Abstract
It has been hypothesized that drugs that serve as substrates for dopamine (DA) and norepinephrine (NE) transporters may be more suitable medications for cocaine dependence than drugs that inhibit DA and NE uptake by binding to transporters. Previous studies have shown that the DA/NE releaser d-amphetamine can decrease cocaine self-administration in preclinical and clinical studies. The present study examined the effects of methylphenidate (MPD), a DA uptake inhibitor, for its ability to decrease cocaine self-administration under conditions designed to reflect clinically relevant regimens of cocaine exposure and pharmacotherapy. Each morning, rhesus monkeys pressed a lever to receive food pellets under a fixed-ratio 50 schedule of reinforcement; cocaine was self-administered under a progressive-ratio schedule of reinforcement in the evening. After cocaine (0.003–0.56 mg/kg per injection, i.v.) dose-response curves were determined, self-administration sessions were suspended and MPD (0.003–0.0056 mg/kg per hour, i.v.; or 1.0–9.0 mg/kg p.o., b.i.d.) was administered for several weeks. A cocaine self-administration session was conducted every 7 days. When a MPD dose was reached that either persistently decreased cocaine self-administration or produced disruptive effects, the cocaine dose-effect curve was re-determined. In most cases, MPD treatment either produced behaviorally disruptive effects or increased cocaine self-administration; it took several weeks for these effects to dissipate. These data are consistent with the largely negative results of clinical trials with MPD. In contrast to the positive effects with the monoamine releaser d-amphetamine under identical conditions, these results do not support use of monoamine uptake inhibitors like MPD as a medication for cocaine dependence.
Introduction
Cocaine abuse persists as a major public health problem for which no pharmacotherapy has proven to be sufficiently effective (Vocci and Ling, 2005). The success of methadone and nicotine replacement therapies in the treatment of opiate and nicotine addiction, respectively, has encouraged efforts to develop an indirect dopamine (DA) receptor agonist to treat stimulant abuse (Grabowski et al., 2004; Herin et al., 2010; Rush and Stoops, 2012). For example, d-amphetamine, a monoamine releaser, has shown positive effects in human cocaine abusers (Grabowski et al., 2004) and in rodent (Chiodo et al., 2008; Chiodo and Roberts, 2009; Thomsen et al., 2013) and monkey (Negus, 2003; Negus and Mello, 2003; Czoty et al., 2010, 2011) models. Although efforts are ongoing to develop novel DA indirect agonists for this purpose (e.g., Carroll et al., 1999; Platt et al., 2002; Lile and Nader, 2003; Rothman et al., 2005; Howell and Kimmel, 2008), one currently approved drug for use in humans is methylphenidate (MPD), a DA and norepinephrine (NE) transporter inhibitor used to treat attention-deficit hyperactivity disorder (ADHD) (Holmes, 1995). MPD has pharmacological and behavioral effects that overlap considerably with those of cocaine (e.g., Bergman et al., 1989; Volkow et al., 1999).
Despite its potential suitability as a medication for cocaine dependence, interactions between MPD and the abuse-related effects of cocaine are incompletely understood. Two laboratory studies in humans have reported decreased subjective and reinforcing effects of cocaine in individuals maintained on oral MPD (Collins et al., 2006; Winhusen et al., 2006). Results of clinical trials, however, have been mixed in terms of the ability of MPD to decrease cocaine-positive urines (Grabowski et al., 1997; Schubiner et al., 2002; Somoza et al., 2004; Levin et al., 2007). Possible confounding variables in these studies include the presence of ADHD and relatively small sample sizes. Studies in laboratory animals may provide a more thorough, unconfounded understanding of whether MPD can alter ongoing cocaine self-administration. However, most previous laboratory animal studies have examined whether adolescent MPD exposure increases vulnerability to effects of cocaine later in life (e.g., Andersen et al., 2002; Thanos et al., 2007; Gill et al., 2012). Although clinically important with respect to the long-term effects of MPD as an ADHD treatment in adolescents, such studies do not address whether MPD has effects consistent with a useful pharmacotherapy for cocaine dependence. Only one study has examined whether administration of MPD alters ongoing cocaine self-administration (Hiranita et al., 2009). In that experiment, MPD was administered acutely prior to behavioral sessions during which rats self-administered cocaine under a five-response fixed-ratio (FR 5) schedule of reinforcement. MPD dose-dependently shifted the cocaine dose-response curve leftward, indicating an increase in potency of cocaine to function as a reinforcer. Thus, one objective of this study was to expand the study of MPD in a nonhuman primate model of cocaine abuse.
The present study examined the effects of chronically administered MPD on cocaine self-administration under a progressive-ratio (PR) schedule of reinforcement in rhesus monkeys. We used an approach to testing putative pharmacotherapies that we recently described in the context of assessing d-amphetamine (Czoty et al., 2011). Briefly, this model is designed to better incorporate clinically relevant variables including the following: 1) subjects with an extensive history of cocaine self-administration, 2) concurrent, daily monitoring of food-reinforced responding and other observable behaviors that may model side effects, 3) an individual-subject design in which MPD dose was adjusted for each monkey based on observed effects (or lack thereof) on cocaine-reinforced responding, 4) assessment of MPD effects on self-administration of a range of cocaine doses, and 5) suspension of access to cocaine during MPD treatment. This latter feature was implemented to model the scenario in which an addict refrains from using cocaine during a brief period at the outset of treatment. Rather than assessing the direct interactions of MPD on daily cocaine self-administration, the effect on cocaine reinforcement was assessed only once per week, permitting 7 consecutive days of MPD treatment in the absence of cocaine.
In a previous study under the same conditions, the monoamine releaser d-amphetamine reliably produced sustained reductions in cocaine self-administration in the absence of long-lasting adverse effects (Czoty et al., 2011). An additional reason for examining MPD in the present study was the ability to compare the results of these two DA indirect agonists and to provide data relevant to the hypothesis that drugs that serve as substrates for DA and NE transporters (i.e., “releasers”) may be more suitable pharmacotherapies for cocaine dependence than drugs that block DA and NE transporters (Negus et al., 2009a,b). In addition to examining the effects of chronic MPD administered intravenously, the effects of daily oral MPD were studied. Finally, another goal of this study was to use the results to further assess the validity of the model by comparing data with this procedure to outcomes from clinical studies.
