, or borderline personality disorder was significantly higher for those with high scores on the Self-Harm scale.
Other analyses indicated that all SI-SDB scales except Substance Abuse were significantly correlated with childhood sexual abuse exposure. Disordered Eating, Self-Harm and Suicidality were all significantly associated with childhood physical abuse exposure, caretaker dysfunction, neglect, and lower social support as a child. These findings are particularly significant as they support the theoretical connection between these behaviors and trauma experiences. Significant associations were not observed between adult trauma and SI-SDB scales, which is also consistent with the theoretical formulations that SDBs are most strongly related to severe trauma exposure during childhood (Ford & Courtois, 2009; Herman, 1997; van der Kolk et al., 2005).
In examining convergent and discriminant validity, all SI-SDB scales, with the exception of Substance Abuse, demonstrated significant correlations with the psychiatric symptom variables. The highest correlations were generally with PTSD and dissociation. Moderately high correlations were also observed between the total SI-SDB scale and the Anxiety, Global Symptom Index, Phobic Anxiety, Depression and Hostility scales of the SCL-90-R. The general pattern of correlations indicates that total SI-SDB scores were more strongly related to trauma and psychiatric variables than individual scale scores. SI-SDB subscale scores showed patterns of correlations with SCL-90 scales that were consistent with expectations. Disordered Eating was most strongly associated with Phobic Anxiety and past PTSD. Sexual Impulsivity was most strongly associated with past PTSD, Global Symptom Index, and Interpersonal Sensitivity (which largely assesses self-esteem). Self-Harm and Suicidality were most strongly associated with past and present PTSD, dissociation, Depression, Anxiety, Global Symptom Index, and Interpersonal Sensitivity. Lower and nonsignificant correlations between the Substance Abuse scale scores and other variables may be the result of inadequate quantification of substance abuse or underreporting about substance abuse or they may indicate that substance abuse is not strongly influenced by trauma exposure and childhood experiences.
The gender differences identified in this study are consistent with certain patterns of psychopathology as noted in the DSM-IV, where substance use disorders are generally seen at higher rates among males and mood disorders are generally more common among females. It would appear that gender differences found on the SI-SDB scale means contributed to the two-factor structure found, but in his review of 36 personality and psychopathology measures in clinical and nonclinical samples, O’Connor (2002) found consistency in the number and nature of factors despite mean level differences in responses between groups.
Limitations and Needed Research
A limitation of the SI-SDB is that it does not assess self-harm and suicidal behaviors that patients perceive as unintentional. This is a difficult set of behaviors to assess because distinctions between intentional and accidental behaviors may be difficult to draw for patients and for clinicians. Further study of how self-harm and suicidal behaviors that patients perceive as unintentional could be valuable.
In addition, in future studies, SI-SDB results should be compared to results on detailed, specific measures for the five types of SDBs. Such research in inpatient and outpatient samples would provide valuable information about the validity of the SI-SDB. Research on the reliability of the SI-SDB is also needed to confirm the stability of reports over time and consistency of ratings across interviewers. In addition, measurement of SDBs in general population samples should be conducted to further validate the measure and generate norms for the SI-SDB.
CONCLUSIONS
The SI-SDB is a brief, easy-to-use interview assessing five clinically significant, dangerous behaviors. Internal validity analyses indicate that the interview measures distinct yet related behaviors. External validity analyses indicate that the SI-SDB scales are significantly related to psychiatric diagnoses, psychiatric symptoms, trauma exposure, and other childhood experiences such as sexual and physical abuse, caretaker dysfunction, and social support. Overall, the SI-SDB appears to validly assess SDBs, although results on the Substance Abuse scale should be interpreted with caution until further validation is available. Additional research is needed to establish the reliability, validity, and norms for the measure.
Acknowledgments
This work was supported by funding from NIMH (R29 MH49401) to Eve Carlson. The authors acknowledge and thank Steven Sharfstein, MD, President and CEO, David Roth, Ph.D., and the staff and patients of Sheppard Pratt Health System for their support and willingness to participate in this research.
