Abstract
Leprosy has been considered a curable disease after the implementation of multidrug therapy (MDT), which has been proven to be safe and effective, by bringing about a significant change in the global and national scenario of leprosy by upgrading the control of leprosy to the next stage of eradication. Since its introduction, the MDT regimens for the treatment of leprosy have undergone several changes especially with regard to the duration of treatment. The advantages of shortened duration of treatment need to be balanced against the risk of relapse and a lot of controversies exist pertaining to this aspect. The fixed-duration (FD) therapy is not popular among academicians and private practitioners who prefer precise diagnosis and treatment with superior MDT regimens and for a longer duration. On the contrary, from a public health-care point of view, precise diagnosis and a longer treatment schedule are not cost effective and not feasible to be implemented in elimination programs. Hence, a fine balance needs to be maintained between achieving a cure for the patient and protecting the society at risk, and this review discusses the various limitations and opportunities of FD therapy with a note on the newer MDT regimens.
Keywords: Fixed duration, leprosy, multibacillary, multidrug therapy, paucibacillary
Introduction
What was known?
Since its introduction, the multidrug therapy (MDT) regimens for the treatment of leprosy have undergone several changes especially with regard to the duration of treatment. The advantages of shortened duration of treatment need to be balanced against the risk of relapse and a lot of controversies exist pertaining to this aspect. The fixed-duration (FD) therapy is not popular among academicians and private practitioners who prefer precise diagnosis and treatment with superior MDT regimens and for a longer duration.
Leprosy, a disease which had been a scourge of mankind for many decades was considered a curable disease after the implementation of multidrug therapy (MDT) by the World Health Organization (WHO) in 1982. MDT has proved its effectiveness in bringing about a significant change in the leprosy scenario, both at the global and national level, by bringing down the case loads to the extent that leprosy no longer continues to be a disease of public health-care importance. In addition to being effective, it has also been proved to be safe as well as acceptable to the patients as well as program managers. In spite of these advantages, there are some controversies regarding the current MDT regimens especially among academicians and private practitioners who prefer precise diagnosis and treatment with superior MDT regimens and for longer duration, but these are not cost effective, thereby not warranting their implementation in the leprosy elimination programs.
Global and Indian Scenario
The global registered prevalence of leprosy in the beginning of 2011 as per the WHO official reports received during 2011, from 130 countries and territories, was 192,246 cases, whereas the number of new cases detected during 2010 was 228,474 and the figure for India was 1,26,800, which accounts for an alarming 55.5%.[1,2] Pockets of high endemicity still remain in some areas of India[1] like Bihar and Chattisgarh which are yet to achieve elimination (with a prevalence rate of 1.12 and 1.94, respectively).[3]
History of MDT
The WHO Executive Board reviewed and endorsed the reports of the ‘study Group on Chemotherapy of Leprosy for Control Programmes’ on 17 May, 1982 which is the official ‘date of birth’ of MDT.[4] MDT was recommended for the following reasons:[5]
To address resistance to dapsone and to discourage resistance to other drugs to be used.
To promote compliance and to move away from long-term monotherapy such as dapsone.
To retain rifampicin in all therapeutic regimens because of its powerful bactericidal action and its effectiveness even when taken once a month.
To promote compliance and cost effectiveness.
There were four successive phases in the implementation of MDT which were as follows:[4]
1982–1985: Introduction of MDT on a global basis.
1986–1990: Expansion of MDT (into the ‘less difficult’ areas).
1991–1999: Elimination strategy.
2000 onward: A fourth period, planned to last six years, designated for the ‘Intensive elimination strategy’ or the ‘Final push’.
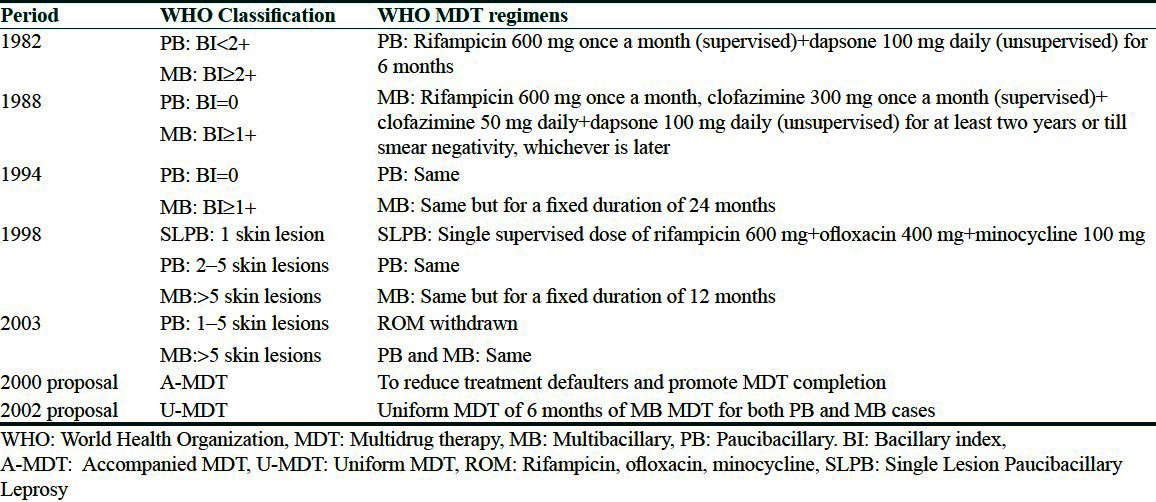
The changes in the classification of paucibacillary (PB) and multibacillary (PB) leprosy and MDT regimens are presented in Table 1.[4,6–9]
Table 1.
