Abstract
Purpose
Little data is available on the relationships between sagittal balance and spinopelvic parameters in osteoporosis. We analyzed sagittal spinopelvic parameters in osteoporotic patients.
Methods
In this prospective study, the patient and control groups comprised 124 osteoporotic patients and 40 controls. Average age was 72.4 ± 6.8 in the osteoporosis group and 42.7 ± 12.5 in the control group, which was significantly different (P < 0.001). Osteoporotic patients were allocated to two groups by sagittal vertical axis, namely, a sagittal balance group (n = 56) and a sagittal imbalance group (n = 68). All 164 study subjects underwent whole spine lateral radiography, which included hip joints. The radiographic parameters investigated were sacral slope, pelvic tilt, pelvic incidence, thoracic kyphosis, lumbar lordosis, and sagittal vertical axis. Statistical analysis was performed to identify significant differences between the two groups.
Results
Osteoporotic patients and controls were found to be significantly different in terms of sagittal vertical axis, sacral slope, pelvic tilt, lumbar lordosis, and thoracic kyphosis. However, no significant difference was observed between patients and controls in terms of pelvic incidence (P > 0.05). Significant differences were found between the balance and imbalance groups in terms of age, lumbar spine bone mineral density (LSBMD), femoral neck BMD (FNBMD), visual analogue scale (VAS) score, sacral slope, and pelvic incidence. Correlation analysis revealed significant relationships between sagittal parameters and osteoporosis. Stepwise logistic regression analysis revealed that FNBMD and pelvic incidence contributed significantly to sagittal balance.
Conclusion
Sagittal spinopelvic parameters were found to be significantly different in patients and normal controls. Significant relationships were found between sagittal spinopelvic parameters in osteoporotic patients. In particular, low FNBMD and high pelvic incidence were significant parameters in determination of sagittal balance in osteoporotic patients.
Keywords: Osteoporosis, Sagittal spinopelvic parameters
Introduction
Osteoporosis is a major issue in the elderly. The incidence of vertebral fractures is expected to increase in the elderly, and those that suffer an osteoporotic vertebral fracture are known to have poorer health-related quality of life [20]. Furthermore, patients with osteoporosis have weaker back extensor strength and poor balance, which result in a propensity to fall [24]. Kyphosis is considered a result of osteoporotic vertebral fracture, and vertebral fractures presenting with an anterior wedge deformity are one of the possible causes of kyphosis [5, 6]. In addition, patients with abnormal kyphotic posture often complain of pain and decreased walking ability [12, 26], and thus, sagittal spinal alignment is important for normal spinal function.
Many studies on spinal sagittal alignment have shown variances of thoracic kyphosis, lumbar lordosis [2], and spinopelvic parameters [19, 22, 27, 28] and shown these alignments are affected by variables, such as, age, spinal fusion, sex, weight, and pelvic morphology [7, 13]. Recently, investigators described sagittal alignment in older populations [10, 25], but little is known about the effects of osteoporosis on sagittal curvature. Accordingly, the aim of this prospective study was to investigate sagittal spinal alignment and pelvic orientation in patients with osteoporosis, and to indentify predictors of sagittal imbalance. In addition, we also investigated differences between osteoporotic patients with or without a vertebral fracture in terms of sagittal spinopelvic alignment.
Patients and methods
One hundred and twenty-four consecutive female patients with osteoporosis were enrolled prospectively at time of examinations at an orthopaedic outpatient clinic between January 2011 and January 2012. Demographic and clinical characteristics and Visual Analogue Scale (VAS: 0–10) pain scores were obtained. Forty normal subjects who underwent whole spine radiographs for simple health checkup were recruited as control group. Subjects with a history of orthopaedic condition were excluded. The study was approved by the Clinical Research Ethics Committee of our institution. Patients were assigned to two groups: balance group, patients with sagittal balance or imbalance group, patients with sagittal imbalance.
