Abstract
Context:
Rosacea significantly affects the quality of life and its pathophysiology is not well understood. It has been suggested that the presence of Demodex folliculorum in the affected skin could be related to the development of rosacea.
Aims:
To study the risk for association between the presence of D. folliculorum in skin biopsies and the diagnosis of rosacea.
Settings and Design:
Analytical, observational, retrospective, case–control study.
Materials and Methods:
Skin biopsies of patients diagnosed clinically as rosacea and the same number of controls were studied. The controls were selected among the facial skin biopsies that were not diagnosed as rosacea. All the slides were analyzed for the presence of D. folliculorum and the density of the infestation was assessed.
Statistical Analysis Used:
Absolute/relative frequencies, mean, standard deviation, odds ratio (OR), Chi square and Independent Student t-test with Epi Info v. 3.4.3®.
Results:
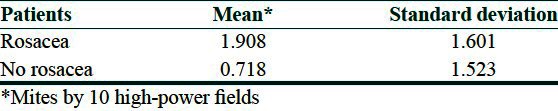
D. folliculorum was present in 80% of the skin biopsies of rosacea patients and in 30% of the controls. The risk of suffering rosacea was increased among persons infested with the mite (OR = 9.33 [95% confidence interval: 2.85-30.60]; P = 0.0001). The mean infestation density among the cases was 1.908 for every 10 high-power fields while it was 0.718 among the controls (P < 0.005). There were no statistically significant differences among the groups with regard to sex and age.
Conclusions:
The presence of D. folliculorum in skin biopsies is associated with the diagnosis of rosacea. The infestation density was increased among the patients with rosacea.
Keywords: Biopsy, Demodex folliculorum, rosacea
Introduction
What is new?
Rosacea is a chronic inflammatory skin disease with a not completely understood pathophysiology.
The pathophysiology of rosacea is not completely understood, and this complicates the treatment of the disease. Several pathogenic mechanisms have been proposed, such as vascular alterations, influence of the weather, dermal matrix degeneration, chemicals and ingested agents, anomalies of the pilosebaceous unit, immunological alterations, reactive oxygen species and bacterial and parasitic agents.[1–6] Among these, the relationship with the presence of the mite Demodex folliculorum is one of the most intriguing. Because of that, the aim of this study was to determine whether the presence of D. folliculorum in skin biopsies is associated with the diagnosis of rosacea. This study is very important because it provides information from a mestizo population that could support the idea of including an acaricide therapy for the treatment of rosacea and may improve the quality of life of these patients.
Materials and Methods
The cases were all the skin biopsies diagnosed clinically as rosacea and received by the Dermatopathology Service of Mexico's General Hospital O.D. between 1975 and 2010. Since in our service we do not have biopsies of healthy skin, the controls were facial skin biopsies that were not diagnosed as rosacea in the same time frame. All the cases were studied and the same amount of controls were randomly selected. For randomization, all the biopsy numbers of the patients that fulfilled the selection criteria for controls were placed inside a bag and they were selected by a lottery. We excluded from the case group all the biopsies that had a clinical diagnosis of rosacea but a contradictory histology or a different histological diagnosis and all the biopsies where the paraffin-embedded tissue could not be found in the archives. We excluded from the control group all skin biopsies that did not have definitive histopathologic diagnosis, that were not from facial skin, that had a diagnosis that could be confounded clinically with rosacea (such as demodicosis, acne, acne–rosacea, rosacea-like syndrome, steroid-induced rosacea, acneiform folliculitis or pseudofolliculitis of the beard), and that did not have paraffin-embedded tissue in the archives. Biopsies in which the paraffin block did not contain tissue or was destroyed in the process of obtaining new slides were excluded from the study [Figure 1].
Figure 1.
