Sir,
Demonstration of intercellular deposition of IgG on the cell surface of the keratinocyte, by direct immunofluorescence (DIF) of perilesional skin, is the gold standard in the diagnosis of pemphigus. Recently, DIF of plucked hair has shown to be a useful test in the diagnosis of pemphigus, with a sensitivity ranging from 85 to 100%.[1–3] Our objective in this study was to determine the utility of DIF of plucked hair in monitoring the disease activity in pemphigus.
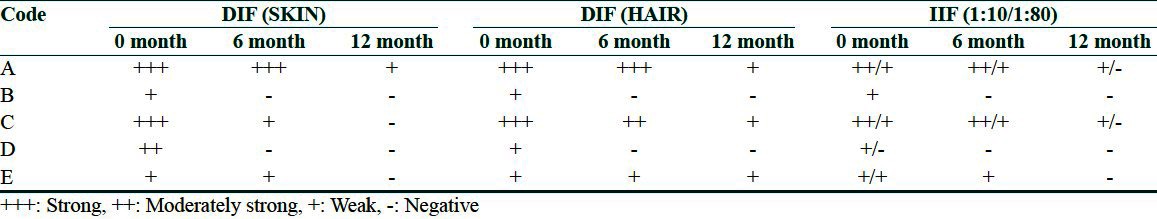
Five patients of pemphigus vulgaris (PV), attending the skin clinic of a tertiary care hospital, were enrolled in the study after obtaining institutional ethical clearance. DIF of perilesional skin, scalp hair and indirect immunofluorescence (IIF) in two dilutions (1:10 and 1:80) using normal skin as substrate was done at 0, 6 and 12 months; skin biopsy for DIF was obtained either from the perilesional skin or from the normal upper back, when the patient was in clinical remission. A detailed history was taken and clinical examination was carried out in them, at each visit. Results of immunofluorescence were recorded as strong (+++), moderately strong (++), weak (+) and negative (-) by the same observer.
Mean age of the patients (two males and three females) in the study group was 51.4 years. For the purpose of recording and comparison, patients were coded alphabetically from A to E. All patients had active disease at the time of enrollment in the study [Table 1]. Intercellular deposition of IgG was seen in all patients with DIF and IIF [Table 2]. At the 6-month follow-up, tests were negative in two patients who were in clinical remission. It remained positive in three patients who showed signs of disease activity. At the 12-month follow-up, three patients were in clinical remission; DIF of hair remained positive in one of them. DIF of hair was positive in the other two patients who had persistent oral ulceration.
Table 1.
Demographic and Clinical profile of patients
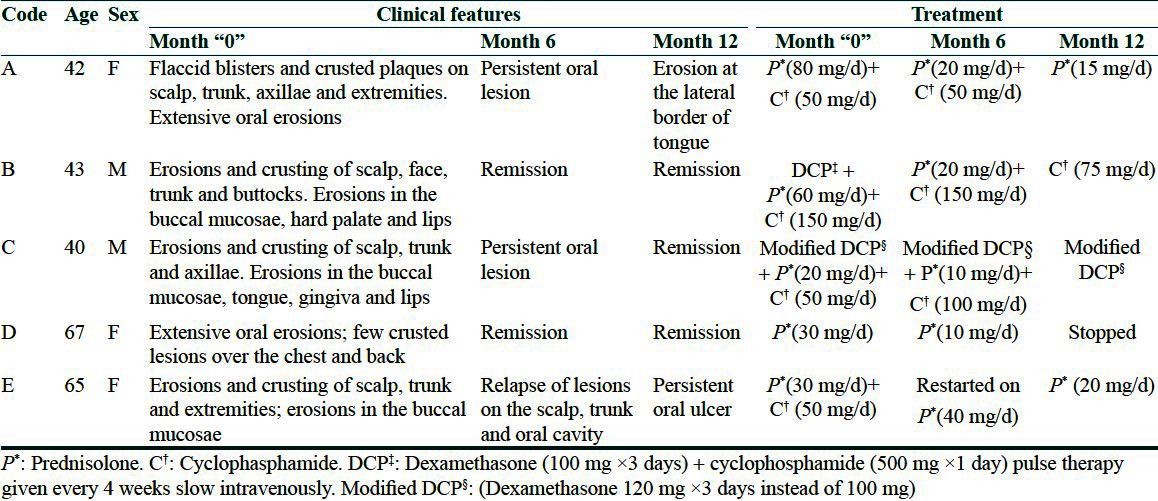
Table 2.
Immunofluorescence results at 0, 6 and 12 months
In this study, we tried to evaluate the role of DIF of hair in monitoring the disease activity. We found it to be a very useful test in the diagnosis as all the patients showed positivity at the time of enrollment. The test was negative in two patients who were in clinical remission at the 6th and 12th months. It remained positive throughout the study period in one patient with persistent oral erosions. Although DIF (skin) was negative in the other two patients at the 12th month, intercellular IgG deposits could be seen in the outer root sheath (ORS) of hair [Figure 1] in both these patients. One among them had persistent oral ulcers while the other patient was in clinical remission. The probable explanation for such a finding is that hair follicle with its ORS has the greatest density of PV antigens. As a result, antibodies may have a greater affinity to these structures and may remain there for a relatively longer period, to be able to be detected by DIF as compared with skin.
Figure 1.
