Abstract
Pet dogs and cats in the USA are commonly exposed to potentially hazardous substances found in domestic environments. Requests for assistance and advice received by the Kansas State Veterinary Diagnostic Laboratory regarding exposures in dogs and cats to substances perceived by their caretakers to be potentially harmful included 1,616 phone calls, over a 3-year period covering 2009–2012. Enquiries occurred more often during summer. Dogs were involved in 84.7 % of calls and cats in 15.3 %. Oral exposures were reported in 95.5 % of calls, dermal exposures in 3.7 % of calls, inhalation exposures in 0.6 % of calls, and parenteral exposures in 0.2 % of calls. Therapeutic drugs were the most frequently reported substances, accounting for 35.4 % of calls, followed by household chemicals (15.5 %); foods (14.8 %); pesticides (13.9 %); plants (12 %), industrial chemicals and fertilizers (3.6 %); cosmetics and personal care products (2.8 %); and animal, insect, and microorganism toxins (2.1 %). Although requests for information or assistance are not a measure of poisoning incidence, it can provide insight regarding relative exposure rates, help to identify changing exposure trends and emerging exposures, and reflect the public concern regarding actual or apparent harmful exposures in pets.
Keywords: Veterinary, Poisoning, Toxicology, Dogs, Cat, Pet
Introduction
The USA has the largest companion animal populations in the world. The most common pets are dogs and cats with more than 72 million pet dogs, and nearly 82 million pet cats. Thirty-nine percent of USA households own at least one dog and about 33 % own at least one cat [1]. The home environment is, arguably, the most important source of toxicological risks to pet dogs and cats. The curious nature of dogs and cats, and their tendency to explore, often put them in accidental contact with potentially harmful substances. The improper use, handling, or storage of hazardous household substances can also increase exposure risk. Changes in the types and relative abundance of hazardous substances in the domestic environment are reflected in the exposures experienced by dogs and cats. There are several reasons for changes in domestic hazardous substance abundance over time. Some chemicals and medications are no longer used or are no longer available; others are introduced or are used more frequently. Pet housing and care practices also change over time, reflecting changes in popular perceptions and caretaker education. It is therefore important to periodically revisit trends in exposures.
Pet caretakers are generally attentive to the health of their animals and become concerned when they observe or suspect exposure to substances they perceive to be harmful. Hence, each day, most poison control centers receive calls from animal caretakers, veterinarians, and other medical or health professionals, who are seeking assistance and advice regarding potentially harmful exposures in animals. Assistance requests therefore reflect a combination of the public concern regarding apparent harmful exposures in pets, as well as the relative abundance of those substances. The purpose of this analysis was to describe reported hazardous substance exposures in dogs and cats, based on calls received by the Kansas State Veterinary Diagnostic Laboratory over a 3-year period from 2009 to 2012.
Materials and Methods
The Toxicology Section of the Kansas State Veterinary Diagnostic Laboratory at the College Of Veterinary Medicine–Kansas State University, provides free telephone consultation services to the general public for inquires related to poisoning in animals. It is not an emergency service. Callers are directed to leave a message in a voice messaging system, and calls are typically answered within one business day. Callers who have poisoning emergencies are directed to contact a local veterinarian or an emergency animal poisoning service. Calls are received from all states of the USA and occasionally from neighboring countries and US Territories. For each received call, data are collected on the exposed species, the substance involved in the suspected or observed exposure, route of exposure, estimated dose or dose range, and observed clinical effects. Only calls related to dogs and cats were included in the analysis. Data were derived from 1,616 calls from July 1, 2009 to June 30, 2012.
