Abstract
Purpose
The purpose of this study is to compare bone union rate between autologous iliac bone and local bone graft in patients treated by posterior lumbar interbody fusion (PLIF) using carbon cage for single level interbody fusion.
Methods
The subjects were 106 patients whose course could be observed for at least 2 years. The diagnosis was lumbar spinal canal stenosis in 46 patients, herniated lumbar disk in 12 patients and degenerative spondylolisthesis in 51 patients. Single interbody PLIF was done using iliac bone graft in 53 patients and local bone graft in 56 patients. Existence of pseudo-arthrosis on X-P (AP and lateral view) was investigated during the same follow up period.
Results
No significant differences were found in operation time and blood loss. Significant differences were also not observed in fusion grade at any follow up period or in fusion progression between the two groups. Donor site pain continued for more than 3 months in five cases (9 %). The final fusion rate was 96.3 versus 98.3 %.
Conclusions
Almost the same results in fusion were obtained from both the local bone group and the autologous iliac bone group. Fusion progression was almost the same. Complications at donor sites were seen in 19 % of the cases. From the above results, it was concluded that local bone graft is as beneficial as autologous iliac bone graft for PLIF at a single level.
Keywords: Posterior lumbar interbody fusion, Autologous iliac bone graft, Local bone graft, Fusion rate
Introduction
To perform a posterior lumber interbody fusion (PLIF), traditionally the required amount of bone for fusion is harvested from autologous iliac crest bone. In recent practice, some of these graft substitutes or autograft expanders such as allografts [1], ceramics [2], demineralized bone matrix [3], recombinant human bone morphogenetic proteins 2 and 7 (rhBMP-2 and 7) [4] and cultured stem cells [5]. Though some are very effective in clinical trials, these methods can be complicated by donor site pain and significantly increased costs. With iliac crest bone harvest, various authors have reported on the occurrence of major or minor complications ranging from 1 to 39 %, which include hematoma, infection, prolonged chronic pain and sensory deficit [6–8] Recently local bone obtained through laminectomy has been reportedly used as stand-alone graft in PLIF procedures showing comparable fusion rates to autologous iliac bone. If true, this could potentially avoid the donor site complications of an iliac crest harvest [9–11]. The purpose of this study is to identify if the bone fusion rates differ between the two groups by examining X-ray images taken at interval follow-up. We hypothesize that adequate laminectomy bone would show similar rates of fusion to autologous iliac bone.
Patients and methods
Patients
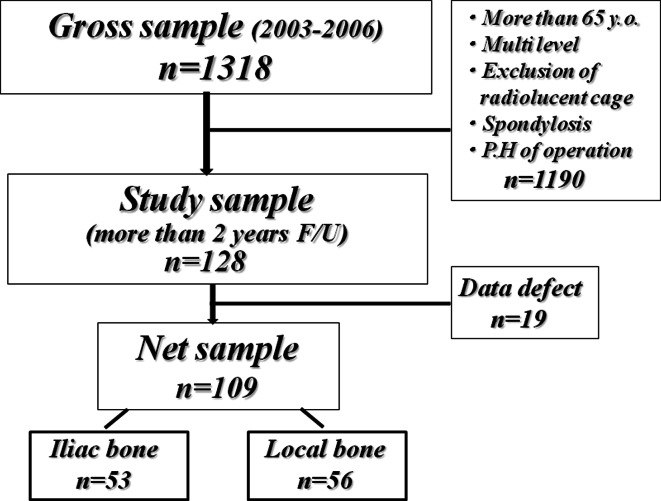
The Nagoya Spine Group consisted of spine surgeons at Nagoya University Hospital and 15 affiliated institutions. Its purpose was to evaluate the surgical treatment of spinal disorders using a prospective and retrospective multicenter clinical study. The Nagoya Spine Group database included 9,096 patients who underwent spine surgery. 1,318 cases were identified who underwent a PLIF including multi-level procedures. Of those cases we examined 109 consecutive patients (59 males and 50 females) with a mean age of 49.5 (19–65 years old) who underwent PLIF from April 2003 to June 2006 retrospectively (Fig. 1). The diagnoses were lumbar disc herniation in 12 cases (including 5 recurrent cases), degenerative lumbar spondylolisthesis in 51 cases, and lumbar spinal canal stenosis in 46 cases which had over 15° instability in the lateral view of the lumber functional X-ray or over 5° local kyphosis angle in the lateral view of the lumber flexion X-ray. For all the patients, PLIF was performed only at a single level: L3/4 for 11 cases (10 %), L4/5 for 82 cases (75 %) and L5/S for 16 cases (15 %). Radiolucent carbon fiber cages (Brantigan, Fa. DePuy-Acromed) were inserted in all of the cases. Autologous iliac bone graft was used in 53 cases and local bone from laminectomy in 56 cases. The cases were non-randomly selected by the surgeon. The average follow-up was 50 months (24–60 months). Body mass index, employment status and smoking history were documented. Those patients with previous back operations (except in recurrent disc herniation), operation for multiple levels, usage of metal cages and lumbar spine spondylolysis were excluded. Appropriate IRB approval was obtained.
