Annular lesions are extremely common and striking in appearance, but can also be misleading. The term “annular” stems from the Latin word “annulus,” meaning ringed. Herein, we enumerate different presentations of annular lesions.
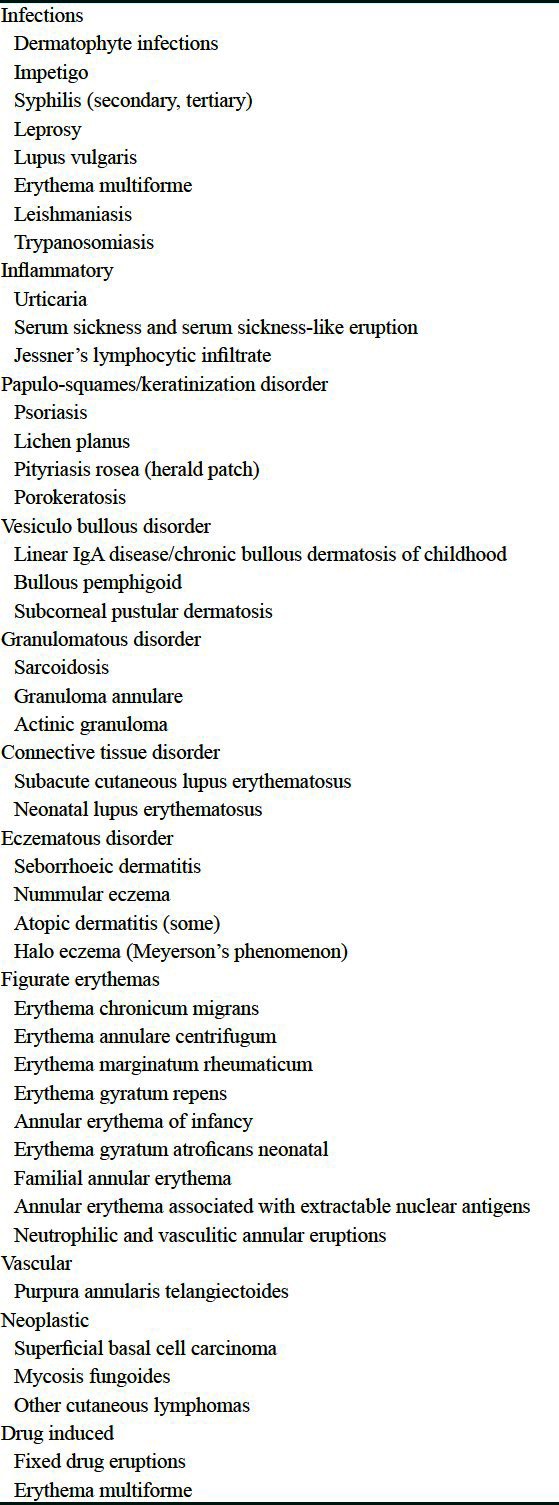
Annular lesions are classified as Table 1.
Table 1.
Causes for annular lesions
Tinea corporis is characterized by annular or polycyclic lesions with erythematous and vesicular or scaly border with central clearing[1] Figure 1]. Tinea imbricata is an unusual form of tinea corporis caused by Trichophyton concentricum, which is characterized by itchy, non-inflammatory, concentric rings.[2] In bullous impetigo, occasionally the bullae spreads peripherally with central clearing, producing annular lesions called Impetigo Circinata. Varnish like yellow crust gives clue to diagnosis.[3] Secondary syphilis may be present as annular lesions. A thin white ring of scales on the surface of the lesion (Biette's collarette) is a valuable sign.[4]
Figure 1.