All osteoporotic patients met the diagnostic criterion for osteoporosis (T score ≤ −2.5) [23], and were considered eligible to participate if they had been medically treated for at least 1 year. Pain originating from the spine was scored, but pain originating from any other part of the body was excluded. Exclusion criteria were concomitant neurological or psychiatric disease. Patients with a history of or a current orthopaedic condition of the spine (spinal disc herniation, degenerative scoliosis, and spinal surgery, etc.) or lower extremities (prosthesis, etc.) were also excluded. However, patients with a history of an osteoporotic vertebral fracture, but not a current symptomatic vertebral fracture, were included.
Anthropometric measurements included body height and body weight. Body mass index (BMI) was determined by dividing weight (kg) by uncorrected height squared (m2). Lumbar spinal bone mineral density (LSBMD) and femoral neck BMD (FNBMD) of the non-dominant proximal femur were measured by dual-energy X-ray absorptiometry (DEXA) (XR-36; Norland Corp., Fort Atkinson, WI, USA). LSBMD was measured for L1 through to L4 in anterior–posterior view.
Participants underwent anteroposterior and lateral whole spine radiography. Radiographs were taken by one technician using a standard technique and the same machine at a distance of 72 inches in the standing position. All lateral radiographs included both hip joints and the C7 vertebra.
Radiographic parameters such as sacral slope, pelvic tilt, pelvic incidence, thoracic kyphosis, lumbar lordosis, and sagittal vertical axis were measured using a picture achieving computer system (PACS Expertise, Marosis, South Korea). Sacral slope was defined as the angle between the sacral end plate and the horizontal. Pelvic tilt was defined as the angle between the line joining the middle of the sacral end plate and hip axis and the vertical. Pelvic incidence was defined as the angle between a line perpendicular to the sacral end plate and a line joining the middle of the sacral plate and the hip axis. Thoracic kyphosis was measured between the upper endplate of T1 or T2 and the lower endplate of the T12 using Cobb’s method. T1–T12 kyphotic angle was used in most subjects and T2–T12 only in 12 subjects in this study. Lumbar lordosis was measured between the upper endplate of L1 and the lower endplate of L5 using Cobb’s method, because the S1 vertebra is often affected by degenerative changes and its contour usually invisible in arthritic patients [21]. Sagittal balance was defined using the sagittal vertical axis, which was defined as the horizontal distance between a plumb line dropped from the center of the C7 body and the posterior-superior corner of the S1 body. A positive value was defined as anterior displacement of the sagittal plumb line. Because the posterosuperior aspect of the S1 body was used as the reference, the normal neutral range for sagittal spinal balance was <3 cm from the posterior-superior corner of the S1 body. Osteoporotic patients were allocated to the sagittal balance group or sagittal imbalance group (sagittal vertical axis >30 mm, respectively). All measurements were performed twice independently by three spine surgeons with an interval of 2 weeks between measurements to decrease intraobserver (Pearson correlation coefficient = 0.921, range 0.887–0.936) and interobserver errors (Pearson correlation coefficient = 0.911, range 0.876–0.935).
Statistical analysis was performed using SPSS ver. 11.5 for Windows (SPSS, Chicago, IL). Data are expressed as mean ± standard deviations. Logistic regression analysis was performed to identify predictors of sagittal imbalance. Initially, univariate logistic regression was used to test for associations, and then forward stepwise multiple logistic regression analysis was used to develop a prediction model. In addition, receiver operating characteristic (ROC) curve analysis was used to determine optimal cut-off values for parameters. The sensitivities and specificities of various variables and standard errors (SEs), 95 % confidence intervals (CIs), and area under curves (AUCs) were calculated. The statistical differences between groups were assessed using the t test or Chi square test. P values of <0.05 were regarded as statistically significant.
Results
The average age of the 124 osteoporotic patients was 72.4 ± 6.8 years. Mean weight and BMI of the 124 patients were 56.3 ± 4.0 kg and 23.0 ± 1.6 kg/m2, respectively, and mean LSBMD and mean FNBMD were 0.766 ± 0.106 and 0.693 ± 0.091 g/cm2, respectively. Mean VAS back pain score was 2.7 ± 1.3. Sagittal parameters of patients and controls are summarized in Table 1, and were patients and controls were found to be significantly different in terms of; sagittal vertical axis, sacral slope, pelvic tilt, lumbar lordosis, and thoracic kyphosis, but not in terms of pelvic incidence (P > 0.05).
