Abstract
Background
Algorithms combining both clinical and genetic data have been developed to improve oral anticoagulant therapy. Three polymorphisms in two genes, VKORC1 and CYP2C9, are the main coumarin dose determinants and no additional polymorphisms of any relevant pharmacogenetic importance have been identified.
Objectives
To identify new genetic variations in VKORC1 with relevance for oral anticoagulant therapy.
Methods and Results
3949 consecutive patients taking acenocoumarol were genotyped for the VKORC1 rs9923231 and CY2C9* polymorphisms. Of these, 145 patients with a dose outside the expected range for the genetic profile determined by these polymorphisms were selected. Clinical factors explained the phenotype in 88 patients. In the remaining 57 patients, all with higher doses than expected, we sequenced the VKORC1 gene and genetic changes were identified in 14 patients. Four patients carried VKORC1 variants previously related to high coumarin doses (L128R, N = 1 and D36Y, N = 3).Three polymorphisms were also detected: rs17878544 (N = 5), rs55894764 (N = 4) and rs7200749 (N = 2) which was in linkage disequilibrium with rs17878544. Finally, 2 patients had lost the rs9923231/rs9934438 linkage. The prevalence of these variations was higher in these patients than in the whole sample. Multivariate linear regression analysis revealed that only D36Y and rs55894764 variants significantly affect the dose, although the improvement in the prediction model is small (from 39% to 40%).
Conclusion
Our strategy identified novel associations of VKORC1 variants with higher acenocoumarol doses albeit with a low effect size. Further studies are necessary to test their influence on the VKORC1 function and the cost/benefit of their inclusion in pharmacogenetic algorithms.
Introduction
The prevention of stroke, deep vein thrombosis, pulmonary embolism or deleterious coronary malfunctions by means of coumarins is one of the most frequently used clinical practices in the world. However, the inherent risk of serious side effects and the wide inter-patient variation in therapeutic dose [1] have highlighted the need to better predict the most suitable dose before starting treatment [2]. The huge variability in the required dose of coumarins to achieve a narrow therapeutic index has been attributed to both clinical factors (mainly age, gender and body mass index) and DNA variants in enzymes, whose activities impact the pharmacokinetic and/or pharmacodynamic of coumarins [3].
In this framework several genome-wide association studies (GWAS) have recently been conducted to detect DNA variants which influence warfarin dosing [4]–[6]. The results of these GWAS have provided a sufficient basis to consider three genetic factors as the strongest markers of coumarin pharmacogenetics: common polymorphisms (SNPs) in VKORC1, the target of the drugs, explain up to ∼30% of variance in coumarin dose, while two SNPs in CYP2C9 (the main metabolizer complex) predict ∼10%. With less impact, rs2108622 in CYP4F2 determines approximately 1.5% of variance in the coumarin dose and non-genetic factors jointly account for another ∼15% [7].
In an attempt to personalize warfarin doses several models have been developed by incorporating both sets of factors into algorithms that explain as much as 50% of dose variability in Caucasians [7], [8]. Such a percentage has been robustly and widely replicated in several studies, making this area one of the most successful applications of pharmacogenetics to date [9], [10], which is why the US FDA updated the warfarin label in 2007 by including genetic data [11]. However, the issue is still conflictive as the American College of Chest Physicians in the last evidence-based clinical practice guideline about antithrombotic therapy and the prevention of thrombosis does not recommend the routine use of pharmacogenetic testing for guiding doses of coumarins in patients initiating anti-vitamin K therapy (Grade 1B) [12].
Regarding other coumarins used in Europe, e.g. phenprocoumon and acenocoumarol, the main dose determinants are quite similar to warfarin [13], [14] and dosing algorithms have also been developed for them [15], [16]. The application of these models should confirm or not whether the genetic forecasting is of use not only clinically but also economically.
Unfortunately, a still undetermined proportion of patients escape genetic forecasting due to unknown factors, genetic mutations in VKORC1 and/or CYP2C9, or interactions with drugs, food and/or herbs [7]. Accordingly, efforts are also ongoing to identify the additional genetic and clinical factors that would decide the individual coumarin dose necessary. In this work we aim to identify hidden genetic factors involved in deviations from theoretical forecasts as defined by the three most decisive factors, VKORC1 and CYP2C9 genotypes.
