Abstract
Purpose
It is well known that arthrodesis is associated with adjacent segment degeneration (ASD). However, previous studies were performed with simple radiography or CT. MRI is most sensitive in assessing the degenerative change of a disc, and this is the first study about ASD by radiography, CT and MRI. We sought to factors related to ASD at cervical spine by an MRI and CT, after anterior cervical spine surgery.
Materials and methods
This is a retrospective cross-sectional study of cervical disc herniation. Patients of cervical disc herniation with only radiculopathy were treated with either arthroplasty (22 patients) or ACDF with cage alone (21 patients). These patients were required to undergo MRI, CT and radiography preoperatively, as well as radiography follow-up for 3 months and 1 year, and we conducted a cross-sectional study by MRI, CT and radiography including clinical evaluations 5 years after. Clinical outcomes were assessed using VAS and NDI. The fusion rate and ASD rate, and radiologic parameters (cervical lordosis, operated segmental height, C2-7 ROM, operated segmental ROM, upper segmental ROM and lower segmental ROM) were measured.
Results
The study groups were demographically similar, and substantial improvements in VAS (for arm) and NDI (for neck) scores were noted, and there were no significant differences between groups. Fusion rates were 95.2 % in the fusion group and 4.5 % in the arthroplasty group. ASD rates of the fusion and arthroplasty groups were 42.9 and 50 %, respectively. Among the radiologic parameters, operated segmental height and operated segmental ROM significantly decreased, while the upper segmental ROM significantly increased in the fusion group. In a comparative study between patients with ASD and without ASD, the clinical results were found to be similar, although preexisting ASD and other segment degeneration were significantly higher in the ASD group. C2-7 ROM was significantly decreased in ASD group, and other radiologic parameters have no significant differences between groups.
Conclusion
The ASD rate of 46.5 % after ACDF or arthroplasty, and arthroplasty did not significantly lower the rate of ASD. ASD occurred in patients who had preexisting ASD and in patients who also had other segment degeneration. ASD may be associated with a natural history of cervical spondylosis rather than arthrodesis.
Keywords: Adjacent segment degeneration, ACDF, Arthroplasty, Spondylosis
Introduction
From long-term experiences of performing lumbosacral fusions on younger patients especially diagnosed with idiopathic scoliosis, increasing adjacent segment degeneration (ASD) at the segment adjacent to fusion has been noticed. Biomechanical studies of lumbar spine demonstrate increased facet load, segmental motion and intradiscal pressure at the segment adjacent to fusion where the fusion was performed and these changes are associated with ASD [1–4]. In the cervical spine, biomechanical characteristics are different from those of lumbar spine. Most cervical fusions are performed from C3 to C7, and these segments are bordered by a highly mobile upper cervical region, which was responsible for approximately half of all cervical motion [5]. These unique characteristics allow ASD in cervical spine to differ from that of lumbar spine.
Anterior cervical discectomy and fusion (ACDF) has been reported to provide >90 % relief of radicular complaints and thus has become a represented treatment for cervical disc herniation. Yet, previous studies have reported cases of ASD after ACDF [5, 6]. ASD rates varied from 25 to 92 % during a long follow-up period [1, 7–11]. However, previous studies on ASD were done only using radiography or CT. MRI is most sensitive in assessing the degenerative change of a disc, and this is the first study to investigate the incidence and prevalence of adjacent segment disease by radiography, CT and MRI at cervical spine.
“Adjacent segment degeneration (ASD)” and “adjacent segment disease” are used to define different types of radiographic disc degeneration adjacent to the level of spine arthrodesis. The term “adjacent segment degeneration (ASD)” is defined as changes at levels adjacent to fusion on radiographic studies; by contrast, “adjacent segment disease” is defined as new clinical findings that correspond to radiographic signs of adjacent segment degeneration (ASD) [5]. ASD is a prerequisite of “adjacent segment disease”. Here, we focused on ASD without clinical symptoms.
Cervical disc arthroplasty had been invented to maintain anatomical disc space height, normal segmental lordosis and physiological motion pattern after surgeries, and these characteristics may reduce or delay the onset of ASD in comparison with ACDF [12–14]. According to recent studies, some investigators have questioned whether arthroplasty would have a long-term success compared to the ACDF, and they recommended for arthroplasty because arthroplasty yields a lower incidence of ASD than ACDF [11, 12, 15]. However, these studies also were performed using only radiography. The objective of this study is to figure out the factors related to adjacent segment degeneration (ASD) after treated with ACDF or arthroplasty with a five-year follow-up of MRI, CT and radiography.
Materials and methods
Subjects and study design
This retrospective and cross-sectional study was undertaken to target patients who were diagnosed with radiculopathy due to single-level cervical disc herniation by surgical methods. Only radiculopathy patients were included to exclude cases of more severe spondylotic characteristics of myelopathy. To conduct a cross-sectional study using results from MRI, CT and radiography postoperatively 5 years from June 2011 to November 2011, we retrospectively gathered patients who were treated by one surgeon (K. S. Kim) with either arthroplasty; Arthroplasty Group (ProDisc-C, Synthes Spine, West Chester, PA), or ACDF with polyetheretherketone (PEEK) cage with iliac crest autograft bone; Fusion Group (Solis cage, Stryker Spine, Allendale, NJ and ostaPek cage, coLinge AG, Zurich, Switzerland) from June 2005 to May 2006. To exclude the plate effect on ASD, we only chose the ACDF with PEEK cage alone [16, 17], and patients who undertook operation from C4 to C7 were chosen. There were 28 patients of arthroplasty group and 26 patients of fusion group. Among 28 patient of arthroplasty group, only 22 patients were included in this study and six patients were excluded due to various reasons (three; cannot contact, three; reject due to distance from residence). Furthermore, among 26 patients of fusion group, 21 patients were included in this study and five patients were also excluded due to various reasons (three; cannot contact, two; reject due to distance from residence). This study was approved by the institutional review board of Gangnam Severance Hospital, Yonsei University College of Medicine (No 3-2010-0254).