Table 1.
Details of the patients
| Normal (n = 40) | Osteoporosis (n = 124) | P value | |
|---|---|---|---|
| Age | 42.7 ± 12.5 | 72.4 ± 6.8 | <0.001 |
| Height | 158.9 ± 4.4 | 156.7 ± 4.1 | <0.001 |
| Weight | 56.8 ± 5.0 | 56.3 ± 4.0 | 0.5468 |
| BMI | 22.5 ± 1.7 | 23.0 ± 1.6 | 0.1004 |
| Sagittal vertical axis | −26.1 ± 13.4 | 35.0 ± 38.3 | <0.001 |
| Sacral slope | 36.8 ± 6.0 | 25.1 ± 9.0 | <0.001 |
| Pelvic tilt | 13.8 ± 6.7 | 24.2 ± 8.5 | <0.001 |
| Pelvic incidence | 50.3 ± 3.6 | 49.3 ± 11.2 | 0.4923 |
| Lumbar lordosis | 40.3 ± 3.9 | 27.3 ± 15.5 | <0.001 |
| Thoracic kyphosis | 38.7 ± 5.5 | 31.3 ± 15.6 | 0.0030 |
Of the 124 patients, 62 (50 %) had history of vertebral fracture. The mean kyphotic angle of 100 vertebral fractures (two T7; seven T8; three T9; four T10; eleven T11; twenty-eight T12; twenty-four L1; twelve L2; six L3; two L4 and one L5) among with 62 patients was 15.4 ± 6.0°. According to sagittal vertical axis, 56 patients were allocated to the balance group and 68 to the imbalance group. These two groups did not differ statistically in terms of the presence of or history of an osteoporotic fracture, pelvic tilt, lumbar lordosis, or thoracic kyphosis (Table 2). However, significant differences were observed between balance and imbalance groups in terms of age, LSBMD, FNBMD, VAS, sacral slope, and pelvic incidence (Fig. 1). Furthermore, correlation analysis revealed significant relationships between sagittal parameters (Table 3).
Table 2.
Details of the osteoporotic patients
| Balance (n = 56) | Imbalance (n = 68) | P value | |
|---|---|---|---|
| Age | 70.9 ± 5.9 | 73.6 ± 7.4 | 0.030 |
| Height | 1.57 ± 0.04 | 1.56 ± 0.04 | 0.383 |
| Weight | 56.1 ± 4.8 | 56.5 ± 3.1 | 0.547 |
| BMI | 22.8 ± 1.5 | 23.2 ± 1.6 | 0.140 |
| History of vertebral fracture | 24 | 38 | 0.207 |
| LSBMD | 0.793 ± 0.090 | 0.744 ± 0.113 | 0.010 |
| FNBMD | 0.722 ± 0.090 | 0.670 ± 0.085 | 0.001 |
| Sagittal vertical axis | 5.0 ± 18.0 | 59.7 ± 32.6 | <0.001 |
| Sacral slope | 23.2 ± 7.6 | 26.7 ± 9.8 | 0.028 |
| Pelvic tilt | 23.2 ± 8.1 | 25.1 ± 8.8 | 0.230 |
| Pelvic incidence | 46.3 ± 10.1 | 51.7 ± 11.5 | 0.007 |
| Lumbar lordosis | 26.3 ± 14.8 | 28.1 ± 16.1 | 0.525 |
| Thoracic kyphosis | 30.7 ± 18.1 | 31.8 ± 13.3 | 0.702 |
| VAS score | 2.4 ± 1.3 | 2.9 ± 1.3 | 0.032 |
Fig. 1.

Lateral standing whole spine radiographs (a sagittal balance group and b sagittal imbalance group) demonstrate that pelvic incidence of sagittal balance group was smaller than that of sagittal imbalance group
Table 3.
