Abstract
Hybrid tumor composed of epidermal cyst and pilomatricoma has been reported in only four times in the English literature. Herein, a cutaneous hybrid tumor composed of epidermal cyst and cystic pilomatricoma in a 58-year-old woman was presented. The tumor was located in the scalp, and measured 1 x 1 x 1 cm. The tumor was cystic and contained atheromatous materials. Histologically, the cyst was composed of epidermal cyst (50% in area) and pilomatricoma (50% in area). The pilomatricoma was composed mostly of basophilic cells. Interestingly, the pilomatricoma element of the cyst showed immunoreactive p53 and Ki-67 (labeling=40%). In conclusion, the fifth case of hybrid tumor composed of epidermal cyst and pilomatricoma was presented.
Introduction
Epidermal cyst of the skin is a very common condition, consisting of epidermis and inner laminated keratin. The squamous epithelium of epidermal cyst shows keratohyaline granules. Pilomatricoma is also frequent neoplasm of the skin, showing hair follicular differentiation. Pilomatricoma shows differentiation towards the matrix and inner sheath of a normal hair follicle as well as hair cortex. Hybrid tumor composed of epidermal cyst and pilomatricoma has been reported in only four times [1-4]. Herein reported a case of cutaneous hybrid tumor composed of epidermal cyst and cystic pilomatricoma with an immunohistochemical examination of p53 and Ki-67.
Case report
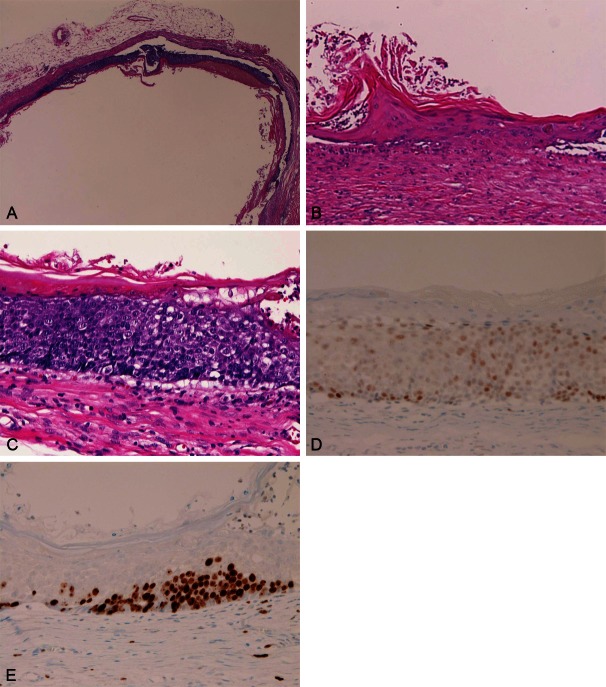
A 58-year-old Japanese woman consulted to our hospital because of a small dermal cyst in the scalp, and total cystectomy was performed. The clinical diagnosis was epidermal cyst. Grossly, the cyst measured 1 x 1 x 1 cm, and was spherical in shape. It was well defined from the surrounding tissues. Cutting showed that cyst contained atheromatous materials. Microscopically, the cyst was epidermal cyst containing laminated keratins (Figure 1A). In about 50% of the cyst, the histological features are those of typical epidermal cyst, consisting of mature squamous epithelium with a granular layer and inner laminated keratins (Figure 1B). In another 50%, the cyst was lined by atypical cells with hyperchromatic nuclei and prominent nucleoli (Figure 1C). The cellularity was very high, and a few mitotic figures were seen (Figure 1C). Nuclear pleomorphism was noted, and there were no invasive features (Figure 1A and 1C). The inner surface contained a thin layer of laminated keratin (Figure 1A and 1B). A small number of “shadow cell”-like cells were noted. An immunohistochemical study was performed with the use of Dako Envision method, as previously described [5,6]. Immunohistochemistry revealed positive p53 expression (Figure 1D), and Ki-67 labeling was high (40%) (Figure 1E) in the atypical areas. The pathological diagnosis was hybrid cyst consisting of epidermal cyst and pilomatricoma.
Figure 1.
A: A low power view of the half of the cyst. In this picture, the cyst walls consist of atypical hypercellular cells with hyperchromatic nuclei. The inner cystic area contains laminated keratin. Normal squamous cells of epidermal cyst are seen focally in this picture. HE, x20. B: Epidermal cyst area of the hybrid tumor. Epidermal squamous epithelium with granular layer is apparent. HE, x200. C: High power view of the atypical cells. The cells show hypercellularity, and have hyperchromatic nuclei with prominent nuclei. The inner surface of the atypical cells shows laminated keratin. These features are thought to be basophilic cells of pilomatricoma. HE, x200. D: The atypical cells are positive for p53 protein. Immunostaining, x200. E: The Ki-67 labeling of the atypical cells is 40%. Immunostaining, x200.