Classification of paucibacillary and multibacillary leprosy and MDT regimens: Changes over time
Differences in Classification of Leprosy Cases and MDT Implementation in India
Until 1995, leprosy cases with more than 10 lesions (counting number of skin and nerve lesions involved) were classified as MB. In addition, all cases where skin smear testing gave positive results were classified as MB, irrespective of the number of skin and nerve lesions. Since 1996, the WHO criterion of six or more skin lesions has been used for MB classification.[10] The criteria of the National Leprosy Eradication Programme (NLEP) to classify PB and MB cases includes the number of nerves involved and the slit-skin smear results apart from the number of skin lesions to increase the sensitivity as well as to account for the pure neuritic cases.[11] Thus since 2009, the classification of PB and MB cases in India as per the recommendations of the NLEP is as follows:
PB: 1–5 skin lesions, no nerve or only one nerve with or without 1–5 skin lesions, slit-skin smears negative at all sites.
MB: ≥6 skin lesions, more than one nerve irrespective of the number of skin lesions, slit-skin smears positive at any site irrespective of the number of skin lesions or nerves.
The duration of treatment and MDT regimens for MB cases differed from those recommended by the WHO during the initial phases. At the time of the introduction of MDT in a district, the Indian Association of Leprologists recommended an intensive phase of 21 days of daily rifampicin 600 mg followed by the monthly pulsed dose recommended by the WHO for all prevalent MB cases. This was modified by the NLEP by reducing the intensive phase to 14 days. Since 1986, based on the reports of the Bombay Leprosy Project Study indicating the equal efficacy of the WHO regimen and intensive phase regimen, the WHO regimen was followed. However, the duration was not restricted to 24 months, but was continued until negativity of smear.[11,12] NLEP introduced 24-month FD MDT in 1994 and 12-month FD MDT since 1998. There has been no change with regard to the treatment regimen or duration of PB cases from the introduction of MDT in 1982.[10]
FD MDT Regimens
Currently, two FD MDT regimens are in vogue, the WHO regimen followed almost worldwide and the Public Health Service regimen followed in the United States.
The WHO regimen
PB: Rifampicin 600 mg monthly plus dapsone 100 mg daily; six cycles in nine months.[13]
MB: Rifampicin 600 mg plus clofazimine 300 mg monthly and dapsone 100 mg plus clofazimine 50 mg daily; 12 cycles in 18 months.
The WHO does not advocate post-therapy surveillance. Patients are advised to report as soon as they note any changes in skin, eyes, or nerves.
US National Hansen's Disease Program (NHDP) treatment recommendations
PB: Dapsone 100 mg daily plus rifampicin 600 mg daily for one year. Follow-up every six months for five years.[14]
MB: Dapsone 100 mg daily plus rifampicin 600 mg daily plus clofazimine 50 mg daily for two years. Follow-up every six months for 10 years.
Advantages of FD MDT
The effectiveness of FD MDT has been proved by its role in the elimination of leprosy and the acceptability by the patients and public health-care administrators worldwide. The validity of the efficacy of FD therapy in MB cases can be confirmed based on the scientific basis by which the duration of the 24-month MDT was further shortened to 12 months, which is as follows:
The modifications in the definitions of PB/MB cases over time have resulted in the misclassification of many cases. There is an increased proportion of MB cases among newly detected cases due to the classification of cases that would otherwise be PB leprosy. Thus, the bacterial load of the majority of currently diagnosed MB patients is significantly lesser than those in the past as also estimated by the WHO wherein the newly detected cases with high bacillary indices (BI ≥ 3) are less than 15%.[15] The net result would be a decrease in the overall requirements of chemotherapy for MB leprosy.