Tinea corporis showing peripheral spreading with central clearing
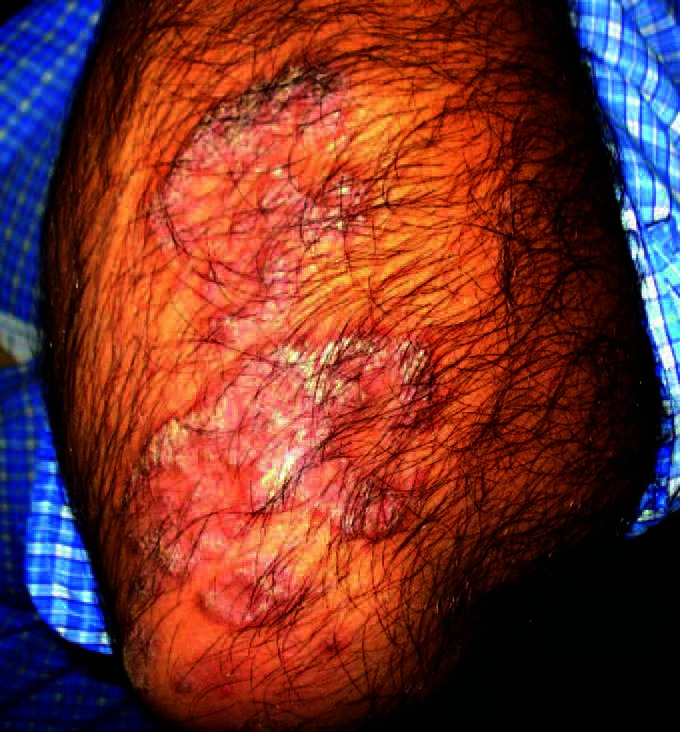
In leprosy, annular lesions usually represent borderline cases. There is loss of sensation over the lesion.[5] Lupus vulgaris may assume annular shape with central thin superficial scar and apple jelly nodule at the edge of the lesion[3] [Figure 2]. Cutaneous leishmaniasis presents with small furuncle at the site of inoculation with gradual peripheral spreading and central crusting giving annular appearance.[6] In secondary stage of Trypanosomiasis, transient erythematous or urticarial rashes, with circinate and annular pattern, will develop on the trunk.[7] Erythema multiforme has target lesions which has three zones: a central area of dusky erythema or purpura, a middle paler zone of oedema, and an outer ring of erythema with well-defined edge.[8]
Figure 2.

Lupus vulgaris
Chronic plaque psoriasis (psoriasis vulgaris) plaque, sometimes extends peripherally, the central part undergoes clearing, causing the formation of annular lesions called annular psoriasis, [Figure 3] which has good prognosis.[9] Subacute annular pustular psoriasis is a generalized type of pustular psoriasis characterized by multiple annular lesions with erythema, scaling, and pustules at the periphery.[10] Annular lichen planus is violaceous in color with very narrow rim of activity and a depressed, slightly atropic center found on penis.[11] Annular lichenoid dermatitis is a distinct entity in youth.[12,13] Herald patch of pitryiasis rosea is an oval or round lesion with typical collarette of scale at the margin.[14] Porokeratosis of Mibelli presents as a dry annular plaque surrounded by a raised, fine keratotic wall with characteristic furrow in it.[15]
Figure 3.
Annular psoriasis. Central cleared zone is often immune to psoriasis
Bullous pemphigoid, in the early stage presents as urticarial lesions. The erythematous component may become serpiginous, with peripheral blister.[16] Subcorneal pustular dermatoses (Sneddon-Wilkinson disease) presents as oval, peasized flaccid pustules which rupture easily, and tend to coalesce, forming annular or serpiginous patterns with a scaly edge. Characteristically, pus accumulates in the lower half of a fully developed pustule, leaving clear fluid in the upper half. Linear immunoglobulin A (IgA) dermatosis presents as lesions comprising urticated plaques and papules, and annular, polycyclic lesions often with blistering around the edge, the string of pearls sign [Figure 4][17].
Figure 4.

Linear IgA dermatosis showing string of pearls appearance
Granuloma annulare presents as closely set, skin-colored, firm, smooth asymptomatic papules arranged in a ring-like fashion [Figure 5]. Lesions usually resolve on its own without leaving any telltale mark.[18]
Figure 5.