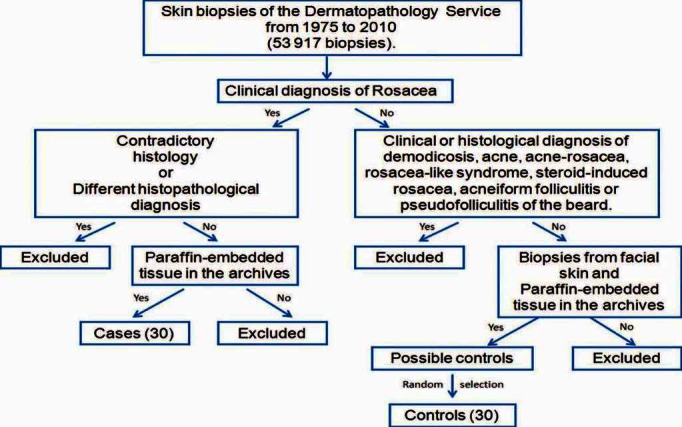
Flow diagram for selection criteria
Among the studied variables, we can mention sex, age and histopathologic diagnosis (rosacea or different from rosacea). We also studied the presence and the density of the infestation by D. folliculorum. The presence of D. folliculorum was defined as the appearance of at least one mite in the hematoxylin and eosin-stained slides. The density of D. folliculorum was defined as the average number of mites found in 10 high-power fields.
From the selected paraffin blocks, we obtained five hematoxylin and eosin-stained slides at the dermatopathology laboratory. The technicians randomly gave new numbers to each case and only they knew by that time which slides were from the case or the control group. Every slide was analyzed simultaneously by both researchers (one certified dermatopathologist and one dermatopathology resident) at high-power (×400) with a conventional dual head light microscope (Carl Zeiss, Jena, Germany) in order to determine the presence and the density of the mite. All decisions were made by consensus. The statistical analysis was performed with the informatic program Epi Info v. 3.4.3 ©, and we determined the absolute and relative (percentage) frequencies for each variable. The mean and standard deviation were calculated for age. The odds ratio (OR) for the diagnosis of rosacea when Demodex was present in the histopathology was calculated. The statistical significance was determined by the Chi square test (presence of D. folliculorum) and the Independent Student t-test (density of D. folliculorum).
Because the study only involved paraffin blocks and slides that were prepared from skin biopsies that were obtained in the past, we did not perform diagnostic or therapeutic interventions on any patient that could compromise their integrity or could harm them physically or morally. We respected the principles of the Helsinki Declaration of 1975 with the modifications of 1993 and The Mexican General Health Law.
Results
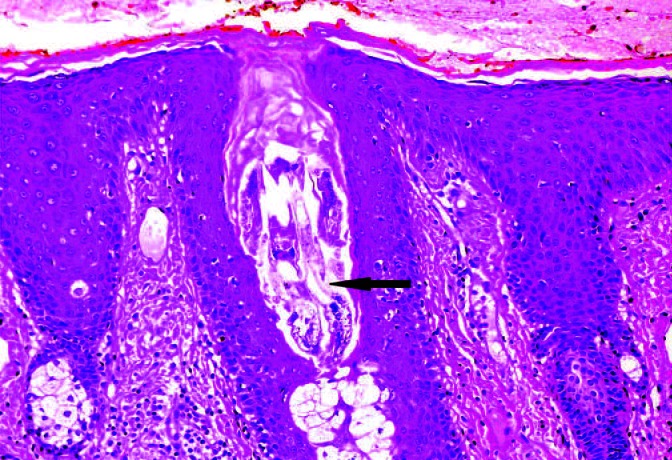
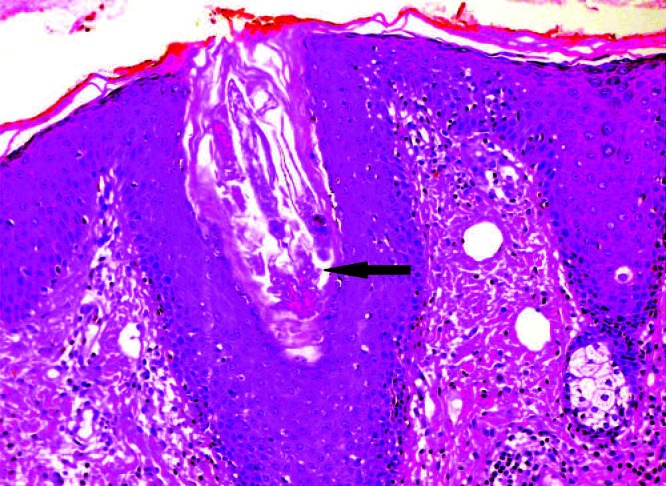
We studied 30 biopsies from patients with rosacea and 30 controls. Sixty percent of the studied biopsies were from female patients in both groups. The mean age of the patients of the rosacea group was 43.27 ± 14.85 years, while in the control group it was 46 ± 16.4 years (P = 0.5014). The diagnoses of the controls were diverse [Table 1]. D. folliculorum was found in 80% of the rosacea biopsies and only in 30% of the control biopsies [Table 2]. D. folliculorum was found inside the hair follicles in all the positive biopsies [Figures 2 and 3]. The OR was 9.33 (95% confidence interval [CI]: 2.85–30.60; P = 0.0001). The mean infestation density by D. folliculorum was higher in the group of patients with rosacea than in the control group [Table 3]. The difference between these means was statistically significant (P = 0.0046).