Outcomes assessment
Arm pain and neck pain were assessed using Visual Analogue Scale (VAS) and Neck Disability Index (NDI), respectively. Patients were required to undergo cervical MRI, CT and radiography preoperatively, as well as serial radiography follow-up for 3 months, 1 year postoperatively. Specially, from June 2011 to November 2011, we performed a cross-sectional study using results from MRI, CT and radiography conducted postoperatively for 5 years. Fusion rate and ASD rate with final CT and MRI, and radiologic parameters (cervical lordosis, operated segmental height, C2-7 ROM, operated segmental ROM, upper segmental ROM and lower segmental ROM) were collected during each follow-up examination. All radiologic outcomes were reviewed by an independent spine surgeon and a radiologist, who was unaware of the treatment details.
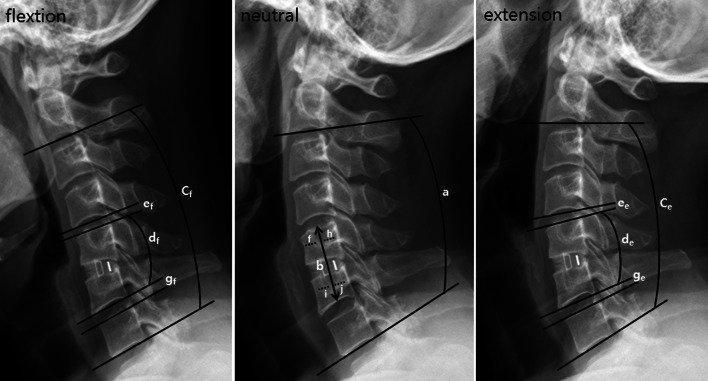
Fusion rates were assessed using the Bridwell grading system with final CT, and only grade I was defined as fusion [18]. To assess ASD, we used two kinds of criteria. One was modified hilibrand criteria with radiography [1], and the other was with MRI and CT. We defined ASD as all kinds of degenerative changes (e.g. posterior osteophyte, decrease disc height ≥25 %, disc signal change, disc herniation, ALL and PLL calcification) at final MRI and CT than preoperative MRI and CT [11]. Various measurements were performed on lateral view of cervical spine radiographs in the neutral and dynamic flexion–extension lateral radiographs obtained at each study point. Cervical lordosis was measured in neutral position between C2 lower endplate and C7 lower endplate using Cobb technique (a) (Fig. 1). Operated segmental height was measured along the line passing through the centre of the vertebral bodies above and below the segments to be operated (b) (Fig. 1). C2-7 ROM (between C2 lower endplate and C7 lower endplate) (cf-ce), operated segmental ROM (between upper endplate of cranial vertebral body and lower endplate of caudal vertebral body) (df-de), upper segmental ROM (between lower endplate and upper endplate of upper adjacent segment disc) (ef-ee) and lower segmental ROM (between lower endplate and upper endplate of lower adjacent segment) (gf-ge) were measured on dynamic lateral radiographs using the Cobb technique (Fig. 1). All radiologic parameters were evaluated with the PACS software and a PACS workstation (Centricity 2.0, General Electrics Medical Systems, Milwaukee, WI).
Fig. 1.
Radiographic measurements. Cervical lordosis was measured in neutral position between C2 lower endplate and C7 lower endplate using Cobb technique (a). Operated segmental height was measured along the line passing through the centre of the vertebral bodies above and below the segments to be operated (b). Length of segment f = h and i = j. C2-7 ROM (between C2 lower endplate and C7 lower endplate) (cf-ce), operated segmental ROM (between upper endplate of cranial vertebral body and lower endplate of caudal vertebral body at operated segment) (df-de), upper segmental ROM (between lower endplate and upper endplate of upper adjacent segment disc) (ef-ee) and lower segmental ROM (between lower endplate and upper endplate of lower adjacent segment) (gf-ge) were measured on dynamic lateral radiographs using the Cobb technique
Statistical methods
Statistical comparisons were primarily based on the observed and recorded follow-up data. SPSS for Windows (version 15.0 K; SPSS, Chicago, IL) was used for the analysis. For statistical comparisons between the groups, chi-square test and Mann–Whitney U test and for intergroup comparisons between preoperative state and postoperative 5 years, Wilcoxon signed-ranks test were used. To know correlations of ASD, spearman and Kendall’s tau bivariate correlation test was used. P values of <0.05 were considered significant.
Source of funding
The funding source for the present study was from Synthes Korea.
Results
Patients demographic characteristics
Between fusion group (21 patients) and arthroplasty group (22 patients), there were no significant differences in the mean age (44.3 vs. 39.9 years) and in the mean follow-up period (64.2 vs. 60.3 months) (Table 1). Operation segments were, respectively, C4/5 = 3:5, C5/6 = 14:13 and C6/7 = 4:4, and no significant difference was present between fusion and arthroplasty groups.
Table 1.