The rates of relapse among MB cases after 12 months of MDT, as estimated by the routine control programs as well as the research projects were very low, about 0.2% annually, similar to those observed after 24 months of MDT.[16] Nevertheless, higher rates of relapse have been reported in some studies[17,18] involving MB patients with a high initial bacillary index (BI) (average BI ≥ 4+). But, such patients are only a minority in the current scenario of the widespread use of MDT, and hence the relapses contributed by them will be small.
The dapsone-clofazimine combination is highly bactericidal as observed from nude mouse experiments and clinical trials wherein daily treatment with this combination killed more than 99.999% of viable Mycobacterium leprae in 3–6 months. Thus, this combination ensures the effective elimination of the spontaneously occurring rifampicin-resistant mutants which are usually not more than 10[4] organisms in an untreated lepromatous leprosy (LL) case.[16]
According to some studies [Steering Committee on Chemotherapy of Mycobacterial Diseases (THEMYC) and clinical trial in Malawi], the response of MB cases receiving fewer than the standard 24 doses of MDT was as promising as those receiving 24 doses or more.[16,19,20]
A retrospective study done on the clinical and bacteriological progress of defaulted MB cases revealed that treatment with less than 12 months of MDT still had favorable therapeutic effects among the majority of MB patients.[21]
Four WHO-sponsored studies to evaluate the efficacy of a variety of drug combinations and treatment periods have found that even though the bacillary load was reduced, a positive BI was still present at the end of 24 or 12 months. But these bacteria were no longer found to be viable as confirmed by mouse footpad inoculation. Moreover, as the immune system of MB cases is grossly deficient to mount an effective defense against M. leprae, the clearance of bacilli from the body becomes a slow process. It has also been observed that although BIs remained positive at the end of the treatment, they gradually declined during follow-up, tending to confirm that bacillary clearance is not affected by prolonging the intake of drugs. Considering these facts, it is possible to stop MDT safely despite a positive BI after a fixed duration of 24 or 12 months. Now, the problem lies in determining the exact duration of MDT to achieve maximum results for MB cases.[20,22,23]
Operationally, a long duration of treatment is a major obstacle to successful implementation of MDT. Thus, a reduction in the length of treatment without jeopardizing effectiveness would potentially facilitate patient compliance and national program activities especially in remote rural areas where medical care is often scarce and frequently inaccessible to most patients.[20]
By shortening the duration of MDT to 12 months, the disadvantages of reduced duration are likely to be minimal and even an occasional relapse or failure of treatment can be treated with the same regimen, as the relapse is due to drug-sensitive persisters.[24]
The advantages of FD MDT in PB cases are based on the following observations:
Though continued visibility of clinically active patches exist in a proportion of patients at the end of six months of therapy, this persisting activity is attributed to the continued inflammatory response of the system to clear the persisting killed mycobacteria, fragments, or antigens. It has been observed that, on follow-up, in 30 to 80% of these patients, the clinical activity gradually comes down and the patients get cured.[25]
Based on these facts, we can conclude that the FD MDT is advantageous when compared to prolonged treatment in MB cases until smear negativity or till resolution of clinical activity in PB cases because clearance of bacterial debris or achievement of skin smear negativity is not influenced by continuance of bactericidal drugs beyond the point of bacterial kill. However, there are certain issues related to the FD MDT in PB cases and MB cases with high initial bacterial load which remain unanswered by FD MDT.
Disadvantages of FD MDT
From a public health-care point of view, the current MDT regimen has proved to be very effective in the elimination of leprosy. However, many experienced dermatologists who are the real consultants in the clinical aspects of the disease (as they look after the individual cases), are skeptical of FD MDT and find that the ‘clinical cure’ does not occur after FD MDT in all the cases of leprosy. Clinically cured patients at the end of 12 months of MDT can still be bacteriologically active and bacteriologically negative patients can still be clinically active. Thus an overwhelming number of dermatologists give importance to clinical activity and do not follow the FDT schedules as suggested by the WHO.