Discussion
The author thanks that the atypical cells in the present epidermal cyst are basophilic cells of the pilomatricoma. Thus, the cyst is a hybrid epidermal cyst and pilomatricoma. The presence of epidermal cyst is apparent in this case, because epidermis component with granular layer was seen. The presence of “shadow-cell”-like cells is in favor of pilomatricoma in the present atypical areas. P53 and Ki-67 have not been examined in pilomatricoma. The present case showed p53 expression and high ki-67 labeling in the atypical area, suggesting that basophilic cells in the present case show p53 mutations and high proliferative activity. The cellular atypia, p53 expression and high Ki-67 labeling may indicate the low grade malignant nature. The presence of keratinization of the inner surface of the atypical cells strongly suggests that the lesion has squamous characteristics. Therefore, the author thinks that the atypical cells in the present case are basophilic cells or malignant squamous cells. The author considers that the former is more likely.
The present atypical cells of the pilomatricoma areas must be differentiated from basal cell hyperplasia, basal cell carcinoma, and carcinoma in situ (CIS) of the epidermal cyst. The present atypical cells are different from basal cell hyperplasia because basal cell hyperplasia does not show such atypia. The present atypical cells are not basal cell carcinoma because cleft formation and nuclear palisading were not seen. In addition, the atypical cells were not basaloid. The histology of the present atypical cells is very similar to CIS of the uterine cervix. Malignant transformation of epidermal cyst is very rare [7-9]. Most of them occur in large epidermal cyst [7-9]. The present epidermal cyst was small measuring 1 x 1 x 1 cm. Most of malignancies associated with epidermal cyst were invasive squamous cell carcinoma [7-9]. CIS arising in epidermal cyst has been reported only once [10] in the English literature: Debaize et al [10] squamous cell CIS in a giant epidermal cyst [4]. Although the author thinks that the atypical areas of the present cyst is basophilic cells of cystic pilomatricoma, the possibility that the lesion is CIS derived within the epidermal cyst cannot be denied histologically and immunohistochemically.
Conflict of interest statement
The author has no conflict of interest.
References
- 1.Pujani M, Agarwal S, Goyal RK, Jyotsna PL, Teiwani N, Rautela A. Pilomatricoma coexisting with epidermal cyst. Int J Dermatol. 2011 doi: 10.1111/j.1365-4632.2010.04618.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Tsuji N, Kurokawa I, Tomie K, Omoto Y, Senba Y, Habe K, Yamanaka K, Isoda K, Tsubura A, Mizutani H. Epidermal cyst with pilomatoricoma (follicular hybrid cyst): immunohistochemical study with epithelial keratins and filaggrin. J Dermatol. 2010;37:922–925. doi: 10.1111/j.1346-8138.2010.00905.x. [DOI] [PubMed] [Google Scholar]
- 3.Urabe K, Xia J, Masuda T, Moroi Y, Furue M, Matsumoto T. Pilomatricoma-like changes in the epidermal cysts of Gardner syndrome with an APC gene mutation. J Dermatol. 2004;31:255–257. doi: 10.1111/j.1346-8138.2004.tb00669.x. [DOI] [PubMed] [Google Scholar]
- 4.Benharroch D, Sacks MI. Pilomatoricoma associated with epidermal cyst. J Cutan Pathol. 1989;16:40–43. doi: 10.1111/j.1600-0560.1989.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 5.Terada T, Kawaguchi M, Furukawa K, Sekido Y, Osamura Y. Minute mixed ductal-endocrine carcinoma of the pancreas with predominant intraductal growth. Pathol Int. 2002;52:740–746. doi: 10.1046/j.1440-1827.2002.01416.x. [DOI] [PubMed] [Google Scholar]
- 6.Terada T, Kawaguchi M. Primary clear cell adenocarcinoma of the peritoneum. Tohoku J Exp Med. 2005;271:271–275. doi: 10.1620/tjem.206.271. [DOI] [PubMed] [Google Scholar]
- 7.Lopez-Rios F, Rodriguez-Peralto JL, Castano E, Benito A. Squamous cell carcinoma arising in a cutaneous epidermal cyst: case report and literature review. Am J Dermatopathol. 1999;21:174–177. doi: 10.1097/00000372-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Cameron DS, Hilsinger RL Jr. Squamous cell carcinoma in an epidermal inclusion cyst: case report. Otolaryngol Head Neck Surg. 2003;129:141–143. doi: 10.1016/S0194-59980300466-2. [DOI] [PubMed] [Google Scholar]
- 9.Malone JC, Sonnier GB, Hughes AP, Hood AF. Poorly differentiated squamous cell carcinoma arising within an epidermal cyst. Int J Dermatol. 1999;38:556–558. doi: 10.1046/j.1365-4362.1999.00704.x. [DOI] [PubMed] [Google Scholar]
- 10.Debaize S, Gebhart M, Fourrez T, Rahier I, Baillon JM. Squamous cell carcinoma arising in a giant epidermal cyst: a case report. Acta Chir Belg. 2002;102:196–198. doi: 10.1080/00015458.2002.11679293. [DOI] [PubMed] [Google Scholar]