Demographic data and ASD rate
| No. of cases | Mean age (years) | Male/Female | Mean F/U (months) | ASD by X-ray | ASD by MRI and CT | |
|---|---|---|---|---|---|---|
| Total | 43 | 42.1 ± 10.1 | 30/13 | 62.2 ± 8.6 | 5 (11.5 %) | 20 (46.5 %) |
| Fusion with cage | 21 | 44.3 ± 12.1 | 11/10 | 64.2 ± 10.2 | 3 (14.3 %) | 9 (42.9 %) |
| Arthroplasty | 22 | 39.9 ± 7.3 | 19/3 | 60.3 ± 6.4 | 2 (9.1 %) | 11 (50.0 %) |
ASD adjacent segment disease
Adjacent segment degeneration (ASD) rates
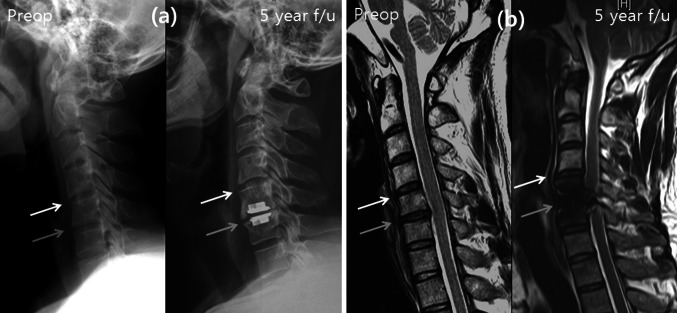
With modified hilibrand criteria with X-ray [1], ASD rates were 11.5 % (5/43), and there was no difference between fusion and arthroplasty group (14.3 % vs. 9.1 %) (Table 1). ASD rates evaluated with MRI and CT were higher than X-ray evaluation, and ASD rate by MRI and CT was 46.5 % on total, and also there was no significant difference between fusion and arthroplasty group (42.9 % vs. 50 %) (Figs. 2, 3; Table 1).
Fig. 2.
Radiography and MRI of ACDF patient at preoperative and 5-year follow-up. Grey arrow indicates operation site, and white arrow indicates upper adjacent segment. At X-ray, there was no significant disc space narrowing and posterior osteophytes (a), but there was disc herniation at upper adjacent segment at MRI (b)
Fig. 3.
