Abstract
To understand sexual decision-making processes among people living with HIV, we compared safer sex self-efficacy, condom attitudes, sexual beliefs, and rates of unprotected anal or vaginal intercourse with at-risk partners (UAVI-AR) in the past 3 months among 476 people living with HIV: 185 men who have sex with men (MSM), 130 heterosexual men, and 161 heterosexual women. Participants were enrolled in SafeTalk, a randomized, controlled trial of a safer sex intervention. We found 15% of MSM, 9% of heterosexual men, and 12% of heterosexual women engaged in UAVI-AR. Groups did not differ in self-efficacy or sexual attitudes/beliefs. However, the associations between these variables and UAVI-AR varied within groups: greater self-efficacy predicted less UAVI-AR for MSM and women, whereas more positive condom attitudes – but not self-efficacy – predicted less UAVI-AR for heterosexual men. These results suggest HIV prevention programs should tailor materials to different subgroups.
Keywords: HIV transmission risk behavior, self-efficacy, safer sex attitudes, condom attitudes, sexual behavior
INTRODUCTION
Understanding sexual behavior and sexual decision-making processes among people living with HIV is critical for preventing the spread of HIV. Nearly one third of people living with HIV continue to engage in unprotected anal or vaginal sex, often with partners of negative or unknown serostatus [1-4]. Such unsafe sexual practices contribute to the 56,000 new HIV infections each year in the United States [5]. This high incidence suggests a critical need for new strategies that help individuals reduce their transmission risk behaviors.
The relationships between sexual attitudes, beliefs, and risky sexual behavior among people living with HIV are not yet fully understood. In particular, little is known about differences that may exist among subgroups of HIV positive individuals, including men who have sex with men (MSM), heterosexual men, and heterosexual women. Yet understanding subgroup differences in the sexual attitudes and beliefs that predict safer sexual behavior, such as self-efficacy, attitudes about condoms, and sexual beliefs about transmission risk, is of critical importance as this understanding could allow for more targeted and efficacious HIV prevention programming. It is surprising that so little is known about subgroup differences among people living with HIV given the differences in sexual attitudes and behaviors that have been noted in non-HIV positive populations [6-8]. The paucity of research in this area is also surprising considering that so many interventions are specifically targeted to individual subgroups [9-11].
The few existing studies that have directly compared MSM, heterosexual men, and women on risky sexual behavior and psychosocial predictors of such behavior have focused on factors such as demographic and clinical characteristics, substance use, and self-efficacy [3, 4, 12]. These studies have provided evidence to suggest there may be important differences among groups that warrant further exploration. For example, women and MSM consistently report more acts of unprotected anal or vaginal intercourse with at-risk partners (UAVI-AR) than heterosexual men [3, 4, 12]. However, subgroup differences in the predictors of UAVI-AR have been more inconsistent across these studies. Specifically, among men, one study found that higher safer sex self-efficacy predicted less risky sex for both MSM and heterosexual men [4], whereas another study found self-efficacy predicted less risky sex for MSM but not heterosexual men [3]. Further, no variables were found to reliably predict risky sex for HIV-positive women across the studies that specifically analyzed subgroup differences [3, 4].
Taken together, these findings highlight potential differences in risky sexual behavior and the predictors of this behavior when gender and sexual orientation are considered. However, findings from these studies are not conclusive, as the association between self-efficacy and risky sex varied between studies. Moreover, several sexual attitudes and beliefs that may be important predictors of condom use, such as attitudes towards condoms [13] and perceived likelihood of infecting others [14], were not examined. Given these inconsistencies and the relative scarcity of research on subgroup differences, there remain important gaps in our understanding of sexual decision-making processes among people living with HIV.
The purpose of this study was to describe and compare rates of unprotected intercourse and safer sex self-efficacy, condom attitudes, and sexual beliefs among MSM, heterosexual men, and women living with HIV. Further, we sought to understand which sexual attitudes and beliefs were most predictive of risky sexual behavior within subgroups. Exploring the relationships between self-efficacy, sexual attitudes/beliefs, and behavior across groups is timely and important, as these variables are theoretically and empirically linked to risky sex [13, 15] and are amenable to change [17, 18], thus making them ideal targets for prevention programs. We had three specific research questions that guided the current project: 1) Do self-efficacy to practice safer sex, attitudes toward condoms, and transmission risk beliefs differ between MSM, heterosexual men, and heterosexual women living with HIV? 2) Among these same groups, are there differences in HIV transmission risk behavior? 3) Does the strength of the relationships between HIV transmission risk behavior and safer sex self-efficacy, condom attitudes, and sexual beliefs vary between subgroups?
METHODS
Study Design and Participants
Data for the current cross-sectional project come from the baseline evaluation of SafeTalk, a two-armed randomized, controlled trial of a safer sex intervention among HIV-infected individuals [18, 19]. Participants were recruited from three clinics in North Carolina that primarily treated patients living with HIV. To be eligible, participants had to be: (1) at least 18 years old; (2) HIV-infected; (3) receiving HIV treatment at one of the three study sites; (4) English-speaking; (5) of sufficient cognitive ability to provide consent and complete intervention counseling; and (6) self-reported having oral, anal, or vaginal sex in the last 12 months. Individuals were excluded if it was their first visit to the clinic, they were deemed too sick to participate by themselves or their providers, they would not be attending the clinic for the duration of study enrollment, or they had participated in a separate safer sex program within the last six months. The University of North Carolina at Chapel Hill’s Office for the Protection of Human Research Subjects approved all study procedures.
