Abstract
Introduction
Many studies regarding spinal sagittal alignment were focused mainly on above-hip structures, not considering the knee joint. Knee–spine syndrome was proposed earlier, but the mechanism of this phenomenon has not been revealed. The aim of the study was to demonstrate how spinopelvic alignment and sagittal balance change in response to simulated knee flexion in normal non-diseased population.
Methods
Thirty young male were enrolled in the study cohort. Two motion-controlled knee braces were used to simulate knee flexion of 0°, 15°, and 30° settings. Whole spine and lower extremity lateral radiographs were taken at each knee setting of 0°, 15°, and 30° flexion. Spinal and pelvic parameters were measured, including two angular parameters, femoropelvic angle (FPA) and femoral tilt angle (FTA).
Results
The following equation can be made; PT (pelvic tilt) = FPA + FTA. The mean values of FPA and lumbar lordosis decreased significantly at 15° and 30° knee settings compared to the parameters at the 0° knee setting, while the mean values of pelvic tilt and sacral slope rarely changed. Results also showed FTA was not correlated with PT, but strongly correlated with FPA (R = −0.83, p < 0.01).
Conclusions
The knee flexion resulted in decrease of lumbar lordosis without a significant change of pelvic posture in non-diseased population group.
Keywords: Simulation, Knee flexion, Femoral tilt angle, Femoropelvic angle, Lumbar lordosis, Pelvic posture
Introduction
With aging population increased, there are many patients who have multiple degenerative diseases. The knee and spine are two of the most commonly affected sites of degenerative diseases. Therefore, it is not uncommon to encounter the patients who had combined knee and spine problems such as knee flexion contracture as well as sagittal spinal imbalance.
With regard to a reciprocal relationship between knee and spine, it has been well known that sagittal imbalance leads to adaptive changes in the pelvis, hip, and knee joint through a compensatory mechanism [5, 10, 12]. To maintain an upright posture, the patient tilts the pelvis backwards, extends the hips and flexes the knees in order to shift the entire rigid spine backwards [12]. However, the reverse way, the effect of knee position on spinal column has rarely been addressed. Murata et al. [11] examined 366 patients with knee pain or low back pain. They observed that the limitation of knee extension was correlated with decrease in lumbar lordosis. They postulated that symptoms from the lumbar spine may be caused by degenerative change in the knee and called this phenomenon as “knee–spine syndrome”. They could suggest the relationship between the knee and spine, but failed to reveal whether the knee flexion limitation results in loss of lumbar lordosis and lumbar spinal symptoms, or vice versa.
In order to elucidate the actual effect of knee flexion on spinal column, it might be helpful to observe the change of spinal alignment or symptoms after eliminating the flexion contracture, e.g., by total knee arthroplasty. Before dealing with the patients with degenerative conditions, we thought it should be taken priority to know the normal response of the spinal column and pelvis to the knee flexion. Thus, this study was designed to demonstrate the normal response of the spinal column to the simulated bilateral knee flexion for healthy young adults who have no pathology in the knee and spine. In addition, we introduced two new parameters to describe the relationship between the knee and pelvic posture. The application of these two parameters in interpreting the spinopelvic alignment will be addressed in discussion section.
Materials and methods
Subjects
The current study was performed under IRB approval in our institute. Thirty young male volunteers were enrolled for the study cohort. They were in 20s or 30s of age with no history of spinal diseases and no radiological abnormalities in the spine. Subjects with a history of hip, knee, ankle diseases were excluded. They were all male with a mean age of 30.4 years (range 26–37).