Fig. 1.
Flow chart of subjects
Surgical method and bone grafting
PLIF was performed using almost the same technique at each hospital. Only two-thirds of the upper lamina toward fusion area was excised to minimize instability, maintaining integrity of the interspinous and supraspinous ligaments connected to one level upper spinous process. Titanium pedicle screws and rods were used for fixation and reduction of degenerative instability was performed. Disc and cartilaginous endplates were removed to prepare the graft bed and the harvested iliac bone or local bone chips morcelized by bone-milling were implanted in the anterior and lateral portion of the interbody space. This was followed by insertion of two carbon cages filled with grafts and reduction of degenerative instability was performed. Posterolateral fusion was not conducted on any of the cases.
Radiographic assessment
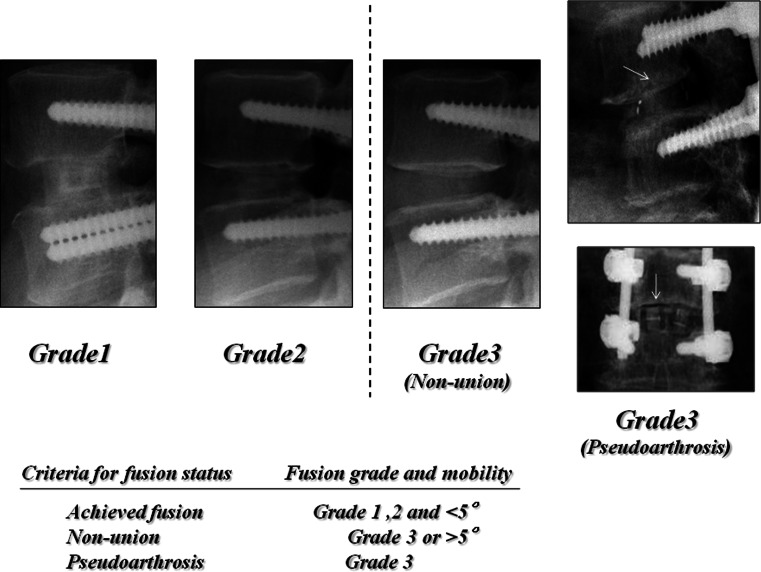
AP and lateral images were obtained at 3, 6, 12, and 24 months postoperatively. Each image was blinded and evaluated by two spinal surgeons. These images were then classified into one of four grades:
Grade 1 Complete fusion achieved with bone bridge formed between the upper and lower vertebral bodies;
Grade 2 Bone bridge not formed, but no translucency observed around the cages, and thick fusion mass formed;
Grade 3 Fusion not achieved, and translucency seen around the cages, pointing to non-union or bone resorption around cages, which indicates pseudoarthrosis (Fig. 2) [12].
Fig. 2.