Procedure
Participants completed an audio computer assisted self-interview (ACASI)-administered survey (Nova Research Co) during their baseline study visit. Participants used headphones and entered their responses directly into the computer. The ACASI approach has been shown to increase privacy, reduce social desirability bias, and enhance the validity of responses to sensitive questions about HIV risk behavior [20, 21]. We attempted to increase the accuracy of data in several additional ways. First, participant confidentiality was stressed throughout the study. Additionally, we programmed the ACASI to verify participants’ answers on the sexual behavior questions (e.g., when they entered n sex partners, the ACASI said, “You entered n. Is this correct?” If they selected “no”, they were asked to re-enter the number). Finally, we programmed the ACASI to conduct logic checks of the numbers of sex partners and sex acts (e.g., if someone said they had 10 total sex acts and 11 “condom-protected” sex acts, they were asked to re-enter the information). The baseline survey lasted 30-60 minutes and assessed participants’ demographic and clinical characteristics, psychosocial factors, attitudes, risky sexual behavior, and the characteristics of their sexual relationships. Participants received a $25.00 gift card to a local grocery store for the baseline visit, as well as vouchers for parking, bus, and meals when needed.
Measures
Demographic and Clinical Factors
We assessed participants’ gender, sexual orientation, age, race/ethnicity, employment status, current relationship status, and clinical characteristics related to HIV (e.g., time since diagnosis, viral load). We assessed binge drinking and crack/cocaine use as indicators of substance abuse. Specifically, we asked how frequently participants engaged in binge drinking (≥ 5 drinks in a single day for men, ≥ 4 drinks for women), which we dichotomized as any or no binge drinking. We also categorized each participant as having used or not used crack/cocaine in the prior 3 months. Finally, we determined participants’ sexual behavior subgroups (MSM, heterosexual men, or heterosexual women) from their gender and the gender of their reported sexual partners. Participants who did not report any sex partners in the past three months were categorized based on their self-reported sexual orientation.
Safer Sex Self-Efficacy
We assessed safer sex self-efficacy with a 15-item self-efficacy scale adapted from self-efficacy scales by Grimley et al. [22] and Parsons et al. [23]. This scale measured participants’ current confidence in using condoms consistently in a variety of situations with different partners. Example items include, “How confident are you that you can use condoms when you’ve been drinking or using drugs before sex?” and “How confident are you that you can use condoms with a new partner?” Items were rated on an 11-point scale, with anchors at 0 (not at all confident), 5 (somewhat confident), and 10 (completely confident). We computed a mean score such that higher scores indicated greater safer sex self-efficacy (Cronbach’s α = 0.91).
Attitudes towards Condoms
Attitudes towards condoms were assessed with a 5-item scale adapted from a study by Thomas et al. [24] that captured the extent to which participants generally believed condoms felt uncomfortable, were embarrassing, and took the fun out of sex. Participants indicated their agreement on a 4-point scale: 1 = Agree a lot, 2 = Agree a little, 3 = Disagree a little, and 4 = Disagree a lot. We computed a mean scale score such that higher scores indicated more positive condom attitudes (Cronbach’s α = 0.75).
Perceived Effectiveness of Condoms in Preventing HIV Transmission
Participants indicated the degree to which they believed using condoms was an effective way to prevent them from giving HIV to someone else on a 5-point scale: 1 = Not at all an effective way to keep you from giving HIV to someone else, 2 = Not a very effective way to keep you from giving HIV to someone else, 3 = A somewhat effective way to keep you from giving HIV to someone else, 4 = A very effective way to keep you from giving HIV to someone else, and 5 = A completely effective way to keep you from giving HIV to someone else. Higher scores indicated a stronger belief that condoms were effective in preventing HIV transmission.
Perceived Risk of Transmission
The perceived risk of transmitting HIV to others was assessed with an item that read, “Imagine you had unprotected sex one time today with an HIV negative partner. What’s the chance that you would give HIV to that partner given your current viral load?” [25]. Responses were reported on a 4-point scale: 1 = No chance, 2 = Low chance, 3 = Medium chance, and 4 = High chance. Higher responses indicated greater perceived concern that HIV transmission was likely during one act of unprotected sex.
Perceived Ability to Use Condoms Correctly
Participants indicated how confident they were that they could use condoms correctly on a scale from 0-10, where 0 = not at all confident, 5 = somewhat confident, and 10 = completely confident that they could use condoms correctly.
Risky Sexual Behaviors
To assess risky sexual behavior, the ACASI gathered detailed information about sexual behavior over the past three months. Separate versions were used for men and women, which allowed the questions to be consistent with the participant’s gender and the reported gender(s) of their sex partners. Participants were asked whether they had HIV-positive, HIV-negative, and HIV serostatus unknown partner types and how many times they had insertive or receptive vaginal or anal intercourse with each partner type in the last three months. For each type of partner and type of sex act, participants were also asked how many times they had used a condom (defined as using a condom from the beginning to the end of penetration). We used the sexual behavior data to calculate four variables: 1) the total number of sexual partners in the past three months, which included partners of any HIV status with whom the participant had oral, vaginal, or anal sex, whether or not a condom was used; 2) the total number of acts of anal or vaginal intercourse with partner(s) of any serostatus in the past three months, whether or not a condom was used1; 3) a dichotomous variable indicating whether or not a participant had unprotected anal or vaginal intercourse (UAVI) with partner(s) of any serostatus in the past three months, and finally 4) a dichotomous variable indicating whether or not a participant had unprotected anal or vaginal intercourse with any at-risk (HIV serostatus negative or unknown) partner(s) (UAVI-AR) in the past three months.