Radiography and MRI of arthroplasty patient at preoperative and 5-year follow-up. Grey arrow indicates operation site, and white arrow indicates upper adjacent segment. At X-ray, there was no significant disc space narrowing and posterior osteophytes (a), but there was a disc herniation and signal change at upper adjacent segment at MRI (b)
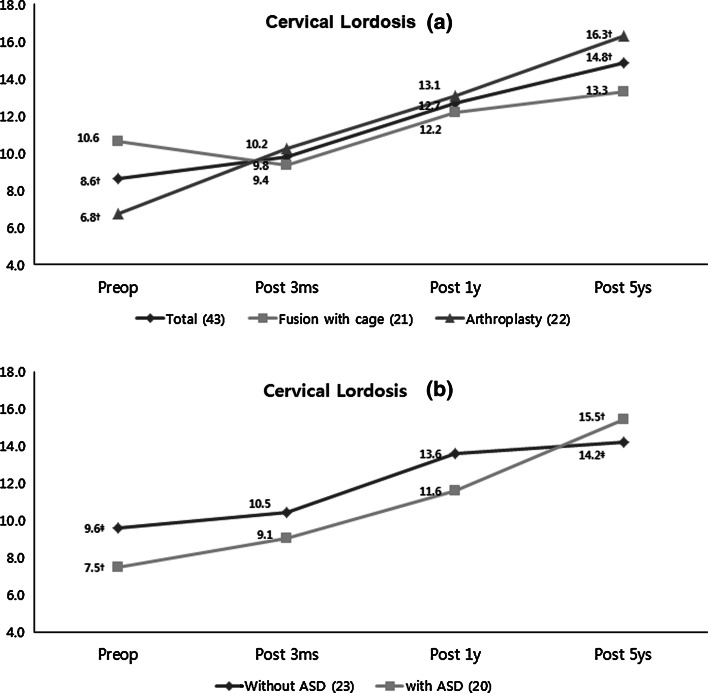
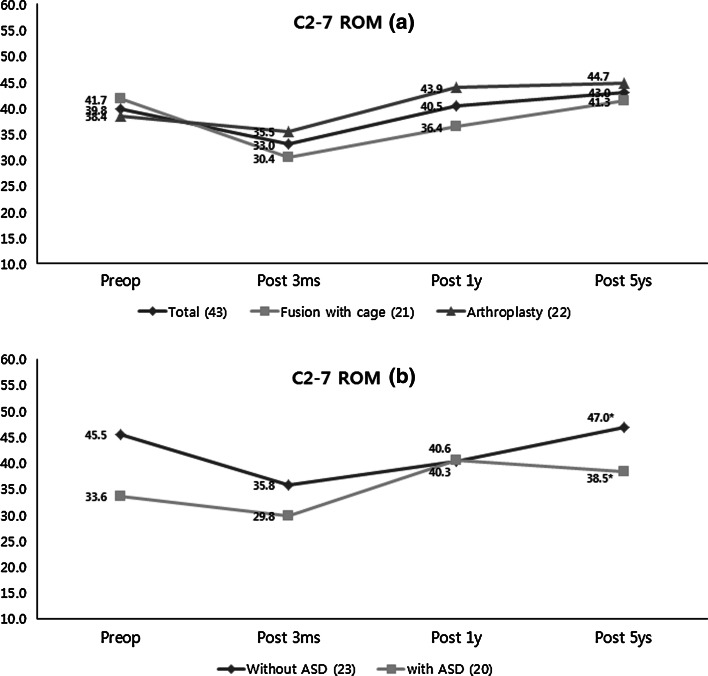
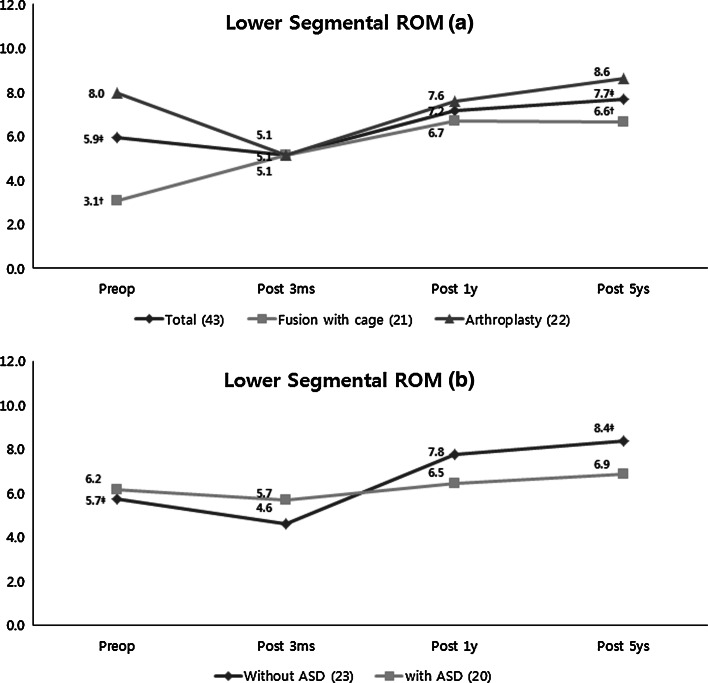
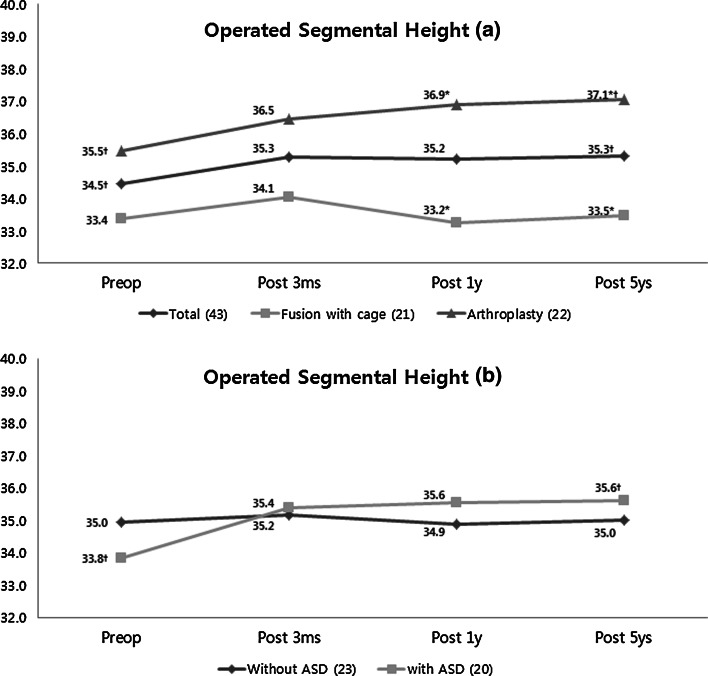
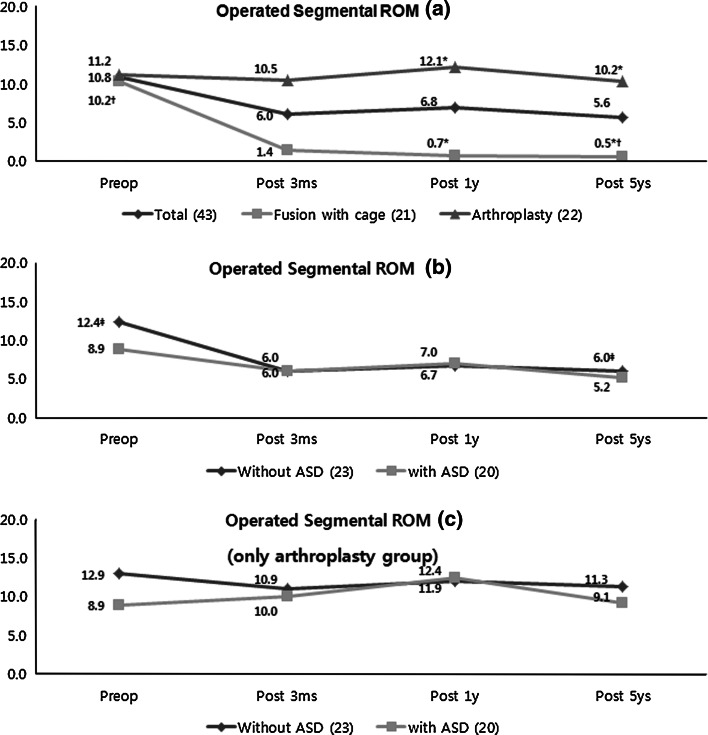
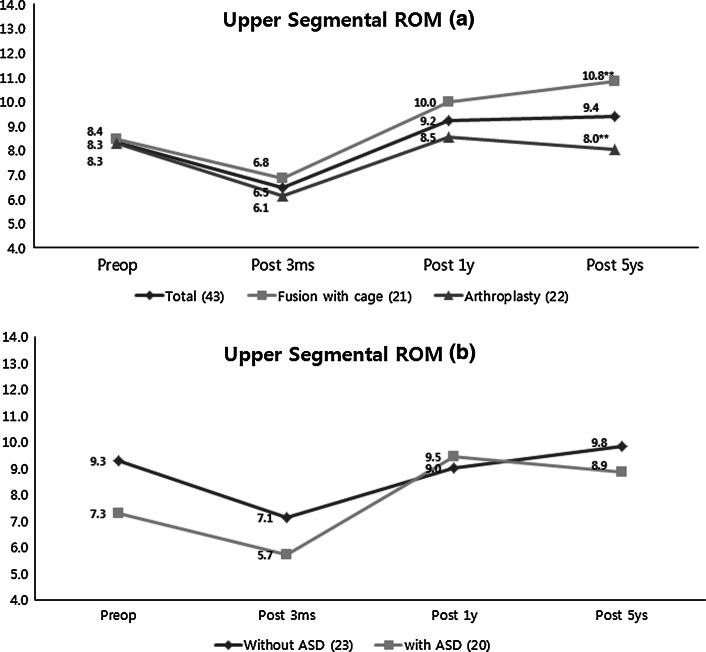
Comparative clinical and radiologic results between fusion and arthroplasty group
Substantial reduction in VAS and NDI occurred in both groups compared with the preoperative values, and there were no significant differences between fusion and arthroplasty group (Table 2). Fusion rates were 95.2 % (20/21) in fusion group and 4.5 % (2/22) in arthroplasty group. All radiographic results were showed in Table 5. Among radiologic parameters, cervical lordosis, C2-7 ROM and lower segmental ROM did not show any differences between groups (Figs. 4a, 6a and 9a). Operated segmental height (33.5 vs. 37.1 mm, p < 0.01) (Fig. 5a) and operated segmental ROM (0.5 vs. 10.2o, p < 0.01) significantly decreased in fusion group (Fig. 7a), and upper segmental ROM (10.8 vs. 8.0o, p < 0.05) significantly increased in fusion group (Fig. 8a).