Materials and Methods
Subjects and Apparatus.
Subjects were five adult male rhesus monkeys (Macaca mulatta), each prepared with a chronic indwelling venous catheter and subcutaneous vascular access port (VAP; Access Technologies, Skokie, IL) under sterile surgical conditions as previously described (Czoty et al., 2006). Monkeys had between 6 and 15 months of experience self-administering cocaine at the outset of these studies with the exception of R-1429, who had self-administered cocaine for over 3 years. Monkeys were housed individually in sound-attenuating chambers (0.91 × 0.91 × 0.91 m; Plas Laboratories, Lansing, MI). The front wall of each cubicle was constructed of Plexiglas to allow the monkey visual access to the laboratory. Each cubicle was equipped with two response levers (BRS/LVE, Beltsville, MD). Four stimulus lights, alternating white and red, were located in a horizontal row above each lever. A receptacle located between the levers was connected via Tygon tubing (Saint-Gobain, Courbevoie, France) to a pellet dispenser located outside the chamber for response-contingent delivery of food pellets. Each animal was fitted with a stainless steel restraint harness and spring arm (Restorations Unlimited, Chicago, IL) that attached to the rear of the cubicle. A peristaltic infusion pump (Cole-Parmer Instrument Co., Vernon Hills, IL) was located on the top of the chamber for delivering injections at a rate of approximately 1.5 ml/10 s. Monkeys received fresh fruit, peanuts, and vegetables several days per week and water was available ad libitum. Animal housing and handling and all experimental procedures were performed in accordance with the 2003 National Research Council Guidelines for the Care and Use of Mammals in Neuroscience and Behavioral Research and were approved by the Animal Care and Use Committee of Wake Forest University. Environmental enrichment was provided as outlined in the Animal Care and Use Committee of Wake Forest University Non-Human Primate Environmental Enrichment Plan.
Food-Reinforced Responding.
Monkeys were trained under a reinforcement schedule in which 50 responses on the left lever resulted in delivery of one food pellet, that is, an FR 50 schedule of reinforcement. Under this schedule, white stimulus lights above the left lever were illuminated and 50 responses resulted in food pellet delivery, extinguishing of white lights and illumination of red stimulus lights for 10 seconds, followed by a 10-second timeout period during which no lights were illuminated and responding had no scheduled consequences. Sessions began at approximately 8:30 AM each day and lasted for approximately 23 hours or until the maximum number of allowed food reinforcers was earned. Thus, only food was available from 8:30 AM to 3:00 PM when the self-administration session began (see Cocaine Self-Administration). At that point, food and cocaine were concurrently available if the monkey had not yet received the maximum number of pellets. The maximum number of pellets that could be earned was determined for each monkey as that required to provide enough food to maintain body weight, measured at least monthly, at approximately 95% of free-feeding levels. When monkeys earned fewer than the maximum number of food pellets, supplementary food (LabDiet Monkey Chow #5045; PMI Nutrition International, St. Louis, MO) was given at approximately 8:00 AM in an amount calculated to raise the total grams of food to the desired level. Target food amounts for the monkeys in the present study ranged from 110 to 180 g. Weights did not change more than 4% during the course of this study.
Cocaine Self-Administration.
Monkeys self-administered (−)cocaine HCl [dissolved in sterile 0.9% saline; National Institute on Drug Abuse (NIDA), Bethesda, MD] under a PR schedule of reinforcement in sessions that began at 3:00 PM each day. Under this schedule, white stimulus lights were illuminated above the right lever and 50 responses on that lever resulted in the first injection of the maintenance dose of cocaine (0.03 mg/kg per injection in approximately 1.5 ml over 10 seconds), extinguishing of white lights and illumination of red stimulus lights for 10 seconds, followed by a 10-min timeout. The response requirement for subsequent injections was determined by the equation used by Richardson and Roberts (1996): ratio = [5 × e(R × 0.2)] – 5, where e is the mathematical constant and R is equal to the reinforcer number. For the present studies, the first response requirement (50 responses) corresponds to the 12th value given by this equation and was followed by 62, 77, 95, 117, 144, 177, 218, 267, 328, 402, 492, 602, 737, 901, 1102, and so forth. Sessions ended when 2 hours elapsed without an injection. Initially, 0.03 mg/kg cocaine was made available in evening PR sessions until responding stabilized (3 consecutive days on which the number of injections were within 2 of the 3-day mean, with no upward or downward trend). Subsequently, other doses of cocaine (0.003–0.56 mg/kg per injection) were substituted in mixed order for the maintenance dose for at least 4 days and until the number of injections earned stabilized.
Chronic MPD Treatment.
After the generation of baseline dose-effect curves, 0.03 mg/kg cocaine was made available in evening PR sessions until responding stabilized, at which point chronic MPD treatment was initiated. When intravenous (±)-MPD (NIDA) treatment was being studied (0.003–0.056 mg/kg per hour; N = 3), at approximately 8:30 AM, the external part of the catheter was connected to a syringe in an infusion pump (Cole-Parmer Instrument Co.) outside the chamber and MPD was infused at a rate of 0.5 ml/h such that monkeys received an initial dose of 0.003 or 0.01 mg/kg per hour. Food-reinforced responding was studied throughout treatment. On the seventh day, the solution being infused was changed from MPD to saline at approximately noon. This time was selected because it takes approximately 3 hours to infuse the residual MPD in the catheter (approximately 1.2 ml). Thus, MPD continued to be infused until approximately 2:55 PM, at which time the catheter was filled with the maintenance dose of cocaine. This procedure minimized the amount of MPD infused as a bolus when the catheter was filled with cocaine immediately before the start of the self-administration session. At 3:00 PM, the maintenance dose of cocaine was made available for self-administration under the PR schedule of reinforcement, signaled by illumination of the white stimulus lights above the right lever. Thus, MPD treatment continued until the start of the cocaine self-administration session. At approximately 8:30 AM on the next day, the catheter was flushed with heparin/saline solution, after which administration of the same dose of MPD was continued. When MPD was administered orally (1.0–9.0 mg/kg b.i.d.; N = 4), MPD was dissolved in sterile 0.9% saline solution at a concentration of 100 mg/ml and the required volume was mixed with mashed banana in a small paper cup and given to the monkey at approximately 8:00 AM and 2:45 PM; the monkey was observed to ensure that all of the banana was consumed. During MPD treatment, monkeys were observed for several minutes each morning and non-systematically throughout the day and any observed locomotor activation, agitation, stereotypies, or other unconditioned behavioral effects were noted.