Bone fusion grade classification
Standing flexion–extension X-rays were also obtained to identify instability. Instability was defined on the basis of abnormal mobility (3 mm or more listhesis, 2 mm or more translation from flexion to extension, 5° or more abnormal tilting movement of the posterior elements in flexion, localized lateral slip, and lateral tilting). When 1 mm or greater circumferential lucency was found around a screw, the patient was judged clear-zone positive. Based on this angle and the above-defined grades, prevalence of bone fusion was determined. The result was labeled as “achieved fusion” when rated Grade 1 or Grade 2 with a flexion–extension angle of less than 5°, “non-union or pseudoarthrosis” when rated Grade 3 or with flexion–extension angle measuring 5° or more. If pseudoarthrosis or non-union was suspected, a confirming CT scan was performed. Other recorded items were clinical operative data, postoperative X-ray assessment (slip percentage, intervertebral angle, and disc height) and perioperative complications. The clinical outcomes at 2 years were also obtained using the Japanese Orthopaedic Association (JOA) scale. Statistical analysis was performed using the χ2 test and paired t test.
Results
Baseline clinical data including age, sex, BMI, employment status, smoking habit and diagnosis exhibited no significant differences between the two groups (Table 1). The duration of surgery was 202 versus 197 min (ICBG vs. local bone group). The blood loss was 408 versus 353 ml. The preoperative and postoperative slippage degrees were 9.0 versus 5.5 % and 5.3 versus 2.7 %, respectively [pre-op (ICBG vs. local bone) and post-op (ICBG vs. local bone)]. The preoperative and postoperative intervertebral angle examined radiographically was 1.4° versus 1.9° and 7.4° versus 7.3°, respectively [pre-op (ICBG vs. local bone) and post-op (ICBG vs. local bone)]. The preoperative and postoperative disc heights were 8.7 versus 9.7 mm and 12.7 versus 12.8 mm [pre-op (ICBG vs. local bone) and post-op (ICBG vs. local bone)]. As stated above, the results of X-ray assessment conducted after the surgery were almost equal between the two groups. JOA score observed at each given interval also revealed no significant difference with final recovery rate of 80.5 versus 82.7 %.
Table 1.
Baseline clinical data
| Iliac bone (n = 53) | Local bone (n = 56) | ||
|---|---|---|---|
| Age | 50.1 ± 13.4 | 48.6 ± 15.3 | n.s |
| Sex (male:female) | 26:27 | 33:23 | n.s. |
| BMI | 24.1 ± 3.9 | 23.7 ± 3.2 | n.s. |
| Smoking | 16/53 | 17/56 | n.s. |
| Employment | |||
| Employed full time | 16 | 17 | |
| Employed parttime | 3 | 3 | |
| Unemployed | 34 | 36 | n.s. |
| Disease | |||
| Disc hernia | 6 | 6 | |
| Spondylolisthesis | 26 | 25 | |
| Canal stenosis | 21 | 25 | n.s. |
| Level | |||
| L3/4 | 4 | 7 | |
| L4/5 | 44 | 38 | |
| L5/S | 5 | 11 | n.s. |
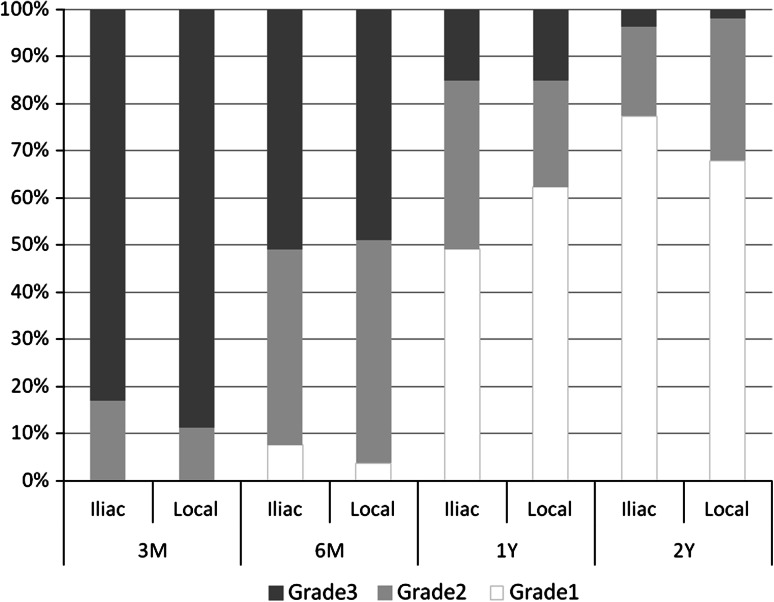
There was no significant difference in intervertebral flexion–extension angle throughout the follow-up period: 3 months: 1.2° versus 1.1°; 6 months: 0.8° versus 0.7°; 1 year: 0.8° versus 0.6°; 2 years: 0.4° versus 0.3° (ICBG vs. local bone group). The same could be said for the fusion grade that indicated fusion progression. The proportion of cases estimated as Grade 1 or 2 was 9 of 53 cases (17 %) versus 6 of 53 cases (11 %) at 3 months, 26 (49 %) versus 27 (51 %) at 6 months, 45 (85 %) versus 46 (87 %) at 1 year, and 51 (96 %) versus 52 (98 %) at 2 years. Non-union or pseudoarthrosis cases rated as Grade 3 after 2 year were 2 of 53 (3.7 %) versus 1 of 56 cases (1.7 %) (Fig. 3). The final fusion rate was 96.3 % for the ICBG group and 98.3 % for the local bone group. Pseudoarthrosis was seen at L4/5 in 2 cases, and L5/S in 1 case.