Table 2.
Comparative clinical results between fusion and arthroplasty
| No. of cases | Pre-VAS | Post-VAS | Pre-NDI | Post-NDI |
|---|---|---|---|---|
| Total (43) | 7.3 ± 1.9 | 2.4 ± 2.3 | 52.0 ± 18.1 | 13.7 ± 12.2 |
| Fusion with cage (21) | 8.0 ± 1.7 | 2.6 ± 2.5 | 40.2 ± 22.1 | 12.2 ± 13.1 |
| Arthroplasty (22) | 6.8 ± 2.1 | 2.3 ± 2.1 | 45.5 ± 20.9 | 12.9 ± 12.5 |
Table 5.
All radiologic parameters at preop, postop 3 months, postop 1 year and postop 5 years
| No. of cases | Cervical lordosis | Operated segmental height | C2-7 ROM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Post 3 months | Post 1 year | Post 5 years | Preop | Post 3 months | Post 1 year | Post 5 years | Preop | Post 3 months | Post 1 year | Post 5 years | |
| Total (43) | −8.6† | −9.8 | −12.7 | −14.8† | 34.5† | 35.3 | 35.2 | 35.3† | 39.8 | 33.0 | 40.5 | 43.0 |
| Fusion with cage (21) | −10.6 | −9.4 | −12.2 | −13.3 | 33.4 | 34.1 | 33.2 | 33.5* | 41.7 | 30.4 | 36.4 | 41.3 |
| Arthroplasty (22) | −6.8† | −10.2 | −13.1 | −16.3† | 35.5† | 36.5 | 36.9 | 37.1†* | 38.4 | 35.5 | 43.9 | 44.7 |
| Without ASD (23) | −9.6‡ | −10.5 | −13.6 | −14.2‡ | 35.0 | 35.2 | 34.9 | 35.0 | 45.5 | 35.8 | 40.3 | 47.0* |
| With ASD (20) | −7.5† | −9.1 | −11.6 | −15.5† | 33.8† | 35.4 | 35.6 | 35.6† | 33.6 | 29.8 | 40.6 | 38.5* |
| Operated segmental ROM | Upper segmental ROM | Lower segmental ROM | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Post 3 months | Post 1 year | Post 5 years | Preop | Post 3 months | Post 1 year | Post 5 years | Preop | Post 3 months | Post 1 year | Post 5 years | |
| Total (43) | 10.8 | 6.0 | 6.8 | 5.6 | 8.3 | 6.5 | 9.2 | 9.4 | 5.9‡ | 5.1 | 7.2 | 7.7‡ |
| Fusion with cage (21) | 10.2 | 1.4 | 0.7 | 0.5* | 8.4 | 6.8 | 10.0 | 10.8** | 3.1† | 5.1 | 6.7 | 6.6† |
| Arthroplasty (22) | 11.2† | 10.5 | 12.1 | 10.2†* | 8.3 | 6.1 | 8.5 | 8.0** | 8.0 | 5.1 | 7.6 | 8.6 |
| Without ASD (23) | 12.4‡ | 6.0 | 6.7 | 6.0‡ | 9.3 | 7.1 | 9.0 | 9.8 | 5.7‡ | 4.6 | 7.8 | 8.4‡ |
| With ASD (20) | 8.9 | 6.0 | 7.0 | 5.2 | 7.3 | 5.7 | 9.5 | 8.9 | 6.2 | 5.7 | 6.5 | 6.9 |
Between groups comparisons with * Mann–Whitney test and p < 0.01, **p < 0.05 and intergroup comparison between post 5 years with preop by † Wilcoxon signed-ranks test and p < 0.01, ‡p < 0.05
Fig. 4.
Cervical lordosis in fusion versus arthroplasty group (a), and group without ASD versus group with ASD (b). There were no significant differences between groups. About intergroup comparisons between postoperative 5 years with preoperative state, cervical lordosis was significantly increased at all group except the fusion group (a, b) (†Wilcoxon signed-ranks test and p < 0.01, ‡p < 0.05)
Fig. 6.
C2-7 ROM in fusion versus arthroplasty group (a), and group without ASD versus group with ASD (b). There was a significant difference between groups without ASD and with ASD at postoperatively 5 years (*Mann–Whitney test, Spearman rs = −0.334, p < 0.01). About intergroup comparison between postoperative 5 years with preoperative state, there were no significant differences
Fig. 9.
Lower segmental ROM in fusion versus arthroplasty group (a), and group without ASD versus group with ASD (b). There were no significant differences between these two groups. About intergroup comparison between postoperative 5 years with preoperative state, lower segmental ROM was significantly increased at total, fusion (a) and groups without ASD (b) (†Wilcoxon signed-ranks test and p < 0.01, ‡p < 0.05)
Fig. 5.
Operated segmental height in fusion versus arthroplasty group (a), and group without ASD versus group with ASD (b). There was a significant difference between fusion and arthroplasty group at postoperatively 1 year and 5 years (a) (*Mann–Whitney test and p < 0.01). About intergroup comparisons between postoperative 5 years with preoperative state, operated segmental height was significantly increased at total, arthroplasty (a) and groups with ASD (b) (†Wilcoxon signed-ranks test and p < 0.01)
Fig. 7.
