Sir,
Hypopigmented mycosis fungoide (HMF) was first reported by Ryan et al. in 1973.[1] It is a rare, atypical and often misdiagnosed variant of MF characterized by persistent hypopigmented patches and occurs mainly in dark-skinned individuals, especially children.[2]
A 29-year-old Chinese woman presented with a nearly 20-year history of asymptomatic hypopigmented patches on her buttocks and extremities. Her parents had first noted hypopigmented patches of the inner thighs. Since then, the lesions gradually progressed to involve her buttocks, waist and arms. In addition, erythema, atrophy and scale appeared in some lesions. She had no obvious subjective symptoms. By the time she was 12 years old, she was diagnosed with vitiligo in a local hospital. There were no systemic symptoms. General physical examination revealed no abnormalities. Skin examination showed large, irregular, hypopigmented patches covered partly by fine scales on her buttocks and extremities. Some of the lesions on the buttocks had mild erythema or cigarette paper-like atrophy [Figure 1]. No sensory loss was found in the lesions. Punch biopsy was taken from the hypopigmented patch on her left buttock. Histopathological examination showed epidermotropism of single and clustered lymphocytes (Pautrier's microabscesses). In the superficial dermis, a band-like infiltrate of lymphocytes was observed. Some of the lymphocytes in the epidermis and dermis exhibited atypical, hyperchromatic nuclei with irregular contours [Figure 2a and b]. Immunohistologically, the phenotype of the atypical cells was CD3+, CD4+, CD5+, CD8+, CD43+, Ki67+, CD20-, CD30-, and CD79a- [Figure 2c, d, e and f]. Complete blood count, liver and renal function tests, ultrasonography of abdomen and pelvis, and chest X-ray were within normal limits. No atypical lymphocytes were seen in peripheral blood smear. T cell receptor gene rearrangement by PCR was negative. With the clinical, histopathlogical and inmmunohistochemical findings, the patient was diagnosed with HMF. We advised the patient for NB-UVB treatment. Then the patient failed to be followed up.
Figure 1.

Irregular, hypopigmented patches on the buttocks, with fine scales, erythema or cigarette paper - like atrophy in some areas
Figure 2.
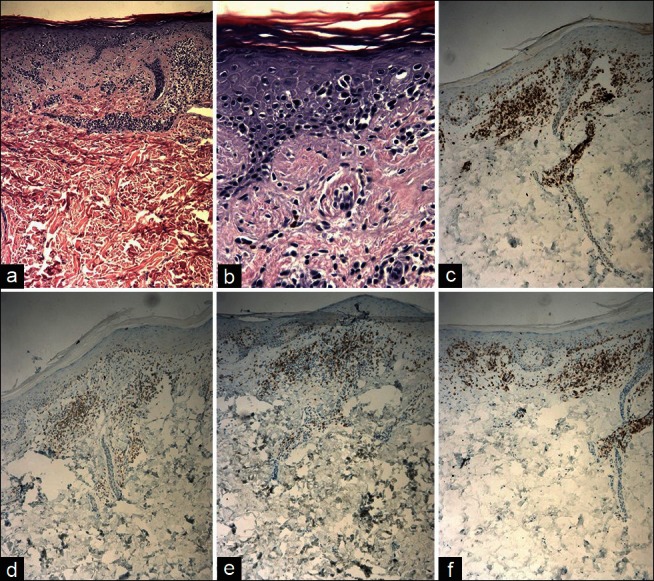
(a,b) H & E stain showing epidermotropism of single and clustered lymphocytes (Pautrier's microabscesses). (c) CD3+ lymphocytes in epidermis and papillary dermis. (d) CD4+ lymphocytes in epidermis and papillary dermis. (e) CD5+ lymphocytes in epidermis and papillary dermis. (f) CD8+ lymphocytes in epidermis and papillary dermis. Original magnifications: (a) 10×, (b) 40×, (c, d, e, f) 10×
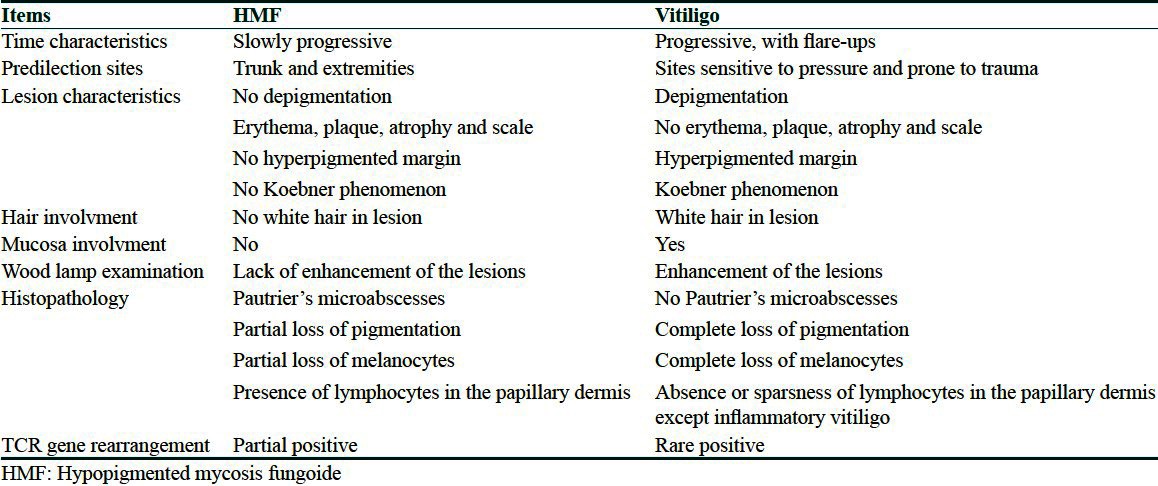
MF is the most common type of cutaneous T-cell lymphoma. HMF is just one of the less common variants of MF. Although rare, the exact frequency of HMF is still unknown. It was reported that there were 113 patients with HMF till 2003.[3] Till now, the HMF cases reported in China are even less, just 7 patients (including our case).[4] It may be related to little awareness of HMF or misdiagnosed as other diseases (such as vitiligo, indeterminate leprosy, postinflammatory hypopigmentation, pityriasis alba, tinea versicolor, sarcoid and leishmaniasis). Before coming to our hospital, the current case was ever diagnosed with vitiligo in the local hospitals. It is therefore important to completely distinguish between HMF and vitiligo. EI-Darouti et al.[5] discussed the differentiation between HMF and vitiligo on histopathological and immunohistochemical aspects. But the clinical differences between the two diseases were not mentioned. So we differentiated HMF and vitiligo by clinical, pathological, immunohistochemical and genetic features [Table 1].