The limitations of the FD MDT pertaining to MB cases are based on the following observations
It has been proved in a few studies that despite two years of regular therapy, 10% of the patients continue to harbor viable persisters. In addition, incomplete killing of M. leprae in patients treated for two years has been confirmed by the demonstration of ATP in 19% of the bacterial suspensions from skin biopsies and the presence of viable bacilli in the nerves of one-third of the patients as tested by the mouse footpad. These observations signify the persistence of viable drug-sensitive bacilli, probably the dormant bacilli that have escaped the bactericidal effect of drugs including rifampicin in a proportion of patients. The fate of these organisms is of prime importance because there is no evidence that MDT knocks down persisters and there is no drug for leprosy that is known to act on dormant organisms. Moreover, lepromatous patients with high initial BI have naturally a poor cell-mediated immunity (CMI) and poor macrophage functioning to deal with these remaining organisms. Hence, treatment cannot be stopped after one or two years, as persisters are likely to grow, resulting in relapse. But, it may take a much longer time than the incubation period of disease, because clofazimine remains in the tissues for a long duration and maintains a check on the growth of M. leprae.[25–27]
Higher rates of relapse of almost 39% have been reported in a subgroup of patients with a large bacterial load (BI ≥ 4+) treated with 24 months of standard MDT, during later years of follow-up in studies where long follow-up has been done.[28] It has been observed that higher the BI or shorter the duration of therapy, the higher the risk of relapse.[28] In a study by Girdhar, et al.,[29] the rate of relapse in patients treated with MDT till they were smear negative was 1.1 per 100 person-years, whereas patients on FD MDT showed a relapse rate of 2.04 per 100 person-years. Similarly, the Marchoux Chemotherapy Study Group observed a relapse rate of 3.4 per 100 person-years with FD MDT.[30]
It has been observed that the bacteriological relapses occurred earlier than clinical worsening and this could not be picked up in many studies with a short follow-up period as slit-skin smear is not routinely being used in the fields.[25]
There is also a difference noted in the rates of relapse based on whether they were field studies or institutional studies. This could be attributed to the following differences: Inclusion of all MB cases in the field studies in contrast to mainly LL/BL (BL: Borderline lepromatous) cases in the institutional studies and more regular as well as long-duration follow-up with periodic clinical and skin smear examination in institutional studies.[25]
The endpoint of treatment of pure neuritic leprosy is difficult to establish due to the highly controversial assessment and cure criteria. It has been shown that several patients show advanced disease and are positive for AFB on histology both in the nerves and in skin, even when one or few nerves are clinically affected. This suggests that it would be better to include these patients in the MB group and give a three-drug combination. The national program recommends that when upto one nerve trunk is thickened, the patients could be treated as PB, whereas those with a large number of affected nerves should receive MB therapy. These recommendations seem justified from the point of view of control, as in these patients bacilli are deep in the skin or nerves and are not discharged for transmission. However, what happens in the long run is not clear as all the organisms may not get killed with the limited treatment and may result in the deterioration of the nerve function. Further, despite adequate treatment, in some cases the nerve function can worsen on account of fibrosis, causing concern.[25]
The cost of treating either all or a targeted subpopulation of MB cases with MDT for a prolonged period or carefully following the same sort of patients for a decade might seem high initially, but might not be excessive. Nevertheless, this needs to be weighed against the lower costs of retreatment of the relapses with a second course of MDT, assuming that there is neither the development of drug-resistant disease nor the development of additional disability in relapse cases.[28]
The limitations associated with FD PB MDT are as follows
The cure or endpoint of treatment of PB cases (smear-negative patients) has been more difficult to define unlike in MB cases wherein the slit-skin smears are indicators of disease activity.[31]
Continued visibility of a clinically active patch in a proportion of patients at the end of six months of therapy has been observed in almost all studies varying from 10 to 67%. Studies conducted in the institutions have shown a larger proportion of patients who are still active as compared to field situations.[25]
When the length of duration of treatment is not long enough for the body to clear out the bacteria, continued inflammatory response results in persistent clinical activity for up to 12-18 months. There is a delayed resolution in a significant number of patients which sometimes may turn out to be failures of treatment. It has also been observed in a few studies that if diamino diphenyl sulphone (DDS) is continued for a further period of six months or MDT is administered for 12 months instead of the recommended six months, the proportion of patients staying active could be significantly reduced.[25]
In several reports, active granuloma has been found in over 50% of the patients on completion of therapy and even six months later, suggesting persisting disease activity.[25]
Studies at the Central JALMA Institute of Leprosy (CJLI), Agra, India have shown that a good number of patients diagnosed as PB leprosy clinically were acid-fast (AFB) bacilli positive in the skin smear, indicating their chances of getting inadequate treatment and these patients would be prone for relapse.[31]
Solutions to Overcome These Problems
The limitations of FD MDT can be overcome by adopting the following measures:
MB cases with an initial average BI ≥ 4+ should receive at least four years of standard WHO MDT as proposed by the Marchoux chemotherapy study group.[30]
Though most of the patients with high BI continue to improve after the completion of the 12-month regimen, an additional 12 months of MDT for MB leprosy may be required for patients showing evidence of deterioration.[32]
The addition of immunotherapy by the Bacillus Calmette–Guérin (BCG) or Mycobacterium welchii vaccine can help to reduce the duration of treatment by 50%.[33]
A regimen of one year with the addition of ofloxacin and minocycline at a monthly dose to the existing MDT can be carried out in an attempt to reduce the duration of therapy as per the trials conducted by the NLEP and CJLI.[34]
Rigorous annual follow-up for at least five years and even more for PB cases and 10 years and even more for MB cases after being released from FD MDT is essential.[24]
Ofloxacin and minocycline with potent bactericidal activity against M. leprae can provide an effective single-dose therapy for PB leprosy when combined with rifampicin as ROM (R: Rimfanpicin, O: Ofloxacin, M: Minocycline) regimen. For MB leprosy, 24 monthly doses (pulsed) of supervised ROM can be advocated for patients refusing or unable to take MDT. ROM is found to be as safe and effective as MDT during dosing, causing no skin pigmentation, and conferring similar clinical, bacteriologic, and histologic improvements, without increased rates of lepra reactions. However, ROM costs four times more than MDT for similar duration regimens, prohibiting mass administration, but patients treated with ROM may remain anonymous to the community and even their families.[35]
The significance of abundant AFB- and MB-type histopathology in patients grouped as PB leprosy should be resolved so that these patients could be given the drug therapy and the duration of therapy they warrant. The techniques that directly evaluate the type and severity of leprosy should be made relevant to the treatment, especially in centers where they are available.[36]
As the workload and financial burden on leprosy organizations has significantly decreased over the years with substantial decrease in the number of leprosy patients, slit-skin smears may again be made an integral part of the leprosy program.