Fig. 3.
The degree of fusion progress
Complications observed in the iliac bone group were three cases of pedicle screw misplacement (none of the cases resulted in neurological deficit), one case of superficial wound infection and nine cases (17 %) of prolonged donor site pain for more than 1 month. This donor site pain continued for more than 3 months in five cases (9 %). As for the local bone group, pedicle screw misplacement was seen in four cases (none of the cases displayed neurological deficit). All of the three cases with pseudoarthrosis were judged clear-zone positive.
Discussion
Since Cloward reported on the technique of PLIF, the iliac crest has been considered an ideal source of graft, in terms of quantity and quality, to achieve solid bone fusion. Nevertheless, problems with harvesting iliac bone have included donor site pain, pelvic instability, and fractures of the pelvis. As a result, many orthopedic surgeons have investigated potential bone graft substitutes such as harvested local bone, allografts, ceramics, demineralized bone matrix, rhBMP-2 and 7 cultured stem cells [1–5]. In particular, synthetic materials may be very useful because they can be provided in an infinite supply, they are easily sterilized and stored, and the significant risk of disease transmission by allograft bone is avoided. These positive gains must be weighed against the significant increased cost of synthetics as well as potentially poor osteoinductivity. In assessing iliac bone harvest, one must also consider increased operative time, blood loss, and postoperative pain. Furthermore, there is no difference in cost between iliac bone and local bone grafts.
Therefore, it is beneficial for the patients if an iliac bone harvest can be avoided [6–8].
It was demonstrated that there is no significant difference in bone fusion achievement between those patients treated with local laminectomy bone and those with harvest iliac crest bone graft. We reported about a retrospective study conducted at a single facility previously [13], whereas the present study is a retrospective study conducted at multiple facilities. As at the single facility, the result indicates no difference between iliac bone and local bone grafts at the multiple facilities. In other words, it is shown that similar results can be obtained with different operators and different environments. Past reports showed that the fusion rate achieved by the autologous iliac bone grafting was as high as 90–100 % [14–16]. Miura et al. [10] reported fusion rate of 100 % in their 12-month follow-up study of autograft implantation, and Hashimoto et al. [17] reported fusion rate of 100 % at 2 years after PLIF where local bone mixed with AW glass ceramics was grafted in a single intervertebral space. However, these studies retrospectively reported on using one graft without simultaneous comparison of autologous iliac bone and local bone graft. Also some studies included both single and multilevel PLIF treated cases. This makes it difficult for the clinician to make a simple comparison of fusion rate between the autologous iliac crest and local bone harvest.