Simulation of knee flexion and radiographic measurement
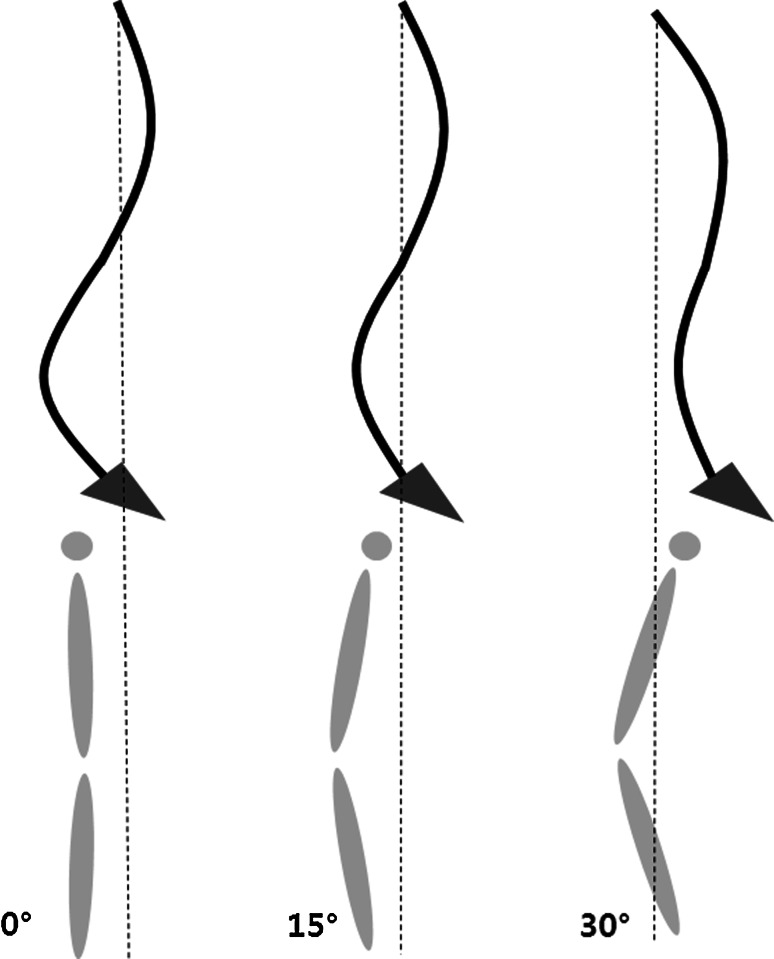
All subjects were asked to put on motion-controlled knee braces on the bilateral knees to produce the knee flexion (Fig. 1). Two different knee settings of 15° and 30° flexion was simulated using this brace. The study was carried out in three steps that consisted of the standing position without the brace and with a 15°-fixed, and 30°-fixed brace. In the current paper, we named the standing position without the brace as 0° position for simplicity.
Fig. 1.

Photograph shows a subject putting on two motion-controlled knee braces
At each step, 14 × 36-in. lateral whole spine and lower extremity lateral radiographs were taken with a 72-in. distance between the subject and radiographic source. Before taken the radiographs of each step, the subjects were asked to wear the brace for 5 min to give a sufficient time so that the simulated knee flexion works. The subjects were instructed to stand in a comfortable position with the fist-on-clavicle position. After taking required position, the subjects had whole spine radiograph taken first followed by lower extremity radiograph, and were asked to keep the position during the term between the two radiographic examinations. The time between the whole spine and lower extremity radiographs took about 10 s. The radiograph of the whole spine was centered on the 12th thoracic vertebra and the radiograph of the lower extremity was centered on the proximal thigh to encompass the cranial endplate of S1 proximally and the knee joint distally.
Parameters
Four parameters were measured on each whole spine radiograph. The lumbar lordosis (LL) is the Cobb’s angle between the cranial endplate of L1 and S1. The thoracic kyphosis (TK) is the Cobb’s angle between the cranial endplate of T4 and T12. The sagittal balances were measured by the perpendicular distance from the plumb line of the center of C7 body to the superoposterior corner of S1 (B1) and the bicoxofemoral axis (B2) to represent the spinal and spinopelvic balance, respectively [17]. The sagittal balance was defined as negative when the C7 plumb line fell behind each reference point.
Five pelvic parameters were measured on each lower extremity radiograph. The measurements of sacral slope (SS), pelvic tilt (PT), and pelvic incidence (PI) confirm with the currently used methods [17].