Table 1.
Diagnoses of the biopsies of the control group
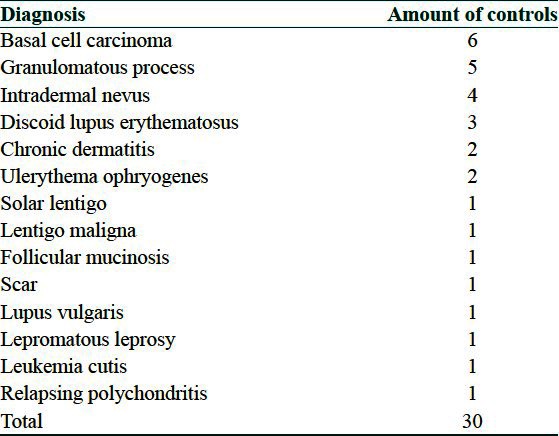
Table 2.
Distribution of Demodex folliculorum in skin biopsies of patients with or without rosacea
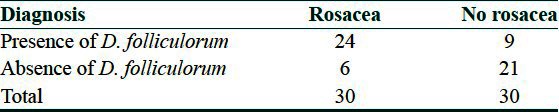
Figure 2.
Demodex mites inside a hair follicle (black arrow)
Figure 3.
Demodex mite: The legs are visible (black arrow)
Table 3.
Density of Demodex folliculorum in skin biopsies of patients with or without rosacea
Discussion
Rosacea is a chronic inflammatory skin disease that is characterized by transient or persistent centrofacial erythema, telangiectasias and, commonly, by papules and pustules.[1] In our study, rosacea affected women more often than men. The male to female ratio was 2:3. This is very similar to the results of a Swedish study that found a male to female ratio of 1:3.[7-8] The disease affects mainly young and middle-aged adults, but it can also affect children.[2,8] Because the face is usually affected, the quality of life of the patients is usually affected.[1,9]
The etiology of rosacea remains obscure. Demodex spp. seem to play an important role in the patophysiology of rosacea. Two different Demodex species have been found in humans: D. folliculorum and D. brevis.[10–14] Demodex spp. could participate in the pathogeny of rosacea by several mechanisms such as causing direct damage to the follicular epithelia, by increased mite density, by obstruction of the hair follicle or the sebaceous duct, by generating foreign body reactions, by inducing host hypersensitivity reactions and by acting as vectors for bacteria (Staphylococcus albus and Bacillus oleronius).[1,5,10,13,15–24]
In our study, D. folliculorum was found in 80% of rosacea biopsies and in only 30% of control biopsies. The fact that the percentage of mite infestation was higher in the rosacea group had also been reported by other studies. In a case–control study of papulo-pustular rosacea patients, D. folliculorum was found in 90.2% of the cases and only in 11.9% of the controls.[18] In another case–control study, Demodex spp. was found in 38.6% of rosacea biopsies, while it was found only in 21.3% of discoid lupus biopsies and in 10.6% of actinic lichen planus biopsies.[8]
The OR for finding D. folliculorum in the biopsies of rosacea patients (cases) was 9.33 (95% CI: 2.85-30.60; P = 0.0001) when compared with biopsies of patients that did not suffer from the disease (controls). This OR is very similar to the one calculated in a meta-analysis of 28,527 patients from 48 studies published in English and Chinese from 10 countries. In this meta-analysis, a significant relationship between Demodex infestation and the development of rosacea was found (OR = 7.57).[17] In a previously mentioned case–control study, the risk for the detection of Demodex spp. in a rosacea biopsy was higher than in discoid lupus biopsies (OR = 2.3) and in actinic lichen planus biopsies (OR = 5.2).[8]