This procedure (making the maintenance dose of cocaine available for one session) was repeated on day 14. If, at that time, the number of cocaine injections was decreased from baseline by approximately 30% or more, treatment was continued another 14 days. If an increase or no decrease in cocaine self-administration had been observed on day 14, or if tolerance to initial decreases developed by day 28, the dose of MPD was then increased and effects of the higher dose of MPD were similarly assessed. If treatment with this dose had no effect or if tolerance developed, the dose was further increased. When a dose was reached that either decreased the number of cocaine injections after approximately 28 days or produced behaviorally disruptive effects, the cocaine dose-response curve was re-determined by making a single dose available for 1 day at 3-day intervals while oral MPD treatment was continued. Next, MPD treatment was discontinued, and over the next 4 months the cocaine dose-effect curve was again determined in the absence of MPD as described above for the initial determination. That is, doses were substituted in mixed order for the maintenance cocaine dose for at least 4 days and until the number of injections earned had stabilized.
Data Analysis.
The dependent variable of primary interest was the number of cocaine injections earned under the PR schedule of reinforcement. In addition, the number of food reinforcers received was recorded in hourly bins. Because individual differences in sensitivity to MPD resulted in different regimens of MPD treatment in the five monkeys, individual data are shown.
Results
Baseline Food- and Cocaine-Reinforced Responding.
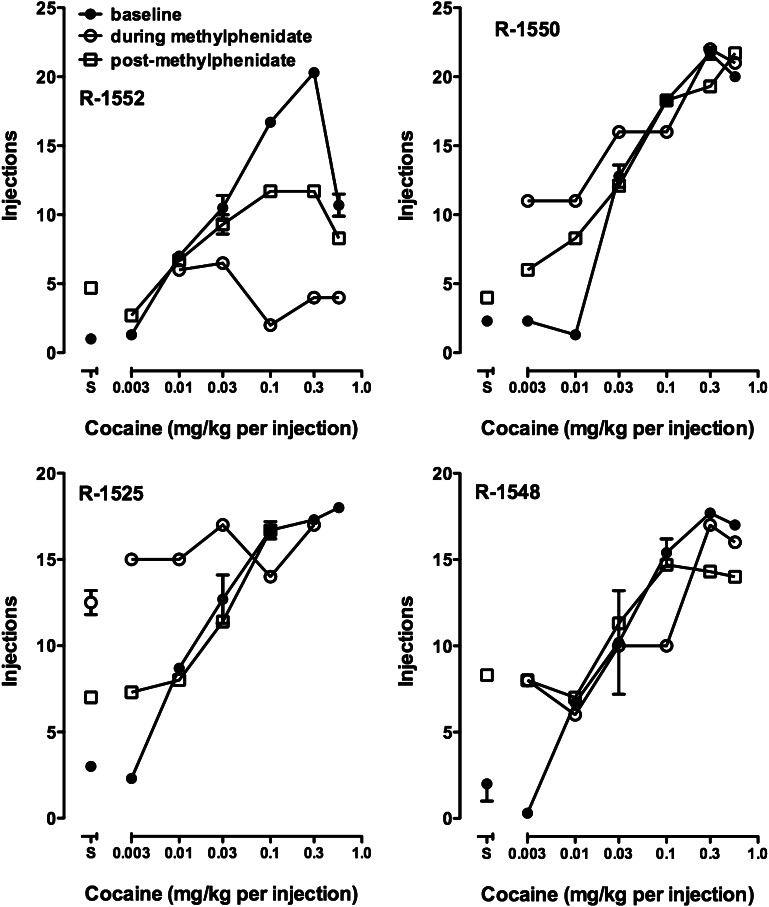
Under baseline conditions, monkeys earned all available food pellets, typically within the first 2 hours of availability with the exception of subject R-1525, who earned approximately half of his ration in the first 2 hours. In cocaine self-administration sessions, the number of injections received increased significantly as a function of the available cocaine dose, up to 0.3 mg/kg cocaine, in all monkeys (Fig. 1, closed symbols). In all cases, the cocaine self-administration session had concluded by 7:30 AM on the morning after the 3:00 PM start.
Fig. 1.
Dose-effect curves for cocaine self-administration before (filled circles), during (open circles), and after (open squares) oral MPD treatment in four monkeys. Each point on the “baseline” and “postmethylphenidate” curves is the mean of the last 3 days of availability of a cocaine dose or saline; data for the “during methylphenidate” curve are from single-session tests of that cocaine dose. When a cocaine dose or saline was made available on more than one occasion, error bars indicate the standard error of the mean. Ordinates: number of cocaine injections earned; abscissae: available cocaine dose.
Effects of Intravenous MPD Treatment on Food- and Cocaine-Reinforced Responding.
During intravenous MPD administration, unconditioned effects of MPD were noted on several days indicated with asterisks along the abscissa in Fig. 2, particularly in R-1429. Such effects included self- or experimenter-directed aggression (e.g., threats, picking or biting the leg and/or harness) as well as increased locomotion. In R-1429, treatment with 0.03 mg/kg per hour MPD produced an approximately 35% decrease in the number of injections earned after 1 week that was maintained at the end of the second week. When the MPD dose was increased to 0.056 mg/kg per hour, increased locomotion was observed. A test session did not occur at day 7 because the monkey had disconnected the needle from the VAP and it was necessary to sedate him to replace the needle. When tested on day 14, however, there was a decrease in cocaine self-administration to which tolerance developed over the first month. At approximately 5 weeks of treatment with this dose, food- and cocaine-maintained responding precipitously decreased. During this time, the monkey was often lying down in his cage, would not take treats from experimenters, and did not eat Monkey Chow placed in his cage. For these health-related reasons, MPD treatment was discontinued and the monkey was removed from the study. Food-maintained responding recovered quickly to baseline levels. Due to the experience with this monkey, doses higher than 0.056 mg/kg per hour were not tested in the other two subjects.