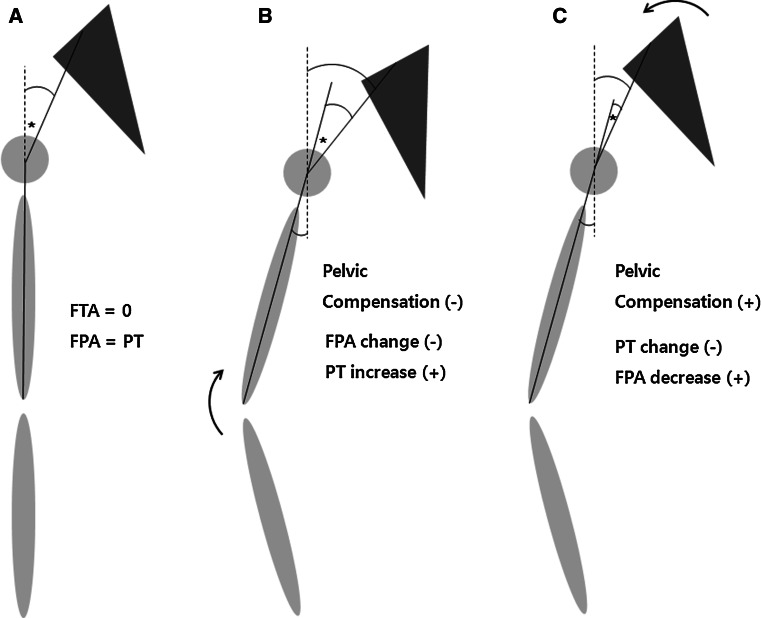
Two angular parameters, the femoral tilt angle (FTA) and femoropelvic angle (FPA), were introduced [9, 13]. The FTA was defined as the angle between a vertical axis and the sagittal femoral axis to represent femoral inclination caused by knee flexion (Fig. 2). The sagittal femoral axis was defined as the line connecting the center of the bicoxofemoral axis and the center of the distal femur. However, the center of the distal femur was difficult to identify because of the metallic hinge images of the knee braces. Hence, an alternative distal reference point was used; the midpoint of two femoral diaphyseal centers at the level of the upper pole of the two patellae. The FPA was defined as the angle between the sagittal femoral axis and a line joining the middle of the cranial S1 endplate to the center of the bicoxofemoral axis (Fig. 2). All radiographs were digitalized into PACS, and measurements were performed using software (Sagimeter®, Optimum Solution Co. Ltd., Bundang, Gyoenggi, Korea).
Fig. 2.
New pelvic parameters; FPA and FTA (asterisk). Note that PT is equal to the sum of FPA and FTA
Analysis
Three different sets of parameters were obtained from one subject according to the three different knee settings of 0° (without brace), 15°, and 30°. The analysis was performed in three steps. First, the mean values of each parameter obtained at the different knee settings were compared each other using a paired t test. Second, the relationship between all parameters was investigated using the Pearson correlation test.
Results
Relationship among the angular parameters
By definition, FPA is determined by the position of both the femur and pelvis, which is represented by FTA and PT. Figure 2 shows a simple equation; PT = FPA + FTA. This equation was proposed earlier by Roussouly and Pinheiro-Franco [13].
Mean values of parameters at three different knee settings
Table 1 lists the mean values of all parameters at each knee setting. Compared to the parameters at the 0° knee setting, the mean values of FPA and LL decreased significantly at 15° and 30° (p < 0.001 for both FPA and LL between 0° and 15° and between 0° and 30°) and the mean values of B1 and B2 increased significantly at 15° and 30° (p = 0.002 for B1 between 0° and 15°, p = 0.032 for B2 between 0° and 15°, p < 0.001 for both B1 and B2 between 0° and 30°). The change of PT and SS at the 15°, 30° knee setting was not significant compared with 0° knee setting. The three different postures are described schematically in Fig. 3 based on the mean value of parameters at each knee setting.
Table 1.