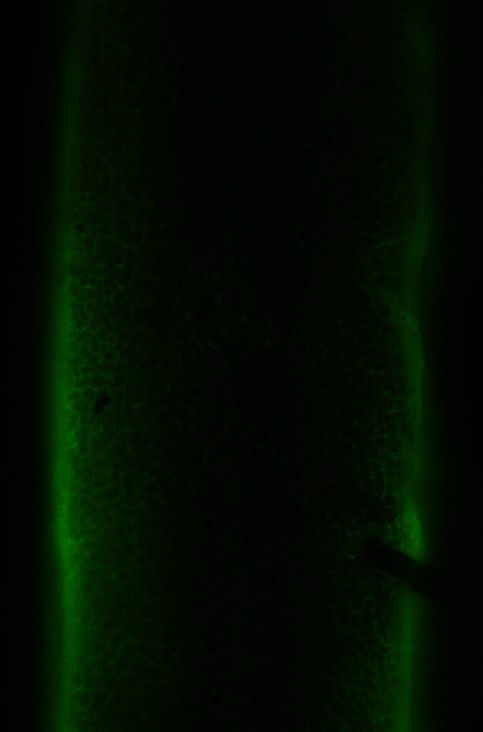
Photomicrograph showing intercellular deposition of IgG in the outer root sheath (direct immunofluorescence, ×20)
The goal of therapy in pemphigus is to achieve clinical and immunological remission. Clinical remission could be achieved in most patients with immunosuppressive agents. The most difficult management decision is how to maintain remission with the least number of medications. IIF has been widely used to monitor the serological activity of pemphigus patients on treatment. The titer of antibodies in the sera of patients is, in many instances, proportionate to the severity of the disease. However, there are too many exceptions for the titer to be regarded as a reliable index for the disease severity;[4] Judd and Lever argued that IIF is not a reliable test for evaluating the status of disease at least in some patients.[5] They found that administration of a high dose of daily steroids resulted in clinical improvement as well as showed a marked fall in the titer of circulating antibodies. However, there was no predictable correlation between the disease activity and antibody titer when the patients were not receiving a high dose of steroids.[5] Earlier studies have observed that DIF performed during the periods of clinical remission is valuable in the management of the disease as negative DIF may be viewed as a state of immunological remission.[6] According to a previous report, many patients with negative DIF findings (73.3%) remained in clinical remission after discontinuation of treatment. All patients with positive DIF findings during remission had a relapse within 3 months after discontinuation of treatment.[7] Thus, DIF findings may be indicative of either further regression or eminent exacerbation. Therapy should be continued in patients with positive DIF results as they have a high chance of relapse.[8] On the other hand, repeated negative DIF during remission is a possible marker for apparent cure of the disease, and treatment may be stopped in such group of patients.[6] Patients in remission may refuse to undergo repeated skin biopsies. DIF of hair may be an ideal choice of substrate as it is a simple and non-invasive test with a high degree of sensitivity and specificity.[3] We recommend further studies using a large number of subjects to be carried out to elucidate our results.
References
- 1.Rao R, Dasari K, Shenoi S, Balachandran C. Demonstration of pemphigus-specific immunofluorescence pattern by direct immunofluorescence of plucked hair. Int J Dermatol. 2009;48:1187–9. doi: 10.1111/j.1365-4632.2009.04153.x. [DOI] [PubMed] [Google Scholar]
- 2.Daneshpazhooh M, Asgari M, Naraghi ZS, Barzgar MR, Akhyani M, Balighi K, et al. A study on plucked hair as a substrate for direct immunofluorescence in pemphigus vulgaris. J Eur Acad Dermatol Venereol. 2009;23:129–31. doi: 10.1111/j.1468-3083.2008.02948.x. [DOI] [PubMed] [Google Scholar]
- 3.Schaerer L, Trueb RM. Direct immunofluorescence of plucked hair. Arch Dermatol. 2003;139:228–9. doi: 10.1001/archderm.139.2.228. [DOI] [PubMed] [Google Scholar]
- 4.Creswell SN, Black MM, Bhogal B, Skeete MV. Correlation of circulating intercellular antibody titres in pemphigus with disease activity. Clin Exp Dermatol. 1981;6:477–83. doi: 10.1111/j.1365-2230.1981.tb02338.x. [DOI] [PubMed] [Google Scholar]
- 5.Judd KP, Lever WF. Correlation of antibodies in skin and serum with disease severity in pemphigus. Arch Dermatol. 1979;115:428–32. [PubMed] [Google Scholar]
- 6.David M, Weissman-Katzenelson V, Ben-Chetrit A, Hazaz B, Ingber A, Sandbank M. The usefulness of immunofluorescent tests in pemphigus patients in clinical remission. Br J Dermatol. 1989;120:391–5. doi: 10.1111/j.1365-2133.1989.tb04165.x. [DOI] [PubMed] [Google Scholar]
- 7.Ratnam KV, Pang BK. Pemphigus in remission: Value of negative immunofluorescence in management. J Am Acad Dermatol. 1994;30:547–50. doi: 10.1016/s0190-9622(94)70060-5. [DOI] [PubMed] [Google Scholar]
- 8.Balighi k, Taheri A, Mansoori P, Chams C. Value of direct immunofluorescence in predicting remission in pemphigus vulgaris. Int J Dermatol. 2006;45:1308–11. doi: 10.1111/j.1365-4632.2006.02916.x. [DOI] [PubMed] [Google Scholar]


