Abstract
BACKGROUND
Little information is available about the relationship of socioeconomic status (SES) to blunted nocturnal ambulatory blood pressure (ABP) dipping among Hispanics and whether this relationship differs by race. We sought to characterize ABP nondipping and its determinants in a sample of Hispanics.
METHODS
We enrolled 180 Hispanic participants not on antihypertensive medications. SES was defined by years of educational attainment. All participants underwent 24-hour ABP monitoring. A decrease of <10% in the ratio between average awake and average asleep systolic BP was considered nondipping.
RESULTS
The mean age of the cohort was 67.1 ± 8.7, mean educational level was 9.4 ± 4.4 years, and 58.9% of the cohort was female. The cohort was comprised of 78.3% Caribbean Hispanics with the rest from Mexico and Central/South America; 41.4% self-identified as white Hispanic, 34.4% self-identified as black Hispanic, and 24.4% did not racially self- identify. The percentage of nondippers was 57.8%. Educational attainment (10.5 years vs. 8.6 years; P <0.01) was significantly higher among dippers than nondippers. In multivariable analyses, each 1-year increase in education was associated with a 9% reduction in the likelihood of being a nondipper (odds ratio [OR], 0.91; 95% confidence interval [CI], 0.84–0.98; P = 0.01). There were significantly greater odds of being a nondipper for black Hispanics than for white Hispanics (OR, 2.83, 95% CI, 1.29–6.23; P = 0.005). Higher SES was significantly protective of nondipping in white Hispanics but not black Hispanics.
CONCLUSIONS
These results document a substantial prevalence of nondipping in a cohort of predominantly normotensive Hispanics. Dipping status varied significantly by race. Lower SES is significantly associated with nondipping status, and race potentially impacts on this relation.
Keywords: ambulatory blood pressure monitoring, blood pressure, Hispanics, hypertension, psychosocial, race, socioeconomic status.
Clinic blood pressure (BP) is not always representative of an individual’s BP during everyday life. Twenty-four-hour ambulatory BP (ABP) monitoring is used to assess individuals’ BP during normal daily activities. ABP normally shows diurnal fluctuation, with higher BP levels during the day and lower levels at night. Sustained adrenergic activity during sleep is associated with a blunting of the typical nocturnal BP reduction. Individuals whose BP remains high at night (nondippers) have more cardiovascular morbidity and mortality1 than those with a normal diurnal pattern. Evidence regarding ABP in Hispanics is limited. Only 2 small studies, which suggest that Hispanics are more likely to be nondippers than non-Hispanic whites, exist.2,3 However, determinants of ABP among Hispanics have been largely unexplored.
Lower socioeconomic status (SES) is associated with increased cardiovascular morbidity and mortality.4,5 The reasons for this association are not completely understood. Sympathetic stimulation has been shown to vary with environmental exposures, such as low SES adversity.6 It is likely that lower SES individuals are exposed to more frequent and severe stressors and thereby experience more frequent sympathetic activation. An altered autonomic tone associated with lower SES may be reflected as ABP nondipping7–10 and be particularly important among Hispanics whom, according to the US Census, are more likely to be living in poverty than non-Hispanic whites.11
In addition, there is evidence that ABP nondipping may be related to adverse psychosocial factors, such as depressive symptoms and lack of social support.12–14 However, there is little information available as to the role of psychosocial factors and SES as they relate to ABP measures among Hispanics. Furthermore, there is clear importance to the role of race as it relates to ABP in non-Hispanic populations, with ABP nondipping being more prevalent among non-Hispanic blacks than among non-Hispanic whites.15,16 The role of race among Hispanics as it relates to ABP has not been explored.
In this study, we further characterize ABP nondipping and its determinants in a sample of Hispanics. Our aim is to examine the association of SES and psychosocial factors with ABP nondipping. We hypothesize that lower SES, lower social support, and higher depressive symptoms are associated with greater ABP nondipping in this Hispanic cohort. As a secondary aim, we explore whether these associations vary by race.