Granuloma annulare in a diabetic
Subacute cutaneous lupus erythematosus (SCLE) [Figure 6] and Neonatal lupus erythematosus (NLE) presents as annular polycyclic lesions. 95% cases of NLE and 70% cases of SCLE show positivity for Anti-Ro/SSa auto antibodies.[19,20]
Figure 6.

Sub acute lupus erythematosus
Petaloid form of seborrhoic dermatitis sometimes assume annular pattern consisting of multiple circinate patches, with a fine branny scaling in their centers, and with dark-red papules with larger greasy scales at their margins.[21] After an acute phase, nummmular or discoid eczema may progress towards a less vesicular and more scaly stage, often with central clearing, and peripheral extension, causing ring-shaped or annular lesions. Nummular patches may accompany the more typical dry, erythematous scaling patches of atopic dermatitis. Meyerson described two patients with multiple pruritic, papulosquamous lesions surrounding melanocytic naevi which resolved spontaneously and termed it as Meyerson phenomenon or Halo eczema.[22]
Figurate erythemas are a group of dermatoses mostly developing in response to an underlying condition. Erythema gyratum repens is characterized by multiple, annular, concentric, rapidly growing erythematous plaques with a trailing scale resembling wood grain.[23] Erythema anulare centrifugum (EAC) presents as multiple, annular, polycyclic, slowly growing erythematous plaques with a trailing scale. It is usually pruritic and often spares palms and soles.[24] Erythema chronicum migrans is a skin finding at early stages of borreliosis, and erythema marginatum is the rapidly disappearing erythematous rash of acute rheumatic fever.[25] Annular erythema of infancy has clinical morphology of EAC but occurs in infancy.[26] Erythema gyratum atrophicans transiens neonatale is now felt to be a variant of NLE.[27] Autosomal dominant annular erythema is noted in a family and termed as familial annular erythemas.[28] Neutrophilic and vasculitic annular eruptions includes acute hemorrhagic oedema of infancy, erythema elevatum diutinum, urticarial vasculitis, Henoch-Schönlein purpura, and some cases of leukocytoclastic vasculitis associated with myeloma, inflammatory bowel disease or pregnancy.[29]
Basal cell carcinoma or rodent ulcer sometimes present as slowly expanding annular plaque with translucent or pearly, raised periphery with central ulceration.[30] Mycosis fungoides in the initial phase of T1/IA andT2/IB may present with annular plaques.[31]
Fixed drug eruptions presents as well-defined erythematous, violaceous or hyperpigmented macule with erythematous ring around it [Figure 7]. It frequently involves oral mucosa, glans penis, hands, and feet.[32]
Figure 7.

Fixed drug eruption with erythematous ring. Sometimes erythematous ring around old lesion is the only sign of recurrence
Purpura annularis telangiectoides or Majocchi's disease is a chronic pigmented purpuric dermatosis characterized by punctiform red patechial telangiectatic patches, with centrifugal growth giving annular or serpiginous appearance. Cayenne pepper spots are characteristic.[33] Annular purpura which may occur when the skin is struck by table tennis ball (ping-pong patch) and in step aerobics.[34,35]
Annular lesions may also rarely be found in lupus erythematosus (LE),[36] chronic variant of sweet syndrome[37] and neutrophilic eccrine hidradinitis.[38]