Appendix
References
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. Journal of Nervous and Mental Disease. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Inventory professional manual. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Briere J, Gil E. Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. American Journal of Orthopsychiatry. 1996;68:609–620. doi: 10.1037/h0080369. [DOI] [PubMed] [Google Scholar]
- Briere J, Spinazzola J. Phenomenology and psychological assessment of complex posttraumatic states. Journal of Traumatic Stress. 2005;18(5):401–412. doi: 10.1002/jts.20048. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Dalenberg C, Armstrong J, Walker Daniels J, Loewenstein R, Roth D. Multivariate prediction of posttraumatic symptoms in psychiatric inpatients. Journal of Traumatic Stress. 2001;14(3):549–567. doi: 10.1023/A:1011164707774. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Dalenberg CJ, McDade-Montez E. Dissociation in Posttraumatic Stress Disorder Part I: Definitions and review of research. Psychological Trauma. 2012;4:479–489. [Google Scholar]
- Carlson EB, Putnam FW. An update on the Dissociative Experiences Scale. Dissociation. 1993;6:16–27. [Google Scholar]
- Caspi Y, Carlson EB, Klein E. Validation of a screening instrument for posttraumatic stress disorder in a community sample of Bedouin men serving in the Israeli Defense Forces. Journal of Traumatic Stress. 2007;20(4):517–527. doi: 10.1002/jts.20237. [DOI] [PubMed] [Google Scholar]
- Cherpital D, Borges L, Wilcox H. Acute alcohol use and suicidal behavior: a review of the literature. Alcohol Clinical Experimental Research. 2004;28:18s–28s. doi: 10.1097/01.alc.0000127411.61634.14. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Kudler HS, Smith RD. Assessment and pharmacotherapy of posttraumatic stress disorder. In: Giller JEL, editor. Biological assessment and treatment of posttraumatic stress disorder. American Psychiatric Press; Washington D.C.: 1990. pp. 205–221. [Google Scholar]
- Davidson JRT, Smith RD, Kudler HS. Validity and reliability of the DSM-III criteria for posttraumatic stress disorder: Experience with a structured interview. Journal of Nervous and Mental Disease. 1989;177:336–341. doi: 10.1097/00005053-198906000-00003. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, socring and procedures manual-II. Clinical Psychometric Research; Towson, MD: 1983. [Google Scholar]
- Favazza A, Conterio R. Female habitual self-mutilators. Acta Psychiatrica Scandinavica. 1989;79:283–289. doi: 10.1111/j.1600-0447.1989.tb10259.x. [DOI] [PubMed] [Google Scholar]
- Firestone RW, Firestone LA. Firestone Assessment of Self-Destructive Thoughts. Psychological Corporation; San Antonio: 1996. [Google Scholar]
- Ford JD, Courtois CA. Defining and understanding complex trauma and complex traumatic stress disorders. In: Courtois CAF, Julian D, editors. Treating Complex Traumatic Stress Disorders: An evidence-based guide. Guilford Press; New York, NY: 2009. pp. 13–30. [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2(2):15–34. [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23(4):253–263. [Google Scholar]
- Harris E, Barraclough B. Suicide as an outcome for mental disorders: a meta-analysis. British Journal of Medical Psychology. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl KD. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64(6):1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Herman JL. Trauma and Recovery. Basic Books; New York, NY: 1997. [Google Scholar]
- Hill LS, Reid F, Morgan JF, Lacey JH. SCOFF, the development of an eating disorder screening questionnaire. International Journal of Eating Disorders. 2009 doi: 10.1002/eat.20679. [DOI] [PubMed] [Google Scholar]
- Hillbrand M, Krystal J, Sharpe K, Foster H. Clinical predictors of self-mutilation in hospitalized forensic patients. Journal of Nervous and Mental Disease. 1994;182:9–13. doi: 10.1097/00005053-199401000-00003. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB, Redlich FC. Social Class and Mental Illness. John Wiley & Sons, Inc.; New York: 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson AJ, Richardson B. Assault experiences of 100 psychiatric inpatients: Evidence of the need for routine inquirty. American Journal of Psychiatry. 1987;14:908–913. doi: 10.1176/ajp.144.7.908. [DOI] [PubMed] [Google Scholar]
- Jobes D, editor. Managing suicidal behavior: A collaborative approach. Guilford Press; New York: 2006. [Google Scholar]
- Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. Journal of Personality Assessment. 1994;62:385–397. doi: 10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. The Lancet. 2004;364:453–461. doi: 10.1016/S0140-6736(04)16770-6. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Comtois KA, Brown MZ, Heard HL, Wagner A. Suicide Attempt Sef-Injury Interview (SASII): Development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychological Assessment. 2006;18(3):303–312. doi: 10.1037/1040-3590.18.3.303. [DOI] [PubMed] [Google Scholar]
- Miner MH, Coleman E, Center BA, Ross M, Simon Rosser BR. The Compulsive Sexual Behavior Inventory: Psychometric properties. Archives of Sexual Behavior. 2007;36:579–587. doi: 10.1007/s10508-006-9127-2. [DOI] [PubMed] [Google Scholar]
- National Center on Addictions and Substance Abuse at Columbia University . Food for thought: Substance abuse and eating disorders. Columbia University; 2001. [Google Scholar]
- Nock MK. Self-injury. Annual Review of Clinical Psychology. 2010;6:339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD. Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment. 2007;19(3):309–317. doi: 10.1037/1040-3590.19.3.309. [DOI] [PubMed] [Google Scholar]
- O’Connor BJ. The search for dimensional structure differences between normality and abnormality: A statistical review of published data on personality and psychopathology. Journal of Personality and Social Psychology. 2002;83(4):962–982. [PubMed] [Google Scholar]
- Pompiii M, Girardi P, Tatarelli G, Ruberto A, Tatarelli R. Suicide and attempted suicide in eating disorders, obesity and weight-image concern. Eating Behavior. 2006;7:384–394. doi: 10.1016/j.eatbeh.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Sansone RA, Wiederman MW, Sansone LA. The Self-Harm Inventory (SHI): Development of a scale for identifying self-destructive behaviors and borderline personality disorder. Journal of Clinical Psychology. 1998;54(7):973–983. doi: 10.1002/(sici)1097-4679(199811)54:7<973::aid-jclp11>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- van der Kolk BA, Roth S, Pelcovitz D, Sunday S, Spinazzola J. Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress. 2005;18(5):389–399. doi: 10.1002/jts.20047. [DOI] [PubMed] [Google Scholar]
- Zlotnick C. Posttraumatic stress disorder (PTSD), PTSD comorbidity, and childhood abuse among incarcerated women. Journal of Nervous and Mental Disease. 1997;185(12):761–763. doi: 10.1097/00005053-199712000-00007. [DOI] [PubMed] [Google Scholar]