Materials and Methods
Patients
A retrospective study recruited 3949 consecutive Caucasian patients taking acenocoumarol from the Antithrombotic Therapy Unit of the Morales Meseguer University Hospital (Murcia, Spain). Patients were eligible to take part in the study if aged 18 years or over and were steadily anticoagulated. A stable period was defined as a period of at least 3 weeks with three or more consecutive INR measurements with <10% change within the target range in the acenocoumarol dose. Exclusion criteria were a diagnosis of cancer, alcohol or drug abuse, acenocoumarol allergy/intolerance, terminal disease,known or suspected pregnancy and intake of amiodarone, antifungal drugs, anti-platelet drugs and/or statins.
Clinical and demographical data were obtained from the medical records and the database: 1947 males (49%); median age, 74±10 years; median body mass index (BMI), 29.5±7.4. Most patients (90%) were anticoagulated with an INR target range of 2.0–3.0 and 10% of them had an INR target range of 2.5–3.5.
All subjects gave their informed consent according to the Helsinki Declaration, and the study was approved by the Ethical Committee of the Morales Meseguer Hospital.
Study Design
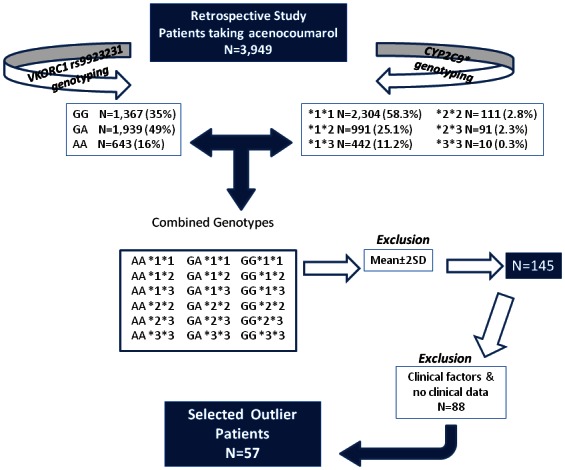
The study design and eligibility are recorded in Figure 1. The three main genetic determinants of acenocoumarol dose (−1639G>A VKORC1 and the two CYP2C9 * SNPs) were applied to define 18 genetic profiles for the whole studied population (N = 3949) (Figure 1). For each profile, we identified the average dose. Patients with dose requirements outside the mean±2SD value according to their genetic profile were identified as ¨outlier ¨ patients. Patients with clinical factors that explained the abnormal dose requirements, as well as those patients with no available clinical data were excluded. In the remaining patients the promoter and coding regions of VKORC1 were sequenced.
Figure 1. Study design: selection of patients from a retrospective cohort of subjects anticogulated with acenocoumarol (N = 3949).
Genotyping
VKORC1 SNPs rs9923231 (−1639 G>A), rs17878544 (both in the promoter) and rs7200749 (L120L), were determined by Taqman analysis using Taqman SNP Genotyping Assays C_30403261_20, C_60247472_10 and C_29057362_10, respectively (Applied Biosystems). VKORC1 rs9934438 (1173C>T located in intron 1) was determined using FRET probes. VKORC1 rs55894764 (R12R) and the D36Y mutation were genotyped by PCR-allelic specific restriction assay using HinfI (Promega) and RsaI (Promega), respectively. CYP2C9*2 (rs1799853) and *3 (rs1057910) genotypes were determined by the Taqman Drug Metabolism Assay C_25625805_10 and C_27104892_10, respectively (Applied Biosystems). We were unable to genotype L128R even by using different Taqman probes or restriction enzymes.
All genotypes were confirmed by sequencing of randomly selected samples.
Sequencing
The promoter region (nucleotide number from 3377 up to 3744, according to sequence accession number AY587020) as well as the coding and flanking regions of VKORC1 gene were sequenced in 57 selected patients. Regions were amplified by PCR and sequencing was carried out in an ABI Prism 3130xl Avant Genetic Analyzer (Applied Biosystems) using standard protocols.
Statistical Analysis
Comparisons between genotype groups were performed by t test and the results are expressed as mean ± SD. Correlations were analyzed by Pearson's correlation test. A multivariate stepwise linear regression was performed to evaluate the potential contribution of different polymorphisms to inter-individual variability in the stable therapeutic acenocoumarol dose. All analyses were carried out using SPSS version 15.0 software (SPSS Inc. Chicago, IL, USA). A P-value<0.05 was considered to be statistically significant.