Statistical Analyses
We conducted descriptive analyses of participant demographic and sexual behavior variables to characterize the sample and determine the percentage of participants who engaged in sexual risk behaviors. Then we conducted five sets of analyses to address our research questions. First, we conducted between-group comparisons on each demographic and clinical variable to determine which variables differed significantly different between groups and should be included as control variables in multivariate analyses. This was accomplished through One-Way ANOVA tests with Bonferroni-adjusted post-hoc group comparisons for the two continuous variables (age and duration of HIV) and Chi Square tests with Bonferroni-adjusted post-hoc group comparisons for the remaining seven dichotomous variables: race (black vs. white/other), education (more that high school vs. high school or less), employment (working vs. not working), marital status (married/committed relationship vs. single/no committed relationship), binge drinking (any vs. none), cocaine use (any vs. none), viral load (undetectable vs. detectable/unknown).
Second, to examine if self-efficacy, condom attitudes, and sexual beliefs varied between MSM, heterosexual men, and women, a series of ANOVA and Chi Square tests were conducted with post-hoc Bonferroni tests to compare mean differences in attitudes between groups. Third, we used logistic regression analyses to determine if the odds of engaging in UAVI and UAVI-AR varied between MSM, heterosexual men, and women. Next, to examine the strength of the relationships between UAVI-AR and self-efficacy, condom attitudes, and sexual beliefs, we conducted multivariate logistic regression analyses for the total sample and then separately for MSM, heterosexual men, and women. These analyses allowed us to determine if the pattern of attitude-behavior relationships differed within subgroups. Finally, we conducted analyses to test for interaction effects among the three subgroups in the relationship between sexual attitudes/beliefs and UAVI-AR. Specifically, we created interaction terms (subgroup x sexual attitude/belief variable) and entered these interaction terms in the final multivariate model. We included the seven demographic and clinical variables as control variables in all multivariate models (i.e., age, race, education, employment, marital status, binge drinking, and viral load). All analyses were conducted using SPSS version 19 [26].
RESULTS
Participant Characteristics
Participants were 490 adults living with HIV who completed the baseline assessment of SafeTalk, a randomized, controlled trial of a safer sex intervention [18, 19]. We screened 902 patients attending one of three clinics between July 2006 and July 2008 and identified 656 who were eligible for participation; 492 of these patients enrolled and 2 people withdrew prior to the first data collection session, resulting in a response rate of 75%. Participants in the trial were followed for approximately 12 months after enrollment. We excluded 14 participants for the current analysis: 7 women who had sex exclusively with women and 7 participants who did not report their sexual orientation and had no sexual partners in the past 3 months (2 men, 4 women, 1 transgender person). Thus, the final sample included 476 participants: 185 MSM2 (39%), 130 heterosexual men (27%), and 161 heterosexual women (34%).
Participants ranged in age from 18-70, with a mean of 42.7 years (SD = 9.1). The average length of time since HIV diagnosis was 9.5 years (SD = 6.1). Participants were primarily African-American (70.8%), and only one third of the sample was employed. See Table 1 for further descriptive information about the sample. As indicated in Table 1, we found six demographic factors differed between groups: age (F = 14.8, p < 0.01), race (χ2 = 19.1, p < 0.01), education (χ2 = 80.0, p < 0.01), employment (χ2 = 9.8, p < 0.01), marital status (χ2 = 6.6, p < 0.05), and binge drinking (χ2 = 19.4, p < 0.01). These were included as control variables in all multivariate models. Additionally, we included viral load as a control variable in analyses since current viral load may influence participant’s transmission risk beliefs.
Table 1.
Participant Descriptive Characteristics
|
Full Sample N = 476 N (%) |
MSM N = 185 N (%) |
Heterosexual Men N = 130 N (%) |
Heterosexual Women N = 161 N (%) |
Test of Group Differences ANOVA or Chi Square |
|
|---|---|---|---|---|---|
| Demographics | |||||
| Age [M (SD)] | 42.7 (9.1) | 40.3 (9.5) a | 45.8 (8.4) b | 42.9 (8.2) c | F = 14.8** |
| Race | |||||
| Black/African-American | 337 (70.8) | 110 (59.5) a | 104 (80.0) b | 123 (76.4) b | χ2 = 19.1** |
| White/Caucasian | 98 (20.6) | 60 (32.4) | 13 (10.0) | 25 (15.5) | |
| Other | 39 (8.2) | 14 (7.6) | 13 (10.0) | 12 (7.5) | |
| Education | |||||
| Some College or More | 201 (42.2) | 124 (67.0) a | 26 (20.0) b | 51 (32.3) b | χ2 = 80.0** |
| High School or Less | 274 (57.6) | 61 (33.0) | 104 (80.0) | 109 (67.7) | |
| Employment | |||||
| Full or Part-Time | 163 (34.2) | 79 (42.7) a | 36 (27.7) b | 48 (29.8) b | χ2 = 9.8** |
| Not Employed | 313 (65.8) | 106 (57.3) | 94 (72.3) | 113 (70.2) | |
| Marital Status | |||||
| Married/Committed | 155 (32.5) | 51 (27.5) a | 40 (30.8) | 64 (39.8) b | χ2 = 6.6* |
| Single | 235 (49.4) | 112 (60.5) | 60 (46.2) | 63 (39.1) | |
| Divorced/Separated/Other | 50 (11.6) | 9 (4.9) | 25 (9.2) | 21 (13.1) | |
| Binge Drinking | 189 (39.7) | 87 (47.0) a | 61 (46.9) a | 41 (25.5) b | χ2 = 19.4** |
| Cocaine Use | 86 (18.1) | 29 (15.7) | 28 (21.5) | 29 (18.0) | χ2 = 2.2 |
| Clinical Characteristics | |||||
| Undetectable Viral Load | 245 (51.5) | 90 (48.6) | 74 (56.9) | 81 (50.3) | χ2 = 2.5 |
| Yrs since Diagnosis [M (SD)] | 9.5 (6.1) | 9.5 (6.2) | 10.2 (6.3) | 9.3 (5.5) | F = 1.1 |
Note. MSM= men who have sex with men. ANOVAs were used to test group differences on continuous variables; Chi Square tests were used to test group differences in dichotomous variables. Different superscripts within a row
indicate significant differences (p < . 05) between groups with Bonferroni-adjusted post-hoc tests.