Mean values and changes of all parameters at each knee setting
| Parameters† | 0° (n = 30) | 15° (n = 30) | 30° (n = 30) |
|---|---|---|---|
| FTA (°) | −2.5 ± 3.0 | 10.1 ± 5.9‡ | 17.8 ± 7.8‡ |
| FPA (°) | 16.4 ± 7.3 | 5.1 ± 10.6‡ | −2.3 ± 13.1‡ |
| PT (°) | 13.9 ± 5.3 | 15.2 ± 7.3 | 15.5 ± 8.7 |
| SS (°) | 36.4 ± 7.0 | 35.7 ± 8.9 | 34.9 ± 9.9 |
| PI (°) | 50.4 ± 9.1 | 50.9 ± 8.9 | 50.4 ± 9.5 |
| LL (°) | 50.7 ± 8.7 | 45.9 ± 10.5‡ | 42.7 ± 10.3‡ |
| TK (°) | 31.5 ± 7.0 | 33.1 ± 7.8 | 30.7 ± 6.7 |
| B1 (mm) | −1.2 ± 19.6 | 23.1 ± 36.4‡ | 47.6 ± 43.5‡ |
| B2 (mm) | −45.2 ± 18.8 | −27.5 ± 39.9‡ | 5.5 ± 53.2‡ |
Values are given by mean ± SD
FPA femoropelvic angle, PT pelvic tilt, SS sacral slope, PT pelvic incidence, LL lumbar lordosis, TK thoracic kyphosis, B1 distance between C7 plumb line and S1 posterior corner, B2 distance between C7 plumb line and bicoxofemoral axis
†FTA indicates femoral tilt angle
‡Significantly different compared with parameters at 0° knee setting (p < 0.05)
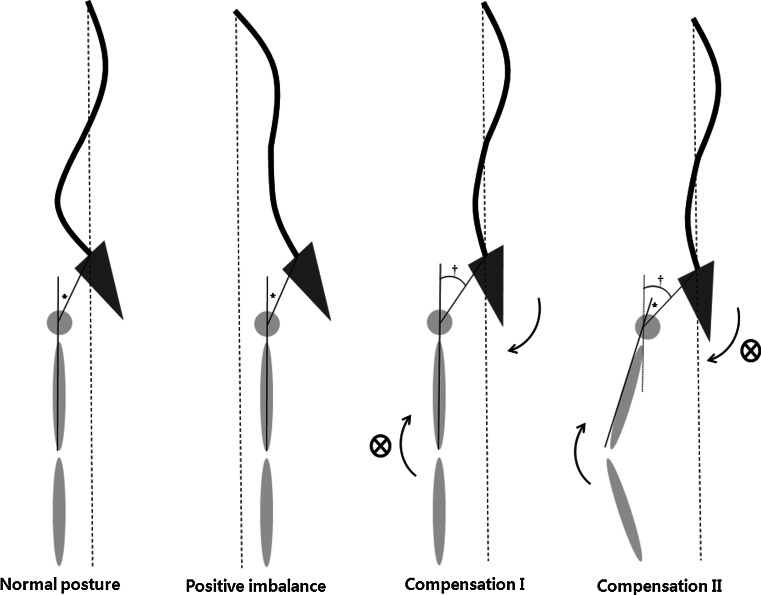
Fig. 3.
Schematic diagrams of the three different postures based on the mean value of parameters at each knee setting. Note that as the angle of knee flexion increases, lumbar lordosis decreases, and sagittal balance shifts anteriorly, while pelvic tilt and sacral slope rarely changed
Correlations among all parameters
The correlations between all parameters are summarized in Table 2. We observed a very strong correlation between FTA and FPA, between SS and LL, and between B1 and B2 (cc > 0.7). There was also large correlation between FTA and B1, between FPA and PT, between FPA and B2, and between SS and PI (cc > 0.5) [3]. However, there were no correlations between FTA and pelvic parameters such as PT, SS, and PT.
Table 2.
Matrix of correlation among all of the parameters (n = 90)
| FTA | FPA | PT | SS | PI | LL | TK | B1 | B2 | |
|---|---|---|---|---|---|---|---|---|---|
| FTA | 1 | −0.83† | −0.07 | −0.16 | −0.20 | −0.41† | 0.00 | 0.54† | 0.49† |
| FPA | 1 | 0.61† | −0.08 | 0.42† | 0.21 | −0.01 | −0.45† | −0.59† | |
| PT | 1 | −0.36† | 0.46† | −0.20 | −0.02 | −0.04 | −0.36† | ||
| SS | 1 | 0.67† | 0.81† | −0.13 | 0.19 | 0.36† | |||
| PI | 1 | 0.61† | −0.14 | 0.15 | 0.05 | ||||
| LL | 1 | 0.02 | −0.26†† | −0.10†† | |||||
| TK | 1 | −0.05 | −0.06 | ||||||
| B1 | 1 | 0.89† | |||||||
| B2 | 1 |
Correlation coefficient (R value) after the Pearson correlation test
†Statistically significant with p value of <0.01
††Statistically significant with p value of <0.05
Discussion
The sagittal standing posture depends not only on the spinal alignment, but also on the hip and knee joint alignment. Currently many studies addressing sagittal spinal alignment were focused mainly on the alignment of above-hip structures, i.e., the hip, pelvis, and spinal column [1, 2, 4, 6, 14, 15, 17]. However, there were few reports including the knee in evaluating sagittal spinal alignment.