Results
Selected outlier patients
The strategy that led us to select outlier patients as well as the genetic profiles defined by VKORC1 -1639G>A and CYPC9* polymorphisms are shown in Figure 1. Eighteen profiles covering all potential combinations were identified in our sample. The mean acenocoumarol dose for VKORC1 rs9923231 and CYP2C9 genotypes is described in Table 1.
Table 1. Prevalence and acenocoumarol reference dose of combined genetic profiles of CYP2C9 and VKORC1 polymorphisms in whole sample (3949 patients) and in 57 outlier patients.
| Profile | CYP2C9 | VKORC1 | Whole sample N (%) | Whole sample reference dose$ | Outlier N | Outlier with dose below reference, N | Outlier with dose above reference, N |
| #1 | *1*1 | GG | 782 (20) | 18±7 | 13 | 1 | 12 |
| #2 | *1*1 | GA | 1132 (29) | 14±5 | 11 | 1 | 10 |
| #3 | *1*1 | AA | 390 (10) | 9±4 | 8 | - | 8 |
| #4 | *1*2 | GG | 349 (9) | 17±6 | 6 | - | 6 |
| #5 | *1*2 | GA | 486 (12) | 13±5 | 9 | - | 9 |
| #6 | *1*2 | AA | 156 (4) | 9±3 | - | - | - |
| #7 | *1*3 | GG | 160 (4) | 14±5 | 4 | - | 4 |
| #8 | *1*3 | GA | 216 (5) | 10±4 | 2 | - | 2 |
| #9 | *1*3 | AA | 66 (2) | 7±3 | 3 | - | 3 |
| #10 | *2*2 | GG | 37 (1) | 15±4 | - | - | - |
| #12 | *2*2 | GA | 56 (1) | 11±6 | 1 | - | 1 |
| #13 | *2*2 | AA | 18 (0.5) | 8±3 | - | - | - |
| #14 | *2*3 | GG | 35 (1) | 13±5 | - | - | - |
| #15 | *2*3 | GA | 44 (1) | 9±3 | - | - | - |
| #16 | *2*3 | AA | 12 (0.3) | 5±1 | - | - | - |
| #17 | *3*3 | GG | 4 (0.1) | 5±2 | - | - | - |
| #18 | *3*3 | GA | 5 (0.13) | 11±10 | - | - | - |
| #1 | *3*3 | AA | 1 (0.03) | 6 | - | - | - |
Profiles were obtained by combining genotypes VKORC1 rs9923231 (−1639G>A) and CYP2C9 rs1799853 and rs1057910.
mg/week expressed as mean ±SD.
One hundred and forty five patients were outside the mean±2SD of their genetic profile (3.7%). For further studies, we excluded those patients with clinical factors potentially involved in the unexpected dose requirement: autoimmune diseases (N = 10); liver failure (N = 6); severe heart failure (N = 8); severe chronic obstructive pulmonary disease (N = 10); acenocoumarol interacting drugs (N = 37); new thrombotic events (N = 6); obesity (N = 2); and associated tumoral diseases (N = 5), as well as those patients with no clinical data (N = 4). Finally, 57 out of 145 were defined as outlier patients (Figure 1).
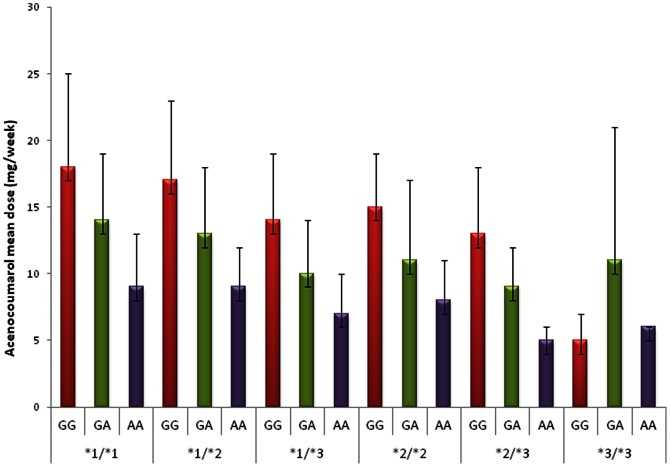
Table 1 shows the mean acenocoumarol dose for each profile as well as the number of cases carrying each profile. According to the prevalence of the polymorphisms defining the profiles, the most frequent profile was represented by the VKORC1 −1639G>A in heterozygous state plus CYP2C9*1 in homozygous state (#2, N = 1132) (Table 1 and Figure 2). In contrast, only one patient carried the profile #18 (homozygous for both VKORC1 -1639A and CYP2C9*3). Table 1 also shows the proportion of outlier patients for each genetic profile. Most of these outlier patients took doses greater than that expected for the genetic profile (Table 1). As shown, the proportion of outlier patients was similar in all profiles (Table 1).