Operated segmental ROM in fusion versus arthroplasty group (a), and group without ASD versus group with ASD (b). There were significant differences between fusion and arthroplasty group (*Mann–Whitney test and p < 0.01). About intergroup comparison between postoperative 5 years with preoperative state, operated segmental ROM was significantly decreased at fusion (a) and groups without ASD (b) (†Wilcoxon signed-ranks test and p < 0.01, ‡p < 0.05). When operated segmental ROM was measured on arthroplasty group, there were no significant differences between groups with ASD and without ASD (c)
Fig. 8.
Upper segmental ROM in fusion versus arthroplasty group (a), and group without ASD versus group with ASD (b). There were significant differences between fusion and arthroplasty group (**Mann–Whitney test and p < 0.05). About intergroup comparison between postoperative 5 years with preoperative state, there were no significant differences
About intergroup comparisons between postoperative 5 years with preoperative state in total patients, cervical lordosis (Fig. 4a), operated segmental height (Fig. 5a) and lower segmental ROM (Fig. 9a) were significantly increased. In arthroplasty group, cervical lordosis (Fig. 4b) and operated segmental height (Fig. 5a) were significantly increased between postoperative 5 years with preoperative state (Fig. 7a); on the other hand, operated segmental ROM (Fig. 7a) was decreased significantly, but upper (Fig. 8a) and lower segmental ROM (Fig. 9a) were increased significantly in fusion group (Fig. 7a). (†Wilcoxon signed-ranks test and p < 0.01, ‡p < 0.05).
Comparative clinical and radiologic results between patients without ASD and with ASD
Between patients without ASD (23 patients) and with ASD (20 patients), there were no significant differences in the mean age (41.2 vs. 43.0 years) and in the mean follow-up period (63.4 vs. 60.8 months) (Table 3). Substantial reduction in VAS and NDI occurred in both groups compared with the preoperative values, and there were no significant differences between these two groups (Table 4). Preexisting ASD (17/20 vs. 12/23) (Mann–Whitney test and Spearman rs = 0.349, p < 0.05) and other segment degeneration (8/20 vs. 0/23) (*Mann–Whitney test and Spearman rs = 0.513, p < 0.01) were significantly higher in ASD group (Table 3). Among the radiologic parameters, only C2-7 ROM at 5 years (38.45 vs. 47.0o, p < 0.01) was significantly decreased in the ASD group (Figs. 4b, 5b, 6b, 7b, 8b, and 9b). There was no patient who needed a secondary operation or an additional treatment due to ASD.
Table 3.
Comparative demographic and radiologic data between groups without ASD and with ASD
| No. of cases | Mean age (years) | Male/Female | Mean F/U (months) | Preop ASD (%) | Other segment degeneration (%) | |
|---|---|---|---|---|---|---|
| Without ASD | 23 | 41.2 ± 11.8 | 16/7 | 63.4 ± 8.6 | 12 (52.2 %)a | 0 (0 %)b |
| With ASD | 20 | 43.0 ± 7.9 | 14/6 | 60.8 ± 8.5 | 17 (85 %)a | 8 (40 %)b |
aSpearman correlation coefficients for correlations between groups without ASD and with ASD (Spearman’s rs = 0.349, P = 0.022)
bSpearman’s rs = 0.513, P = 0.000
Table 4.
Comparative clinical results between groups without ASD and with ASD
| No. of cases | Pre-VAS | Post-VAS | Pre-NDI | Post-NDI |
|---|---|---|---|---|
| Without ASD (23) | 7.5 ± 1.9 | 2.6 ± 2.6 | 47.7 ± 21.9 | 13.8 ± 14.9 |
| With ASD (20) | 7.2 ± 2.0 | 2.3 ± 2.1 | 43.4 ± 20.3 | 12.0 ± 9.7 |
About intergroup comparisons between postoperative 5 years with preoperative state in group with ASD, cervical lordosis (Fig. 4b) and operated segmental height (Fig. 5b) were increased significantly; on the other hand, cervical lordosis (Fig. 4b) and lower segmental ROM (Fig. 9b) were significantly increased, but operated segmental ROM (Fig. 7b) was decreased significantly between postoperative 5 years with preoperative state in group without ASD. When operated segmental ROM was measured on arthroplasty group, there were no significant differences between groups with ASD and without ASD (Fig. 7c). (†Wilcoxon signed-ranks test and p < 0.01, ‡p < 0.05).
Discussion
ASD rates after cervical anterior fusion varied from 25 to 92 % during a long follow-up period [1, 7–11, 19]. Previously, Hilibrand et al. [1] reported that the prevalence of symptomatic adjacent segment disease after ACDF is 2.9 % per year in the 1 year and 25.6 % after 10 years. Surprisingly, Goffin et al. [7] also reported 92 % of prevalence after 5 year. Many previous studies tried to figure out the reason of ASD after cervical arthrodesis, and biomechanical studies have shown evidence of hypermobility and increased stress at levels adjacent to the site of fused segment [20, 21]. However, Matsunaga et al. [22] calculated that there was no increase in the strain adjacent to a single-level ACDF, and Hilibrand et al. [1] reported a reduced rate of adjacent segment disease in patients who underwent multilevel fusion compared with those treated by single-level fusion and a more likelihood of ASD in older patients. They also insisted that symptomatic adjacent segment disease is the result of progressive cervical spondylosis and is not caused by the arthrodesis itself [1, 23]. In a study by Goffin et al, 1 % loss of disc space height was considered to be evidence of disc degeneration and only 6.1 % of patients required a surgery due to symptomatic adjacent segment disease over 8 years [7]. Gore et al. [24] studied 159 initially asymptomatic patients, and in that study, 34 % of the subjects who had no initial radiographic evidence of degenerative disease developed symptomatic adjacent segment disease over 10 years. Recent MRI follow-up study for asymptomatic volunteers showed degeneration of cervical disc in the range of 60 to 70 % in ten year and natural disc degeneration rates higher than ASD after ACDF [25]. In comparative studies between ACDF and arthroplasty, they reported a lower rate of ASD because of preservation of neck motion [11, 15, 26]. However, these studies followed only X-ray or CT and lacked long-term results [1, 7–11], and other studies insisted no difference in ASD rate between ACDF and arthroplasty [12, 27]. Even till now, we do not know the related factors, incidence and prevalence of ASD after ACDF and arthroplasty.