Results
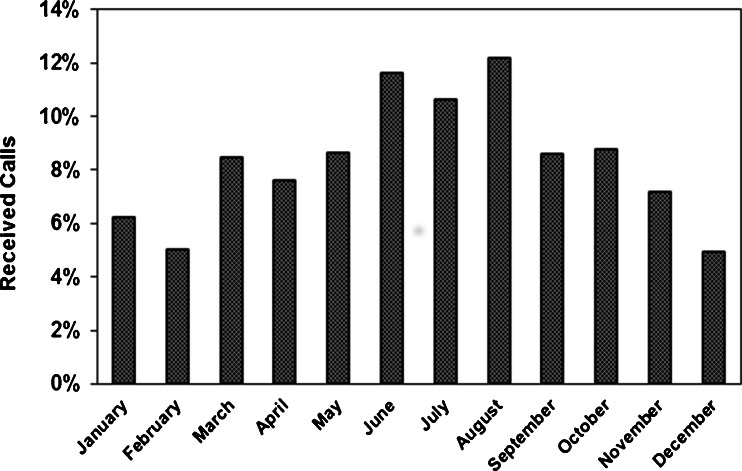
Enquiries involving dogs accounted for 84.7 % of received calls, compared to cats at 15.3 %. Call numbers were lower during winter (December, January, and February), while being higher during the summer (June, July, and August), at 16.2 and 34.5 %, respectively (Fig. 1).
Fig. 1.
Seasonal distribution of animal poison information calls at Kansas State University from 2009 to 2012
Calls were received from all states of the USA. The five states that generated the highest numbers of calls were California (9.7 %), Florida (6.9 %), Illinois (6.6 %), Kansas (6.0 %), and Texas (5.2 %). The lowest call numbers were from North Dakota (0.2 %), Alaska (0.3 %), Hawaii (0.4 %), Idaho (0.4 %), and New Hampshire (0.4 %).
The vast majority of exposures in dogs and cats were via the oral route (95.5 %), followed by dermal (3.7 %), inhalation (0.6 %), and parenteral (0.2 %). Most calls were related to drugs, followed by household products, food, pesticides, plants, and others (Table 1).
Table 1.
Substances reported in animal poison information calls at Kansas State University from 2009 to 2012
| Substance group | Dog (%) | Cat (%) | Total (%) |
|---|---|---|---|
| Drugs | 31.0 | 4.4 | 35.4 |
| Household products | 12.5 | 3.0 | 15.5 |
| Food | 13.0 | 1.7 | 14.8 |
| Pesticides | 11.3 | 2.6 | 13.9 |
| Plants | 9.0 | 3.0 | 12.0 |
| Chemicals and fertilizers | 3.3 | 0.3 | 3.6 |
| Cosmetics and personal care products | 2.5 | 0.3 | 2.8 |
| Animal, insect and microorganism toxins | 2.0 | 0.1 | 2.1 |
| Total | 84.6 | 15.4 | 100 |
Among drugs, human drugs were more commonly involved compared to veterinary drugs, at 91.2 and 8.8 %, respectively. Nonsteroidal anti-inflammatory drugs (NSAIDs), including acetaminophen, ibuprofen, and aspirin, formed the largest group. Parasiticides and insecticides for veterinary use (such as ivermectin and pyrethroids) were the most commonly reported veterinary preparations. Other commonly reported drugs included vitamins, supplements, and minerals group (mainly vitamin D and iron supplements), antimicrobial drugs (antibiotics, sulfonamide, and antifungals), and anxiolytics and antidepressants (Table 2).
Table 2.