Several studies have shown that there is an increased density of Demodex mites in the skin of rosacea patients.[5,8,13,16–19] It has been proposed that a density above 5 mites/cm2 increases the pathogenic potential of Demodex spp.[13,20] The mean density of infestation in our study was 1.908 mites per 10 high-power fields among patients with rosacea and 0.718 mites per 10 high-power fields among controls. These results are in accordance with other studies that have shown a higher density of mite infestation among rosacea patients. In a case–control study of papulo-pustular rosacea patients, the main D. folliculorum density was 2.03 mites per visual field in the case group and 0.16 mites in the control group.[18] In another case–control study, the mean mite count determined by superficial skin biopsy was 49.8 in the rosacea group and 10.8 in the control group.[19] The fact that, in our study, we found a lower infestation density could be explained, at least in part, by the technique used for mite detection. In our study, we worked with the mites present in paraffin-embedded tissue, while the other studies used the material expressed from hair follicles[18] or superficial skin biopsy.[19] It has been demonstrated that superficial skin biopsy is a technique with a higher mite recovery rate than conventional biopsy, but it cannot be used to study biopsies that have already been paraffin-embedded.
Taking all together, we can conclude that at least among the studied population, the presence of D. folliculorum in the skin and the higher infestation densities could favor the development of rosacea. This information is particularly useful for countries with mestizo populations, like countries from Latin America, because most of the previously available information was obtained on white populations.
Acknowledgments
The authors are grateful to technicians Israel Marcelino Domínguez and Alejandro Keintel Márquez and to Miss Jazmin Díaz Montes for their collaboration in this research project.
What is new?
In our mestizo population, the presence of D. folliculorum in the skin and the higher infestation seem to be related with rosacea.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327–41. doi: 10.1016/j.jaad.2004.03.030. [DOI] [PubMed] [Google Scholar]
- 2.Rodríguez Acar M, Martínez Muñoz JA. Rosácea infantil. Rev Cent Dermatol Pascua. 2011;20:18–21. [Google Scholar]
- 3.Alonzo ML, Guarneros A, Valdés Webster RL. Rosácea ocular: Presentación de un caso. Rev Cent Dermatol Pascua. 2006;15:173–6. [Google Scholar]
- 4.Khaled A, Hammami H, Zeglaoui F, Tounsi J, Zermani R, Kamoun MR, et al. Rosacea: 244 Tunisian cases. Tunis Med. 2010;88:597–601. [PubMed] [Google Scholar]
- 5.Yamasaki K, Gallo RL. The molecular pathology of rosacea. J Dermatol Sci. 2009;55:77–81. doi: 10.1016/j.jdermsci.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bae YI, Yun SJ, Lee JB, Kim SJ, Won YH, Lee SC. Clinical evaluation of 168 korean patients with rosacea: The sun exposure correlates with the erythematotelangiectatic subtype. Ann Dermatol. 2009;21:243–9. doi: 10.5021/ad.2009.21.3.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Culp B, Scheinfeld N. Rosacea: A review. P T. 2009;34:38–45. [PMC free article] [PubMed] [Google Scholar]
- 8.Moravvej H, Dehghan-Mangabadi M, Abbasian MR, Meshkat-Razavi G. Association of rosacea with demodicosis. Arch Iran Med. 2007;10:199–203. [PubMed] [Google Scholar]