Correlations of the parameters in osteoporotic patients
| Age | BMI | FNBMD | LSBMD | SS | PT | PI | LL | TK | VAS | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sagittal vertical axis (SVA) | r | 0.271* | −0.003 | −0.281* | −-0.168 | 0.117 | 0.073 | 0.155 | −0.120 | −0.047 | 0.380* |
| Age | r | 0.027 | −0.164 | 0.088 | −0.005 | 0.099 | 0.081 | −0.150 | 0.009 | 0.110 | |
| BMI | r | −0.072 | −0.101 | −0.079 | 0.125 | 0.056 | −0.006 | 0.058 | 0.084 | ||
| FNBMD | r | 0.548* | −0.016 | −0.095 | −0.118 | −0.048 | 0.046 | −0.485* | |||
| LSBMD | r | 0.039 | −0.400* | −0.293* | −0.058 | −0.061 | −0.532* | ||||
| Sacral slope (SS) | r | −0.172 | 0.651* | 0.607* | 0.266* | −0.316* | |||||
| Pelvic tilt (PT) | r | 0.622* | −0.209* | −0.036 | 0.226* | ||||||
| Pelvic incidence (PI) | r | 0.304* | 0.179* | −0.039 | |||||||
| Lumbar lordosis (LL) | r | 0.632* | −0.218* | ||||||||
| Thoracic kyphosis (TK) | r | 0.098 | |||||||||
* P < 0.05
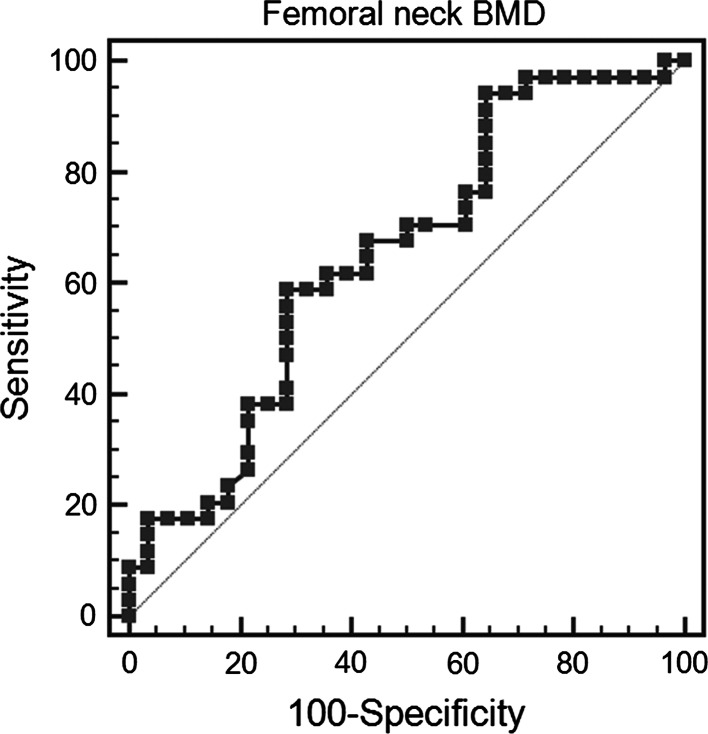
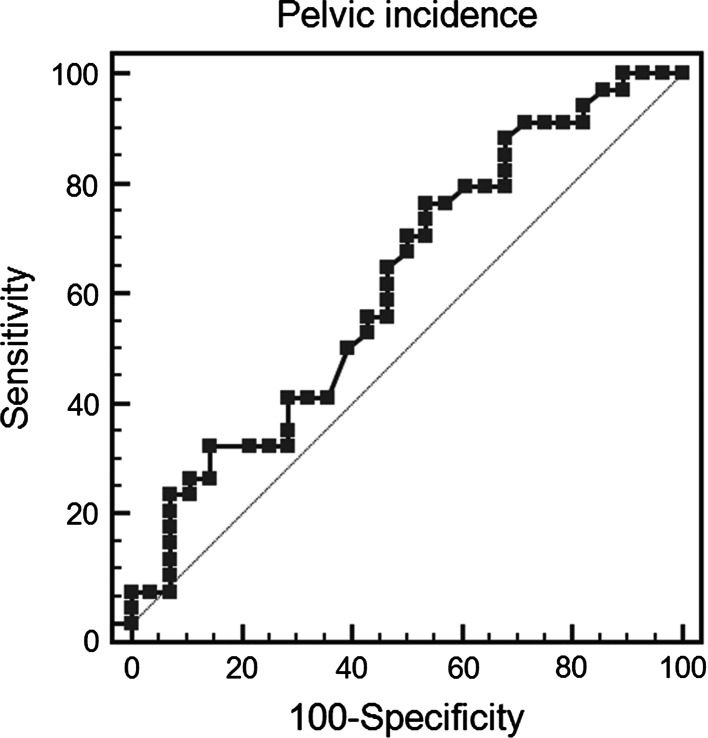
Multivariate logistic regression showed that FNBMD (P = 0.005) and pelvic incidence (P = 0.023) were predictors of sagittal imbalance in patients (Table 4). ROC analyses of quantitative indices were performed to determine the optimal cut-off values for FNBMD and pelvic incidence for predicting the presence of sagittal imbalance. For FNBMD, ROC curve analysis provided an optimum cut-off value was 0.676 g/cm2, which had a sensitivity and specificity of 58.8 and 71.4 %, respectively (Fig. 2) The AUC was 0.649 (SE 0.050, 95 % CI 0.558–0.732, P = 0.003). For pelvic incidence, the optimum cut-off value was 44.0°, which had a sensitivity and specificity of 76.5 and 46.4 %, respectively (Fig. 3). The AUC was 0.619 (SE 0.051, 95 % CI 0.527–0.704, P = 0.0120). Comparison of these ROC analyses showed no statistical difference between the abilities of FNBMD and pelvic incidence to detect sagittal imbalance (difference between areas 0.030, SE 0.066, 95 % CI −0.100–0.160, P = 0.652).