Drugs reported in animal poison information calls at Kansas State University from 2009 to 2012
| Druga | Dog (%) | Cat (%) | Total (%) |
|---|---|---|---|
| NSAID and acetaminophen | 17.1 | 3.0 | 20.1 |
| Vitamins, supplements and minerals | 10.0 | 1.9 | 11.9 |
| Antimicrobials | 9.6 | 1.6 | 11.2 |
| Anxiolytics and antidepressants | 5.9 | 0.7 | 6.6 |
| Birth control medications | 5.6 | 0.3 | 5.9 |
| Hormones | 4.5 | 0.9 | 5.4 |
| Tranquilizers and sleep aids | 3.9 | 1.0 | 4.9 |
| Blood pressure medications | 4.3 | 0.2 | 4.5 |
| ADHD medications | 3.6 | 0.3 | 3.9 |
| Anti-histamines | 3.2 | 0.4 | 3.6 |
| Anthelmintics | 3.3 | 0.2 | 3.5 |
| Decongestants | 2.4 | 0.2 | 2.6 |
| Pain relievers and muscle relaxants | 2.6 | 0.4 | 3.0 |
| Diabetes medications | 1.2 | 0.2 | 1.4 |
| Laxatives and antidiarrheals | 1.2 | 0.2 | 1.4 |
| Parkinson's disease medications | 1.2 | 0.0 | 1.2 |
| Local anesthetics | 0.9 | 0.2 | 1.1 |
| Antiseptics and disinfectants | 0.9 | 0.2 | 1.1 |
| Urinary tract medications | 1.0 | 0.0 | 1.0 |
| Bronchodilators | 0.9 | 0.0 | 0.9 |
| Cholesterol lowering agents | 0.5 | 0.2 | 0.7 |
| Others | 3.7 | 0.4 | 4.1 |
| Total | 87.5 | 12.5 | 100 |
aThis group was involved in 35.4 % of all received calls
Chemicals used in the home were reported in 15.5 % of calls. Cleaners such as detergents, bleach, and solvents, were most common, closely followed by automotive products such as antifreeze (ethylene glycol) and gasoline (Table 3).
Table 3.
Household products reported in animal poison information calls at Kansas State University from 2009 to 2012
| Household productsa | Dog (%) | Cat (%) | Total (%) |
|---|---|---|---|
| Cleaners | 27.2 | 7.6 | 34.8 |
| Automotive products | 22.8 | 6.8 | 29.6 |
| Foreign bodies | 19.2 | 4.4 | 23.6 |
| Matches and fireworks | 4.4 | 0.0 | 4.4 |
| Cigarettes and nicotinic | 3.2 | 0.0 | 3.2 |
| Others | 4.0 | 0.4 | 4.4 |
| Total | 80.8 | 19.2 | 100 |
aThis group was involved in 15.5 % of all received calls
Foods were reported in 14.8 % of calls. Chocolate- and cocoa-based products were the most common foods involved, followed by sweeteners (mostly products sweetened with xylitol), onions and garlic, raisins and grapes, nuts, sea food, and alcohol (Table 4).
Table 4.
Common foods reported in animal poison information calls at Kansas State University from 2009 to 2012
| Food typea | Dog (%) | Cat (%) | Total (%) |
|---|---|---|---|
| Chocolate and cocoa products | 33.5 | 4.2 | 37.7 |
| Sweeteners | 17.1 | 2.1 | 19.2 |
| Onions and garlic | 12.6 | 2.9 | 15.5 |
| Raisins and grapes | 9.2 | 1.7 | 10.9 |
| Macadamia nuts and walnuts | 3.3 | 0.4 | 3.7 |
| Almonds | 2.5 | 0.0 | 2.5 |
| Seafood | 1.7 | 0.0 | 1.7 |
| Alcohol | 1.3 | 0.0 | 1.3 |
| Others | 7.1 | 0.4 | 7.5 |
| Total | 88.3 | 11.7 | 100 |
aThis group was involved in 14.8 % of all received calls
Pesticides were reported in 13.9 % of enquiries. Ant and roach baits were the most common pesticides, followed by anticoagulant rodenticides, insecticides, and herbicides (Table 5).
Table 5.
Pesticides reported in animal poison information calls at Kansas State University from 2009 to 2012
| Pesticidea | Dog (%) | Cat (%) | Total (%) |
|---|---|---|---|
| Ant and roach baits | 28.5 | 4.0 | 32.5 |
| Rodenticides | 24.0 | 8.0 | 32.0 |
| Insecticides | 19.1 | 6.2 | 25.3 |
| Herbicides | 9.7 | 0.4 | 10.2 |
| Total | 81.3 | 18.7 | 100 |
aThis group was involved in 13.9 % of all received calls
A wide variety of outdoor and indoor plants were reported. The most common plants were lilies (Liliaceae) (19.5 %), aroids (Araceae) (13.3 %), cycads (8.7 %), golden pothes (7.7 %), various berries (7.2 %), ivy (6.1 %), yew (5.6 %), oleander (5.6 %), avocado (4.1 %), and hibiscus (3.6 %). The remaining 18.6 % of reported plants included marijuana, tomato leaves, asparagus, plums, and apricots. Dogs were involved in 74.9 % of plant reports and cats in 25.1 %.