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Kanwar AJ, De D. Superficial fungal infections. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. Mumbai: Bhalani Publishing House; 2010. pp. 261–3. [Google Scholar]
- 2.Hay RJ. Tinea imbricata. Curr Top Med Mycol. 1988;2:55–72. doi: 10.1007/978-1-4612-3730-3_3. [DOI] [PubMed] [Google Scholar]
- 3.Singh G, Kaur V, Singh S. Bacterial infectons. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. Mumbai: Bhalani Publishing House; 2010. pp. 227–47. [Google Scholar]
- 4.Sanchez MR. Sexually transmitted diseases. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ, editors. Fitzpatrick's Dermatology in General Medicine. New York: McGraw Hill; 2008. p. 1959. [Google Scholar]
- 5.Jopling WH, Mcdougall AC. Handbook of Leprosy. New Delhi: CBS Publishers and Distributors; 2002. The Disease; p. 43. [Google Scholar]
- 6.Nadim A, Faghih M. The epidemiology of cutaneous leishmaniasis in the Isfahan province of Iran. I. The reservoir II. The human disease. Trans R Soc Trop Med Hyg. 1968;61:534–49. doi: 10.1016/0035-9203(68)90140-5. [DOI] [PubMed] [Google Scholar]
- 7.Gelfand M. The early clinical features of Rhodesian trypanosomiasis with special reference to the “chancre” (local reaction) Trans R Soc Trop Med Hyg. 1966;60:376–9. doi: 10.1016/0035-9203(66)90304-x. [DOI] [PubMed] [Google Scholar]
- 8.Hsu S, Le EH, Khoshevis MR. Differential diagnosis of annular lesions. Am Fam Physician. 2001;64:289–97. [PubMed] [Google Scholar]
- 9.Pavithran K, Karunakaran M, Palit A, Raghunath S. Disorders of keratinization. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. Mumbai: Bhalani Publishing House; 2010. p. 1033. [Google Scholar]
- 10.Baker H. Pustular psoriasis. Dermatol Clin. 1984;2:455. [Google Scholar]
- 11.Reich HL, Nguyen JT, James WD. Annular lichen planus: A case series of 20 patients. J Am Acad Dermatol. 2004;50:595–9. doi: 10.1016/j.jaad.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Annessi G, Paradisi M, Angelo C, Perez M, Puddu P, Girolomoni G. Annular lichenoid dermatitis of youth. J Am Acad Dermatol. 2003;49:1029–36. doi: 10.1016/s0190-9622(03)02147-9. [DOI] [PubMed] [Google Scholar]
- 13.Kleikamp S, Kutzner H, Frosch PJ. Annular lichenoid dermatitis of youth-a further case in a 12-year-old girl. J Dtsch Dermatol Ges. 2008;6:653–6. doi: 10.1111/j.1610-0387.2008.06575.x. [DOI] [PubMed] [Google Scholar]
- 14.Parsons JM. Pityriasis rosea update: 1986. J Am Acad Dermatol. 1986;15:159–67. doi: 10.1016/s0190-9622(86)70151-5. [DOI] [PubMed] [Google Scholar]
- 15.Virgili A, Strumia R. Annular hyperkeratosis. Porokeratosis of Mibelli. Arch Dermatol. 1986;122:586–7. doi: 10.1001/archderm.122.5.586. [DOI] [PubMed] [Google Scholar]
- 16.Stanley JR. Bullous pemphigoid. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ, editors. Fitzpatrick's Dermatology in General Medicine. New York: McGraw Hill; 2008. pp. 476–80. [Google Scholar]
- 17.Wojnarowska F, Venning VA. Immunobullous diseases. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Oxford: Wiley-Blackwell; 2010. pp. 40–21. [Google Scholar]
- 18.Mathai R. Necrobiotic disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. Mumbai: Bhalani Publishing House; 2010. pp. 1194–5. [Google Scholar]
- 19.Sontheimer RD. Subacute cutaneous lupus erythematosus: A decade's perspective. Med Clin North Am. 1989;73:1073. doi: 10.1016/s0025-7125(16)30620-4. [DOI] [PubMed] [Google Scholar]
- 20.Lee LA. Neonatal lupus erythematosus. J Invest Dermatol. 1993;100:9–13. doi: 10.1111/1523-1747.ep12355173. [DOI] [PubMed] [Google Scholar]