Considering many patients have both knee osteoarthritis causing unilateral or bilateral flexion contracture and spine problems such as low back pain or sagittal imbalance, we hypothesized knee flexion contracture caused by knee osteoarthritis would affect the spinal column. The investigation of the change in spinal sagittal alignment and lumbar symptoms after removal of knee flexion contracture by total knee arthroplasty will be one of the feasible methods to prove this hypothesis. However, it is nearly impossible to reveal the subsequent change of spinal column as to the knee flexion contracture in case the patients have concurrent diseases at the knee and spine. We wished to know the change of spinopelvic alignment and spinal sagittal balance as to the different knee positions, so the current study was designed simulating knee flexion in normal populations. Two new parameters, FTA and FPA, were used to describe the relationship between the femur and pelvis.
The current data show that FTA was correlated negatively with LL and positively with B1 and B2. This means that knee flexion resulted in loss of lumbar lordosis and anterior shift of sagittal balance. The mean decreases of FPA were 11.3° and 18.7° at 15° and 30° settings while the mean increases of PT were just 1.3° and 1.6° at 15° and 30° settings. Results also show FTA was not correlated with PT, but FTA was strongly correlated with FPA (cc = −0.83, p < 0.01). Taken together, this means that knee flexion did not influence the position of pelvis significantly, while it did cause loss of lumbar lordosis and anterior shift of sagittal balance.
Some might wonder the fact that knee flexion results in a forward push of sagittal balance because that is counterintuitive to what we normally see. In pathologic patients who stand with a forward sagittal imbalance, knee flexion actually helps compensate their spinal malalignment even without changing their pelvic parameters. The important point is what is a primary factor, the knee or spine. We focused on the knee condition primarily and the subsequent change of spinal column secondarily. Thus, the current results should be discriminated from the phenomenon found in the patients with fixed sagittal imbalance.
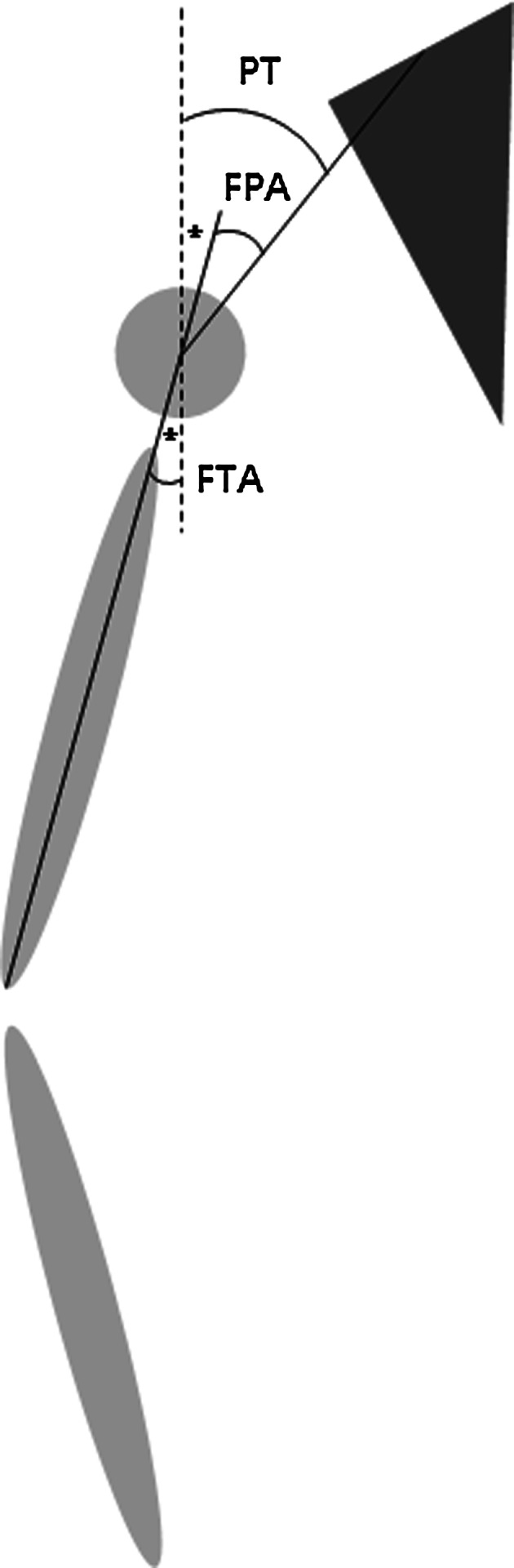
The results were further analyzed in terms of the concept of compensation. Figure 4 compares two different postures in response to knee flexion and gives a detailed explanation of spinopelvic alignment including the knee joint. Figure 4a shows a person standing without knee flexion and hip flexion where FTA is 0° and FPA is equal to PT. Figure 4b shows as to the knee flexion the relationship between the femur and pelvis is unchanged, which means that knee flexion is not compensated by the pelvis. Because the pelvis does not rotate around the axis of the femoral head, FPA does not change compared with Fig. 4a. However, PT does increase as much as FTA increases. On the other hand, Fig. 4c shows as to the knee flexion the pelvis remains unchanged where PT does not change. However, from the standpoint of the femur, the pelvis rotates anteriorly around the axis of the femoral head where FPA decreases as much as FTA increases. The current results can be well explained (Fig. 4c).
Fig. 4.
Two different responses according to the knee flexion. a Standing without knee and hip flexion. The angle of FPA (asterisk) is equal to PT. b No pelvic compensation. Note that FPA does not change and PT increases with knee flexion. c Pelvic compensation. Note that PT does not change and FPA decreases with knee flexion
