Sir,
Sixty-five percent of cutaneous lymphomas are of T-cell origin.[1] Primary cutaneous lymphomas are those in which skin involvement by tumor is clinically evident with no extracutaneous disease at the time of diagnosis or 6 months thereafter.[2] Lymphoproliferative disorders of the primary cutaneous CD30+ type, of T cell origin, consist of lymphomatoidpapulosis and CD30+ anaplastic large cell lymphoma.[3,4] There are no clinical differences in presentation, course or prognosis between anaplastic and nonanaplastic CD30+ primary nodal large cell lymphoma (LCL).[4]
A 65-year-old diabetic man demonstrated a fleshy, irregular, slightly painful, firm swelling, comprising lobulated nodules on the middle of flexor aspect of right forearm [Figure 1] present for 1 year. The lesion was treated as keloid on several occasions with no results.
Figure 1.

Lobulated mass on the right forearm near the bend of elbow of the patient
Regional draining lymph nodes were not palpable. Blood biochemistry, including serum calcium, was normal. Hemoglobin was 9.7 gm/dL. Peripheral blood smear examination showed a microcytic hypochromic blood picture. Bone marrow aspiration biopsy showed erythroid hyperplasia with features of iron deficiency erythropoesis and no evidence of infiltration. There was no evidence of lymphadenopathy on computed tomography (CT) scans of the chest, abdomen and pelvis.
Excision biopsy and histopathology revealed a lesion composed of sheets and nests of polygonal cells with large vesicular nucleoli and eosinophilic cytoplasm [Figure 2]. The tumor showed brisk mitotic activity.
Figure 2.
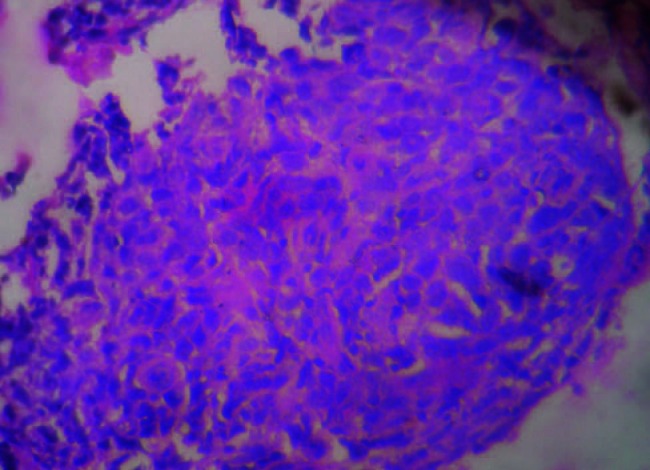
Histopathology of tumor displaying sheets and nests of polygonal cells with large vesicular nucleoli and eosinophilic cytoplasm (H and E, ×10)
Immunohistochemistry revealed expression of CD30 by the tumor cells that were immunonegative for CD20, CD3 and EMA.
A final diagnosis of primary cutaneous anaplastic large cell lymphoma was made. Patient was sent to the radiotherapist for treatment after removal of the tumor. Three months have elapsed after completion of radiotherapy without any recurrence of the tumor.
CD30+ primary cutaneous large cell lymphoma (PCLCL) presents as one to several localized nodules or tumors with ulceration. The trunk and extremities are most commonly involved. There are no features suggestive of mycosis fungoides. Presentation may be variable, with this lesion being mistaken for other skin disorders, like adult onset eczema, pyodermagangrenosum, pyogenic granuloma, morpheaor squamous cell carcinoma.[5]
Additional common manifestations are epidermal ulceration (63%), prominent vascular proliferation (60%), pseudoepitheliomatous hyperplasia (55%), tumor necrosis (55%) and vascular infiltration by neoplastic cells (44%).
CD30+ anaplastic large cell lymphomas are typically associated with poor prognosis when they are systemic.[4] Primary cutaneous CD30+ T-cell lymphoma arising as an isolated nodule on the right leg of a person who had a heart transplant several years earlier make interesting study. The nodule responded favorably to excisional biopsy and radiotherapy.[6] It is crucial to distinguish CD30+ PCLCL from LCL with secondary cutaneous involvement. CT scan of the abdomen and bone marrow examination are necessary to rule out systemic anaplastic large cell lymphoma with secondary cutaneous involvement. Patients with secondary skin disease generally have worse prognosis and need excision or radiation. Chemotherapy is reserved for patients with systemic involvement. Treatment of patients with only skin and nodal disease is controversial, with some practitioners favoring radiation and chemotherapy for these patients.
Primary cutaneous CD30-positive large T-cell lymphoma is distinguished from other cutaneous T-cell lymphomas by the expression of the CD30 antigen on immunohistological staining.
Chronic swelling in an elderly person without systemic manifestations or lymphatic involvement can still be a variety of lymphoma, which if diagnosed and treated early, bestows excellent prognosis.
References
- 1.Garbea A, Dippel E, Hildenbrand R, Bleyl U, Schadendorf D, Goerdt S. Cutaneous large B-cell lymphoma of the leg masquerading as a chronic venous ulcer. Br J Dermatol. 2002;146:144–7. doi: 10.1046/j.0007-0963.2001.04520.x. [DOI] [PubMed] [Google Scholar]
- 2.Willemze R, Kerl H, Sterry W, Berti E, Cerroni L, Chimenti S, et al. EORTC classification for primary cutaneous lymphomas: A proposal from the Cutaneous Lymphoma Study Group of the European Organization for Research and Treatment of Cancer. Blood. 1997;90:354–71. [PubMed] [Google Scholar]
- 3.Hembury TA, Lee B, Gascoyne RD, Macpherson N, Yang B, House N, et al. Primary cutaneous diffuse large B-cell lymphoma: A clinicopathologic study of 15 cases. Am J Clin Pathol. 2002;117:574–80. doi: 10.1309/edal-r8ha-u3el-t37d. [DOI] [PubMed] [Google Scholar]
- 4.Beljaards RC, Kaudewitz P, Berti E, Gianotti R, Neumann C, Rosso R, et al. Primary cutaneous CD30-positive large cell lymphoma: Definition of a new type of cutaneouslymphoma with a favorable prognosis. A European Multicenter Study of 47 patients. Cancer. 1993;71:2097–104. doi: 10.1002/1097-0142(19930315)71:6<2097::aid-cncr2820710626>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 5.Krishnan J, Tomaszewski MM, Kao GF. Primary cutaneous CD30-positive anaplastic large cell lymphoma. Report of 27 cases. J Cutan Pathol. 1993;20:193–202. doi: 10.1111/j.1600-0560.1993.tb00643.x. [DOI] [PubMed] [Google Scholar]
- 6.Belloni-Fortina A, Montesco MC, Piaserico S, Bordignon M, Tona F, Feltrin G, et al. Primary cutaneous CD30+ anaplastic large cell lymphoma in a heart transplant patient: Case report and literature review. Acta Derm Venereol. 2009;89:74–7. doi: 10.2340/00015555-0543. [DOI] [PubMed] [Google Scholar]