Newer MDT Regimens
Newer regimens that are more effective and operationally less demanding are the need of the hour because of certain drawbacks with the existing MDT regimens, such as:[37–39]
The longer duration of therapy for MB leprosy is a disadvantage from the operational point of view.
Daspone and clofazimine are only weakly bactericidal against M. leprae, and as these weaker drugs determine the minimal effective duration of the current regimen, further shortening of the duration of treatment might result in higher rates of relapse.
Daily administration of dapsone and clofazimine are not directly supervised.
Side effects of the drugs in the current regimen like clofazimine-induced disoloration of skin, hypersensitivity to dapsone, rifampicin-induced hepatitis, and so on.
Emergence of resistance to dapsone and rifampicin.
The various newer MDT regimens include the following:
MB cases
-
Rifampicin-susceptible MB patient:[40]
- Fully supervisable, monthly administered regimen rifapentine 900 mg (or rifampicin 600 mg) plus moxifloxacin 400 mg plus clarithromycin 1000 mg (or minocycline 200 mg) administered once monthly under supervision for 12 months.
-
Rifampicin-resistant MB patient: Fully supervised regimen in two phases:[41]
- An initial six-month intensive phase followed by an 18-month continuation phase. The intensive phase: Moxifloxacin 400 mg—clofazimine 50 mg—clarithromycin 500 mg—minocycline 100 mg all taken daily.
- The continuation phase: Moxifloxacin 400 mg—clarithromycin 1000 mg—minocycline 200 mg all taken once monthly.
- Intensive phase: Daily administration of 50 mg clofazimine, together with two of the following drugs: 400 mg ofloxacin, 100 mg minocycline, or 500 mg clarithromycin for six months.
- Continuation phase: Daily administration of 50 mg clofazimine, together with 100 mg minocycline or 400 mg ofloxacin for an additional 18 months.
- If available, ofloxacin may be replaced by moxifloxacin 400 mg, which has stronger bactericidal activity against M. leprae.[42]
-
Fully supervisable, monthly administered regimens:
Six-week quadruple regimen: Rifampicin 600 mg plus ofloxacin 400 mg plus clofazimine 100 mg plus minocycline 100 mg once a week for six weeks.[44]
Once a month, supervised rifampicin 600 mg plus ofloxacin 400 mg plus minocycline 100 mg in addition to self-administered dapsone 100 mg plus clofazimine 50 mg daily for 12 months.[45]
Daily rifampicin 600 mg plus sparfloxacin 200 mg plus clarithromycin 500 mg plus minocycline 100 mg for 12 weeks.[46]
PB cases
Accompanied MDT
The patient is provided the entire supply of MDT drugs at the time of diagnosis, while someone close to or important to the patient assumes the responsibility of helping him or her complete a full course of treatment.[47] It is a simple but a wrong solution for implementing supervised therapy because of confused operational difficulties with technical justifications; it ignores the facts of poor adherence of leprosy patients to self-medication completely, lacks evidence-based justification, and neglects the importance of regular contacts between health-care workers and patients, which is crucial for the prevention of impairment.
Uniform MDT
Advantages
The uniform MDT (U-MDT) regimen could be effective and operationally convenient in the context of the integration of leprosy into general health-care services.[48]
Drug compliance with a shorter duration can make it an acceptable regimen for MB patients.
Clofazimine-related pigmentation of the skin is usually short lived and acceptable to PB patients.