- 21.Berth-jones J. Eczema, lichenification, Prurigo and erythroderma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Oxford: Wiley-Blackwell; 2010. pp. 23.9–23.31. [Google Scholar]
- 22.Meyerson LB. A peculiar papulosquamous eruption involving pigmented nevi. Arch Dermatol. 1971;103:510–2. [PubMed] [Google Scholar]
- 23.Bolognia JL, Jorizzo JL, Rapini RP. Erythemas. In: Espana A, editor. Dermatology. 1st ed. Edinburg: Mosby; 2003. pp. 303–11. [Google Scholar]
- 24.Wong LC, Kakakios A, Rogers M. Congenital annular erythema persisting in a 15-year-old girl. Australas J Dermatol. 2002;43:55–61. doi: 10.1046/j.1440-0960.2002.00556.x. [DOI] [PubMed] [Google Scholar]
- 25.Serdar ZA, Mansur AT, Yasar SP, Endogru E, Gunes P. Erythema gyratum repens-like atypical and persistent figurate erythema. Indian J Dermatol. 2009;54:24–6. [Google Scholar]
- 26.Peterson AO Jr, Jarratt M. Annular erythema of infancy. Arch Dermatol. 1981;117:145–8. [PubMed] [Google Scholar]
- 27.Puig L, Moreno A, Alomar A, de Moragas JM. Erythema gyratum atrophicans transiens neonatale: A variant of cutaneous neonatal lupus erythematosus. Pediatr Dermatol. 1988;5:112–6. doi: 10.1111/j.1525-1470.1988.tb01150.x. [DOI] [PubMed] [Google Scholar]
- 28.Beare JM, Froggatt P, Jones JH, Neill DW. Familial annular erythema. An apparently new dominant mutation. Br J Dermatol. 1966;78:59–68. doi: 10.1111/j.1365-2133.1966.tb12176.x. [DOI] [PubMed] [Google Scholar]
- 29.Nousari HC, Kimyai-Asadi A, Stone JH. Annular leukocytoclastic vasculitis associated with monoclonal gammopathy of unknown significance. J Am Acad Dermatol. 2000;43:955–7. doi: 10.1067/mjd.2000.103643. [DOI] [PubMed] [Google Scholar]
- 30.Afzelius LE, Ehnhage A, Nordgren H. Basal cell carcinoma in the head and neck. The importance of location and histological picture, studied with a new scoring system, in predicting recurrences. Acta Pathol Microbiol Scand A. 1980;88:5–9. [PubMed] [Google Scholar]
- 31.Kashani-Sabet M, McMillan A, Zackheim HS. A modified staging classification for cutaneous T-cell lymphoma. J Am Acad Dermatol. 2001;45:700–6. doi: 10.1067/mjd.2001.117722. [DOI] [PubMed] [Google Scholar]
- 32.Bilimoria PE, Shah BJ. Drug reactions. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. Mumbai: Bhalani Publishing House; 2010. p. 1647. [Google Scholar]
- 33.Majocchi D. Purpura annularis telangiectoides.“Telangiectasis follicuritis annulata”. Arch Dermatol Syph. 11898;43:447–68. [Google Scholar]
- 34.Scott MJ, Jr, Scott MJ., III Pingpong patches. Cutis. 1989;43:363–5. [PubMed] [Google Scholar]
- 35.Allan SJ, Humphreys F, Buxton PK. Annular purpura and step aerobics. Clin Exp Dermatol. 1994;19:418. doi: 10.1111/j.1365-2230.1994.tb02698.x. [DOI] [PubMed] [Google Scholar]
- 36.Piqué E, Palacios S, Santana Z. Leukocytoclastic vasculitis presenting as an erythema gyratum repens–like eruption on a patient with systemic lupus erythematosus. J Am Acad Dermatol. 2002;47:S254–6. doi: 10.1067/mjd.2002.108590. [DOI] [PubMed] [Google Scholar]
- 37.von den Driesch P. Sweet's syndrome (acute febrile neutrophilic dermatosis) J Am Acad Dermatol. 1994;31:535–56. doi: 10.1016/s0190-9622(94)70215-2. [DOI] [PubMed] [Google Scholar]
- 38.Scong VY, Appell ML, Sanders DY, Omura EF. Annular plaques on the dorsa of the hands. Neutrophilic eccrine hidradenitis. Arch Dermatol. 1991;127:1398–9. doi: 10.1001/archderm.127.9.1398. 1400-2. [DOI] [PubMed] [Google Scholar]