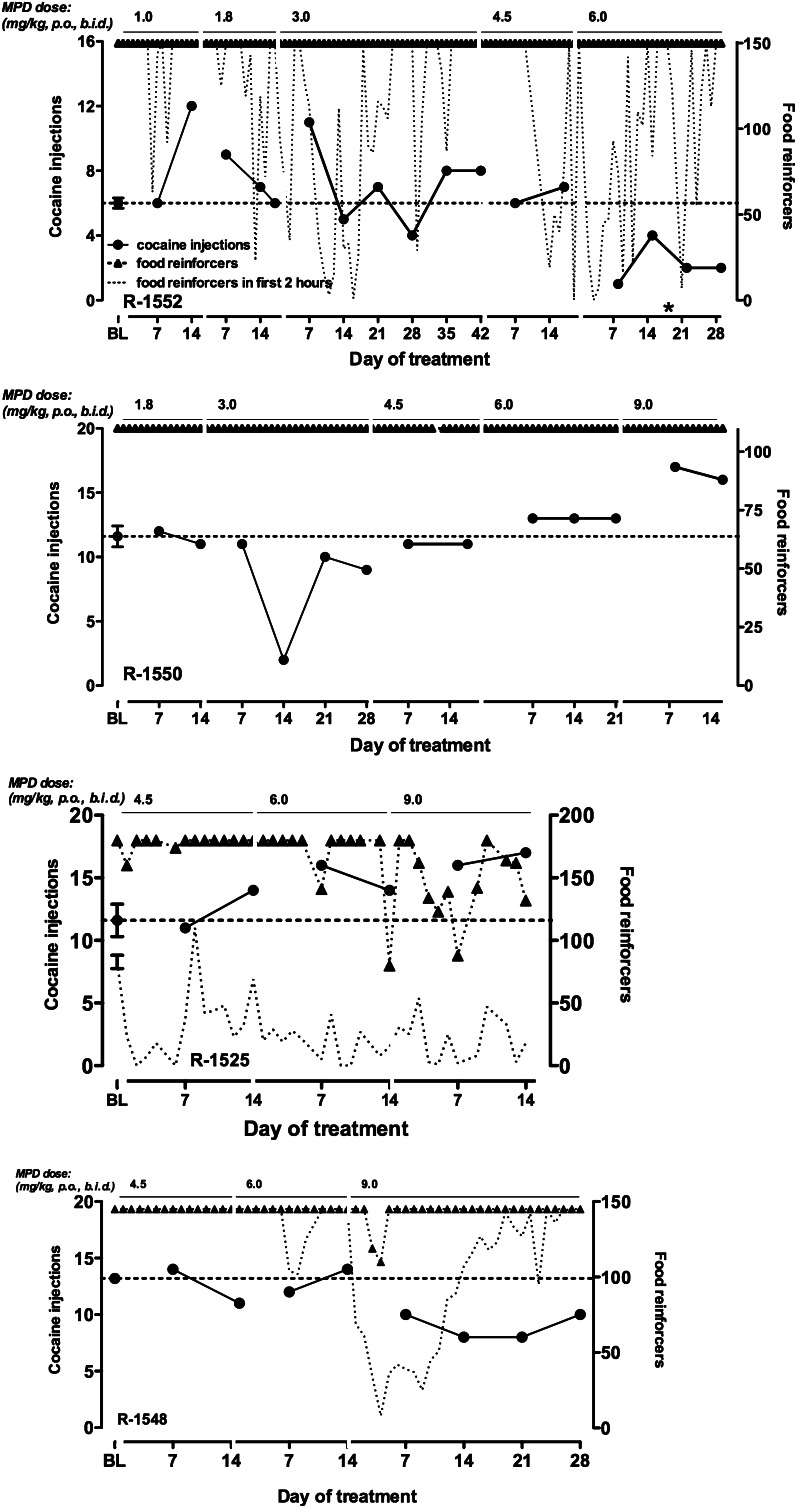
Fig. 2.
Cocaine self-administration and food-maintained responding during intravenous MPD treatment in individual monkeys. Left ordinates: number of cocaine injections received; right ordinates: number of food reinforcers earned; abscissae: day of exposure to each MPD dose, which is indicated across the top of each panel. The point above baseline (BL) represents the mean (± S.E.M.) number of injections earned on the 3 days prior to initiation of MPD treatment. The dashed line in each graph indicates the mean number of injections received under baseline conditions (i.e., prior to MPD treatment). The dotted line in each graph represents the number of pellets earned in the first 2 hours of food pellet availability.
In R-1552, cocaine self-administration was transiently increased during treatment with the lowest dose of MPD (0.01 mg/kg per hour). This effect dissipated after approximately 3 weeks. Treatment with a higher dose did not affect cocaine self-administration, but altered the pattern of food-maintained responding. Although the monkey received his total allotment of food pellets on almost every day, he tended to earn these pellets throughout a greater portion of the day, as is evidenced by the decreased number of pellets earned in the first 2 hours of the session (dotted lines in Fig. 2). Treatment with the highest MPD dose also did not alter cocaine-maintained responding. Treatment was discontinued when, as a result of increased locomotion, the catheter became twisted and disconnected from the syringe pump. In contrast to the disruptive effects and inability of intravenous MPD to persistently decrease cocaine self-administration in R-1429 and R-1552, results of i.v. MPD treatment were more selective for cocaine self-administration in comparison with food-maintained responding in R-1550 (Fig. 2). MPD treatment in this monkey produced a dose-related decrease in the number of cocaine injections earned in the absence of any disruption in food-maintained responding and only one occurrence of increased locomotion. The maximum decrease in the number of cocaine injections received was approximately 50% and appeared to be consistent over time, that is, there was no trend toward an increasing effect or tolerance during treatment. Note that data for day 7 of treatment with 0.01 mg/kg per hour MPD have been excluded from the graphs for R-1552 and R-1550. Monkeys’ responding was disrupted due to the presence of unfamiliar personnel in the laboratory on this day.