As continued inflammatory response results in persistent activity in leprosy, addition of clofazimine can help in PB patients.
Granulomas regressed faster if clofazimine was added to the PB regimen.
Disadvantages
U-MDT will overtreat PB leprosy patients and undertreat MB patients, especially those with a high initial BI.
Conclusions
The MDT regimens for the treatment of leprosy have undergone several changes especially with regard to the duration of treatment. The advantages of a shortened duration of treatment need to be balanced against the risk of relapse. In addition, the fact that completion of MDT and removal of the details of the patient from the register may not be equivalent to the cure of leprosy should be borne in mind while treating leprosy patients. Thus, the duration of MDT required depends on the aim, resources, motivation of the individual, and his availability for follow-up. In the field setup, where the aim is to interrupt the transmission of leprosy, a fixed duration of 24 or 12 months with three-drug MDT for MB patients is likely to do the job. This is because in the fields, due to extensive screening, the patients are picked up at an early stage and hence, there are not too many patients with large bacterial load who pose a threat to relapse. Moreover, the operationally feasible six-month PB therapy will also help in reducing the active case load. Nevertheless, these patients are to be kept under regular follow-up for varying periods to look for evidence of deterioration especially MB patients with high BI or PB patients with involvement of the nerve trunk. Retreatment with MB therapy should be instituted if there is worsening or evidence of relapse, as all studies have shown that the relapses are due to drug-sensitive persisters. On the other hand, for the institutional patients, where the aim is the cure of the individual patient in addition to the interruption of transmission, an extended treatment of four years or until smear negativity is desirable for all highly bacillated patients with BI ≥ 4+. Ethical issues also need to be considered and a fine balance needs to be maintained between achieving a cure for the patient and protecting the society at risk. This would be possible only when the treatment of an individual is ensured till attainment of complete cure, at least wherever feasible.
What is new?
The duration of MDT required depends on the aim, resources, motivation of the individual, and his availability for follow-up. In the field setup, where the aim is to interrupt the transmission of leprosy, a fixed duration of 24 or 12 months with three-drug MDT for MB patients is likely to do the job. On the other hand, for the institutional patients, where the aim is the cure of the individual patient in addition to the interruption of transmission, an extended treatment of four years or until smear negativity is desirable for all highly bacillated patients with BI > 4+.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.WHO. Leprosy today. [Last assessed on 2012 Aug 05]. Available from: http://www.who.int/lep/en/
- 2.India's alarming share of global new leprosy cases. [Last assessed on 2012 Aug 05]. Available from: http://www.thehindu.com/sci-tech/science/article2995018.ece .
- 3.Desikan KV. Elimination of leprosy and possibility of eradication: The Indian scenario. Indian J Med Res. 2012;135:3–5. doi: 10.4103/0971-5916.93415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daumerie D. Implementation of MDT-Successive steps. In: Sansarricq H, editor. Multidrug therapy against leprosy: Development and implementation over the past 25 years. Geneva: WHO Library Cataloguing-in-Publication Data; 2004. pp. 45–57. [Google Scholar]
- 5.WHO Study Group. WHO Technical Report Series no. 847. Geneva: World Health Organization; 1994. Chemotherapy of leprosy. [PubMed] [Google Scholar]
- 6.Sansarricq H. The Study Group. In: Sansarricq H, editor. Multidrug therapy against leprosy: Development and implementation over the past 25 years. Geneva: WHO Library Cataloguing-in-Publication Data; 2004. pp. 45–57. [Google Scholar]
- 7.Jopling WH, McDougall AC. 5th ed. New Delhi: CBS Publishers and Distributors; 1996. Handbook of leprosy; pp. 101–17. [Google Scholar]
- 8.Hastings RC, Opromolla DVA, editors. Leprosy. 2nd ed. Edinburgh: Churchill Livingstone; 1994. Dharmendra. Classifications of leprosy; pp. 179–90. [Google Scholar]
- 9.Jacobson RR. Treatment of leprosy. In: Hastings RC, Opromolla DV, editors. Leprosy. 2nd ed. Edinburgh: Churchill Livingstone; 1994. pp. 317–49. [Google Scholar]
- 10.Rao CK. Implementation of WHO MDT in India 1982–2001. In: Sansarricq H, editor. Multidrug therapy against leprosy: Development and implementation over the past 25 years. Geneva: WHO Library Cataloguing-in-Publication Data; 2004. pp. 92–105. [Google Scholar]
- 11.Pai VV, Ganapathi R, Rao R. Development and evolution of WHO MDT and newer treatment regimens. In: Kar HK, Kumar B, editors. IAL textbook of leprosy. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2010. pp. 353–67. [Google Scholar]
- 12.Mishra RS, Kumar J. Classification. In: Kar HK, Kumar B, editors. IAL textbook of leprosy. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2010. pp. 144–51. [Google Scholar]
- 13.WHO recommended MDT regimens. [Last assessed on 2012 Aug 05]. Available from: http://www.who.int/lep/mdt/regimens/en/index.html .
