Abstract
A multidisciplinary model is a useful approach in the management of hepatocellular carcinoma (HCC) to coordinate, individualize, and optimize care. The HCC Multidisciplinary Team (MDT) at Temple University Hospital was established in 2008 and comprises hepatologists, interventional radiologists, transplant surgeons, oncologists, residents, midlevel providers, and support staff. Patients may be enrolled by referral from (1) oncologists at Temple, (2) the hepatitis screening clinic recently established at Temple and staffed by hepatology residents, or (3) community practices. MDT conferences are held weekly, during which cases are discussed (based on medical history, interpretation of images, and laboratory analyses) and treatment plans are formulated. The Temple treatment algorithm follows current standards of care, guided by tumor volume and morphology, but the novel multidisciplinary interaction challenges members to tailor therapy to achieve the best possible outcomes. Patients with a solitary lesion ≤ 2 cm may receive no treatment until eligible for transplantation or locoregional therapy or resection, with imaging every 3 to 6 months to monitor tumor progression. In patients with tumors > 2 cm and ≤ 5 cm, microwave ablation therapy is used if lesions are discrete and accessible. Conventional transarterial chemoembolization (TACE) or drug-eluting bead TACE (DEB-TACE) or yttrium-90 microspheres are utilized in multifocal disease. Patients with lesions > 5 cm are candidates for TACE for downstaging the tumor. Sorafenib is typically reserved for unresectable lesions between 2 cm and 5 cm. Frequently, we administer sorafenib continuously and in combination with DEB-TACE. In our experience, sorafenib does not produce effects on the tumor vasculature or blood flow that would impair the efficacy of DEB-TACE. The literature documents improved outcomes in HCC and other cancers associated with the introduction of multidisciplinary care. The role and organization of the MDT is influenced by team culture, expertise, and process, as well as institutional and larger environmental contexts.
Keywords: HCC, coordinated care, interdisciplinary, transplant
Introduction
Hepatocellular carcinoma (HCC) is a disease of multifactorial etiology that presents multiple management challenges and thus a need for coordinated medical care.1 In the United States, the incidence of HCC has dramatically increased over the past 3 decades and is projected to continue rising due to the increasing incidence of hepatitis C virus (HCV) infection and non-alcoholic fatty liver disease (NAFLD).2 Chronic hepatitis B virus (HBV) infection and HCV infection are leading risk factors for HCC worldwide; in countries where HBV infection is not endemic, HCV and alcoholic cirrhosis are generally considered to be the most important risk factors for HCC. NAFLD and its clinical phenotype of diabetes and obesity also contribute substantially to the disease burden in Western countries.1–4
The clinical presentation of HCC varies widely. Early HCC is characteristically silent and slow-growing with few symptoms until late in the disease, leading to diagnosis in the advanced stage for many patients.1 This may severely limit treatment options. However, with newer technologies and implementation of surveillance programs, patients can be diagnosed earlier, permitting utilization of a greater range of treatments.3 Early and accurate diagnosis of tumors relies on clinical suspicion, screening protocols, serologic testing, radiologic imaging by computed tomography and magnetic resonance imaging, and confirmation by tissue biopsy when clinically necessary.1–4
Clearly, HCC is a complex disease and its management must address the unique challenges of underlying liver dysfunction and cancer treatment. This manuscript will describe the Temple University Hospital approach to integrating the expertise of many clinician specialists to expedite treatment and enhance outcomes for patients with HCC, regardless of etiology. We believe that the experience and perspectives gained at our center may be useful to other institutions in establishing multispecialty models to advance HCC care through earlier intervention with curative therapies.