There were a few studies that followed up fusion progression over time. Miura et al. [10] found the fusion rates to be 72.4 % after 6 months and 100 % after 12 months, and Kim et al. [18] observed the fusion mass around cages and found 10 % to be present after 6 months and 35 % after 12 months. Diedrich et al. [19] reported that few fusion cases were seen within 6 months and fusion took 20.7 months in average. However, none of the above assessed intervertebral instability at given intervals in bone fusion progression. In contrast, we employed bony mass assessment using X-ray for stricter fusion evaluation and found that about half of the cases achieved bone fusion at 6 months and almost all cases achieved bone fusion within 1 year.
Many authors have reported on iliac bone donor site complications, which ranged from 1 to 39 % depending on the literature. Banwart et al. [20] studied 225 cases and found 10 % had major complications including hematoma, infection, reoperation, chronic pain and 39 % minor complications including sensory deficit, drain disorder and superficial infection. The 106 cases researched by Robertson and Wray et al. [21], included patients who suffered from aggravated donor site pain and sensory deficit for 6 months before those symptoms were alleviated, and thus revealed the possibility of various problems accompanying iliac bone harvest. We also observed donor site pain continuing more than 1 month in 17 % of patients, five of whom (9 %) suffered from prolonged pain for more than 3 months. Therefore, it is beneficial for the patients if iliac bone harvest can be avoided. And the high fusion rate proved that local bone graft is enough to PLIF procedure in any aspects of complication, costs and availability outside the developed countries.
We understand that the present study has some limitations. Firstly, only single level PLIF cases were studied. Local bone harvest from the laminectomy may not be adequate for a multilevel PLIF procedure. According to Dirip et al. [22], posterolateral fusion (PLF) had no significant differences between the two groups when it was employed for a single level, but the local bone graft group had apparently lower fusion rates when it comes to multilevel PLF treatment. Secondly, radiologic assessment of fusion is never perfect. In this study, a CT scan was not available in most cases because patients did not have a CT scan in each follow-up period. Fusion was therefore assessed from plain radiograph and flexion–extension views by a blind observer. Ideally, a CT scan with 2 mm slices and sagittal reconstructions would provide a better tool to assess fusion status. Thirdly, some variations in surgical technique could not be avoided in the multicenter study; we have reviewed the data at the individual centers showing no overall fusion rate difference (data not shown). Since this is a retrospective comparative study, we might have been somewhat biased in selecting our operation method. With RCT it is possible to exclude almost all study limitations as stated above. Additionally, RCT is relatively easy to perform and should be employed in future study. In conclusion, our data suggest that local bone graft is as beneficial as autologous iliac bone graft for PLIF at a single level.
Conflict of interest
None.
References
- 1.An HS, Lynch K, Toth J. Prospective comparison of autograft vs. allograft for adult posterolateral lumbar spine fusion: differences among freeze-dried, frozen, and mixed grafts. J Spinal Disord. 1995;8:131–135. doi: 10.1097/00002517-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Le Huec JC, Lesprit E, Delavigne C, et al. Tri-calcium phosphate ceramics and allografts as bone substitutes for spinal fusion in idiopathic scoliosis: comparative clinical results at four years. Acta Orthop Belg. 1997;63:202–211. [PubMed] [Google Scholar]