indicate significant differences (p < . 05) between groups with Bonferroni-adjusted post-hoc tests.
indicate significant differences (p < . 05) between groups with Bonferroni-adjusted post-hoc tests.
p < 0.05,
p < 0.01.
Sexual Self-efficacy, Attitudes, and Beliefs
Sexual attitude and belief scores were similar across groups (see Table 2 for mean scores and group comparisons). Specifically, MSM, heterosexual men, and women did not differ regarding their self-efficacy, belief in condom effectiveness, perceived ability to use condoms correctly, or transmission risk beliefs (p > 0.20). A trend toward significant differences was observed in condom attitudes [F = 2.47, p = 0.09], with MSM having slightly less positive attitudes towards condoms than women (mean difference = −0.18, p = 0.09), but no differences were found between heterosexual men and either of the other two groups. Additionally, we found small to moderate correlations between self-efficacy, attitudes, and beliefs within the full sample (rs = 0.03 to 0.42). The strongest correlation was between self-efficacy and perceived ability to use condoms correctly (r = 0.42, p < 0.01).
Table 2.
Descriptive and Comparative Statistics for Sexual Attitudes and Behaviors
|
Full Sample M (SD) |
MSM M (SD) |
Heterosexual Men M (SD) |
Heterosexual Women M (SD) |
Test of Group Differences ANOVA or Chi Square |
|
|---|---|---|---|---|---|
| Sexual Attitudes | |||||
| Safer Sex Self-Efficacy | |||||
| Possible Scale Scores Ranged from 0-10 | 8.4 (2.0) | 8.2 (2.2) | 8.5 (1.8) | 8.6 (2.0) | F = 0.3 |
| Attitudes about Condoms | |||||
| Possible Scale Scores Ranged from 0-4 | 3.0 (0.8) | 2.9 (0.7) | 2.9 (0.8) | 3.1 (0.8) | F = 2.5+ |
| Perceived Condom Effectiveness | |||||
| Not at All / Not Very / Somewhat Effective n (%) | 147 (30.9) | 60 (32.4) | 42 (32.3) | 46 (28.0) | χ2 = 0.98 |
| Very / Completely Effective n (%) | 329 (69.1) | 125 (67.6) | 88 (67.7) | 116 (72.0) | |
| Perceived Risk of Transmission | |||||
| No Chance / Low Chance n (%) | 155 (32.6) | 66 (35.7) | 33 (25.4) | 56 (34.8) | χ2 = 4.31 |
| Medium Chance / High Chance n (%) | 313 (65.8) | 116 (62.7) | 95 (73.1) | 102 (63.4) | |
| Perceived Ability to Correctly Use Condoms | |||||
| Possible Item Scores Ranged from 0-10 | 9.3 (1.7) | 9.4 (1.5) | 9.3 (1.7) | 9.2 (1.9) | F = 1.6 |
| Frequency of Sexual Behavior in Past 3 Months | |||||
| Number of Sex Partners | 1.4 (1.8) | 2.0 (2.5) a | 1.2 (1.3) b | 0.9 (0.6) b | F = 19.0*** |
| Number of Acts of Intercourse | 7.0 (15.6) | 7.9 (17.7) | 4.6 (8.6) | 8.0 (17.3) | F = 2.2 |
Note. MSM= men who have sex with men. ANOVAs were used to test group differences on continuous variables; Chi Square tests were used to test group differences in dichotomous variables. Different superscripts within a row
indicate significant differences (p < . 05) between groups with Bonferroni-adjusted post-hoc tests.
indicate significant differences (p < . 05) between groups with Bonferroni-adjusted post-hoc tests.
indicate significant differences (p < . 05) between groups with Bonferroni-adjusted post-hoc tests.
p < 0.10,
p <.001.