Industrial chemical products and fertilizers were reported in 3.6 % of calls. Plant fertilizers accounted for 50 % of reports in this category, followed by industrial products (15.5 %), corrosive agents (13.8 %), oxidizers (10.3 %), and others (10.4 %). Dogs were involved in 93.1 % of reports in this category, and cats in 6.9 %.
Cosmetic and personal care products were reported in 2.8 % of calls. This category included skin lotions, hair dyes, lens solution, nail varnish, and others.
Animal, insect and microorganism toxins accounted for 2.0 % of reports. Mycotoxins contributed 24.2 % of reports in this category, followed by spider and snake bites (21.2 %), cyanobacteria (18.2 %), and others.
Discussion
This overview of enquiries to an animal poisoning information service from pet owners and caretakers reflects pet owner concerns regarding exposures to perceived hazards. It provides an indirect indication of the relative incidence of exposures in pet populations. It is influenced by the public perception of what substances are hazardous to pet health. It should not, therefore, be interpreted as a dependable indication of poisoning risk because it does not provide reliable evidence of poisoning. In spite of these limitations, the data do provide a window into important trends in pet exposures to potentially toxic substances.
Dogs were involved in 84.7 % of all enquiries, compared to 15.3 % for cats. This correlates well with similar studies. For example, in a review of phone calls received by the Animal Poison Control Center between 2002 and 2010, it was shown that 76.5 % of calls involved dogs, and 13.1 % involved cats [2]. Data from the Texas Poison Center Network (TPCN) showed that 87 % of reports involved dogs and11% involved cats [3]. The 1993–1994 report of the American Association of Poison Control Centers reported that dogs were involved in 82.8 % of cases and cats in 13.6 % of cases [4]. The predominance of dogs also appears true for countries other than the USA. A retrospective study from Brazil, for example, including exposures from 2002 to 2008, reported that dogs were involved in 86.1 % of exposures and cats in 13.9 % [5]. An earlier Brazilian study, reporting exposures from 1998 to 2002, showed that doges were involved in 81.2 % of exposures and cats in 18.8 % [6]. Based on these statistics, exposure to hazardous substances appear to be more common in dogs than in cats. It is not correlated to pet numbers. There are slightly more pet cats in the USA at an estimated 81.7 million compared to an estimated 72 million dogs [1]. The high proportion of dog reports may be explained by behavioral differences between dogs and cats. Dogs are less selective and more prone to scavenging compared to cats. Cats are more selective and tend to refuse any material that does not present a familiar odor that it associates with food [7].
The increased number of calls in the months of summer may be explained by the fact that pets are more active and spend more time outside during warmer weather, and they are therefore more likely to interact with hazardous substances in the environment. This pattern was consistent with other studies [2, 4].
The geographic origins of enquiries were widespread. The highest number of enquiries by state was from California and the lowest from North Dakota. It was not correlated with population density or proximity to Kansas. The information service is not actively advertised or promoted in any region, and the spatial pattern remains difficult to explain, but could be related to the relative availability of alternative services, or indirect marketing by local third parties such as veterinary practices and pet care services.
The high proportion of enquiries reporting oral exposures (95.5 %) was consistent with other studies, such as Forrester and Stanley in 2004[3], where 95 % of exposures were via ingestion. Human medications were the most important sources of exposure to hazardous substances in dogs and cats. Since 2002, human medications have consistently been responsible for most poisonings in pets in the USA and elsewhere [2, 5, 6, 8]. NSAIDs were the most commonly reported medications. NSAIDs, including multiple products that are available without prescription, are extensively used for pain and inflammation management. The high rates of pet exposures to the other types of medications, such as anxiolytics and antidepressants, hormones, blood pressure medications, sedatives and sleep aids, as well as dietary supplements such as vitamins, minerals, and amino acids, are also likely to be related to their widespread use. These data compare well to exposures reported to the ASPCA Animal Poison Control Center during 2009, which indicated that the most common human pharmaceuticals involved were acetaminophen (5.10 %), ibuprofen (2.08 %), vitamin D (1.31 %), loratidine (1.28 %), lisinopril (1.26 %), aspirin (1.21 %), and iron (1.05 %) [2]. Similarly, data collected from the Texas Poison Center Network indicated that analgesics, antimicrobials, topical preparations, and hormones accounted for 4.3, 3.7, 2.9, and 2.4 % of calls, respectively[3].