Effects of oral MPD treatment on food- and cocaine-reinforced responding.
In two monkeys (R-1552 and R-1550), oral administration of MPD began immediately after treatment with i.v. 0.056 mg/kg per hour MPD was completed. Oral MPD treatment was also tested in R-1548 and R-1525 who had not received MPD intravenously. In R-1552, similar to what was observed during i.v. treatment, lower doses of oral MPD resulted in transient increases in cocaine self-administration (Fig. 3). In general, however, no persistent effects were observed up to a dose of 4.5 mg/kg b.i.d., in any of the four monkeys (Fig. 3). In R-1552, treatment with 6.0 mg/kg MPD b.i.d, resulted in a decrease in the number of cocaine injections received under the PR schedule that persisted up to 4 weeks of treatment. There was no decrease in the total number of food reinforcers earned at this or any MPD dose in R-1552. However, similar to the effects of continuous i.v. treatment, twice-daily oral MPD treatment altered the pattern of food-maintained responding such that fewer pellets were earned in the first 2 hours of availability (dotted line in Fig. 3, top panel).
Fig. 3.
Cocaine self-administration and food-maintained responding during oral MPD treatment in individual monkeys. Otherwise, as in Fig. 2. BL, baseline.
Effects of oral MPD in R-1550 differed from those observed with intravenous MPD. Whereas continuous i.v. treatment decreased cocaine self-administration, twice-daily treatment with 9.0 mg/kg MPD increased the number of cocaine injections earned under the PR schedule. No lasting effects were observed with lower doses. As seen during i.v. treatment, there was no disruption in the number or pattern of food pellets earned. Similarly, in R-1525, only increases in self-administration were observed with higher MPD doses (6.0 and 9.0 mg/kg b.i.d.) In this monkey, MPD treatment caused disruptions in both total food reinforcers earned and in the pattern of food-maintained responding across the day. Finally, in R-1548, the highest MPD dose (9.0 mg/kg b.i.d.) produced a small but sustained decrease in cocaine-maintained responding. Disruption of the pattern of food-maintained responding by oral MPD was dependent on the MPD dose in this monkey.
Re-Determination of Dose-Effect Curves During Oral MPD Treatment.
Once a dose of MPD was found that either decreased cocaine self-administration for at least 28 days or when 9.0 mg/kg p.o., b.i.d. was reached, additional cocaine doses were made available for a single self-administration session at 3-day intervals until a complete dose-effect curve was determined. In R-1552, in whom MPD treatment decreased self-administration of 0.03 mg/kg per injection cocaine, the entire cocaine dose-effect curve was shifted downward (Fig. 1, open circles). In R-1548, intake of a low cocaine dose was increased although fewer injections of a higher dose (0.1 mg/kg) were received; other points on the dose-effect curve were not different from the baseline curve. In the two monkeys in whom the self-administration of the maintenance dose of cocaine was increased by MPD (R-1525 and R-1550), the low end of the cocaine dose-effect curve was shifted upward (Fig. 1).
Cocaine Self-Administration After Termination of MPD Treatment.
Once cocaine dose-effect curves had been re-determined during MPD administration, MPD treatment was terminated. Food-maintained responding continued to be measured daily, and monkeys were allowed access to the maintenance dose of cocaine (0.03 mg/kg per injection) under the PR schedule. Over the next several months, cocaine doses were substituted for the maintenance dose of cocaine until a dose-effect curve was again completed. In general, dose-effect curves only partially shifted back toward baseline (Fig. 1, open squares), despite that several weeks had passed since termination of MPD treatment.
Discussion
Drugs that interact with the DA transporter have received much attention as potential pharmacotherapies for cocaine abuse due to the importance of DA in mediating the abuse-related behavioral effects of cocaine. To date, however, substantial clinical evidence for the effectiveness of any such compound is lacking, with the exception of d-amphetamine (e.g., Grabowski et al., 2004), a DA and NE releaser whose potential as a medication is compromised by its high abuse liability [see Mariani and Levin (2012)]. The primary goal of the present studies was to assess the therapeutic potential of the DA uptake inhibitor MPD as a medication for cocaine abuse. A unique cocaine self-administration procedure was used that was designed to reflect many clinically relevant aspects of cocaine use and medication treatment (Czoty et al., 2011). For example, the present studies examined chronic oral treatment in cocaine-experienced monkeys using a PR schedule. Cocaine self-administration was suspended during the first week of treatment to model the frequent (although not universal) clinical situation in which a cocaine addict is able to abstain from using cocaine for a brief period of time during the initial phase of treatment due to hospitalization, incarceration, or motivation to remain abstinent when starting treatment. Each monkey’s response to treatment was monitored individually and adjustments to the treatment regimen (i.e., increasing the MPD dose) were made based on the individual’s response (i.e., a single-subject design) [see Ator and Griffiths (2003)]. Finally, food-maintained responding along with close observation of the animals’ appearance and behavior provided an index of potential side effects.
In the present study, although some reductions in cocaine self-administration were observed in some subjects, neither chronic intravenous nor chronic oral treatment with MPD exhibited an encouraging profile with respect to potential as a medication for cocaine abuse. When administered intravenously to three monkeys, MPD decreased cocaine self-administration in one monkey, but treatment had to be discontinued in two monkeys due to adverse health and behavioral effects that subsided almost immediately upon cessation of MPD administration. These effects included agitation, heightened aggression, disruption of the pattern of food-maintained responding, and, in one case, a reduction in total food pellets consumed per 24 hours. These data can be interpreted to suggest that chronic MPD treatment (at least by the i.v. route) would be expected to produce severe side effects that would limit compliance and perhaps cause adverse health effects in patients.