General Sexual Behavior Patterns and Frequency of Risky Sexual Behavior
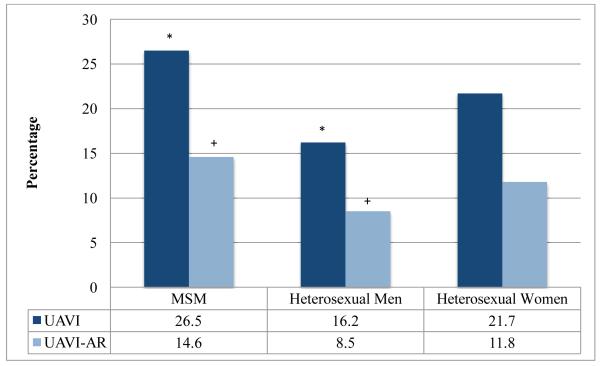
Overall, 55% of MSM, 50% of heterosexual men, and 52% of women reported engaging in anal or vaginal intercourse in the past three months. The mean number of sexual partners and the mean number of acts of intercourse over the past three months are shown in the bottom part of Table 2. When unprotected intercourse was examined in the full sample, we found 22% of participants engaged in UAVI and 12% engaged in UAVI-AR. Figure 1 shows the percentage of MSM, heterosexual men, and women engaging in UAVI and UAVI-AR. As indicated in the figure, MSM were significantly more likely than heterosexual men to engage in UAVI [Unadjusted OR = 1.91, 95% CI (1.08, 3.38), p = 0.03], and MSM were slightly more likely than heterosexual men to engage in UAVI-AR [Unadjusted OR = 1.88, 95% CI (0.90, 3.95), p = 0.09]. Rates of UAVI and UAVI-AR for women did not differ significantly from MSM or heterosexual men.
Figure 1.
Percentage of Participants Engaging in Unprotected Sex
Note. MSM = men who have sex with men. UAVI = unprotected anal or vaginal intercourse with any partner. UAVI-AR = unprotected anal or vaginal intercourse with an at-risk partner who was HIV serostatus negative or unknown (primary outcome variable). Sexual behavior was reported over the past three months. +p < .10, *p < .05.
Examining the Relationship between Sexual Attitudes and Transmission Risk Behavior
As shown in Table 3, within the full sample, safer sex self-efficacy emerged as a significant independent predictor of UAVI-AR [Adjusted OR = 0.65, 95% CI (0.54, 0.78), p < 0.001], such that participants with higher safer sex self-efficacy were less likely to engage in UAVI-AR than participants with lower self-efficacy. However, a slightly different pattern emerged when we examined each subgroup individually. Specifically, greater safer sex self-efficacy was predictive of less UAVI-AR for MSM [Adjusted OR = 0.67, 95% CI (0.52, 0.89), p < 0.001] and women [Adjusted OR = 0.49, 95% CI (0.33, 0.72), p < 0.001], whereas more positive condom attitudes, but not self-efficacy, were predictive of less UAVI-AR for heterosexual men [Adjusted OR = 0.21, 95% CI (0.06, 0.76), p < 0.05]. No other sexual beliefs emerged as significant unique predictors of transmission risk behavior when the effects of self-efficacy and attitudes towards condoms were controlled.
Table 3.
Multivariate Logistic Regression Analyses with Sexual Attitudes Predicting UAVI-AR Within Groups
| Full Sample | MSM | Heterosexual Men | Heterosexual Women | |||||
|---|---|---|---|---|---|---|---|---|
| Adjusted OR |
(95% CI) | Adjusted OR |
(95% CI) | Adjusted OR |
(95% CI) | Adjusted OR |
(95% CI) | |
| Predictors | ||||||||
| Safer Sex Self-Efficacy | 0.66*** | (0.56, 0.79) | 0.67** | (0.52, 0.89) | 0.99 | (0.56, 1.74) | 0.49*** | (0.33, 0.72) |
| Positive Condom Attitudes | 0.69 | (0.44, 1.09) | 0.76 | (0.33, 1.74) | 0.21* | (0.06, 0.76) | 0.63 | (0.8, 1.41) |
| Perceive Condoms as Very/Completely Effective |
0.78 | (0.41, 1.50) | 1.09 | (0.39, 3.08) | 0.78 | (0.16, 3.74) | 0.42 | (0.11, 1.56) |
| Perceive Medium/High Risk of HIV Transmission |
1.00 | (0.51, 1.94) | 1.26 | (0.45, 3.52) | 0.42 | (0.09, 1.91) | 1.16 | (0.32, 4.22) |
| Perceive Higher Ability to Correctly Use Condoms |
1.17 | (0.97, 1.42) | 1.23 | (0.88, 1.72) | 1.01 | (0.60, 1.69) | 1.25 | (0.89, 1.76) |
| Control Variables | ||||||||
| Age | 0.94** | (0.91, 0.98) | 0.96 | (0.90, 1.02) | 0.91+ | (0.83, 1.00) | 0.92* | (0.85, 1.00) |
| Black Race | 1.49 | (0.71, 3.10) | 1.33 | (0.45, 3.90) | 0.90 | (0.19, 4.24) | 2.56 | (0.45, 14.45) |
| Post High School Education | 1.18 | (0.60, 2.33) | 0.70 | (0.25, 2.01) | 3.94 | (0.52, 29.79) | 3.08 | (0.70, 13.50) |
| Employed Full or Part Time | 1.17 | (0.60, 2.30) | 1.66 | (0.61, 4.51) | 0.71 | (0.12, 4.28) | 0.98 | (0.23, 4.24) |
| Married/Committed Relationship | 1.73+ | (0.91, 3.29) | 1.20 | (0.42, 3.39) | 3.93+ | (0.77, 20.02) | 2.23 | (0.64, 7.81) |
| Binge Drinking | 0.96 | (0.51, 1.81) | 0.59 | (0.22, 1.60) | 1.86 | (0.43, 8.09) | 3.00 | (0.80, 7.81) |
| Undetectable Viral Load | 0.60 | (0.31, 1.14) | 0.73 | (0.27, 1.97) | 0.58 | (0.13, 2.61) | 0.49 | (0.13, 1.87) |
Note: UAVI-AR= unprotected anal or vaginal intercourse with an at-risk partner who was HIV serostatus negative or unknown. MSM = men who have sex with men. Final n for full sample in multivariate model = 439 (172 MSM, 122 heterosexual men, 145 heterosexual women).
p < .10,
p < .05,
p < .01,
p < .001.