- 14.Worobec SM. Treatment of leprosy/Hansen's disease in the early 21st century. Dermatol Ther. 2009;22:518–37. doi: 10.1111/j.1529-8019.2009.01274.x. [DOI] [PubMed] [Google Scholar]
- 15.MDT: Duration of treatment FAQ. [Last assessed on 2012 Aug 05]. Available from: http://www.who.int/lep/mdt/duration/en/inde×2.html .
- 16.Ji B. Why multidrug therapy for multibacillary leprosy can be shortened to 12 months. Lepr Rev. 1998;69:106–9. doi: 10.5935/0305-7518.19980009. [DOI] [PubMed] [Google Scholar]
- 17.Shaw IN, Christian M, Jesudasan K, Kurian N, Rao GS. Effectiveness of multidrug therapy in multibacillary leprosy: A long-term follow-up of 34 multibacillary leprosy patients treated with multidrug regimens till skin smear negativity. Lepr Rev. 2003;74:141–7. [PubMed] [Google Scholar]
- 18.Girdhar BK, Girdhar A, Kumar A. Relapses in multibacillary leprosy patients: Effect of length of therapy. Lepr Rev. 2000;71:144–53. doi: 10.5935/0305-7518.20000017. [DOI] [PubMed] [Google Scholar]
- 19.Pönnighaus JM, Boerrigter G. Are 18 doses of WHO/MDT sufficient for multibacillary leprosy; results of a trial in Malawi. Int J Lepr Other Mycobact Dis. 1995;63:1–7. [PubMed] [Google Scholar]
- 20.Sales AM, Sabroza PC, Nery JA, Dupprè NC, Sarno EN. No difference in leprosy treatment outcomes comparing 12- and 24-dose multidrug regimens: A preliminary study. Cad Saude Publica. 2007;23:815–22. doi: 10.1590/s0102-311x2007000400009. [DOI] [PubMed] [Google Scholar]
- 21.Shetty VP, Wakade AV, Ghate SD, Pai VV, Ganapati RR, Antia NH. Clinical, histopathological and bacteriological study of 52 referral MB cases relapsing after MDT. Lepr Rev. 2005;76:241–52. [PubMed] [Google Scholar]
- 22.Pattyn SR, Bourland J, Grillone S, Groenen G, Ghys P. Combined regimens of one year duration in the treatment of multibacillary leprosy–Combined regimens with rifampicin administered during one year. Lepr Rev. 1989;60:109–17. [PubMed] [Google Scholar]
- 23.Pattyn SR. Efficacy of different regimens in multibacillary leprosy. Lepr Rev. 1986;57:265–71. doi: 10.5935/0305-7518.19860116. [DOI] [PubMed] [Google Scholar]
- 24.Pai VV. Chemotherapy of leprosy-further challenges. [Last assessed on 2012 Aug 05]. Available from: http://medind.nic.in/haa/t06/i2/haat06i2p72.pdf .
- 25.Girdhar BK, Girdhar A. Short course treatment of leprosy: Present status. [Last assessed on 2012 Aug 05]. Available from: http://icmr.nic.in/bufeb02.pdf .
- 26.Anonymous Persisting Mycobacterium leprae among THELEP trial patients in Bamako and Chingleput. Subcommittee on Clinical Trials of the Chemotherapy of Leprosy (THELEP) Scientific Working Group of the UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases. Lepr Rev. 1987;58:325–37. [PubMed] [Google Scholar]
- 27.Sharma A, Sharma VK, Rajwanshi A, Das A, Kaur I, Kumar B. Presence of M.leprae in tissues in slit skin smear negative multibacillary (MB) patients after WHO-MBR. Lepr Rev. 1999;70:281–6. doi: 10.5935/0305-7518.19990031. [DOI] [PubMed] [Google Scholar]
- 28.Lemaster JW, Shwe T, Butlin CR, Roche PW. Prediction of ‘highly skin smear positive’ cases among MB leprosy patients using clinical parameters. Lepr Rev. 2001;72:23–8. doi: 10.5935/0305-7518.20010005. [DOI] [PubMed] [Google Scholar]
- 29.Girdhar BK, Girdhar A, Kumar A. Relapses in multibacillary leprosy patients: Effect of length of therapy. Lepr Rev. 2000;71:144–53. doi: 10.5935/0305-7518.20000017. [DOI] [PubMed] [Google Scholar]
- 30.Jamet P, Ji B. Relapse after long-term follow up of multibacillary patients treated by WHO multidrug regimen. Marchoux Chemotherapy Study Group. Int J Lepr Other Mycobact Dis. 1995;63:195–201. [PubMed] [Google Scholar]
- 31.Prasad PV, Babu A, Kaviarasan PK, Viswanathan P, Tippoo R. MDT-MB therapy in paucibacillary leprosy: A clinicopathological assessment. Indian J Dermatol Venereol Leprol. 2005;71:242–5. doi: 10.4103/0378-6323.16614. [DOI] [PubMed] [Google Scholar]
- 32.Leprosy elimination: MDT: Duration of treatment FAQ. [Last assessed on 2012 Aug 05]. Available from: http://www.who.int/lep/mdt/duration/en/inde×1.html .