The transition to oral administration of MPD was associated with a much lower rate of such effects. Over several months in four subjects, only one instance of increased locomotion was observed, with no instances of agitation or aggression and no other detrimental effects to the monkeys’ health. MPD did, however, reduce the overall number of food reinforcers earned in one monkey, and disrupted the pattern of food-maintained responding in three of four subjects. These effects on food-maintained responding are not in and of themselves necessarily discouraging [see Mello and Negus (1996)]. In our previous studies with d-amphetamine using this model (Czoty et al., 2011), decreases in the total number of food reinforcers earned were commonly observed upon increasing the treatment dose of d-amphetamine. However, in every case, tolerance developed to the effects of d-amphetamine on food-maintained responding while decreases in cocaine self-administration persisted [also see Negus and Mello (2003)]. In the present experiments, however, tolerance was only evident in one of the three affected monkeys (R-1548), and the monkey whose food-maintained responding was unaffected by MPD showed an increase in cocaine self-administration. Taken together, it is evident that although oral MPD treatment was better tolerated than chronic intravenous administration, some disruption was observed that might suggest lasting side effects. Of greater concern is the observation that chronic MPD administration increased cocaine self-administration in two monkeys, in accordance with data in rats (Hiranita et al., 2009), and that decreases in self-administration of the maintenance dose of cocaine in the other two subjects were, at most, partial.
Once the MPD treatment dose either decreased self-administration of 0.03 mg/kg cocaine (6.0 mg/kg b.i.d. in R-1552) or reached the highest dose we tested (9.0 mg/kg b.i.d.), treatment with that MPD dose was continued and other doses of cocaine were tested at 3-day intervals. In this manner, a cocaine dose-effect curve was re-determined to better characterize the effects of MPD on the reinforcing effects of cocaine. In the subject in whom self-administration was decreased by oral MPD (R-1552), the entire dose-effect curve was shifted downward. The other three subjects self-administered more injections of lower cocaine doses compared with baseline; the higher end of the curve was, for the most part, similar to baseline levels of self-administration. Strikingly, when the dose-effect curve was again re-determined during the 4 months after MPD treatment had been discontinued, dose-effect curves had still not fully recovered to baseline. Regardless of the direction of effects of MPD on cocaine self-administration, they persisted for several weeks after MPD administration had concluded.
Perhaps the most surprising aspect of these studies was that the doses that affected cocaine self-administration (6.0–9.0 mg/kg b.i.d.) were substantially higher than those considered safe in humans. For example, the highest dose tested in human studies was 60 mg/d (Collins et al., 2006; Levin et al., 2007), which is less than 1 mg/kg in an average-sized human. Doses necessary to observe effects in the present study reached 12-18 mg/kg per day, much higher than in the aforementioned studies and higher than doses used to treat adult ADHD (e.g., 0.4–1.4 mg/kg per day in a 70-kg human) (Bouffard et al., 2003; Biederman et al., 2010). One reason for this difference may be that, unlike the present studies, clinical studies have used sustained-release formulations. We attempted to mimic this method of MPD delivery as much as possible by using continuous intravenous infusion but found that this approach was associated with a relatively high rate of adverse effects in two monkeys. Another implication is that the (lower) doses in the present study, which best approximate those used clinically, have no effect on self-administration. The necessity to use higher doses in the present study in monkeys may also explain why rates of adverse effects seen in these monkeys were relatively high compared with the few adverse effects observed in most studies in humans (e.g., Grabowski et al., 1997).
The differences in effects of d-amphetamine and MPD observed using this procedure add to a growing set of data suggesting that drugs that serve as substrates for DA and NE transporters (i.e., monoamine releasers) may be more suitable medications for cocaine dependence than drugs that inhibit DA and NE uptake by binding to transporters. Although the DA-selective uptake inhibitor GBR 12909 and cocaine itself have been shown to selectively decrease cocaine- versus food-maintained responding (Glowa et al., 1995a,b; Glowa and Fantegrossi, 1997), this effect is less evident under lean conditions of reinforcement (i.e., lower cocaine doses and higher response requirements) (Stafford et al., 2001). Chronic treatment with other monoamine transporter inhibitors including mazindol, RTI-112, RTI-113, and indatraline resulted in reductions in both food- and cocaine-maintained responding (Kleven and Woolverton, 1993; Negus et al., 1999, 2009a). On the other hand, amphetamine-like DA/NE releasers have shown more consistent selectivity in their behavioral effects (e.g., Negus et al., 2007, 2009b). Although the mechanisms underlying the behavioral differences between releasers and uptake inhibitors remain to be elucidated, pharmacotherapeutic approaches that reduce the abuse liability of amphetamine-like compounds, such as prodrugs (e.g., phendimetrazine; Rothman et al., 2002; Banks et al., 2012), appear to be a more promising avenue for development of “agonist” medications for cocaine dependence than DA/NE transporter inhibitors.
In summary, neither intravenous nor oral MPD treatment reliably decreased cocaine self-administration in the absence of behaviorally disruptive effects, using a paradigm designed to incorporate clinically relevant aspects of cocaine use and pharmacotherapeutic treatment. Clearly these adjustments do not completely recapitulate the clinical condition in that cocaine availability was limited and abstinence was forced (rather than voluntary) and occurred throughout the testing period. Moreover there are many other aspects that have not been, and possibly cannot be, incorporated into animal models (e.g., uniquely human negative consequences of drug use and progressive psychiatric consequences). Nonetheless, it is hoped that enhancing the face value of the procedure as a model of drug abuse and pharmacotherapy will also increase its predictive validity. The results of the present studies are concordant with clinical findings and suggest that MPD would not be a safe and effective treatment of cocaine dependence.
Acknowledgments
The authors thank Tonya Calhoun for excellent technical assistance.
Abbreviations
- ADHD
attention-deficit hyperactivity disorder
- DA
dopamine
- FR
fixed ratio
- GBR 12909
1-(2-[bis(4-fluorophenyl)methoxy]ethyl)-4-(3-phenylpropyl)piperazine dihydrochloride
- MPD
methylphenidate
- NE
norepinephrine
- PR
progressive ratio
- RTI-112
3β-(3-methyl-4-chlorophenyl)tropane-2β-carboxylic acid methyl ester hydrochloride
- RTI-113
3β-(4-chlorophenyl)tropane-2β-carboxylic acid phenyl ester hydrochloride
- VAP
vascular access port
Authorship Contributions
Participated in research design: Czoty, Nader.
Conducted experiments: Martelle, Gould.
Performed data analysis: Czoty.
Wrote or contributed to the writing of the manuscript: Czoty, Martelle, Gould, Nader.