Here, we observed that ASD rates by simple radiography (11.5 %) are less than those of MRI and CT (46.5 %) (Table 1; Figs. 2, 3). Recently, there have been several trials to assess ASD with MRI, and usability of MRI to assess ASD has been reported. Matumoto et al. [27–30] reported 40–60 % degenerative change in adjacent disc after ACDF using MRI, and other study by CT also reported that asymptomatic ASD was detected as 50 %, and this result is very similar with our results. There has been no comparative study between ACDF and arthroplasty with MRI. The ASD is associated with natural degenerative progression or biomechanical effect of fusion and can be prevented by arthroplasty or motion preservation? This is the first comparative study to understand the incidence, prevalence and causes of adjacent segment disease through a 5-year follow-up of radiography, CT and MRI between ACDF and arthroplasty. From this 5-year follow-up of MRI and CT study, we demonstrate that ASD rates were 46.5 % (20/43) after ACDF or arthroplasty and that arthroplasty did not reduce the incidence of ASD than that of ACDF. In spite of increase in the upper segmental ROM and subsidence in the operated segment in the fusion group, there was no significant difference between fusion and arthroplasty group in ASD rates. For fusion group, we only chose ACDF with only PEEK box cage without a plate. The use of cage and plate for ACDF has several merits in respect to lordotic alignment, cage subsidence and fusion rate [17, 31–33], but because plate fixation increases fixation force, a stress generated in the adjacent disc, these effect can increase the possibility to get ASD rather than ACDF with cage alone [17, 31]. Currently, cage made of PEEK is primarily used for ACDF due to its biomechanical similarities to those of bone [17]. Furthermore, cylindrical cage fails to prevent kyphosis and to preserve natural intervertebral alignment, making PEEK box cage more suitable for ACDF [34].
In a comparative result between groups ASD and without ASD, among many radiographic parameters, only preexisting ASD and other segment postoperative degeneration out of the adjacent segment were associated with postoperative ASD, and this means that ASD is related to the natural degenerative process instead of arthrodesis itself. In spite of the fact that upper segmental ROM increased in fusion than arthroplasty group, there was no significant difference between fusion and arthroplasty group in ASD rate, and group with ASD and group without ASD showed no difference in adjacent segment ROM. C2-7 ROM at 5 years later decreased in group with ASD than in group without ASD, and at 1-year postoperative, ROM had no difference between groups with ASD and without ASD. Time difference of C2-7 ROM between group with ASD and group without ASD may show that C2-7 ROM decrease is the result of both natural degenerative change and ASD in cervical spine. In the aspect of operated segmental ROM, to exclude the reductive effect of operated segmental ROM by ACDF, when we compared only arthroplasty group between with ASD and without ASD, there were no significant differences (9.1 vs. 11.3 mm) (Fig. 7c). It means that operated segmental ROM decrease did not associate with ASD.
At intergroup comparisons between postoperative 5 years with preoperative state, we can observe differences between ACDF and arthroplasty. Operated segmental ROM, upper and lower segmental ROM were preserved at arthroplasty group, but these trait did not relate with decrease rate of ASD. In spite of decrease in operated segmental ROM at fusion group, there was no difference of ASD rate between arthroplasty and fusion groups, and there was no difference of group with ASD and group without ASD in operated segmental ROM. It means that decrease in operated segmental ROM is not related with ASD. In addition about upper and lower segmental ROM, between group with ASD and group without ASD, there were no differences, and this results reflect that upper and lower segmental ROM change did not relate with ASD. The cervical lordosis was increased in total patients, arthroplasty, both groups without and with ASD, and we can guess that the increase in cervical lordosis did not relate with ASD. Operated segmental height was increased significantly in ASD group 5 years later, and preoperatively operated segmental height was less than group without ASD. From this result, we can know that ASD is associated with preoperative severe degenerative change at operated segment, and it will be another clue that the cause of ASD may be associated with a natural history of cervical spondylosis rather than arthrodesis.
We have investigated adjacent segment degeneration without clinical symptom, and there was no patient who required operation or other treatment due to ASD. As already described in the introduction, “adjacent segment degeneration (ASD)” and “adjacent segment disease” are used interchangeably [5]. Since ASD is a before step of “adjacent segment disease”, we focused on ASD without clinical symptoms. In this study, there was no difference in the clinical result between patients with ASD and without ASD. We postulate that ASD without symptom did not make any difference in clinical result because ASD is associated with the natural history of cervical spondylosis.
Of course, this study has many limitations. Foremost, very few patients were used and only one segment ACDF and arthroplasty were included in this study. To know the exact cause of ASD, we need larger group of patients treated with ACDF and arthroplasty and should include a multi-segment operation. Secondly, only asymptomatic adjacent segment degeneration was included. The characteristic of adjacent segment disease and ASD may also be different, and we need a further study focusing on the difference between adjacent segment disease and asymptomatic ASD. In spite of these limitations, from this study, we can get a clue of the factors of ASD and an understanding that ASD may be associated with a natural history of cervical spondylosis rather than arthrodesis.
Acknowledgments
The authors thank Su Jin Lee, MS at Department of Neurosurgery, Gangnam Severance Hospital, for her large effort for this study.
Conflict of interest
None.