Figure 2. Ranking of acenocoumarol dose distribution in VKORC1 and CYP2C9 combined genetic profiles in 3949 anticoagulated patients.
VKORC1 sequencing
Sequencing of the coding and promoter region in the 57 selected patients revealed a wild-type VKORC1 genotype in according to reference sequence, in 43 of them (75%). VKORC1 variants were identified in 14 outlier patients (25%), all of them with a higher acenocoumarol dose than expected (Table 2). We identified two mutations associated with high coumarin requirements and previously related with unsuccessful anticoagulation: 3 cases with D36Y [17], [18] and 1 case with L128R [19]. Additionally, there was a high prevalence of other polymorphisms: rs7200749 (L120L) in 2 patients (3.5%), rs55894764 (R12R) in 4 patients (7%), and rs17878544 a promoter variant (g.3350A>G) not found in Caucasian ancestry [20] in 5 patients (8.8%). We also identified 2 patients with no linkage disequilibrium (LD) between rs9923231 (-1639G>A) and rs9934438 (1173C>T) (3.5%) (Table 2). Additionally 2 outlier patients carried simultaneously rs17878544 and rs7200749. One patient was heterozygous for both rs55894764 and L128R (not shown).
Table 2. New variants of VKORC1 identified in this study and their impact on acenocoumarol dose in whole sample (3949 patients) and in 57 outlier patients.
| VKORC1 variants | Outlier N (%) | Outlier Dose* | Whole sample N (%) | Whole sample Dose* | P | |
| D36Y | GG GT+TT | 54 (94.7) 3+0 (5.3) | 29±11 36±3 | 3935 (99.6) 14+0 (0.4) | 14±6 22±9 | 0.004 |
| L128R | TT TG+GG | 56 (98.2) 1+0 (1.8) | 29±11 36 | N.D. | N.D. | N.D. |
| R12R (rs55894764) | GG GA+AA | 53 (93.0) 4+0 (7.0) | 29±11 36±6 | 3744 (95) 198+4 (5.2) | 14±5 16±6 | <0.001 |
| L120L (rs7200749) | CC CT+TT | 55 (96.5) 2+0 (3.5) | 29±11 29±0.6 | 3861 (97.8) 85+3 (2.2) | 14±6 16±7 | 0.001 |
| g. 3350A>G (rs17878544) | AA AG+GG | 52 (91.2) 5 (8.8) | 28±10 40±13 | 3782(95.8) 161+5 (4.2) | 14±6 15±7 | 0.002 |
| LD rs2323991/ rs9934438 | Yes No | 55 (96.5) 2 (3.5) | 30±11 14±11 | 3943 (99.9) 6 (0.2) | 14±6 14±5 | 0.813 |
mean ±SD of acenocoumarol expressed as mg/week. P value is calculated by t test to compare acenocoumarol dose depending on genotypes in the whole sample. One sample is missed for genotyping rs17878544 and three for R12R.
VKORC1 genotyping in the whole sample
These findings encouraged us to test for the prevalence of these VKORC1 variants in the whole cohort of 3949 anticoagulated patients (Table 2).
Our findings confirmed that rs55894764 (R12R) is a common polymorphism in Caucasians with a minor allelic frequency (MAF) of 5.2% (Table 2). Interestingly, carriers seem to have higher requirements of acenocoumarol than non-carriers (14 vs 16 mg/week; p<0.001) (Table 2). On the other hand, D36Y variant was found in 14 patients (0.4%), all in heterozygous state, and this finding was also associated with a higher acenocoumarol dose (22 mg/week carriers vs 14 mg/week non-carriers; p = 0.004) (Table 2).
rs7200749 (L120L) was also a common polymorphism in our population (MAF = 2.3%), and was significantly associated with an increased dose of anticoagulant (carriers 16 vs non-carriers 14 mg/week; p = 0.001) (Table 2).
rs17878544, located in the promoter region of VKORC1, had a frequency of 4% in our population, with a significant relationship between dose and genotype. Thus, AA carriers needed a slightly lower acenocoumarol dose than G carriers (14 vs 15 mg/week respectively; p = 0.002) (Table 2).