Footnotes
This research was supported by the National Institutes of Health National Institute on Drug Abuse [Grant DA-06634].
References
- Andersen SL, Arvanitogiannis A, Pliakas AM, LeBlanc C, Carlezon WA., Jr (2002) Altered responsiveness to cocaine in rats exposed to methylphenidate during development. Nat Neurosci 5:13–14 [DOI] [PubMed] [Google Scholar]
- Ator NA, Griffiths RR. (2003) Principles of drug abuse liability assessment in laboratory animals. Drug Alcohol Depend 70 (Suppl)S55–S72 [DOI] [PubMed] [Google Scholar]
- Banks ML, Blough BE, Fennell TR, Snyder RW, Negus SS. (2012) Role of phenmetrazine as an active metabolite of phendimetrazine: Evidence from studies of drug discrimination and pharmacokinetics in rhesus monkeys. Drug Alcohol Depend DOI: [published ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman J, Madras BK, Johnson SE, Spealman RD. (1989) Effects of cocaine and related drugs in nonhuman primates. III. Self-administration by squirrel monkeys. J Pharmacol Exp Ther 251:150–155 [PubMed] [Google Scholar]
- Biederman J, Mick E, Surman C, Doyle R, Hammerness P, Kotarski M, Spencer T. (2010) A randomized, 3-phase, 34-week, double-blind, long-term efficacy study of osmotic-release oral system-methylphenidate in adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 30:549–553 [DOI] [PubMed] [Google Scholar]
- Bouffard R, Hechtman L, Minde K, Iaboni-Kassab F. (2003) The efficacy of 2 different dosages of methylphenidate in treating adults with attention-deficit hyperactivity disorder. Can J Psychiatry 48:546–554 [DOI] [PubMed] [Google Scholar]
- Carroll FI, Howell LL, Kuhar MJ. (1999) Pharmacotherapies for treatment of cocaine abuse: preclinical aspects. J Med Chem 42:2721–2736 [DOI] [PubMed] [Google Scholar]
- Chiodo KA, Läck CM, Roberts DC. (2008) Cocaine self-administration reinforced on a progressive ratio schedule decreases with continuous D-amphetamine treatment in rats. Psychopharmacology (Berl) 200:465–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiodo KA, Roberts DC. (2009) Decreased reinforcing effects of cocaine following 2 weeks of continuous D-amphetamine treatment in rats. Psychopharmacology (Berl) 206:447–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SL, Levin FR, Foltin RW, Kleber HD, Evans SM. (2006) Response to cocaine, alone and in combination with methylphenidate, in cocaine abusers with ADHD. Drug Alcohol Depend 82:158–167 [DOI] [PubMed] [Google Scholar]
- Czoty PW, Gould RW, Martelle JL, Nader MA. (2011) Prolonged attenuation of the reinforcing strength of cocaine by chronic d-amphetamine in rhesus monkeys. Neuropsychopharmacology 36:539–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czoty PW, Martelle JL, Nader MA. (2006) Influence of abstinence and conditions of cocaine access on the reinforcing strength of cocaine in nonhuman primates. Drug Alcohol Depend 85:213–220 [DOI] [PubMed] [Google Scholar]
- Czoty PW, Martelle JL, Nader MA. (2010) Effects of chronic d-amphetamine administration on the reinforcing strength of cocaine in rhesus monkeys. Psychopharmacology (Berl) 209:375–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill KE, Pierre PJ, Daunais J, Bennett AJ, Martelle S, Gage HD, Swanson JM, Nader MA, Porrino LJ. (2012) Chronic treatment with extended release methylphenidate does not alter dopamine systems or increase vulnerability for cocaine self-administration: a study in nonhuman primates. Neuropsychopharmacology 37:2555–2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowa JR, Fantegrossi WE. (1997) Effects of dopaminergic drugs on food- and cocaine-maintained responding. IV: Continuous cocaine infusions. Drug Alcohol Depend 45:71–79 [DOI] [PubMed] [Google Scholar]
- Glowa JR, Wojnicki F, Matecka D, Bacher J, Mansbach R, Balster R, and Rice K (1995a) Effects of dopamine reuptake inhibitors on food- and cocaine-maintained responding: I. Dependence on unit dose of cocaine. Exp Clin Psychopharmacol 3:219–231 [Google Scholar]
- Glowa JR, Wojnicki FHE, Matecka D, Rice KC. (1995b) Effects of dopamine reuptake inhibitors on food- and cocaine-maintained responding: II. Comparisons with other drugs and repeated administrations. Exp Clin Psychopharmacol 3:232–239 [Google Scholar]
- Grabowski J, Roache JD, Schmitz JM, Rhoades H, Creson D, Korszun A. (1997) Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 17:485–488 [DOI] [PubMed] [Google Scholar]
- Grabowski J, Shearer J, Merrill J, Negus SS. (2004) Agonist-like, replacement pharmacotherapy for stimulant abuse and dependence. Addict Behav 29:1439–1464 [DOI] [PubMed] [Google Scholar]
- Herin DV, Rush CR, Grabowski J. (2010) Agonist-like pharmacotherapy for stimulant dependence: preclinical, human laboratory, and clinical studies. Ann N Y Acad Sci 1187:76–100 [DOI] [PubMed] [Google Scholar]
- Hiranita T, Soto PL, Newman AH, Katz JL. (2009) Assessment of reinforcing effects of benztropine analogs and their effects on cocaine self-administration in rats: comparisons with monoamine uptake inhibitors. J Pharmacol Exp Ther 329:677–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes VF. (1995) Medical use of psychostimulants: an overview. Int J Psychiatry Med 25:1–19 [DOI] [PubMed] [Google Scholar]
- Howell LL, Kimmel HL. (2008) Monoamine transporters and psychostimulant addiction. Biochem Pharmacol 75:196–217 [DOI] [PubMed] [Google Scholar]
- Kleven MS, Woolverton WL. (1993) Effects of three monoamine uptake inhibitors on behavior maintained by cocaine or food presentation in rhesus monkeys. Drug Alcohol Depend 31:149–158 [DOI] [PubMed] [Google Scholar]