Table 4.
Stepwise multiple logistic regression analysis in osteoporotic patients
| Variables | Coefficient | Standard error | 95 % CI | Odds ratio | P value |
|---|---|---|---|---|---|
| FNBMD | −6.278 | 2.224 | 0.000 ~ 0.147 | 0.002 | 0.005 |
| PI | 0.043 | 0.019 | 1.006 ~ 1.083 | 1.044 | 0.023 |
| Constant | 2.466 | ||||
Fig. 2.
Receiver operating characteristic results for FNBMD with respect to the detection of sagittal imbalance in osteoporosis
Fig. 3.
Receiver operating characteristic results for pelvic incidence
Discussion
Although the treatment of spinal deformities associated with osteoporosis has become an increasingly important component in many spinal surgery practices, the relevance of pelvic measures in osteoporosis remains unclear. A small number of studies have addressed sagittal spinal alignment of the elderly [10, 25], but data on relations between specific radiologic pelvic parameters and osteoporosis is lacking.
Some parameters can be used to evaluate the effect of lumbosacral pelvic orientation on sagittal alignment of the spine in normal population, and sacral inclination, pelvic tilt, and pelvic incidence have been investigated [4, 13, 17]. However, changes in lumbar lordosis, sacral inclination angle, and sagittal vertical axis are known to occur with age [7, 10, 25], little is known about the contribution of osteoporosis to sagittal curvature. Accordingly, we investigated the sagittal spinal alignment and pelvic orientation in patients with osteoporosis and indentified predictors of sagittal balance. In the present study, sagittal parameters were found to differ significantly in osteoporotic patients with or without sagittal balance, and furthermore, these parameters were found to be related to each other.