METHODS
The Northern Manhattan Study (NOMAS) is a population-based prospective study ongoing since 1992, designed to evaluate the effects of medical, socioeconomic, and other risk factors on the incidence of cardiovascular disease and stroke in a multiethnic community cohort. The methods of recruitment and enrollment into NOMAS have been detailed elsewhere.17 Briefly, participants were eligible if they met the following criteria: (i) had never been diagnosed with a stroke; (ii) were aged >39 years; and (iii) resided in northern Manhattan for at least 3 months in a household with a telephone. The study was approved by the Columbia University and University of Miami Institutional Review Boards. All participants gave informed consent.
Alcohol use, smoking, and body mass index (BMI) data were collected as part of NOMAS and are included as covariablees for this analysis. Alcohol use was determined by participant acknowledgement of any alcohol consumption in the previous 12 months. Smoking status was defined as ever smoked >100 cigarettes, cigars, and pipefulls in a lifetime. Height (in inches) and weight (in pounds) measurements were obtained by trained research staff with the use of calibrated scales. BMI was calculated as weight in kilograms divided by height squared in meters after transformation.
As part of this ancillary study, additional psychosocial variables, SES variables, and ABP measures were obtained on 180 Hispanic participants drawn from the NOMAS population-based sample between December 2006 and February 2011. Use of antihypertensive medication or presence of severe hypertension (based on the average of two resting BP measurements ≥220mm Hg systolic or ≥110mm Hg diastolic) were exclusion criteria. Most ABP measures were obtained concurrently with the Cardiovascular Abnormalities and Brain Lesions study, a separate ancillary study also based on the NOMAS cohort.18 Race/ethnicity was based on self-identification through a series of interview questions modeled after the 2000U.S. Census. All participants self-identified as Hispanic and were then asked to racially self-identify as black or white. It was explained that being Hispanic is an ethnicity not a race and that identifying as black Hispanic or white Hispanic is distinct from being non-Hispanic black or non-Hispanic white. Spanish versions of all questionnaires were available. All assessments were conducted by trained bilingual research staff in English or Spanish, depending on the primary language of the participant. This ancillary study was approved by the Columbia University Institutional Review Board. All participants gave informed consent to participate in the study.
ABP measures
ABP was assessed using Spacelabs Ultralite ABP monitors (Spacelabs Healthcare, Redmond, WA). The accuracy and reliability of the device have been described.19,20 Before use, the devices were calibrated by a trained research assistant with a reference mercury sphygmomanometer with target agreement within ±5mm Hg. An appropriately sized BP cuff was placed on the subject’s nondominant arm, and the ABP monitor was programmed to automatically take a reading every 15 minutes during awake hours, and every 30 minutes during sleep. The average time-weighted awake and sleep systolic BP (SBP) and diastolic BP values were computed using participant diary-entered reports of sleep onset and wake-up times. ABP nondipping was defined as a decline in nocturnal systolic BP (SBP) of less than 10% relative to awake SBP,21 which translates to a value >0.9 for the ratio of the mean sleep SBP to the mean awake SBP (ABP night/day ratio). Thus, individuals were assigned to 2 categories of ABP dipping pattern (dippers: ratio ≤0.90; non-dippers: ratio >0.90). This cutoff has been associated with various clinical outcomes in multiple studies.21 Recordings were retrieved and analyzed with the aid of ABP report management system software (Spacelabs Systems).
SES and psychosocial measures
Information about educational level and income was obtained by questionnaire. Educational attainment as an SES marker strongly predicts generalized cardiovascular risk and mortality22 and was assessed as the number of years of completed education. Family annual income was assessed from 5 categories (<$5,000, $5,000–$15,999, $16,000–$34,999, $35,000–$74,999, ≥$75,000). High education and high income status categories were defined as above the median cut-point of education (9.0 years) and income category ($5,000–$15,999).