References
- 1.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Weinhoffer SL, Guyer RD, Herbert M, Griffith SL. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976) 1995;20:526–531. doi: 10.1097/00007632-199503010-00004. [DOI] [PubMed] [Google Scholar]
- 3.Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine (Phila Pa 1976) 1984;9:574–581. doi: 10.1097/00007632-198409000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Bushell GR, Ghosh DP, Taylor TK, Sutherland JM, Braund KG. The effect of spinal fusion on the collagen and proteoglycans of the canine intervertebral disc. J Surg Res. 1978;25:61–69. doi: 10.1016/0022-4804(78)90159-2. [DOI] [PubMed] [Google Scholar]
- 5.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4:190–194. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, Van Calenbergh F, van Loon J. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Cherubino P, Benazzo F, Borromeo U, Perle S. Degenerative arthritis of the adjacent spinal joints following anterior cervical spinal fusion: clinicoradiologic and statistical correlations. Ital J Orthop Traumatol. 1990;16:533–543. [PubMed] [Google Scholar]
- 9.Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical fusion. Spine (Phila Pa 1976) 1980;5:399–401. doi: 10.1097/00007632-198009000-00002. [DOI] [PubMed] [Google Scholar]
- 10.McGrory BJ, Klassen RA. Arthrodesis of the cervical spine for fractures and dislocations in children and adolescents. A long-term follow-up study. J Bone Joint Surg Am. 1994;76:1606–1616. doi: 10.2106/00004623-199411000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3:417–423. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 12.Burkus JK, Haid RW, Traynelis VC, Mummaneni PV. Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2010;13:308–318. doi: 10.3171/2010.3.SPINE09513. [DOI] [PubMed] [Google Scholar]
- 13.Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009;34:101–107. doi: 10.1097/BRS.0b013e31818ee263. [DOI] [PubMed] [Google Scholar]
- 14.Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6:198–209. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 15.Sasso RC, Anderson PA, Riew KD, Heller JG. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011;93:1684–1692. doi: 10.2106/JBJS.J.00476. [DOI] [PubMed] [Google Scholar]
- 16.Joo YH, Lee JW, Kwon KY, Rhee JJ, Lee HK. Comparison of fusion with cage alone and plate instrumentation in two-level cervical degenerative disease. J Korean Neurosurg Soc. 2010;48:342–346. doi: 10.3340/jkns.2010.48.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP. The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine (Phila Pa 1976) 2009;34:2886–2892. doi: 10.1097/BRS.0b013e3181b64f2c. [DOI] [PubMed] [Google Scholar]
- 18.Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410–1418. [PubMed] [Google Scholar]
- 19.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976) 1993;18:2167–2173. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Seo M, Choi D. Adjacent segment disease after fusion for cervical spondylosis; myth or reality? Br J Neurosurg. 2008;22:195–199. doi: 10.1080/02688690701790605. [DOI] [PubMed] [Google Scholar]
- 21.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 22.Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 1999;24:670–675. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 23.McCormick PC. The adjacent segment. J Neurosurg Spine. 2007;6:1–4. doi: 10.3171/spi.2007.6.1.1. [DOI] [PubMed] [Google Scholar]
- 24.Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine (Phila Pa 1976) 2001;26:2463–2466. doi: 10.1097/00007632-200111150-00013. [DOI] [PubMed] [Google Scholar]
- 25.Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami A, Ikegami T, Takahata T, Hashimoto T. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 2010;35:36–43. doi: 10.1097/BRS.0b013e3181b8a80d. [DOI] [PubMed] [Google Scholar]
- 26.Upadhyaya CD, Wu JC, Trost G, Haid RW, Traynelis VC, Tay B, Coric D, Mummaneni PV. Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine. 2011;16:216–228. doi: 10.3171/2011.6.SPINE10623. [DOI] [PubMed] [Google Scholar]
- 27.Nunley PD, Jawahar A, Kerr EJ, 3rd, Gordon CJ, Cavanaugh DA, Birdsong EM, Stocks M, Danielson G. Factors affecting the incidence of symptomatic adjacent level disease in cervical spine after total disc arthroplasty: 2–4 years follow-up of 3 prospective randomized trials. Spine. 2012;15:445–451. doi: 10.1097/BRS.0b013e31822174b3. [DOI] [PubMed] [Google Scholar]
- 28.Neal CJ, Rosner MK, Kuklo TR. Magnetic resonance imaging evaluation of adjacent segments after disc arthroplasty. J Neurosurg Spine. 2005;3:342–347. doi: 10.3171/spi.2005.3.5.0342. [DOI] [PubMed] [Google Scholar]
- 29.Antosh IJ, DeVine JG, Carpenter CT, Woebkenberg BJ, Yoest SM. Magnetic resonance imaging evaluation of adjacent segments after cervical disc arthroplasty: magnet strength and its effect on image quality. Clinical article. J Neurosurg Spine. 2010;13:722–726. doi: 10.3171/2010.5.SPINE09721. [DOI] [PubMed] [Google Scholar]
- 30.Sugawara T, Itoh Y, Hirano Y, Higashiyama N, Mizoi K. Long term outcome and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir (Wien) 2009;151:303–309. doi: 10.1007/s00701-009-0217-5. [DOI] [PubMed] [Google Scholar]
- 31.Hakalo J, Pezowicz C, Wronski J, Bedzinski R, Kasprowicz M. Comparative biomechanical study of cervical spine stabilisation by cage alone, cage with plate, or plate-cage: a porcine model. J Orthop Surg (Hong Kong) 2008;16:9–13. doi: 10.1177/230949900801600103. [DOI] [PubMed] [Google Scholar]
- 32.Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011;3:16–23. doi: 10.4055/cios.2011.3.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 2008;15:1017–1022. doi: 10.1016/j.jocn.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 34.Kolstad F, Nygaard OP, Andresen H, Leivseth G. Anterior cervical arthrodesis using a “stand alone” cylindrical titanium cage: prospective analysis of radiographic parameters. Spine (Phila Pa 1976) 2010;35:1545–1550. doi: 10.1097/BRS.0b013e3181d259c1. [DOI] [PubMed] [Google Scholar]