It has been known that the key parameters representing pelvic compensation is PT in evaluation of sagittal imbalance [7, 16]. However, considering the knee joint and femur together, Fig. 4b shows no pelvic compensation occurs in spite of PT increase while Fig. 4c shows pelvic compensation occurs without PT change. These findings suggest that PT might not represent the pelvic rotation or pelvic compensation properly when considering the posture of the femur and knee joint. FPA, determined by the relationship between the femur and pelvis, describes better the pelvic rotation as to the femur. Thus, we assume that FPA would be a suitable parameter for representing pelvic rotation or compensation if the patient have flexion contracture of the knee or hip. We suggest that FPA can represent true pelvic compensation and PT can represent apparent pelvic compensation.
Here, it needs to re-look the terminology for describing the compensation of the sagittal plane imbalance. A positive imbalance of spinal curvature induces a compensatory mechanism, which consists of retroversion of the pelvis, hip extension, knee flexion, and ankle dorsiflexion [7, 8, 18]. The terms, “pelvic retroversion” and “hip extension”, need to be clarified because it possibly lacks a reference point to measure. As outlined earlier, the femur has an inseparable relationship with the pelvis. Therefore, the description of pelvic compensation should include the femur as the reference point. Figure 5 shows two different compensatory postures. Both of two compensatory postures render the sagittal balance shift posteriorly and PT appears to be approximately about the same. The pelvis apparently looks retroverted in both postures, compensation I occurs only by pelvic retroversion and hip extension without knee flexion and compensation II occurs by knee flexion without pelvic retroversion or hip extension. It should be of note that FPA is increased in compensation I and decreased in compensation II. Given that the knee and hip posture should be included for the an assessment of the sagittal imbalance and its compensation, it was assumed that FPA could serve as an important angular parameter to describe the compensatory posture in addition to PT.
Fig. 5.
Two different compensating postures for positive sagittal imbalance. Compensation I occurs only by pelvic retroversion or hip extension without knee flexion. Compensation II occurs by knee flexion without pelvic retroversion or hip extension. It should be noted that although PT (dagger) in both compensatory postures appears similar, FPA (asterisk) increases in compensation I and decreases in compensation II
Our findings should be distinguished from the conventional compensating mechanism to the severe kyphosis (Table 3). In case of fixed sagittal imbalance where the spine is rigid, the first response to compensate imbalance is pelvic retroversion and hip extension. If hip extension reaches its limitation, flexion of the knees may occur. Pelvic retroversion makes PT increase and knee flexion makes more increase of PT. Thus, because of the stiffness of lumbar spine, loss of LL is well correlated with the increase of PT. In the our study, in case of experimental knee flexion contracture, trunk tends to move backward. We think the lumbar spine would response first to maintain the balance because the lumbar spine is flexible. The pelvis does not need to rotate, so the hip has the flexion posture. PT was the product of an adaptation of the pelvic position between the femoral shaft and lumbar spine. If the lumbar spine is flexible, PT will not be directly correlated to LL. Decrease of LL is influenced directly by the flexion of knees, thus loss of LL is correlated with FTA, which represents the degree of knee flexion.