We conducted follow-up interaction analyses to test if the strength of the associations between UAVI-AR and safer sex self-efficacy, condom attitudes, and transmission risk beliefs varied significantly among groups. None of these interactions were significant.
DISCUSSION
Similar to past research [1, 3, 4, 12], we found that almost a quarter of the individuals living with HIV in our study engaged in at least one act of unprotected intercourse with a partner of any serostatus in the past three months, and 12% had unprotected intercourse with partner who was of HIV negative or unknown serostatus. In an effort to inform programs that seek to reduce the risky sexual practices of people living with HIV, we sought to shed light on an understudied area: the role that self-efficacy, condom attitudes, and sexual beliefs play in the sexual practices of people living with HIV. We were particularly interested in examining if these relationships differed between men who have sex with men (MSM), heterosexual men, and heterosexual women.
This was the first study we were aware of that directly compared multiple safer sex related sexual attitudes and beliefs between MSM, heterosexual men, and women in a sample of people living with HIV. Prior research conducted primarily in non HIV-positive samples has produced mixed results when the self-efficacy and sexual attitudes of men and women are compared. For example, some studies have found that women have more positive attitudes toward condoms than men [23, 27] and higher self-efficacy to use condoms [23], whereas other studies have not found significant differences in sexual attitudes between men and women [28, 29]. In the present research, we did not find significant differences across subgroups; instead, all groups reported very similar scores on the self-efficacy, sexual attitude, and belief measures.
Although subgroups in this study did not differ in their average levels of self-efficacy, sexual attitudes, and beliefs, we did find that the association between these factors and transmission risk behavior varied within groups. Specifically, when controlling for self-efficacy and safer sex beliefs, condom attitudes were unrelated to risky sexual behavior for MSM and women, but condom attitudes emerged as an important predictor of safer sex behavior for heterosexual men living with HIV. Among heterosexual men, those with less favorable attitudes toward condoms were more likely to engage in unprotected sex with at-risk partners. This suggests that directly targeting condom attitudes, particularly for heterosexual men, may be a more effective way of decreasing HIV risk behavior than targeting sexual beliefs that are more often the focus of HIV prevention messages, such as belief in condom effectiveness or belief in the risk of transmitting HIV to others [15, 30]. One way to increase positive attitudes towards condoms may be to increase the perception of sexual pleasure associated with condom use through eroticizing safer sex behavior for heterosexual men [17]. This could be explored in future prevention with positives programming.
We were not surprised to find that positive attitudes toward condoms were a predictor of safer sexual behavior for heterosexual men, as this finding is in line with both behavioral theory [31] and a large body of empirical research [13]. However, we were surprised to find that attitudes toward condoms were not an independent predictor of condom use for MSM or women after self-efficacy and other sexual attitudes were controlled. We wondered if this difference could be attributed to the type of sex that MSM engage in (i.e., insertive versus receptive anal sex), as it is possible that condom use may have a larger impact on the sexual pleasure of intercourse for MSM who are exclusively or primarily the insertive sexual partner [32, 33]; whereas MSM who are primarily or exclusively the receptive sexual partner and women may be less influenced by their attitudes about condoms. We examined this possibility through follow-up analyses comparing condom attitudes between MSM who were exclusively insertive partners (n = 21) versus MSM who were exclusively receptive partners (n = 26) over the past three months (data not shown). We did not find significant differences between groups in mean condom attitude scores or the relationship between attitudes and safer sex behavior. However, the small samples may have limited our power to find significant relationships. This possibility should be explored in future research.
Although condom attitudes were the most predictive of safer sex behavior for heterosexual men living with HIV, it was increased self-efficacy, not attitudes about condoms or sexual beliefs about transmission risk, that was most predictive of safer sex behavior for MSM and women. Among MSM, this finding is consistent with prior research that has examined group differences among people living with HIV [3, 4] and highlights the ongoing need for behavioral interventions that specifically target increasing confidence to use condoms in all sexual situations among MSM living with HIV. Perhaps MSM have had more exposure to programs that promote condoms as a way to prevent sexually transmitted infections, like HIV, so that their attitudes toward condoms are not as operative for determining condom use compared to heterosexual men.
It is also plausible that heterosexual men, as the insertive partners, are more influenced by their attitudes about condoms than women, as men’s pleasure ratings for unprotected sex are higher than women’s and the sexual pleasure of the insertive partner is more closely linked to condom use [33, 34]; however, it is less clear why there exists a closer link between self-efficacy and risk behavior for MSM than heterosexual men. Because women have less control over condom use, it is possible that risk behavior may be more closely tied to their ability to negotiate and communicate about condoms [15]. Perhaps self-efficacy for condom negotiation drives risky sexual behavior more for women and MSM, and HIV prevention programs for these groups should facilitate confidence to negotiate condom use, which is less needed for heterosexual men. In contrast, eroticizing condoms and enhancing positive attitudes towards them is likely more needed in programs for heterosexual men.