The Temple model of multidisciplinary care in HCC
History and evolution
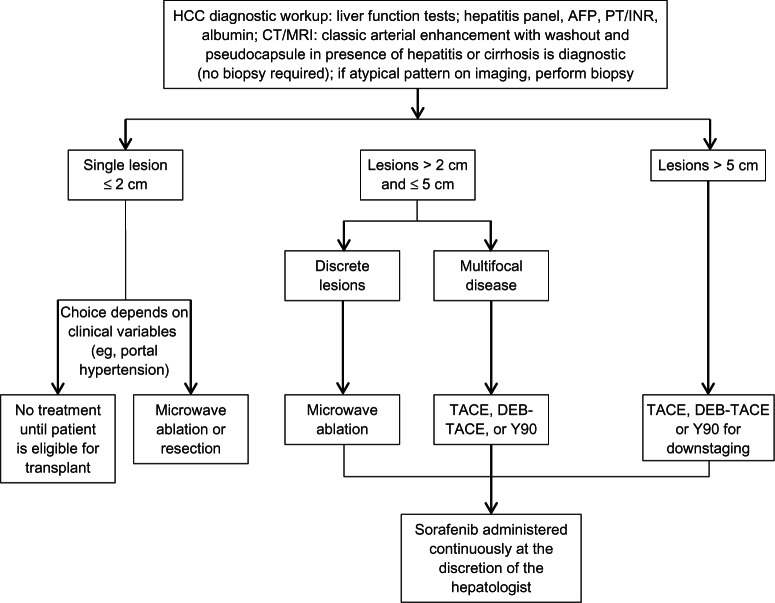
The Temple approach to HCC management (Figure 1) follows the standard of care as developed according to the Barcelona Clinic Liver Cancer staging strategy and supported by the American Association for the Study of Liver Diseases and National Comprehensive Cancer Network practice guidelines.1–5 Given the established complexity of the disease and the multimodal approaches to HCC diagnosis and treatment, we believe that patients benefit from a coordinated approach to individualize, optimize, and expedite care. To this end, a multidisciplinary team (MDT) has evolved within the clinical environment of HCC management at Temple University Hospital. Prior to establishment of the Temple MDT, care of HCC patients was coordinated primarily by hepatologists. In 2007, a small team comprising one hepatologist (MB) and one interventional radiologist (IR) (GC) began to meet every other week to review imaging data, discuss patient cases, determine transplant eligibility, and develop treatment plans for selected patients. These meetings became the springboard for integrating additional specialists and the establishment of a regular weekly conference schedule in 2008 for consultation and teaching. Over the ensuing months, reactivation of the liver transplant program led to the addition of a transplant surgeon and a second hepatologist. Notably, the establishment of an MDT nurse coordinator position was critical in facilitating patient entry into the MDT system; maintaining patient data; and ensuring that assessments, interventions, and follow-up visits were scheduled and completed efficiently. Subsequently, as the number of enrollees increased, the MDT expanded to include a radiologist, an additional IR, a third hepatologist, an oncologist, a pathologist, a nurse practitioner, a hepatology nurse, and an IR coordinator. Additional support services are provided by psychologists, social workers, and nutritionists, as required. Currently, the IR coordinator and nurse practitioner work together to coordinate patient care as well as MDT meeting agendas. Notably, transplant, hepatology, and radiology residents regularly attend and participate in the MDT conferences. Currently, the MDT manages the ongoing care of 50 patients. At weekly conferences, imaging data are reviewed and treatment plans revised for approximately 12 to 15 patients; for other enrollees, treatment plans may be in progress and further consultation may be on hold pending completion of a locoregional therapy (LRT) procedure or availability of imaging data.
Figure 1.
The Temple University multidisciplinary team treatment approach for patients with HCC.4
Abbreviations: AFP, alpha-fetoprotein; CT, computed tomography; DEB-TACE, drug-eluting bead TACE; HCC, hepatocellular carcinoma; MRI, magnetic resonance imaging; PT/INR, prothrombin time/International Normalized Ratio; TACE, transarterial chemoembolization; Y90, yttrium-90.