- 33.Sehgal VN, Sardana K. Immunoprophylaxis of leprosy: Current status and future prospects. Indian J Dermatol Venereol Leprol. 2007;73:71–2. doi: 10.4103/0378-6323.31888. [DOI] [PubMed] [Google Scholar]
- 34.Katoch K, Katoch VM, Natarajan M, Gupta UD, Sharma VD, Singh HB. Long term follow-up results of 1 year MDT in MB leprosy patients treated with standard MDT+once a month Minocycline and Ofloxacin. Indian J Lepr. 2008;80:331–44. [PubMed] [Google Scholar]
- 35.Villahermosa LG, Fajardo TT, Jr, Abalos RM, Cellona RV, Balagon MV, Dela Cruz EC, et al. Parallel assessment of 24 monthly doses of rifampin, ofloxacin, and minocycline versus two years of World Health Organization multi-drug therapy for multi-bacillary leprosy. Am J Trop Med Hyg. 2004;70:197–200. [PubMed] [Google Scholar]
- 36.Rao PN, Pratap D, Ramana Reddy AV, Sujai S. Evaluation of leprosy patients with 1 to 5 skin lesions with relevance to their grouping into paucibacillary or multibacillary disease. Indian J Dermatol Venereol Leprol. 2006;72:207–10. doi: 10.4103/0378-6323.25781. [DOI] [PubMed] [Google Scholar]
- 37.Prasad P, Kaviarasan PK. Leprosy therapy, past and present: Can we hope to eliminate it? Indian J Dermatol. 2010;55:316–24. doi: 10.4103/0019-5154.74528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bandit C. Recent Advances in Leprosy Chemotherapy. J Trop Med Parasitol. 2006;29:68–76. [Google Scholar]
- 39.Ji B. Chemotherapy and chemoprophylaxis of leprosy. [Last assessed on 2012 Aug 05]. Available from: http://www.tropika.net/review/020226-Leprosy_Chemotherapy/article.pdf .
- 40.Ji B, Grosset J. Combination of rifapentine-moxifloxacin-minocycline (PMM) for the treatment of leprosy. Lepr Rev. 2000;71:S81–7. doi: 10.5935/0305-7518.20000074. [DOI] [PubMed] [Google Scholar]
- 41.Report of the ninth meeting of the WHO technical advisory group on leprosy control. World Health Organization, Regional Office for South-East Asia. 2008 [Google Scholar]
- 42.WHO Expert Committee on Leprosy. WHO Technical Report Series 968. 2012 [PubMed] [Google Scholar]
- 43.LEPROSY–NEW DRUG REGIMENS. [Last accessed on 2012 Aug 05]. Available from: http://www.who.int/tdr/research/progress/9900/methods_treatment/en/inde×5.html .
- 44.Pattyn S, Grillone S. Relapse rates and a 10-year follow-up of a 6-week quadruple drug regimen for multibacillary leprosy. Lepr Rev. 2002;73:245–7. [PubMed] [Google Scholar]
- 45.Katoch K, Katoch VM, Natrajan M, Sharma VD, Singh HB, Gupta UD. Chemotherapy trials in MB leprosy using conventional and newer drugs pefloxacin and minocycline. Indian J Dermatol Venereol Leprol. 2000;66:18–25. [PubMed] [Google Scholar]
- 46.Tejasvi T, Khaitan BK, Khanna N, Pandhi RK, Singh MK. Evaluation of a new fixed duration (12 weeks) multi-drug regimen of bactericidal drugs in multibacillary leprosy. Indian J Lepr. 2006;78:329–37. [PubMed] [Google Scholar]
- 47.Ji B. Accompanied MDT (AMDT)-more questions than answers. Lepr Rev. 2002;73:301–7. [PubMed] [Google Scholar]
- 48.Ji B, Saunderson P. Uniform MDT (U-MDT) regimen for all leprosy patients-another example of wishful thinking. Lepr Rev. 2003;74:2–6. [PubMed] [Google Scholar]


