Abstract
Paraquat, a widely used herbicide in the world, has caused severe and fatal poisonings. Because of its high toxicity, the European Union withdrew paraquat from its market in July 2007. The purpose of this report is to describe cases of paraquat poisoning recorded at the Poison Control Center in Marseille over the 9-year period starting and ending 4.5 years before and after the paraquat ban. Data analysis showed that the most severe exposures were linked to ingestion. The fatality rate of deliberate consumption was near 50 % (34 suicide attempts and 15 deaths). Our data showed a marginal decline in total number of poisonings observed after the paraquat ban (38 vs 33 after the ban) mostly due to a decrease in the number of unintentional exposure (21 vs 16 after the ban). However, there was no apparent change in the number suicidal attempts using paraquat. Regarding geographical distribution, data showed that most poisonings in mainland France were unintentional, while poisonings in overseas French territories were mostly voluntary. Despite the European ban and the preventive measures, paraquat continues to contribute to severe and life-threatening poisonings in Southeastern and overseas France.
Keywords: Paraquat, Herbicide, Intoxication, Multivisceral failure, Pulmonary fibrosis, Poison center
Introduction
Paraquat is the trade name for 1,1′-dimethyl-4,4′-bipyridylium that was developed in the early 1960s by Imperial Chemical Industries, now Syngenta. It is a commonly used contact herbicide because of its wide range of action and low cost. However, this is an extremely hazardous substance, and there is no effective treatment for systemic toxicity [1]. Indeed, paraquat can cause multiple organ failure, including liver insufficiency and lung fibrosis that can be life-threatening because of respiratory failure [2, 3]. The risk of acute paraquat poisoning has triggered much debate since its market release in 1962. A number of risk mitigation measures were introduced to prevent poisoning; stenching agents, blue-green dye, thickeners, and emetics were added; the concentration of paraquat was reduced to 10 %; paraquat bottles had been equipped with safety caps; labeling requirements had been changed; packaging and availability were restricted to professional users [4, 5]. In July 2007, in view of continued occurrence of paraquat poisoning, the European Union judged mitigation measures as inadequate and finally decided to ban the sale of paraquat completely [6]. Despite this ban, involuntary and deliberate poisonings have continued to occur. Self-poisoning with pesticides is a topical issue and the subject of several publications in the medical literature. It seems that a complete ban on the most hazardous products is not always enough [7, 8]. The purpose of this report is to describe the experience of the Marseille Poison Control Center (MPCC) with paraquat poisoning over a period starting and ending 4.5 years before and after the European Union paraquat ban.
Method
The cases of paraquat poisoning in this study were compiled from the records of the MPCC for the inclusive years between 2003 and 2011. Data were extracted from the Information Network of the French Poison Control Centers. The Marseille database was searched for cases involving exposure to products coded as “paraquat” including the following trade names: Gramoxone®, R-Bix®, and Gramoxone Plus®. Data analysis focused on the time and location of the poisoning as well as circumstances (unintentional or voluntary, based on the patient’s statement) and outcome.
The MPCC covers the southeastern part of France, including three regions of mainland France (Provence-Côte-d’Azur, Languedoc-Roussillon, and Corsica) as well as overseas French territories (OFT) in the Indian Ocean (Reunion Island and Mayotte). In addition, the MPCC maintains a regular working relationship with Americas French departments including several hospitals in French Guiana. The MPCC’s catchment area includes approximately nine million people, i.e., 14 % of French population. Based on these coverage limitations, it is expressly stated that the data presented herein correspond to the experience of a local poison control center and cannot be considered as representative of national epidemiologic patterns in France. MPCC records approximately 25,000 intoxications per year including about 1,000 poisonings linked to plant products and 2,500 suicide attempts. An average of 3 % of the MPCC’s calls is from OFT.
Results
During the period from 2003 to 2011, the overall rate of suicide attempts per year from pesticides reported to MPCC remained unchanged (approximately 65). In the studied period, the MPCC recorded a total of 71 cases of paraquat poisonings (0.03 % of all calls reported at the MPCC per year and 6 % of the annual deaths). The number of cases reported before and after the ban was 38 and 33, respectively. The table shows paraquat poisonings reported to the MPCC during the study period by geographic area, nature of the exposure, and number of deaths.
At the MPCC, 37 poisonings by unintentional exposure were reported from 2003 to 2011. The location of the exposure varied among the cases, including workplace in 16 (nine before and eight after the ban), garden in 7 (six before and one after the ban), and undetermined in 13. The route of exposure was ingestion in 14 cases, dermal contact in 10, and eye contact in 8. Unintentional poisonings commonly occurred during the preparation or application of the herbicide solution. In one case, the exposure was subcutaneous, while the product was being handled in an experimental laboratory. The unintentional ingestions occurred during the preparation of the product for use: opening the herbicide package, using the mouth to blow air through the spray nozzle to clear it, or using teeth to twist off the bottle caps. All cases with unintentional poisonings in this series had minor toxicity.