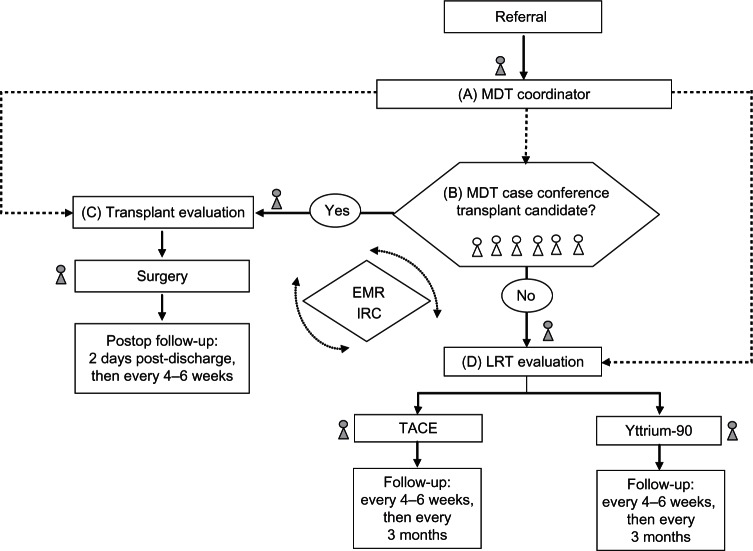
Patient flow in the Temple MDT model
Patients are “enrolled” directly through MDT members or by referral from other Temple University Hospital specialists or community hepatologists (Figure 2). The recently established Temple Hepatitis Clinic is also an important source of patient referrals. This clinic is staffed by hepatology residents and provides screening and surveillance for patients at risk, allowing increased opportunity for earlier intervention and more intensive monitoring in patients with smaller, more easily treatable tumors. Patients who subsequently develop new lesions are then eligible for expedited care due to the availability of, and easy access to, prior laboratory and other clinical data.
Figure 2.
Patient flow through the Temple University MDT care model for HCC management is depicted in this flow diagram.
Notes: Following intake by the MDT coordinator (A), patient data are reviewed by the MDT (B) to determine transplant eligibility. Under the direction of the transplant nurse (C), transplant candidates undergo comprehensive evaluation and multimodal screening tests (eg, serum chemistries, MRI, CT, pulmonary function, and cardiac tests). Those who are currently ineligible for transplant (D) are screened for LRT (TACE or Y90 radioembolization) and undergo further assessments to confirm eligibility (eg, arteriography, 99mTc scans). Throughout the course of care, the MDT coordinator provides support in scheduling and explaining procedures and addresses concerns and questions. Post-transplant and post-LRT, patient progress is collaboratively reviewed each week. MDT members can access and share information via the EMR system and with the assistance of the IRC, who stores images and other data in a central repository.
Abbreviations: CT, computed tomography; EMR, electronic medical record; HCC, hepatocellular carcinoma; IRC, interventional radiology coordinator; LRT, locoregional therapy; MDT, multidisciplinary team; MRI, magnetic resonance imaging; TACE, transarterial chemoembolization; Y90, yttrium-90.
MDT patients typically receive outpatient care through a single specialty clinic (eg, hepatology), but are carefully educated about the team approach through all phases of treatment. Occasionally, a multispecialty visit may be scheduled when a multimodality approach is considered. At each clinic visit, the patient meets with the MDT coordinator and hepatology nurse to relay current clinical information, undergo laboratory and other clinical assessments and treatments, and schedule future visits. Patient education regarding the treatment pathway, preventive health measures, and side effect management constitutes a key component of HCC care; the hepatology nurse and coordinator work diligently to liaise with other MDT members to communicate the appropriate information for expediting and optimizing treatments. Follow-up check-in and reminder calls are managed through the coordinator and MDT nurses. Because care is individualized for each patient, personalized follow-up interviews and monitoring parameters may vary in frequency. The Temple Hospital electronic medical record system facilitates the sharing of information among team members and is routinely utilized to inform the coordinator about the completion of a specific diagnostic evaluation or intervention or the availability of new data to be communicated to the MDT and patient.
All MDT members and their residents are invited to participate in a 1–2 hour weekly conference, during which all new and recurrent patients are discussed and evaluated based on interpretation of images, laboratory analyses, medical history, and other data. Due to time constraints, patients with the most acute conditions or most significant changes in clinical status are often prioritized, but the team strives to discuss the needs of every enrolled patient. A primary goal of the conference is to evaluate patients’ eligibility for liver transplantation. To that end, MDT members present updates regarding each patient’s clinical exam and imaging results and provide opinions regarding the next steps for evaluation and treatment. The meeting format fosters collaborative interaction during visualization of radiographic images with interpretive dialog from the attending radiologist, followed by input from other MDT members. Potential conflicts or divergence of opinion are further debated and ultimately resolved by consensus or by the attending hepatologist. When appropriate, clinicians outside the core MDT are consulted. Weekly MDT conference agendas are developed and distributed by the MDT coordinator staff. Similarly, compilation and distribution of meeting minutes is managed by coordinators as are follow-up actions, such as patient scheduling and chart updates.