- 3.Frenkel SR, Moskovich R, Spivak J, et al. Demineralized bone matrix. Enhancement of spinal fusion. Spine. 1993;18:1634–1639. doi: 10.1097/00007632-199309000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Holliger EH, Trawick RH, Boden SD, et al. Morphology of the lumbar intertransverse process fusion mass in the rabbit model: a comparison between two bone graft materials-rhBMP-2 and autograft. J Spinal Disord. 1996;9:125–128. doi: 10.1097/00002517-199604000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Tay BK, Le AX, Heilman M, et al. Use of a collagen-hydroxyapatite matrix in spinal fusion. A rabbit model. Spine. 1998;23:2276–2281. doi: 10.1097/00007632-199811010-00005. [DOI] [PubMed] [Google Scholar]
- 6.Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3:192–195. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Keller EE, Triplett WW. Iliac bone grafting: review of 160 consecutive cases. J Oral Maxillofac Surg. 1987;45:11–14. doi: 10.1016/0278-2391(87)90079-6. [DOI] [PubMed] [Google Scholar]
- 8.Summers BN, Eisenstein SM. Donor site pain from the ilium: a complication of lumbar spine fusion. J Bone Joint Surg Br. 1989;71:677–680. doi: 10.1302/0301-620X.71B4.2768321. [DOI] [PubMed] [Google Scholar]
- 9.Violas P, Chapuis M, Bracq H. Local autograft bone in the surgical management of adolescent idiopathic scoliosis. Spine. 2004;29:189–192. doi: 10.1097/01.BRS.0000105536.65164.B1. [DOI] [PubMed] [Google Scholar]
- 10.Miura Y, Imagama S, Yoda M, et al. Is local bone viable as a source of bone graft in posterior lumbar interbody fusion? Spine. 2003;28:2386–2389. doi: 10.1097/01.BRS.0000085326.73430.68. [DOI] [PubMed] [Google Scholar]
- 11.Hashimoto T, Oha F, Shigenobu K, et al. Mid-term clinical results of Graf stabilization for lumbar degenerative pathologies: a minimum 2-year follow-up. Spine J. 2001;1:283–289. doi: 10.1016/S1529-9430(01)00028-6. [DOI] [PubMed] [Google Scholar]
- 12.Tsuchiya K, Bridwell KH, Kuklo TR et al (2006) Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine 31(3):303–308 [DOI] [PubMed]
- 13.Ito Z, Matsuyama Y, Sakai Y et al (2010) Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion. Spine 35(21):E1101–E1105 [DOI] [PubMed]
- 14.Brantigan JW, Steffee AD, Lewis ML, et al. Lumbar interbody fusion using the Brantigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine. 2000;25:1437–1446. doi: 10.1097/00007632-200006010-00017. [DOI] [PubMed] [Google Scholar]
- 15.Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg. 1999;91:186–192. doi: 10.3171/spi.1999.91.2.0186. [DOI] [PubMed] [Google Scholar]
- 16.Christensen FB, Hansen ES, Eiskjaer SP, et al. Circumferential lumbar spinal fusion with Brantigan cage versus posterolateral fusion with titanium Cotrel-Dubousset instrumentation: a prospective, randomized clinical study of 146 patients. Spine. 2002;27:2674–2683. doi: 10.1097/00007632-200212010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Hashimoto T, Shigenobu K, Kanayama M, et al. Clinical results of single-level posterior lumbar interbody fusion using the Brantigan I/F carbon cage filled with a mixture of local morselized bone and bioactive ceramic granules. Spine. 2002;27:258–262. doi: 10.1097/00007632-200202010-00011. [DOI] [PubMed] [Google Scholar]
- 18.Kim KS, Ki YT, Lee JC. Radiological changes in the bone fusion site after posterior lumbar interbody fusion using carbon cages impacted with laminar bone chips: follow-up study over more than 4 years. Spine. 2005;30:655–660. doi: 10.1097/01.brs.0000155421.07796.7f. [DOI] [PubMed] [Google Scholar]
- 19.Diedrich O, Perlick L, Schmitt O, et al. Radiographic characteristics on conventional radiographs after posterior lumbar interbody fusion: comparative study between radiotranslucent and radiopaque cages. J Spinal Disord. 2001;14:522–532. doi: 10.1097/00002517-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity: a statistical evaluation. Spine 20:1055–1060 [DOI] [PubMed]
- 21.Robertson PA, Wray AC. Natural history of posterior iliac crest bone graft donation for spinal surgery: a prospective analysis of morbidity. Spine. 2001;26:1473–1476. doi: 10.1097/00007632-200107010-00018. [DOI] [PubMed] [Google Scholar]
- 22.Sengupta DK, Truumees E, Patel CK et al (2006) Outcome of local bone versus autogenous iliac crest bone graft in the instrumented posterolateral fusion of the lumbar spine. Spine 31:985–991 [DOI] [PubMed]