All fatal paraquat poisonings, recorded between 2003 and 2011, were due to deliberate ingestion at home (five unknown location cases) with suicidal intention based on the patient’s history. Almost 50 % of the attempted suicides using paraquat (15/34) led to death of the victim. In this series, 66 % of deaths occurred rapidly, i.e., within the first 48 h after ingestion, due to multiple system organ failure or refractory hypotension. The remaining 33 % of deaths occurred late, i.e., within the first month; they were due to extensive pulmonary fibrosis and intractable hypoxemia. The likely explanation for survivors from intentional ingestions of paraquat was that the quantity ingested was minimal.
The table shows several differences in the geographical distribution of poisonings before and after the paraquat ban (Table 1). Prior to the ban, MPCC recorded a similar number of overall cases for mainland France and OFT. After the ban, the number of cases in mainland France appeared to have decreased unlike in OFT. The slight decrease in the number of cases following the ban appeared to have been due to decreased unintentional poisoning in mainland France, especially during gardening (five before and one after the ban). In OFT where most exposures involved deliberate ingestions, no apparent decrease in the number of paraquat poisonings was observed. Moreover during the study period, 3 deaths in mainland area and 12 deaths in overseas areas were reported in MPCC. Further study of these geographical differences showed that the impact of the paraquat ban also appeared to vary according to location at OFT. On Reunion Island in the Indian Ocean, the number of paraquat poisonings went from ten cases including eight deliberate ingestions before the ban to one after the ban. French Guiana in South America showed an increase in the number of paraquat poisonings from 6 including 5 deliberate ingestions before the ban to 14 including 11 deliberate ingestions after the ban. In French Polynesia, the number of cases showed little change, i.e., four poisonings including three deliberate ingestions before the ban versus six including two deliberate ingestions after the ban.
Table 1.
Cases of paraquat poisoning reported to MPCC before and after the European Union ban in July 2007
| Poisonings by paraquat reported in MPCC | Mainland France | OFT | ||
|---|---|---|---|---|
| Unintentional | Voluntary | Unintentional | Voluntary | |
| From 1 January 2003 to 30 June 2007 | 18 | 20 | ||
| 17 | 1 (1 death) | 4 | 16 (8 deaths) | |
| From 1 July 2007 to 31 December 2011 | 11 | 22 | ||
| 8 | 3 (2 deaths) | 8 | 14 (4 deaths) | |
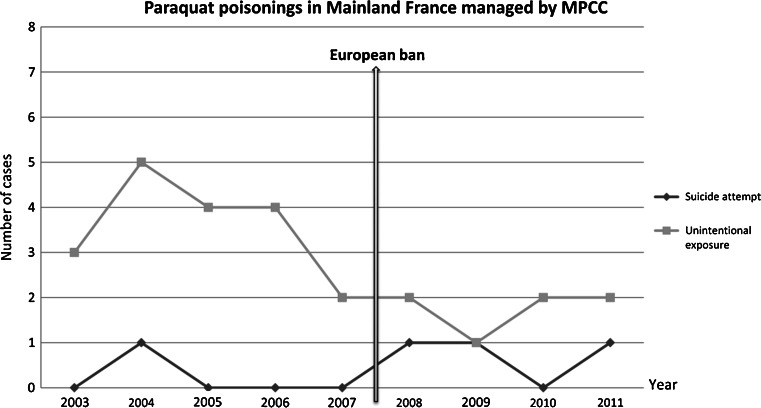
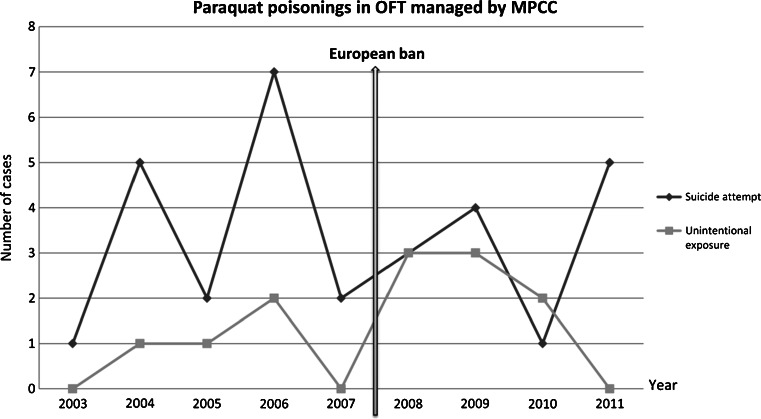
Figures 1 and 2 show details of paraquat poisonings per year, in mainland and in overseas, respectively. The first graph (Fig. 1) shows an apparent small decrease in cases of unintentional exposure after the European ban. Contrary to this finding, the cases of intentional ingestions of paraquat did not change during the same period. Overall, it appears that there were more unintentional poisonings than intentional poisonings in mainland France. The second graph (Fig. 2) demonstrates large variability in rates of suicide attempts and unintentional exposures. The ban in July 2007 seems not to have an impact in paraquat exposures in OFT where the most frequent cases were intentional exposures.
Fig. 1.
Cases of paraquat poisoning in mainland France reported to MPCC before and after the European Union ban in July 2007
Fig. 2.