Taken together, the results of this study suggest that a “one size fits all” prevention program may not work equally well for all people, and programs should instead tailor materials based on subgroup. While studies have shown that theory-based interventions are more effective than those with a non-theoretical basis [35], health behavior theories rarely account for moderation; that is, the fact that not all factors are equally predictive of behavior across groups. The applicability of behavioral theories that simultaneously account for the role of sexual attitudes and self-efficacy to predict sexual behavior, such as the theory of planned behavior [36], may not be equivalent among all subgroups of people living with HIV. More research is needed to examine gender differences in these behavioral theories. A complete test of these differences may significantly contribute both theoretically and practically to inform future prevention efforts.
Limitations
Because the study reported here is cross-sectional, our ability to draw conclusions about causality or directionality in the relationship between sexual attitudes and safer sex behavior is somewhat limited. Although sexual attitudes can influence sexual behavior, they can also change in response to sexual behavior [37]. It would be useful to investigate the relationship between sexual attitudes, beliefs, and behavior prospectively to determine directionality and examine if group differences in sexual attitudes and behaviors remain stable over time and relationships. Additionally, we relied on self-reports of unprotected sex, a behavior that is likely to be perceived as socially undesirable among people living with HIV. Even in confidential or completely anonymous studies of socially sensitive topics, there is evidence that some people bias their answers in directions that are socially desirable [38]. We used an ACASI to minimize potential bias, although it is possible that there was still some underreporting of transmission risk behavior in this study. Future work may benefit from the inclusion of reports from sexual partners. Finally, our sample was recruited from the southern United States, primarily African American, and largely unemployed. While the southern U.S. is the area of the country where the HIV epidemic is rising most rapidly, particularly among heterosexuals and minorities, our ability to generalize our findings to other populations in other areas of the U.S. or around the world is therefore limited.
CONCLUSION
This study highlights the ongoing need for HIV prevention programs among people living with HIV. In line with suggestions from prior investigators [3, 4], our results suggest that prevention programs may be more effective to the extent that they tailor materials to different risk groups of people living with HIV. For heterosexual men, in particular, prevention efforts may be more effective to the extent that they specifically address condom attitudes and increase perceptions of condom pleasure. For MSM and heterosexual women, programs should increase safer sex self-efficacy by building individual’s confidence to successfully negotiate condom use, particularly with partners at risk for HIV.
Footnotes
We did not include sexual frequency data from two participants who were extreme outliers (greater than 4 SD from the mean) on this variable.
Six men reported vaginal or anal sex with both male and female partners and were included in the MSM category. We reran multivariate analyses in the MSM sample with these six men excluded and the results remained unchanged.
REFERENCES
- 1.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: Implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 2.Kalichman SC. HIV transmission risk behaviors of men and women living with HIV-AIDS: prevalence, predictors and emerging clinical interventions. Clin Psych: Sci Prac. 2000;1:32–47. [Google Scholar]
- 3.Courtenay-Quirk C, Pals SL, Colfax G, McKirnan D, Gooden L, Eroğlu D. Factors associated with sexual risk behavior among persons living with HIV: gender and sexual identity group differences. AIDS Behav. 2008;12:685–94. doi: 10.1007/s10461-007-9259-y. [DOI] [PubMed] [Google Scholar]
- 4.Golin CE, Marks G, Wright J, et al. Psychosocial characteristics and sexual behaviors of people in care for HIV infection: An examination of men who have sex with men, heterosexual men and women. AIDS Behav. 2009;13:1129–42. doi: 10.1007/s10461-009-9613-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall HI, Song R, Rhodes P, Prejean J, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–29. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baumeister RF, Catanese KR, Vohs KD. Is there a gender difference in strength of sex drive? Theoretical views, conceptual distinctions, and a review of relevant evidence. Pers Soc Psych Rev. 2001;5:242–73. [Google Scholar]
- 7.Oliver MB, Hyde JS. Gender differences in sexuality: A meta-analysis. Psych Bull. 1993;114:29–51. doi: 10.1037/0033-2909.114.1.29. [DOI] [PubMed] [Google Scholar]
- 8.Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, Bajos N. Sexual behaviour in context: a global perspective. Lancet. 2006;368:1706–28. doi: 10.1016/S0140-6736(06)69479-8. [DOI] [PubMed] [Google Scholar]
- 9.Herbst JH, Sherba RT, Crepaz N, Britton J, Zohrabyan L, Stall RD, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men (MSM) J Acquir Immune Defic Syndr. 2005;35:228–41. [PubMed] [Google Scholar]
- 10.Mize SJS, Robinson BE, Bockting WO, Scheltema KE. Meta-analysis of the effectiveness of HIV prevention interventions for women. AIDS Care. 2002;14:163–80. doi: 10.1080/09540120220104686. [DOI] [PubMed] [Google Scholar]