Many common household items can be hazardous to dogs and cats including cleaning solutions, bleach, automotive products, and hydrocarbons (such as solid fuel, gasoline, and solvents used in paints). Household products were the second most frequently reported at a rate of 15.5 % of enquiries. Similar trends were observed in other studies [3, 8–10].
Several human foods, while safe for humans, may be hazardous to pets. Chocolate- and cocoa-based products were the most commonly reported hazardous foods, followed by products sweetened with xylitol, onions and garlic, grapes and raisins, and macadamia nuts. These findings were variable among similar investigations.
Pesticides accounted for a substantial fraction of calls at 13.9 %. Insecticides were the most frequently reported pesticides, with ant and roach baits being the most common formulations. This may be explained by the widespread use of these products, the inclusion of attractants, such as peanut butter and sweetening substances, and the typical placement of such bait stations at floor level where they are easily reached by pets. Common active ingredients in ant and roach baits include avermectins, bendiocarb, boric acid, chlorpyrifos, fipronil, hydramethylnon, propoxur, sodium borate, and sulfluramid. Ingestions of toxic doses of these compounds via ant and roach baits are, however, not common [11]. Other reported pesticides included anticoagulants, bromethalin-based rodenticides, and herbicides. The most common exposures to toxic doses of pesticides are typically associated with pyrethrins/pyrethroids, carbamates, and organophosphates, due to their widespread use and potency [8, 12]. The results of this study cannot be used directly for comparison because poisoning could not be confirmed. Pesticides were, however, reported at higher relative rates in other studies. For example, the ASPCA Animal Poison Control Center reported that 25.51 % of calls during 2009 involved pesticides. Similarly, the Texas Poison Center Network reported that 29.6 % of calls involved pesticides during 1998–2002 [3] and the same rate (29.6 % of 41,854 calls involving dogs and cats) was reported by the American Association of Poison Control Centers (AAPCC)in the USA during 1990 [13]. A study conducted in Italy reported that pesticides were involved in 39–63 % of calls to a Poison Control Centre in Milan between 2000 and 2010 [8].
Plants were reported in 12 % of enquiries. A similar fraction (11.6 %) was reported for calls received by the ASPCA Animal Poison Center [14], while the AAPCC reported that 12.1 % of inquiries involved plants [15]. Liliaceae spp. was the most frequently reported plants, followed by Araceae spp., cycads, and more than 20 others. Lilium spp. and Hemerocallis spp. were found to be the most common plants reported to the AAPCC in 2010 followed by Spathiphyllum spp. and Cycas revolute [2, 16]. The ASPCA Animal Poison Center at the University of Illinois reported more than 70 different species of plants, involved in 2199 of received calls [14]. In France, Liliacae spp. and Aracae spp. were the two major plant families reported [12], while in Italy, Dieffenbachia spp. Ficus benjamina, Nerium oleander, and Lilium spp. were the most commonly reported plants [8].
Fertilizers, cosmetic products, microbial and zootoxins, and other miscellaneous chemicals accounted for 9 % enquiries. Similar rates of exposure to these compounds have been reported by many peer studies. For instance, TPCN reported a relative rate of 2.7 % for cosmetic products [3] and the AAPCC recorded 2.2 % of inquiries related to fertilizers [15].