Cases of paraquat poisoning in overseas France territories reported to MPCC before and after the European Union ban in July 2007
Discussion
Our results showed an apparent decrease in unintentional exposures to paraquat in mainland France, during the ban. However, the suicide rate did not change and remained low. In OFT, the proportion of suicide attempts from paraquat poisoning appeared to be higher than that in mainland France, and this difference remained unchanged after the ban. Hypotheses can be proposed to explain this difference between the two locations.
One hypothesis is the increased availability of paraquat in OFT compared to mainland France. The tropical or equatorial climate in OFT contributes to an abundance of flora, which promotes the use of herbicides to control their growth. Furthermore, the increased dependence of the local economy on agriculture at OFT compared to mainland France can place a high proportion of the population in direct contact with herbicides at OFT. Chang and colleagues [7] showed that trends in pesticide suicide in Taiwan were influenced by the access to pesticides with the size of agricultural workforce. Because paraquat is efficient and economical, it is considered by the local population as a “perfect” product which cannot be replaced by other ones. One of the consequences of this situation is the use of paraquat not only by professionals but also by the general population. Since the European paraquat ban, the geographical situation of OFT, like French Guiana (proximity with neighboring countries like Suriname or Brazil where paraquat use is authorized), has enabled people to cross the border to purchase paraquat and illegally bring it back to OFT. This unauthorized practice is suggested by the presence of foreign labels (Portuguese and Dutch) on paraquat bottles reported to MPCC from French Guiana between 2008 and 2011.
Another hypothesis is the increased publicity of deaths from paraquat poisoning in OFT compared to mainland France. For example, a series of sensationalist articles were published in 1980 in local newspapers about the deadly effects of paraquat poisonings. These articles could have inadvertently called attention to paraquat as a highly effective method for suicide [5]. This is a perverse consequence from the sharing of information that poison centers were able to avoid in mainland area, owing to the understanding and cooperation of journalists.
Limitations
The findings from this study are limited by several factors. This study should not be considered as an exhaustive evaluation of paraquat poisonings in France because it is based on reports from one poison center. Furthermore, data were collected using a retrospective design and from voluntary medical reports; thus, there can be reporting bias in the study. For example, the increased proportion of suicide poisonings from paraquat in OFT compared to mainland France can be due to the practice of preferential reporting of cases with severe poisoning to poison centers in mainland France. The time difference between the two locations, cost of telephone communications, and request for additional medical consultation can support this pattern of practice. In addition, the date of the ban used in this study only served as an index of the change in policy. The local population could have started to change their use of paraquat prior to this date.
Conclusion
We conclude that paraquat continues to contribute to severe poisonings in our catchment area in France despite the European ban and recommend that national poison control centers retain responsibility for monitoring paraquat poisonings.
Contributor Information
Morgane Kervégant, Phone: +33-4-91752525.
Corinne Schmitt, Email: corinne.schmitt@ap-hm.fr.
References
- 1.Gawarammana IB, Buckley NA. Medical management of paraquat ingestion. Br J Clin Pharmacol. 2011;72(5):745–57. doi: 10.1111/j.1365-2125.2011.04026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bismuth C, Garnier R, Baud FJ, Muszynski J, Keyes C. Paraquat poisoning. An overview of the current status. Drug Saf. 1990;5(4):243–51. doi: 10.2165/00002018-199005040-00002. [DOI] [PubMed] [Google Scholar]
- 3.Sittipunt C. Paraquat poisoning. Respir Care. 2005;50(3):383–5. [PubMed] [Google Scholar]
- 4.Sénat (2009) Impacts de l’utilisation de la chlordécone et des pesticides aux Antilles: bilan et perspectives d’évolution. Available from http://www.senat.fr/rap/r08-487/r08-487.html. Accessed in September 28 2012.
- 5.Comité de Coordination de Toxicovigilance (2007) Intoxications par des préparations herbicides contenant du paraquat. Available from http://www.centres-antipoison.net/cctv/rapport_cctv_paraquat_2007.pdf. Accessed in September 28 2012.
- 6.EUR-Lex (2007) Judgment of the Court of First Instance: European Directive 91/414/EEC case T-229/04. Available from http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:62004TJ0229:EN:NOT. Accessed in September 28 2012.
- 7.Chang SS, Lu TH, Eddleston M, Konradsen F, Sterne JA, Lin JJ, et al. Factors associated with the decline in suicide by pesticide poisoning in Taiwan: a time trend analysis, 1987–2010. Clin Toxicol (Phila) 2012;50(6):471–480. doi: 10.3109/15563650.2012.688835. [DOI] [PubMed] [Google Scholar]
- 8.Eddleston M, Adhikari S, Egodage S, Ranganath H, Mohamed F, Manuweera G, et al. Effects of a provincial ban of two toxic organophosphorus insecticides on pesticide poisoning hospital admissions. Clin Toxicol (Phila) 2012;50(3):202–209. doi: 10.3109/15563650.2012.660573. [DOI] [PMC free article] [PubMed] [Google Scholar]