Although correlations between sagittal parameters and the development of spinal disorders have not been confirmed in osteoporosis, differences and relationships between sagittal radiological parameters can provide clues when examining spinal deformities in osteoporotic patients. In the present study, pelvic incidence was much higher in the imbalance group than in the balance group. Pelvic incidence is a morphologic parameter, which is unaffected by posture or pelvic position, and is considered to be invariable at the end of growth. Because pelvic incidence is the algebraic sum of sacral slope and pelvic tilt, a greater value means that either or both of these values are elevated. Patients with a high pelvic incidence value usually have large sacral slope and lumbar lordosis values, which is consistent with our findings. Furthermore, a large lumbar lordosis value is a well-known factor of excessive mechanical stress on posterior articular joints, and thus, is indicative of accelerated arthritic changes and predisposition to slippage [1]. However, the present study indicates that lumbar lordosis is not a primary concern because its value was significantly lower in patients than in controls. In addition, the imbalance group had a higher sacral slope, but not a higher pelvic tilt, than the balance group. Since pelvic tilt represents posterior sacropelvic translation in compensation for sagittal imbalance, a compensatory higher value of pelvic tilt could be anticipated in the imbalance group. This trend was observed, but was not statistically significant in the present study, which is because patients had no remaining further pelvic compensatory ability [15].
In general, correlations between lumbar lordosis and sacral slope or pelvic tilt at the pelvic level are stronger for sacral slope than for pelvic tilt [3, 16, 17]. These correlations in sagittal alignment were consistent with those observed in the present study. Thus, it appears that spinal misalignment and pelvic abnormality are closely related in osteoporosis. To some extent, a reduction in lumbar lordosis can be compensated by a similar reduction in sacral slope to maintain the relative position of the C7 plumb line [14]. As previously reported, a reduction in sacral slope is an indicator of the amount of pelvic extension, where compensation is occurring [11].
In this study, it was found that pelvic incidence was higher in the osteoporotic imbalance group than in the osteoporotic balanced group. The pelvic incidence is a fundamental link between the pelvic and spinal alignment parameters. It is the primary determent of pelvic orientation; hence, lumbar lordosis is closely correlated with it. As the pelvic incidence increases, so should lordosis. Overall increased pelvic incidence combined with similar values of lumbar lordosis seen in younger populations may explain the increased anterior positioning of the C7 plumb line in older subjects. As the pelvic parameters are more fixed and independent than those of thoracic and lumbar spine, it thus becomes critical for treating surgeons to remain even more diligent about maintaining lordosis so as to ensure sagittal balance postoperatively.
Gross orientation and spinopelvic balance are important during disease progression [8, 9, 17, 18]. Glassman et al. [8, 9] reported that global alignment of the sagittal vertical axis is associated with pain and reduced function, and Lafage et al. [17] found that pelvic tilt is associated with health-related quality of life in the setting of adult deformity, which is consistent with our findings. In fact, in the present study, we found that VAS scores were significantly correlated with sagittal vertical axis and lumbar lordosis and that these spinal parameters were closely related to pelvic orientation.
Some authors have reported a significant correlation between age and spinal sagittal vertical axis and failed to find any other significant correlation between sagittal vertical axis and spinopelvic parameters [25]. In the present study, age and FNBMD were significantly correlated to sagittal vertical axis. This could be predictable because BMD decreases with age. However, our multivariate logistic regression analysis showed that low FNBMD and high pelvic incidence were important determining factors of sagittal balance in osteoporotic patients.
An abnormal kyphotic posture is considered a result of an osteoporotic fracture [5, 6], and it is obvious that vertebral fractures presenting with an anterior wedge deformity are a cause of local kyphosis. However, little is known about regional compensation of the sagittal curvature and of the impact of osteoporotic vertebral fractures on sagittal balance. In this study, osteoporotic patients with or without sagittal balance were no different in terms of the incidence of osteoporotic vertebral fractures. However, this finding should be validated by large population-based study.
This study has several limitations that require consideration. First, the number of normal controls was relatively small, which diminished the statistical power of the study and its ability to detect correlations. Second, only sagittal vertical axis was used for determination of sagittal balance in this study. More relevant indexes which have recently been published to determine the global sagittal balance by analyzing the position of C7 were not utilized. Therefore, further studies will be needed. Third, symptoms were evaluated using VAS scores, and although we excluded symptoms originating from body regions, pain assessments may have been influenced by other joints. Furthermore, VAS scores do not provide an accurate measure of symptoms, and thus, some other complementary scoring systems should have been utilized.