In conclusion, requests for assistance and information at the Toxicology Section of the Kansas State Veterinary Diagnostic Laboratory revealed that dogs and cats are exposed to a wide range of potentially hazardous substances, with exposures to human medications being the most common. Human medications are therefore a highly significant source of toxicological risk to pets, in addition to classic veterinary toxicants such as pesticides, household chemical products, and plants. The detection of such trends are helpful in guiding the training and continuing education of veterinarians, veterinary technicians, and others involved in preventing and treating poisoning in companion animals. Companion animal exposure data also provides an indirect indication of hazardous substance use patterns by people in domestic settings, and reflect general public perceptions on what substances found in domestic settings are regarded as hazardous.
Acknowledgments
Conflict of Interest
There is no conflict of interest to report.
References
- 1.American Veterinary Medical Association (2007) All pets. In: US pet ownership and demographics sourcebook. Schaumburg: American Veterinary Medical Association. pp 7–32
- 2.McLean MK, Hansen SR. An overview of trends in animal poisoning cases in the United States: 2002–2010. Vet Clin North Am Small Anim Pract. 2012;42(2):219–228. doi: 10.1016/j.cvsm.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 3.Forrester MB, Stanley SK. Patterns of animal poisonings reported to the Texas Poison Center Network: 1998–2002. Vet Hum Toxicol. 2004;46(2):96–99. [PubMed] [Google Scholar]
- 4.Hornfeldt CS, Murphy MJ. Poisonings of animals: the 1993–1994 report of the American Association of Poison Control Centers. Vet Hum Toxicol. 1997;39(6):361–365. [PubMed] [Google Scholar]
- 5.Medeiros RJ, Monteiro FO, Silva GCD, Nascimento JA. Poisoning dogs and cats attended in the Veterinarian College of Federal Fluminense University during the period of 2002 to 2008. Cienc Rural. 2009;39(7):2105–2110. doi: 10.1590/S0103-84782009005000151. [DOI] [Google Scholar]
- 6.Xavier FG, Kogika MM, De S. Common causes of poisoning in dogs and cats in a Brazilian veterinary teaching hospital from 1998 to 2000. Vet Hum Toxicol. 2002;44(2):115–116. [PubMed] [Google Scholar]
- 7.Nutrient requirements of dogs and cats. New York: National Academies Press; 2006. pp. 22–26. [Google Scholar]
- 8.Caloni F, Cortinovis C, Rivolta M, Davanzo F (2102) Animal poisoning in Italy: 10 years of epidemiological data from the Poison Control Centre of Milan. Vet Rec 170(16): 415 [DOI] [PubMed]
- 9.Vandenbroucke V, Van Pelt H, De Backer P, Croubels S. Animal poisonings in Belgium: a review of the past decade. Vlaams Diergeneeskundig Tijdschrift. 2010;79(4):259–268. [Google Scholar]
- 10.Barbier N (2005) Annual Review of Toxicological Information /Centre Nacional of Veterinarians for 2003. PhD Thesis, Veterinary Lyon: p:220
- 11.Antox [database] (2005) Urbana, Ill: American Society for the Prevention of Cruelty to Animals National Animal Poison Control Center. Accessed 2005
- 12.Berny P, Caloni F, Croubels S, Sachana M, Vandenbroucke V, Davanzo F, Guitart R. Animal poisoning in Europe. Part 2: Companion animals. Vet J. 2010;183(3):255–259. doi: 10.1016/j.tvjl.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 13.Murphy MJ. Toxin exposure in dogs and cats: drugs and household products. J Am Vet Med Assoc. 1994;205(4):557–560. [PubMed] [Google Scholar]
- 14.Haliurton JC, Buck WB. Animal Poison Control Center summary of telephone inquiries during first three years of service. J Am Vet Med Assoc. 1983;182:514–515. [PubMed] [Google Scholar]
- 15.Hornfeldt CS, Murphy MJ. 1990 Report of the American Association of Poison Control Centers: poisoning in animals. J Am Vet Med Assoc. 1992;200(8):1077–1080. [PubMed] [Google Scholar]
- 16.Slater MR, Gwqltney-Brant S. Exposure circumstances and outcomes of 48 households with 57 cats exposed to toxic lily species. J Am Anim Hosp Assoc. 2011;47(6):386–390. doi: 10.5326/JAAHA-MS-5629. [DOI] [PubMed] [Google Scholar]