Temple MDT treatment approach
It is commonplace for oncologists to require histologic evidence of cancer in any suspicious lesion for which a diagnosis of cancer is under consideration. This is not a requirement in HCC, as biopsy of a liver tumor may result in spread of cancer cells outside the liver, creating an opportunity for later metastasis. Instead, the radiologic behavior of the lesion is utilized to make the diagnosis without pathologic evaluation, as evidenced by arterial enhancement during the initial contrast injection with washout in the venous phase. In addition, we measure the serum alpha-fetoprotein (AFP); in patients with normal or near-normal AFP and atypical radiologic features, a biopsy is performed to establish a diagnosis.
At the Temple University Hospital, HCC treatment is guided by tumor morphology and number, based on standard guidelines. Our primary goal is to identify candidates for radical therapies with curative potential. Well-selected patients with small tumors who are ineligible for resection or transplantation may be candidates for percutaneous ethanol ablation,1–5 but this modality is not often employed by our group. In recent years, microwave ablation has emerged as a thermal ablative modality possessing many advantages such as convection profile, larger ablation volumes, and faster ablation times.6
Arterial embolization therapy – transarterial chemoembolization (TACE) and yttrium-90 (Y90) radioembolization – is palliative treatment generally reserved for patients with intermediate-stage HCC not amenable to resection, transplantation, or ablation.1–5 The best candidates for embolization are patients with excellent performance status, serum bilirubin ≤ 2.0 mg/dL, Child-Pugh A status, and multifocal noninvasive HCC. TACE administration at our center parallels evidence from two randomized clinical trials demonstrating increased survival following arterial embolization therapy over supportive care.7,8 In the first study, Llovet et al showed that TACE administered every 6 months significantly reduced the risk of death in patients with Child-Pugh A or B cirrhosis and unresectable HCC compared to symptomatic conservative treatment (hazard ratio [HR] 0.47, 95% confidence interval [CI] 0.25–0.91; P = 0.025).7 In the second trial, patients with Okuda stage I/II unresectable HCC treated with TACE every 2 to 3 months experienced a significant reduction in mortality risk compared to those treated symptomatically (relative risk 0.49, 95% CI 0.29–0.81; P = 0.006).8 In addition, a 2003 meta-analysis of six randomized controlled trials primarily in patients with Child-Pugh A status found that TACE/transarterial embolization improved 2-year survival compared with controls (odds ratio 0.53, 95% CI 0.32–0.89; P = 0.017).9 Although these studies provide valuable support for TACE use, we perform TACE selectively at our center and the MDT evaluates each patient individually at 4 to 6 weeks after the procedure to assess the need and potential timing for repeat TACE treatment. Drug-eluting bead TACE (DEB-TACE) or Y90 microspheres are used in multifocal disease or infiltrative lesions for patients who meet transplant criteria.10 At our center, Y90 treatment is preferred for patients with tumors occupying more than half of the liver or for patients who are frail and/or have portal vein thrombosis. Patients with lesions > 5 cm may be candidates for DEB-TACE or Y90 to downstage the tumor so the patient may be eligible for resection or transplantation. If indicated, alternating DEB-TACE and Y90 treatments are administered in poor responders.