Social support
The CARDIA Study Social Support Scale (CSSS) has been validated and used in previous studies.23,24 The CSSS score was calculated using a weighted mean of instrumental support (4 items), network adequacy (4 items), emotional support (one item), and a social network index (2 items). The intent of a total CSSS score was to assess the overall amount of support available to the individual. Scores below the median cut-point total CSSS score of 2.9 were defined as low social support.
Depressive symptoms
The Center for Epidemiological Studies Depression (CES-D) self-report scale is designed to measure depressive symptomatology.25 The CES-D has 4 separate factors—depressed affect, somatic symptoms, positive affect, and interpersonal relations—thus encompassing the major components of depressive symptoms. Higher scores indicate a higher degree of depressive symptoms. A score of ≥16 has been used previously as the cut point for high depressive symptoms.26,27
Statistical analysis
Baseline characteristics of participants are presented for the overall population and compared according to dipping status using means ± SD for continuous variables and proportions for categorical variables. Differences between dippers and nondippers for each characteristic were assessed using the t test for continuous variables and the χ2 test for categorical variables. Medians were used to define education, income, and social support where these are used as dichotomous independent variables. The ABP night/day ratio was used in the analysis as a continuous variable but was also dichotomized as described to determine ABP dipping status. Pearson correlation coefficients were used to estimate the degree of correlation between ABP night/day ratio and psychosocial and SES measures. Linear and logistic regression were used to assess the association of SES and psychosocial factors with ABP night/day ratio and ABP dipping status, respectively, both in univariable and multivariable models. To control for variables with established effects on ABP dipping, age, sex, BMI, and tobacco use were selected as covariables.28 We conducted exploratory analyses as to whether race impacts the psychosocial and SES and ABP relationship using χ2 models to examine the relative prevalence of ABP nondipping among the different race groups. This portion of the analysis was limited to participants who self-identified as black Hispanic or white Hispanic. We tested for an interaction of SES (using interaction terms for education and income separately) and race on ABP dipping status by introducing the interaction terms into an age- and sex-adjusted model. Statistical significance was determined at the α = 0.05 level using 2-sided tests. Statistical analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
RESULTS
Most of the participants were elderly and female; more than half were smokers and consumed some level of alcohol. Seventy-eight percent of the sample consisted of Caribbean Hispanics (Dominican Republic, Puerto Rico, and Cuba), with the rest from Mexico and Central/South America. More than 75% of the cohort was able to self-identify race, with most participants self-identifying as white Hispanic. The cohort on average had a ninth-grade education and a mean annual income between $5,000 and $15,999. Few participants had depressive symptoms, as evidenced by a low mean CES-D score across the cohort. Almost 60% of the cohort reported high levels of social support. More than half of the cohort were nondippers. The cohort was normotensive on average, with <7% of the cohort being untreated hypertensives (Table 1).
Table 1.
Characteristics of subjects (n = 180)
| Characteristic | Percentage or mean ± SD |
|---|---|
| Demographic variables | |
| Age, years | 67.1±8.7 |
| Female/male, % | 58.9/41.1 |
| Smoker | 52.8% |
| Alcohol use | 63.3% |
| Hispanic race | |
| White | 41.1% |
| Black | 34.4% |
| Other/no response | 24.4% |
| SES and psychosocial variables | |
| Education, years | 9.4±4.4 |
| Income category | 2.4±1.0 |
| CES-D score | 7.8±9.6 |
| High depressive symptoms | 18.0% |
| CSSS score | 2.9±0.4 |
| High social support | 58.3% |
| BP components | |
| SBP, mm Hg | 126.6±14.3 |
| ABP night/day ratio | 0.9±0.07 |
| Nondippers | 57.8% |
| SBP category distribution | |
| Normotensive | 46.7% |
| Prehypertensive | 46.7% |
| Hypertensive | 6.7% |
Abbreviations: ABP, ambulatory blood pressure; BP, blood pressure; CES-D, Center for Epidemiological Studies Depression; CSSS, CARDIA Study Social Support Scale; SBP, systolic blood pressure; SES, socioeconomic status.