- 11.Neumann MS, Johnson WD, Semaan S, Flores S, Peersman G, Hedges LV, Sogolow E. Review and meta-analysis of HIV prevention intervention research for heterosexual adult populations in the United States. J Acquir Immune Defic Syndr. 2002;30:S1006–S1117. [PubMed] [Google Scholar]
- 12.Morin SF, Myers JJ, Shade SB, Koester K, Maiorana A, Dawson-Rose C. Predicting HIV transmission risk among HIV-infected patients seen in clinical settings. AIDS Behav. 2007;11:S6–11. doi: 10.1007/s10461-007-9253-4. [DOI] [PubMed] [Google Scholar]
- 13.Albarracín D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psych Bull. 2001;127:142–61. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crepaz N, Hart T, Marks G. Highly active antiretroviral therapy and sexual risk behavior: a meta-analytic review. JAMA. 2004;292:224–36. doi: 10.1001/jama.292.2.224. [DOI] [PubMed] [Google Scholar]
- 15.Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: A meta-analysis. Psych Bull. 1999;125:90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- 16.Ross MW. Attitudes towards condoms and condom use: A review. Int J STD AIDS. 1992;3:10–16. doi: 10.1177/095646249200300103. [DOI] [PubMed] [Google Scholar]
- 17.Scott-Sheldon LAJ, Johnson BT. Eroticizing Creates Safer Sex: A Research Synthesis. The Journal of Primary Prevention. 2006;27:619–40. doi: 10.1007/s10935-006-0059-3. [DOI] [PubMed] [Google Scholar]
- 18.Golin CE, Earp JA, Grodensky CA, Patel SN, Suchindran C, Parikh M, Kalichman S, Patterson K, Swygard H, Quinlivan EB, Amola K, Chariyeva Z, Groves J. Longitudinal Effects of SafeTalk, a Motivational Interviewing-Based Program to Improve Safer Sex Practices Among People Living with HIV/AIDS. Manuscript In Press. [DOI] [PMC free article] [PubMed]
- 19.Przybyla SM, Golin CE, Davis RA, Grodensky CA, Suchindran CM. Serostatus Disclosure to Sexual Partners among Persons Living with HIV in the Southeastern United States. Poster Presented at the American Public Health Association Annual Meeting for October 25-29, 2008; San Diego, CA. [Google Scholar]
- 20.Jarlais D, Paone D, Milliken J, Turner C, Miller H, Gribble J, Shi Q, Hagan H, Friedman S. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353:1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 21.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–73. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 22.Grimley DM, Prochaska GE, Prochaska JO, Velicer WF, Galavotti C, Cabral RJ, Lansky A. Cross-validation of measures assessing decisional balance and self-efficacy for condom use. Am J Health Behav. 1996;20(6):406–16. [Google Scholar]
- 23.Parsons JT, Halkitis PN, Bimbi D, Borkowski T. Perceptions of the benefits and costs associated with condom use and unprotected sex among late adolescent college students. J Adoles. 2000;23:377–91. doi: 10.1006/jado.2000.0326. [DOI] [PubMed] [Google Scholar]
- 24.Thomas JC, Lansky A, Weiner DH, Earp JE, Schoenbach VJ. Behaviors that facilitate sexual transmission of HIV and STDs in a rural community. AIDS Behav. 1999;3:257–267. [Google Scholar]
- 25.Kalichman SC, Nachimson D, Cheery C. AIDS treatment advances and behavioral prevention set-backs: preliminary assessment of reduced threat perceptions. Health Psych. 1998;17:546–550. doi: 10.1037//0278-6133.17.6.546. [DOI] [PubMed] [Google Scholar]
- 26.SPSS for Windows, Rel. 19.0.0. SPSS Inc.; Chicago: 2010. [Google Scholar]
- 27.Sacco WP, Thompson K, Rickman RL, Levine B, Reed DL. Gender differences in AIDS-relevant condom attitudes and condom use. Poster presented at the 99th Annual Convention of the American Psychological Association; San Francisco, CA. August, 1991. [Google Scholar]
- 28.Brown IS. Development of a scale to measure attitude toward the condom as a method of birth control. J Sex Res. 1984;20:255–63. [Google Scholar]
- 29.Reilly T, Woo G. Predictors of High-Risk Sexual Behavior Among People Living With HIV/AIDS. AIDS Behav. 2001;5:205–217. [Google Scholar]
- 30.Trafimow D, Sheeran P. Some tests of the distinction between cognitive and affective beliefs. J Exp Soc Psych. 1998;34:378–97. [Google Scholar]
- 31.Fishbein M, Ajzen A. Beliefs, attitudes, intentions, and behavior: An introduction to theory and research. Addison-Wesley; Reading, MA: 1975. [Google Scholar]
- 32.Kelly JA, Kalichman SC. Reinforcement value of unsafe sex as a predictor of condom use and continued HIV/AIDS risk behavior among gay and bisexual men. Health Psych. 1998;17:328–335. doi: 10.1037//0278-6133.17.4.328. [DOI] [PubMed] [Google Scholar]
- 33.Randolph ME, Pinkerton SD, Bogart LM, Cecil H, Abramson PR. Sexual pleasure and condom use. Arch Sex Behav. 2007;36:844–848. doi: 10.1007/S10508-007-9213-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conley TD, Collins BE. Differences between condom users and condom nonusers in their multidimensional condom attitudes. J Applied Soc Psych. 2005;35:603–20. [Google Scholar]
- 35.Crepaz N, Lyles CM, Wolitski RJ, et al. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20:143–157. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- 36.Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action control: From cognition to behavior. Springer-Verlag; Berlin and New York: 1985. [Google Scholar]
- 37.Fazio RH. A practical guide to the use of response latency in social psychological research. In: Hendrick C, Clack MS, editors. Research methods in personality and social psychology. Sage; Newbury Park: 1990. [Google Scholar]
- 38.Meston CM, Heiman JR, Trapnell PD, Paulhus DL. Socially desirable responding and sexuality self-reports. J Sex Research. 1998;35:148–57. [Google Scholar]