In patients with advanced HCC marked by vascular invasion and/or extrahepatic disease, traditional systemic chemotherapies have marginal antitumor activity and fail to impact survival.1–5 At present, the oral multikinase inhibitor sorafenib is the only approved systemic treatment available for unresectable, advanced HCC based on two Phase III controlled trials that showed that median overall survival was significantly longer with sorafenib than with placebo.11,12 In the multinational, randomized, double-blind, placebo-controlled SHARP trial, sorafenib-treated patients exhibited significantly prolonged median survival (10.7 vs 7.9 months, HR 0.69, 95% CI 0.55–0.87; P < 0.001) and time to radiologic progression (5.5 vs 2.8 months, HR 0.58, 95% CI 0.45–0.74; P < 0.001) over placebo.12 In the Asia-Pacific trial, a similar reduction in risk for death was observed in sorafenib-treated patients (HR 0.68, 95% CI 0.50–0.9; P = 0.014) despite a study population with greater extrahepatic spread and poorer performance status.11 Notably, recent trials evaluating other tyrosine kinase inhibitors (sunitinib, linifanib, and brivanib) compared in a head-to-head fashion with sorafenib have shown no survival advantage over sorafenib as initial therapy in advanced HCC; thus sorafenib remains the only systemic agent showing a survival advantage in unresectable, advanced HCC.13,14
At our center, the MDT hepatologist often initiates treatment with sorafenib in patients with lesions > 2 cm who are not eligible for resection, prior to LRT with microwave ablation, radiofrequency ablation, Y90, or TACE. In our hands, we have not observed vascular crimping or blood flow alterations that might impede the response to LRT. Our primary goal is to limit tumor growth and downgrade the cancer until the patient is eligible for transplantation. Patients who exhibit disease progression despite treatment are recommended for participation in clinical trials.
Perceived impact of the MDT model on HCC care
Although objective data measuring the impact of the MDT approach on health care outcomes and resource utilization are not yet available, several benefits have already been realized from both MDT member and patient perspectives. MDT members unanimously cite the benefits of collaboration and collegiality inherent in a productive multispecialty culture. Importantly, the MDT is strongly committed to efficiently identifying potential transplant candidates and instituting appropriate therapies to enhance candidacy and delay disease progression. Once identified, transplant candidates continue to receive extensive support from multiple specialties, including transplant surgeons, hepatologists, gastroenterologists, radiologists, nurse practitioners, nurse coordinators, social workers, psychologists, and financial counselors. Here, a well-coordinated MDT approach can best address the needs of patients as they transition through all phases of the transplantation procedure.
MDT members frequently emphasize a greater efficiency in patient triage and rely on the input of colleagues in developing rational treatment plans. For example, inclusion of a dedicated radiologist has enhanced the value of the program, as imaging reports can now be tailored to assist the transplant surgeon, IR, and hepatologist in selecting the appropriate treatments. In addition, members emphasize the positive impact on the Temple training program; the MDT conference is well attended and reported by attendees to be “one of the best teaching and mentoring experiences.” At Temple University Hospital, MDT clinicians appreciate the support and input from midlevel providers (eg, nurse practitioners and residents) in challenging treatment decisions by sharing the patient’s perspective and their respective experience, as appropriate. The MDT encourages sharing of multiple viewpoints in a collegial environment that yields significant insight into possible therapeutic options. Clinicians support each other through collaborative decision-making and mentorship while enriching the fellow/resident training program. Although the potential benefits of the Temple MDT are significant, the biggest challenge currently involves the need for additional administrative support to coordinate care and allow further expansion of the MDT program. In addition, it must be noted that new and novel therapies are needed to supplement our current systemic armamentarium to promote opportunities for prolonged survival and cure.
MDT members believe that patients and their caregivers exhibit a clear understanding of treatment options and the anticipated treatment pathways. Importantly, patients and care-givers are knowledgeable regarding MDT roles and understand when and whom to call for questions and concerns. Moreover, patients voice a high level of confidence in and comfort with MDT health care providers, as they are shepherded through day-long visits and testing. MDT members state that being informed of a consistent plan and rationale for treatment is critical to patient acceptance of the plan. As a result, MDT members report that patients are, in fact, engaged and generally more compliant with the treatment plan offered. In the event that a plan becomes complex and confusing, patients are re-centered through contact with the MDT nurse or coordinator. Frequent follow-ups initiated by the MDT coordinator staff have successfully reinforced the patient-centered model. MDT nurse-driven education of patients and families about procedures and treatments has been well received.
Other models of HCC multidisciplinary management
Given the challenges of managing patients with HCC, multidisciplinary management programs have emerged at several institutions and have continued to evolve over the past decade. Overall, these programs appear diverse in structure, with their function determined primarily by the expertise of the respective multidisciplinary teams. Van Cleave et al described the early experience of implementing multidisciplinary supportive care for patients with HCC at the Philadelphia Veterans Affairs Medical Center.15 Between January 1995 and May 1998, 22 patients with HCC received best supportive care modeled on hospice care from a team consisting of physicians, nurses, pharmacists, social workers, psychologists, and chaplains. The goal was to preserve quality of life. Additionally, representatives from radiology, surgical oncology, radiation oncology, and medical oncology services convened at multidisciplinary tumor conferences with the mission of optimizing management for complicated cases and determining the best site of care (eg, clinic or hospice). Collaboration among clinicians continued following enrollment in the clinic and during hospitalization in order to ensure adequate management of pain and other disease-related symptoms.