Finally, loss of LD between rs9923231and rs9934438 was found in 6 patients (0.15%) (r2 = 0.98, D´ = 0.99)(Table 2). These data were very similar to those previously described in the bibliography [21]. The clinical data as well as the genetic profile of these 6 patients are shown in Table 3.
Table 3. Clinical characteristics and genetic profiles of 6 patients who lost the LD between VKORC1 polymorphisms rs2323991 and rs9934438.
| Patient | Age | Sex | Diagnostic | rs9923231 | rs9934438 | CYP2C9 | Dose# |
| A | 65 | Female | PE | GG | CT | *1*1 | 19 |
| B | 70 | Female | AF | GA | CC | *1*2 | 18 |
| C | 82 | Female | AF | GA | TT | *1*1 | 5 |
| D | 78 | Female | AF | GA | TT | *1*1 | 9 |
| E | 48 | Male | AF | AA | CT | *1*1 | 24 |
| F | 65 | Female | DVT | AA | CT | *1*2 | 12 |
#Dose as mg of acenocoumarol per week PE: pulmonary embolism; AF: atrial fibrillation; DVT: deep venous thrombosis
When the LD was analyzed among all SNPs found in this study, i.e., rs55894764, rs7200749, rs17878544 and rs9923231, only rs17878544 was in LD with rs7200749 (r2 = 0.53, D´ = 0.99).
Our data showed that the VKORC1 changes were much more frequent in the outlier group than in the whole sample. Thus, Table 2 describes the differences of frequencies of the new VKORC1 variants between the outlier group and the whole sample.
Additive regression model to predict the acenocoumarol dose
We further performed a multivariate linear regression model by including thefactors (both demographic and genetic) that resulted statistically significant in the univariate analysis. The results obtained for the multivariate linear regression model showed that, among demographical factors, only age had a significant effect on acenocoumarol dose. Thus, together with VKORC1 rs9923231 and CYP2C9 genotypes, the model yielded a R2 = 0.391 (Table 4). Interestingly, two variants identified in this study, D36Y and rs55894764, were also significantly associated with the requirement for acenocoumarol (beta coefficient 0.061and 0.034, respectively) (Table 4). However, their global contributions to dose prediction were small (from 39% to 40%).
Table 4. Summary of the additive regression model (stepwise method): predictor contribution to steady therapeutic dose of acenocumarol in 3949 anticoagulated patients.
| R2 | P | ß coefficient (p) | |
| −1639 G>A (rs9923231) | 0.210 | <0.001 | −0.461 (<0.001) |
| plus Age | 0.340 | <0.001 | −0.364 (<0.001) |
| plus CYP2C9 | 0.391 | <0.001 | −0.216 (<0.001) |
| plus D36Y | 0.395 | <0.001 | −0.061 (<0.001) |
| plus R12R (rs55894764) | 0.400 | <0.001 | 0.034 (0.006) |
Discussion
Several mathematical models exist that combine both clinical and genetic data to predict the required dose of coumarins, to improve the dosing forecast in patients starting oral anticoagulant therapy [10]. The efforts of many cooperative groups of researchers have led to algorithms with r2 ∼50% [7], [15]. This means that a not negligible proportion of patients will still be outside the range of the best forecast models. All these data have clearly been recovered in the Clinical Pharmacogenetics Implementation Consortium published guidelines for warfarin dosing [22]. Our aim here was to identify new genetic factors that might contribute to the patient´s requirements of acenocoumarol.
The retrospective study of 3949 consecutive patients taking a steady acenocoumarol dose revealed that a small proportion of patients (N = 145, 3.7%) escaped the wide ranges of acenocoumarol dose governed by VKORC1 and CYP2C9 genotypes. Clinical factors potentially involved in such an abnormal response were identified in 88 of these patients (61%). The VKORC1 gene was sequenced in the remaining patients (N = 57) in order to identify new genetic variants involved in the anticoagulant therapy. Fourteen patients (25%) had genetic alterations within VKORC1. For this reason, we evaluated whether these VKORC1 genetic variations might contribute explaining the unexpected acenocoumarol dose of these patients.