- 9.Baldwin HE. Systemic therapy for rosacea. Skin Therapy Lett. 2007;12:1–5. [PubMed] [Google Scholar]
- 10.Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10:505–10. doi: 10.1097/ACI.0b013e32833df9f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zomorodian K, Geramishoar M, Saadat F, Tarazoie B, Norouzi M, Rezaie S. Facial demodicosis. Eur J Dermatol. 2004;14:121–2. [PubMed] [Google Scholar]
- 12.Rodríguez H. Prevalencia de Demodex sp. en pacientes con blefaritis. Anales de la Facultad de Medicina. 2000;61:299–304. [Google Scholar]
- 13.Lacey N, Kavanagh K, Tseng SC. Under the lash: Demodex mites in human diseases. Biochem (Lond) 2009;31:2–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Jansen T, Kastner U, Kreuter A, Altmeyer P. Rosacea-like demodicidosis associated with acquired immunodeficiency syndrome. Br J Dermatol. 2001;144:139–42. doi: 10.1046/j.1365-2133.2001.03794.x. [DOI] [PubMed] [Google Scholar]
- 15.Hsu CK, Hsu MM, Lee JY. Demodicosis: A clinicopathological study. J Am Acad Dermatol. 2009;60:453–62. doi: 10.1016/j.jaad.2008.10.058. [DOI] [PubMed] [Google Scholar]
- 16.Lee JY, Hsu CK. Granulomatous rosacea-like demodicidosis. Dermatol Online J. 2007;13:9. [PubMed] [Google Scholar]
- 17.Zhao YE, Wu LP, Peng Y, Cheng H. Retrospective analysis of the association between Demodex infestation and rosacea. Arch Dermatol. 2010;146:896–902. doi: 10.1001/archdermatol.2010.196. [DOI] [PubMed] [Google Scholar]
- 18.Georgala S, Katoulis AC, Kylafis GD, Koumantaki-Mathioudaki E, Georgala C, Aroni K. Increased density of Demodex folliculorum and evidence of delayed hypersensitivity reaction in subjects with papulopustular rosacea. J Eur Acad Dermatol Venereol. 2001;15:441–4. doi: 10.1046/j.1468-3083.2001.00331.x. [DOI] [PubMed] [Google Scholar]
- 19.Bonnar E, Eustace P, Powell FC. The Demodex mite population in rosacea. J Am Acad Dermatol. 1993;28:443–8. doi: 10.1016/0190-9622(93)70065-2. [DOI] [PubMed] [Google Scholar]
- 20.Bikowski JB, Del Rosso JQ. Demodex dermatitis: A retrospective analysis of clinical diagnosis and successful treatment with topical crotamiton. J Clin Aesthet Dermatol. 2009;2:20–5. [PMC free article] [PubMed] [Google Scholar]
- 21.Pena GP, Andrade Filho JS. Is demodex really non-pathogenic? Rev Inst Med Trop Sao Paulo. 2000;42:171–3. doi: 10.1590/s0036-46652000000300012. [DOI] [PubMed] [Google Scholar]
- 22.Monsef A, Eghbalian F. Histopathologic study of rosacea and the role of Demodex folliculorum. Iranian Journal of Pathology. 2006;1:169–72. [Google Scholar]
- 23.Lacey N, Delaney S, Kavanagh K, Powell FC. Mite-related bacterial antigens stimulate inflammatory cells in rosacea. Br J Dermatol. 2007;157:474–81. doi: 10.1111/j.1365-2133.2007.08028.x. [DOI] [PubMed] [Google Scholar]
- 24.Li J, O'Reilly N, Sheha H, Katz R, Raju VK, Kavanagh K, et al. Correlation between ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in patients with Facial rosacea. Ophthalmology. 2010;117:870–7. doi: 10.1016/j.ophtha.2009.09.057. [DOI] [PMC free article] [PubMed] [Google Scholar]