- Levin FR, Evans SM, Brooks DJ, Garawi F. (2007) Treatment of cocaine dependent treatment seekers with adult ADHD: double-blind comparison of methylphenidate and placebo. Drug Alcohol Depend 87:20–29 [DOI] [PubMed] [Google Scholar]
- Lile JA, Nader MA. (2003) The abuse liability and therapeutic potential of drugs evaluated for cocaine addiction as predicted by animal models. Curr Neuropharmacol 1:21–46 [Google Scholar]
- Mariani JJ, Levin FR. (2012) Psychostimulant treatment of cocaine dependence. Psychiatr Clin North Am 35:425–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mello NK, Negus SS. (1996) Preclinical evaluation of pharmacotherapies for treatment of cocaine and opioid abuse using drug self-administration procedures. Neuropsychopharmacology 14:375–424 [DOI] [PubMed] [Google Scholar]
- Negus SS. (2003) Rapid assessment of choice between cocaine and food in rhesus monkeys: effects of environmental manipulations and treatment with d-amphetamine and flupenthixol. Neuropsychopharmacology 28:919–931 [DOI] [PubMed] [Google Scholar]
- Negus SS, Baumann MH, Rothman RB, Mello NK, Blough BE. (2009a) Selective suppression of cocaine- versus food-maintained responding by monoamine releasers in rhesus monkeys: benzylpiperazine, (+)phenmetrazine, and 4-benzylpiperidine. J Pharmacol Exp Ther 329:272–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negus SS, Brandt MR, Mello NK. (1999) Effects of the long-acting monoamine reuptake inhibitor indatraline on cocaine self-administration in rhesus monkeys. J Pharmacol Exp Ther 291:60–69 [PubMed] [Google Scholar]
- Negus SS, Mello NK. (2003) Effects of chronic d-amphetamine treatment on cocaine- and food-maintained responding under a second-order schedule in rhesus monkeys. Drug Alcohol Depend 70:39–52 [DOI] [PubMed] [Google Scholar]
- Negus SS, Mello NK, Blough BE, Baumann MH, Rothman RB. (2007) Monoamine releasers with varying selectivity for dopamine/norepinephrine versus serotonin release as candidate “agonist” medications for cocaine dependence: studies in assays of cocaine discrimination and cocaine self-administration in rhesus monkeys. J Pharmacol Exp Ther 320:627–636 [DOI] [PubMed] [Google Scholar]
- Negus SS, Mello NK, Kimmel HL, Howell LL, Carroll FI. (2009b) Effects of the monoamine uptake inhibitors RTI-112 and RTI-113 on cocaine- and food-maintained responding in rhesus monkeys. Pharmacol Biochem Behav 91:333–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt DM, Rowlett JK, Spealman RD. (2002) Behavioral effects of cocaine and dopaminergic strategies for preclinical medication development. Psychopharmacology (Berl) 163:265–282 [DOI] [PubMed] [Google Scholar]
- Richardson NR, Roberts DCS. (1996) Progressive ratio schedules in drug self-administration studies in rats: a method to evaluate reinforcing efficacy. J Neurosci Methods 66:1–11 [DOI] [PubMed] [Google Scholar]
- Rothman RB, Blough BE, Woolverton WL, Anderson KG, Negus SS, Mello NK, Roth BL, Baumann MH. (2005) Development of a rationally designed, low abuse potential, biogenic amine releaser that suppresses cocaine self-administration. J Pharmacol Exp Ther 313:1361–1369 [DOI] [PubMed] [Google Scholar]
- Rothman RB, Katsnelson M, Vu N, Partilla JS, Dersch CM, Blough BE, Baumann MH. (2002) Interaction of the anorectic medication, phendimetrazine, and its metabolites with monoamine transporters in rat brain. Eur J Pharmacol 447:51–57 [DOI] [PubMed] [Google Scholar]
- Rush CR, Stoops WW. (2012) Agonist replacement therapy for cocaine dependence: a translational review. Future Med Chem 4:245–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubiner H, Saules KK, Arfken CL, Johanson CE, Schuster CR, Lockhart N, Edwards A, Donlin J, Pihlgren E. (2002) Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol 10:286–294 [DOI] [PubMed] [Google Scholar]
- Somoza EC, Winhusen TM, Bridge TP, Rotrosen JP, Vanderburg DG, Harrer JM, Mezinskis JP, Montgomery MA, Ciraulo DA, Wulsin LR, et al. (2004) An open-label pilot study of methylphenidate in the treatment of cocaine dependent patients with adult attention deficit/hyperactivity disorder. J Addict Dis 23:77–92 [DOI] [PubMed] [Google Scholar]
- Stafford D, LeSage MG, Rice KC, Glowa JR. (2001) A comparison of cocaine, GBR 12909, and phentermine self-administration by rhesus monkeys on a progressive-ratio schedule. Drug Alcohol Depend 62:41–47 [DOI] [PubMed] [Google Scholar]
- Thanos PK, Michaelides M, Benveniste H, Wang GJ, Volkow ND. (2007) Effects of chronic oral methylphenidate on cocaine self-administration and striatal dopamine D2 receptors in rodents. Pharmacol Biochem Behav 87:426–433 [DOI] [PubMed] [Google Scholar]
- Thomsen M, Barrett AC, Negus SS, Caine SB. (2013) Cocaine versus food choice procedure in rats: environmental manipulations and effects of amphetamine. J Exp Anal Behav 99:211–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vocci F, Ling W. (2005) Medications development: successes and challenges. Pharmacol Ther 108:94–108 [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Fischman M, Foltin R, Abumrad NN, Gatley SJ, Logan J, Wong C, Gifford A, et al. (1999) Methylphenidate and cocaine have a similar in vivo potency to block dopamine transporters in the human brain. Life Sci 65:PL7–PL12 [DOI] [PubMed] [Google Scholar]
- Winhusen TM, Somoza E, Singal BM, Harrer J, Apparaju S, Mezinskis J, Desai P, Elkashef A, Chiang CN, Horn P. (2006) Methylphenidate and cocaine: a placebo-controlled drug interaction study. Pharmacol Biochem Behav 85:29–38 [DOI] [PubMed] [Google Scholar]