We highlight the identification of two VKORC1 variants previously linked to high coumarin doses, D36Y and L128R. The D36Y mutation has been reported as a functional mutation leading to warfarin resistance or high warfarin requirements [17], [18]. It is exceptionally common in Jews of Ethiopian origin (allele frequency 15%) and to lesser extent in Ashkenazi Jews (4%) or in Sephardi Jewish (0.6%) [23], [24]. These data clearly show that in some ethnic groups a proportion of patients would be misclassified if only the main CYP2C9 and VKORC1 variants were screened [24]. Here, in a large Caucasian cohort, the low frequency of this mutation, recently described in a small unselected patient cohort [25], is confirmed. Further studies analyzing the cost/benefit relationship of including D36Y in primary pharmacogenetic screening for initial dosing should be performed. Whatever the case, we believe that genotyping D36Y could be of benefit for those patients requiring significantly higher doses than that determined by genetic and clinical algorithms. On the other hand, although we were unable to genotype L128R on a large scale this genotype has been previously described only in rare cases with warfarin resistance [19], [26]., Similarly to D36Y, therefore, it may be speculated that this mutation should only be considered in those few patients that escape the expected forecast.
Additionally, our study suggests novel associations of VKORC1 variants potentially involved in the pharmacogenetics of acenocoumarol. Thus, rs55894764 (R12R) was originally described in wild rats trapped in anticoagulant-exposed areas and so it might be a sign of strong evolutionary selection [27]. Our findings indicated that this variation is a polymorphism in our population that is carried by 5% of Caucasian subjects.
Although its relation with in vivo warfarin resistance remains elusive [27], heterozygous carriers were found to have higher acenocoumarol requirements. Further studies are required to verify this potential association and, if found, it might be of interest to performed functional studies to identify the mechanism explaining why a silent polymorphism might have functional effects on VKORC1.
Another synonymous polymorphism, rs7200749 (L120L) identified in this study has been described by two groups to have different effects on warfarin dose. In Caucasian patients this SNP had no relationship to dose [28], whereas an increase in warfarin dosage was described in a South African black population [29]. Our study suggests that this polymorphism increases the requirements for acenocoumarol with a clear genotype-dose correlation. However, in the absence of homozygous subjects, phenotypic-genotypic associations are difficult to establish. To date, rs17878544 has only been described in populations with African ancestry, and is characteristic of a haplotype predictive of high warfarin dose [20]. Given the historical connections of Spain with the African/South American slave trade and the long coexistence with Muslim from neighboring African countries, the high frequency of this allele in Spanish people may indicate population affinity.
This synonymous change could have per se a functional effect [30], although we think that its potential functional effect might be explained by its LD with rs17878544 located at VKORC1 promoter region. Further studies, including reporter approaches, are required to sustain this hypothesis.
Finally, the loss of LD between rs9923231 and rs9934438 might also contribute to explaining the small proportion of patients taking unexpectedly high acenocoumarol doses. No more alterations were found in the sequenced VKORC1 regions of these few patients. Although our data showed that, if we take into account rs9934438, the acenocoumarol steady doses are nearer those to be expected than if we take into account rs9923231, additional studies in other populations would confirm or discard this observation. Additionally, new approaches would clarify whether rs9934438 (regardless of rs9923231) has structural consequences for VKORC1 activity and/or function.
Our work has some limitations, as the significance of these findings cannot fully be understood without functional experiments showing differential protein expression. Moreover, in this work we did not genotype for other SNPs known to contribute with smaller effect to higher dose requirements, such as in the CYP4F2 [14], GGCX [31] or CALU [32] genes. Then, we could not rule out these SNPs as contributors to higher dose requirements in the outlier group.
In summary, in a large cohort of acenocoumarol-treated patients we found novel associations of VKORC1 variants with a higher stable dose, albeit with a low effect size. Newly available strategies such as exome sequencing or the analysis of the copy number variation [33] would help to identify variations responsible for outlier anticoagulant dosing.
Acknowledgments
Authors acknowledge the technical support of N. Garcia-Barberá.