Since 2001, the multidisciplinary liver tumor group at the Tom Baker Cancer Centre in Alberta, Canada has grown in diversity and size. The team, including three hepatobiliary surgeons, three transplant hepatologists, a medical oncologist, an advanced care nurse practitioner, and diagnostic and interventional radiologists, meets weekly to discuss management strategies for patients with HCC. This MDT adheres to the Alberta HCC Algorithm, which incorporates the principles of the Barcelona Clinic Liver Cancer staging system while clearly defining transplant criteria and the role of LRTs in early-stage HCC.16
Established in 2003, the University of California-San Francisco Veterans Affairs Medical Center (UCSF-VAMC) MDT implemented a practice of “fluid referral” as a means of referring patients among disciplines.17 An observational study comparing the outcomes for 121 patients treated for 3 years by the UCSF-VAMC MDT program and 62 patients from an American Cancer Society registry found that the UCSF-VAMC program promoted referral and evaluation at earlier stages of HCC (P < 0.0001). This in turn led to a significantly greater proportion of patients receiving treatment (P < 0.0001) as well as marked improvement in survival (65% post-MDT vs 21% pre-MDT; P < 0.0001).
Conclusion and future considerations
Fundamentally, the Temple MDT program builds on existing standards of care with the aim of improving outcomes and patient compliance. Patients benefit from the commitment of multiple caregivers who provide support and follow patients throughout the disease course. Multiple physicians and other providers are available to help with patient questions or concerns, and patients are supported as they move through the system. Patients derive comfort and confidence from knowing that their care is managed by the MDT, which in turn promotes patient engagement and compliance.
The Temple MDT conferences provide an opportunity for shared learning and have become so well attended and regarded that members have petitioned for future continuing medical education credit offerings for attendees. Furthermore, the team plans to further develop and report metrics to track the success and efficiency of MDT care. Future plans include comparative analyses of HCC care for patients enrolled in an MDT program versus traditional care; this will include cost assessments as well as survival and quality-of-life outcomes.
Notably, the recent addition of the Fox Chase Cancer Center to the Temple University Hospital System has been met enthusiastically by the Temple MDT, with expectations for a substantially increased patient volume and greater clinical trial involvement, particularly in the area of multimodality approaches. In addition, the MDT hopes to expand enrollment to include patients with colorectal cancer-related metastases. As a result, a larger dedicated team and longer multidisciplinary conference time will provide greater opportunities for student and fellow participation and mentoring.
Treatment of one of the few curable cancers such as HCC requires the expertise of multiple health care professionals. The MDT model is well suited to facilitating efficient and effective individualized treatment strategies to delay disease progression, extend survival, and maintain an acceptable quality of life. The experience described here can serve as a guide for other groups that are considering the development of an MDT for HCC care.
Team culture is an important factor when considering the establishment of an MDT. Full participation of all team members is obligatory for effective functioning of the team.18 Teams with shared egalitarian values tend to work together effectively. The multisource environ ment of an MDT facilitates sharing of consultative findings and exchange of ideas. This in turn aids in standardization of screening procedures, alignment of treatment protocols, and coordination of patient care.19 Overall, the MDT creates a milieu conducive to rapid transfer of clinical information among team members, thereby contributing to optimized care.
Acknowledgments
The content of this manuscript was developed by interviews with MDT members. The authors acknowledge the medical writing and editorial support provided by Percolation Communications LLC and funded by Onyx Pharmaceuticals, Inc. and Bayer HealthCare; and the continued support of MDT members Ray Fabrizio, MD; Ashok Jain, MD; Andreas Karachristos, MD; Natasha Morley, RN; Santiago Munoz, MD; Vishal Patel, MD; Ashwin Shetty, MD; Marie Schodle, RN; Parminder Bath Sohal, NP; and Rebecca Thomas, MD.