In conclusion, this study shows significant relationships between sagittal spinopelvic parameters in osteoporosis patients. In particular, osteoporotic patients and normal controls were found to differ significantly in terms of sagittal spinopelvic parameters. Furthermore, significant correlations were found between sagittal parameters in osteoporotic patients, and low FNBMD and high pelvic incidence were found to be important predictors of sagittal balance in osteoporotic patients.
Conflict of interest
None.
References
- 1.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61:981–986. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 4.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Smet AA, Robinson RG, Johnson BE, Lukert BP. Spinal compression fractures in osteoporotic women: patterns and relationship to hyperkyphosis. Radiology. 1988;166:497–500. doi: 10.1148/radiology.166.2.3336728. [DOI] [PubMed] [Google Scholar]
- 6.Ensrud KE, Black DM, Harris F, Ettinger B, Cummings SR. Correlates of kyphosis in older women. J Am Geriatr Soc. 1997;45:682–687. doi: 10.1111/j.1532-5415.1997.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 7.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]
- 8.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 9.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 10.Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord. 2003;16:44–50. doi: 10.1097/00024720-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Hasday CA, Passoff TL, Perry J. Gait abnormalities arising from iatrogenic loss of lumbar lordosis secondary to Harrington instrumentation in lumbar fractures. Spine. 1983;8:501–511. doi: 10.1097/00007632-198307000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Hirose D, Ishida K, Nagano Y, Takahashi T, Yamamoto H. Posture of the trunk in the sagittal plane is associated with gait in community-dwelling elderly population. Clin Biomech. 2004;19:57–63. doi: 10.1016/j.clinbiomech.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Jackson RP, Peterson MD, McManus AC, Hales C. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine. 1998;23:1750–1767. doi: 10.1097/00007632-199808150-00008. [DOI] [PubMed] [Google Scholar]
- 15.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–319. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JH, Kim KT, Suk KS, Lee SH, Jeong BO, Kim JS, Eoh JH, Kim YJ. Analysis of spinopelvic parameters in lumbar degenerative kyphosis: correlation with spinal stenosis and spondylolisthesis. Spine. 2010;35:E1386–E1391. doi: 10.1097/BRS.0b013e3181e88be6. [DOI] [PubMed] [Google Scholar]
- 17.Lefage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine. 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 18.Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacThiong JM, Berthonnaud E, Dimar JR, 2nd, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine. 2004;29:1642–1647. doi: 10.1097/01.BRS.0000132312.78469.7B. [DOI] [PubMed] [Google Scholar]
- 20.Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15:1384–1392. doi: 10.1359/jbmr.2000.15.7.1384. [DOI] [PubMed] [Google Scholar]
- 21.Polly DW, Kilkelly FX, McHale KA, Asplund LM, Mulligan M, Chang AS. Measurement of lumbar lordosis: evaluation of intraobserver, interobserver, and technique variability. Spine. 1996;21:1530–1536. doi: 10.1097/00007632-199607010-00008. [DOI] [PubMed] [Google Scholar]
- 22.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 23.Seeman E, Bianchi G, Khosla S, Kanis JA, Orwoll E. Bone fragility in men—where are we? Osteoporos Int. 2006;17:1577–1583. doi: 10.1007/s00198-006-0160-8. [DOI] [PubMed] [Google Scholar]
- 24.Sinaki M, Brey RH, Hughes CA, Larson DR, Kaufman KR. Balance disorder and increased risk of falls in osteoporosis and kyphosis. Osteoporos Int. 2005;16:1004–1010. doi: 10.1007/s00198-004-1791-2. [DOI] [PubMed] [Google Scholar]
- 25.Takeda N, Kobayashi T, Atsuta Y, Matsuno T, Shirado O, Minami A. Changes in the sagittal spinal alignment of the elderly without vertebral fractures: a minimum 10-year longitudinal study. J Orthop Sci. 2009;14:748–753. doi: 10.1007/s00776-009-1394-z. [DOI] [PubMed] [Google Scholar]
- 26.Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis: clinical, radiological and epidemiological studies. Spine. 1988;13:1317–1326. doi: 10.1097/00007632-198811000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Vaz G, Roussouly P, Berthonnaud P, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]