Funding Statement
This work was supported by research grants from ISCIII (PI08/1531), ISCIII (Red RECAVA RD06/0014/0039), Fundación Séneca (07703/GERM/07), Río Hortega contract from Instituto Carlos III (ISCIII) (VPA). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Vandvik PO, Lincoff AM, Gore JM, Gutterman DD, Sonnenberg FA, et al. (2012) Primary and Secondary Prevention of Cardiovascular Disease: Antithrombotic Therapy and Prevention of Thrombosis, American College of Chest Physicians. Evidence-Based Clinical Practice Guidelines 9thed. Chest 141: e637S–68S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wadelius M, Chen LY, Lindh JD, Eriksson N, Ghori MJ, et al. (2009) The largest prospective warfarin-treated cohort supports genetic forecasting. Blood 113: 784–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gage BF, Eby C, Johnson JA, Deych E, Rieder MJ, et al. (2008) Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther 84: 326–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takeuchi F, McGinnis R, Bourgeois S, Barnes C, Eriksson N, et al. (2009) A Genome-Wide Association Study Confirms VKORC1, CYP2C9, and CYP4F2 as Principal Genetic Determinants of Warfarin Dose. PLoS Genet 5: e1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Teichert M, Eijgelsheim M, Rivadeneira F, Uitterlinden AG, van Schaik RH, et al. (2009) A genome-wide association study of acenocoumarol maintenance dosage. Hum Mol Genet 18: 3758–3768. [DOI] [PubMed] [Google Scholar]
- 6. Daly AK (2010) Genome-wide association studies in pharmacogenomics. Nat Rev Genet 11: 241–6. [DOI] [PubMed] [Google Scholar]
- 7. International Warfarin Pharmacogenetics Consortium, Klein TE, Altman RB, Eriksson N, Gage BF, et al. (2009) Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med 360: 753–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Finkelman BS, Gage BF, Johnson JA, Brensinger CM, Kimmel SE (2011) Genetic warfarin dosing: tables versus algorithms. J Am Coll Cardiol 57: 612–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kurnik D, Loebstein R, Halkin H, Gak E, Almog S (2009) 10 years of oral anticoagulant pharmacogenomics: what difference will it make? A critical appraisal. Pharmacogenomics 10: 1955–1965. [DOI] [PubMed] [Google Scholar]
- 10. Becquemont L, Alfirevic A, Amstutz U, Brauch H, Jacqz-Aigrain E, et al. (2011) Practical recommendations for pharmacogenomics-based prescription: 2010 ESF-UB Conference on Pharmacogenetics and Pharmacogenomics. Pharmacogenomics 12: 113–124. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Food and Drug Administration (2007) Press Release: FDA approves updated warfarin (Coumadin) prescribing information. Rockville, MD: FDA. Available: http://www.fda.gov/bbs/topics/NEWS/2007/NEW01684.html. Accessed 2008 May 19.
- 12. Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, et al. (2012) Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141: e152S–84S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pérez-Andreu V, Roldán V, González-Conejero R, Hernández-Romero D, Vicente V, et al. (2009) Implications of pharmacogenetics for oral anticoagulants metabolism. Curr Drug Metab 10: 632–642. [DOI] [PubMed] [Google Scholar]
- 14. Pérez-Andreu V, Roldán V, Antón AI, García-Barberá N, Corral J, et al. (2009) Pharmacogenetic relevance of CYP4F2 V433M polymorphism on acenocoumarol therapy. Blood 113: 4977–4979. [DOI] [PubMed] [Google Scholar]
- 15. van Schie RM, Wessels JA, le Cessie S, de Boer A, Schalekamp T, et al. (2011) EU-PACT Study Group Loading and maintenance dose algorithms for phenprocoumon and acenocoumarol using patient characteristics and pharmacogenetic data. Eur Heart J 32: 1909–1917. [DOI] [PubMed] [Google Scholar]
- 16. Verde Z, Ruiz JR, Santiago C, Valle B, Bandrés F, et al. (2010) A novel, single algorithm approach to predict acenocoumarol dose based on CYP2C9 and VKORC1 allele variants. PLoS One 5: e11210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Loebstein R, Dvoskin I, Halkin H, Vecsler M, Lubetsky A, et al. (2007) A coding VKORC1 Asp36Tyr polymorphism predisposes to warfarin resistance. Blood 109: 2477–2480. [DOI] [PubMed] [Google Scholar]