Footnotes
Disclosure
Dr Black has served as a speaker for Onyx, Bayer, Vertex, Merck, and Genentech. Dr Cohen has no relationships to disclose. The authors report no other conflicts of interest in this work.
References
- 1.Gish RG. Hepatocellular carcinoma: overcoming challenges in disease management. Clin Gastroenterol Hepatol. 2006;4(3):252–261. doi: 10.1016/j.cgh.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Cabrera R, Nelson DR. Review article: the management of hepatocellular carcinoma. Aliment Pharmacol Ther. 2010;31(4):461–476. doi: 10.1111/j.1365-2036.2009.04200.x. [DOI] [PubMed] [Google Scholar]
- 3.Bruix J, Sherman M, Practice Guidelines Committee, American Association for the Study of Liver Diseases Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 4.Bruix J, Sherman M, American Association for the Study of Liver Diseases Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verslype C, Van Cutsem E, Dicato M, et al. The management of hepatocellular carcinoma. Current expert opinion and recommendations derived from the 10th World Congress on Gastrointestinal Cancer, Barcelona, 2008. Ann Oncol. 2009;20(Suppl 7):vii1–vii6. doi: 10.1093/annonc/mdp281. [DOI] [PubMed] [Google Scholar]
- 6.Liang P, Wang Y. Microwave ablation of hepatocellular carcinoma. Oncology. 2007;72(Suppl 1):124–131. doi: 10.1159/000111718. [DOI] [PubMed] [Google Scholar]
- 7.Llovet JM, Real MI, Montaña X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359(9319):1734–1739. doi: 10.1016/S0140-6736(02)08649-X. [DOI] [PubMed] [Google Scholar]
- 8.Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35(5):1164–1171. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 9.Llovet JM, Bruix J. Systematic review of randomized trials for unresect-able hepatocellular carcinoma: Chemoembolization improves survival. Hepatology. 2003;37(2):429–442. doi: 10.1053/jhep.2003.50047. [DOI] [PubMed] [Google Scholar]
- 10.Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011;140(2:):497–507. doi: 10.1053/j.gastro.2010.10.049. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng AL, Kang YK, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10(1):25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 12.Llovet JM, Ricci S, Mazzaferro V, et al. SHARP Investigators Study Group Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 13.Cheng A, Kang Y, Lin D, et al. Phase III trial of sunitinib (Su) versus sorafenib (So) in advanced hepatocellular carcinoma (HCC) J Clin Oncol. 2011;29(Suppl) Abstr 4000. [Google Scholar]
- 14.Johnson P, Qin S, W PJ, et al. Brivanib (BRI) versus sorafenib (SOR) as first-line therapy in patients with unresectable, advanced hepatocellular carcinoma (HCC): results from the phase 3 BRISK-FL study [abstract LB-6]; Proceedings of the 63rd Annual Meeting of the American Association for the Study of Liver Diseases; November 9–13, 2012; Boston, MA, USA. [Google Scholar]
- 15.Van Cleave J, Devine P, Odom-Ball P. Multidisciplinary care of hepatocellular carcinoma. Cancer Pract. 1999;7(6):302–308. doi: 10.1046/j.1523-5394.1999.76007.x. [DOI] [PubMed] [Google Scholar]
- 16.Burak KW, Kneteman NM. An evidence-based multidisciplinary approach to the management of hepatocellular carcinoma (HCC): the Alberta HCC algorithm. Can J Gastroenterol. 2010;24(11):643–650. doi: 10.1155/2010/410574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang TT, Sawhney R, Monto A, et al. Implementation of a multidisciplinary treatment team for hepatocellular cancer at a Veterans Affairs Medical Center improves survival. HPB (Oxford) 2008;10(6):405–411. doi: 10.1080/13651820802356572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fennell ML, Das IP, Clauser S, Petrelli N, Salner A. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr. 2010;2010(40):72–80. doi: 10.1093/jncimonographs/lgq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gish RG, Lencioni R, Di Bisceglie AM, Raoul JL, Mazzaferro V. Role of the multidisciplinary team in the diagnosis and treatment of hepatocellular carcinoma. Expert Rev Gastroenterol Hepatol. 2012;6(2):173–185. doi: 10.1586/egh.11.105. [DOI] [PubMed] [Google Scholar]