Table 1.
Differential dignosis of hypopigmented mycosis fungoide and vitiligo
Like classic MF, HMF has an indolent clinical course with slow progress over years or decades. The skin lesions of HMF have a predilection for the trunk and extremities which are similar to that of classic MF. The persistent hypopigmented macules and patches are the main lesions in HMF which are asymptomatic, ill-defined and mild dry. In addition, slightly atrophy or scaling or infiltrated erythematous patches or plaques may be seen in HMF. Histologically, epidermotropism of T cells or Pautrier's abscess can be observed in HMF, which is indistinguishable from classic MF. Unlike classical MF which usually shows CD4 positive T cells, HMF often shows a T supressor CD8(+) phenotype. Some patients with HMF have a positive T-cell receptor gene rearrangement.[3] Ultrastructural studies reveal degeneration of melanocytes adjacent to mycosis cells. The degenerative changes in melanocytes include swelling of cytoplasmic organelles, spherical incompletely melanized melanosomes and disintegrating melanocytes.
HMF treatment is similar to that of early-stage MF. The treatment of HMF consists of topical nitrogen mustard, topical carmustine, topical corticosteroid, psoralen plus ultraviolet A (PUVA) and narrow band ultraviolet B (NB-UVB). According to Sezer et al.,[6] NB-UVB is the promising treatment for HMF due to some additional advantages (safer and more convenient) compared with PUVA. The patients with HMF often show a good response to the above treatments. But recurrences are common.
References
- 1.Ryan EA, Sanderson KV, Bartak P, Samman PD. Can mycosis fungoides begin in the epidermis? A hypothesis. Br J Dermatol. 1973;88:419–29. doi: 10.1111/j.1365-2133.1973.tb15444.x. [DOI] [PubMed] [Google Scholar]
- 2.Al-Ratrout1 JT, Al-Nazer M, Ansari NA. Hypopigmented mycosis fungoides in a twenty-year-old Saudi woman with fair skin. Indian J Dermatol. 2006;51:115–7. [Google Scholar]
- 3.Ardigó M, Borroni G, Muscardin L, Kerl H, Cerroni L. Hypopigmented mycosis fungoides in Caucasian patients: A clinicopathologic study of 7 cases. J Am Acad Dermatol. 2003;49:264–70. doi: 10.1067/s0190-9622(03)00907-1. [DOI] [PubMed] [Google Scholar]
- 4.Wang T, Liu YH, Zheng HY, Sun QN, Jin HZ, Li F, et al. Hypopigmented mycosis fungoides in children: A clinicopathological study of 6 cases. Zhonghua Yi Xue Za Zhi. 2010;90:3287–90. [PubMed] [Google Scholar]
- 5.EI-Darouti MA, Marzouk SA, Azzam O, Fawzi MM, Abdel-Halim MR, Zayed AA, et al. Vitiligo vs. hypopigmented mycosis fungoides (histopathological and immunohistochemical study, univariate analysis) Eur J Dermatol. 2006;16:17–22. [PubMed] [Google Scholar]
- 6.Sezer E, Sezer T, Senayli A, Koseoglu D, Filiz N. Hypopigmented mycosis fungoides in a Caucasian child. Eur J Dermatol. 2006;16:584. [PubMed] [Google Scholar]