Table 3.
Different compensating mechanisms according to the primary events
| Primary event | Severe kyphosis | Knee flexion contracture |
|---|---|---|
| Trunk movement | Forward | Backward |
| Stiffness of lumbar spine | Stiff | Flexible |
| Primary compensation | Pelvic retroversion | Decrease of LL |
| Secondary compensation | Hip extension | Hip flexion |
| Knee flexion | No pelvic rotation | |
| Correlation | LL ∝ PT | LL ∝ FTA |
We acknowledge that the current study has several limitations. Although we put a short period (10 s), there can be some normal swaying of the subjects that may render their sagittal balance somewhat variable over a course of two sets of radiographs. The EOS system would enable more accurate analysis of spinopelvic balance and knee position. The brace could simulate knee flexion, but it cannot represent the real flexion contracture as seen in patients with a longstanding established flexion contracture. However, it is impossible to make a long-period flexion contracture in normal subjects. Instead, we gave 5 min before taking radiograph of each step to secure the sufficient time. The relative small volume of the study is a potential source of bias. Enrolling a sufficient number of subjects was difficult because this study was carried out targeting young asymptomatic volunteers and the six-time radiation exposures might be onerous. Finally, it is not sure that this experimental study reflects the pathologic condition because it is relatively rare to find bilateral knee flexion contracture due to arthritis. A unilateral flexion contracture would give an effect of leg discrepancy rather than trunk displacement.
In current study, we revealed that the knee position can affect the spinopelvic alignment and sagittal balance by the quantitative measurements of the pelvic and spinal parameters for normal population. Considering many patients have combined spine and knee degenerative disease, and understanding the relationship between the knee and spine is as important as that of above-hip structures when evaluating and managing these patients properly. The two angular parameters, FTA and FPA, could be utilized to interpret the complex association of the knee joint, femur, hip joint, and pelvis. We hope that the current data can serve as a basic background for the future study.
Acknowledgments
The current study was supported by Central Research Fund (nonprofit academic fund) from our institute. This study was conducted under approval of IRB.
Conflict of interest
None.
References
- 1.Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine (Phila Pa 1976) 1989;14:717–721. doi: 10.1097/00007632-198907000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 3.Cohen J. Statistical power analysis for the behavioural sciences. 2. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 4.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976) 1995;20:1351–1358. [PubMed] [Google Scholar]
- 5.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 6.Jackson RP, Hales C. Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers. Spine (Phila Pa 1976) 2000;25:2808–2815. doi: 10.1097/00007632-200011010-00014. [DOI] [PubMed] [Google Scholar]
- 7.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 8.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mangione P, Senegas J. Sagittal balance of the spine. Rev Chir Orthop Reparatrice Appar Mot. 1997;83:22–32. [PubMed] [Google Scholar]
- 10.Min K, Hahn F, Leonardi M. Lumbar spinal osteotomy for kyphosis in ankylosing spondylitis: the significance of the whole body kyphosis angle. J Spinal Disord Tech. 2007;20:149–153. doi: 10.1097/01.bsd.0000211252.67576.d9. [DOI] [PubMed] [Google Scholar]
- 11.Murata Y, Takahashi K, Yamagata M, Hanaoka E, Moriya H. The knee–spine syndrome. Association between lumbar lordosis and extension of the knee. J Bone Joint Surg Br. 2003;85:95–99. doi: 10.1302/0301-620X.85B1.13389. [DOI] [PubMed] [Google Scholar]
- 12.Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19:1824–1836. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J. 2011;20(Suppl 5):609–618. doi: 10.1007/s00586-011-1928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 2006;31:E959–E967. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 15.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 16.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 17.Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, Yanagibashi Y. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 2005;30:1650–1657. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]