- 18. Watzka M, Geisen C, Bevans CG, Sittinger K, Spohn G, et al. (2011) Thirteen novel VKORC1 mutations associated with oral anticoagulant resistance: insights into improved patient diagnosis and treatment. J Thromb Haemost 9: 109–118. [DOI] [PubMed] [Google Scholar]
- 19. Harrington DJ, Gorska R, Wheeler R, Davidson S, Murden S, et al. (2008) Pharmacodynamic resistance to warfarin is associated with nucleotide substitutions in VKORC1. J Thromb Haemost 6: 1663–1670. [DOI] [PubMed] [Google Scholar]
- 20. Limdi NA, Beasley TM, Crowley MR, Goldstein JA, Rieder MJ, et al. (2008) VKORC1 polymorphisms, haplotypes and haplotype groups on warfarin dose among African-Americans and European-Americans. Pharmacogenomics 9: 1445–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang D, Chen H, Momary KM, Cavallari LH, Johnson JA, et al. (2008) Regulatory polymorphism in vitamin K epoxide reductase complex subunit 1 (VKORC1) affects gene expression and warfarin dose requirement. Blood 112: 1013–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Johnson JA, Gong L, Whirl-Carrillo M, Gage BF, Scott SA, et al. (2011) Guidelines for CYP2C9 and VKORC1 genotypes and warfarin dosing. Clin Pharmacol Ther 90: 625–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aklillu E, Leong C, Loebstein R, Halkin H, Gak E (2008) VKORC1 Asp36Tyr warfarin resistance marker is common in Ethiopian individuals. Blood 111: 3903–3904. [DOI] [PubMed] [Google Scholar]
- 24. Scott SA, Edelmann L, Kornreich R, Desnick RJ (2008) Warfarin pharmacogenetics: CYP2C9 and VKORC1 genotypes predict different sensitivity and resistance frequencies in the Ashkenazi and Sephardi Jewish populations. Am J Hum Genet 82: 495–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shuen AY, Wong BY, Fu L, Selby R, Cole DE (2012) Evaluation of the warfarin-resistance polymorphism, VKORC1 Asp36Tyr, and its effect on dosage algorithms in a genetically heterogeneous anticoagulant clinic. Clin Biochem 45: 397–401. [DOI] [PubMed] [Google Scholar]
- 26. Bodin L, Perdu J, Diry M, Horellou MH, Loriot MA (2008) Multiple genetic alterations in vitamin K epoxide reductase complex subunit 1 gene (VKORC1) can explain the high dose requirement during oral anticoagulation in humans. J Thromb Haemost 6: 1436–1439. [DOI] [PubMed] [Google Scholar]
- 27. Rost S, Pelz HJ, Menzel S, MacNicoll AD, León V, et al. (2009) Novel mutations in the VKORC1 gene of wild rats and mice--a response to 50 years of selection pressure by warfarin? BMC Genet 10: 4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. D'Andrea G, D'Ambrosio RL, Di Perna P, Chetta M, Santacroce R, et al. (2005) A polymorphism in the VKORC1 gene is associated with an interindividual variability in the dose-anticoagulant effect of warfarin. Blood 105: 645–649. [DOI] [PubMed] [Google Scholar]
- 29. Mitchell C, Gregersen N, Krause A (2011) Novel CYP2C9 and VKORC1 gene variants associated with warfarin dosage variability in the South African black population. Pharmacogenomics 12: 953–963. [DOI] [PubMed] [Google Scholar]
- 30. Sauna ZE, Kimchi-Sarfaty C (2011) Understanding the contribution of synonymous mutations to human disease. Nat Rev Genet 12: 683–691. [DOI] [PubMed] [Google Scholar]
- 31. King CR, Deych E, Milligan P, Eby C, Lenzini P, et al. (2010) Gamma-glutamyl carboxylase and its influence on warfarin dose. Thromb Haemost 104: 750–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. González-Conejero R, Corral J, Roldán V, Ferrer F, Sánchez-Serrano I, et al. (2007) The genetic interaction between VKORC1 c1173t and calumenin a29809g modulates the anticoagulant response of acenocoumarol. J Thromb Haemost 5: 1701–1706. [DOI] [PubMed] [Google Scholar]
- 33. Krumm N, Sudmant PH, Ko A, O'Roak BJ, Malig M, et al. (2012) Copy number variation detection and genotyping from exome sequence data. Genome Res 22: 1525–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]