Univariate determinants of ABP dipping status
Among the demographic characteristics, age and sex were the only consistent demographic determinants of ABP dipping status. Being male was actually protective of ABP nondipping (odds ratio [OR], 0.44; 95% confidence interval [CI], 0.24–0.80; P < 0.01). BMI, smoking, and alcohol use were not associated with ABP dipping status. Among the psychosocial components, CES-D or CSSS scores were not significantly different according to ABP dipping status (Table 2).
Table 2.
Characteristics by ambulatory blood pressure dipping status
| Dipper (n = 76) | Nondipper (n = 104) | P value | |
|---|---|---|---|
| Demographic variables | |||
| Age, years | 65.4 ± 8.6 | 68.4 ± 8.6 | 0.02 |
| BMI, kg/m2 | 27.7 ± 3.9 | 27.7 ± 3.9 | 0.92 |
| Male | 52.6% | 32.7% | 0.007 |
| Smoker | 60.5% | 47.1% | 0.08 |
| Alcohol use | 64.5% | 62.5% | 0.79 |
| SES and psychosocial variables | |||
| Education, years | 10.5 ± 4.3 | 8.6 ± 4.3 | 0.004 |
| High education | 59.2% | 42.3% | 0.03 |
| Income category | 2.6 ± 0.9 | 2.2 ± 1.1 | <0.01 |
| High income | 48.7% | 21.2% | 0.0001 |
| CES-D score | 7.5 ± 8.9 | 8.1 ± 10.1 | 0.66 |
| High depressive symptoms | 14.7% | 20.4% | 0.33 |
| CSSS score | 2.8 ± 0.4 | 2.9 ± 0.4 | 0.10 |
| High social support | 42.1% | 55.8% | 0.07 |
Abbreviations: BMI, body mass index; CES-D, Center for Epidemiological Studies Depression; CSSS, CARDIA Study Social Support Scale; SES, socioeconomic status.
SES impact on ABP dipping
There was a moderate inverse correlation between years of education and ABP night/day ratio (Pearson r = −0.27; P < 0.01). Mean educational attainment and income level were significantly greater among dippers than among nondippers (Table 2). The percentage of subjects with high educational levels was 42% among nondippers and 59% among dippers (P = 0.03). Increasing income and education were each associated with lower ABP night/day ratio. Each increasing year of education or increasing category of income was associated with a 10% and 43% less likely chance of being a nondipper, respectively (Table 3). These relations persisted on multivariable analysis. After adjusting for age, sex, BMI, and tobacco use, higher-educated Hispanics had a significantly lower prevalence of nondipping than their less-educated counterparts (OR, 0.91; 95% CI, 0.84–0.98; P = 0.01) (Tables 4 and 5). Among those with low education, those with low income were more likely to be nondippers than those with high income (76.5% vs. 34.8%; P = 0.0003). Among those with high education, those with low income were no more likely to be nondippers than those with high income (56.6% vs. 38.9%; P = 0.10). Educational attainment was significantly associated with ABP nondipping status and day/night ratio among women but not men. Income level was significantly associated with nondipping status and ABP day/night ratio among men but not women (Table 5).
Table 3.
Univariable predictors of ambulatory blood pressure nondipping
| Variable | Regression coefficient | SE | P value |
|---|---|---|---|
| ABP nondipping statusa | |||
| Age, years | 0.04 | 0.02 | 0.02 |
| Male | −0.83 | 0.31 | <0.01 |
| Smoker | −0.54 | 0.31 | 0.08 |
| Alcohol use | −0.09 | 0.31 | 0.79 |
| BMI, kg/m2 | 0.03 | 0.04 | 0.56 |
| CES-D score | 0.01 | 0.02 | 0.65 |
| CSSS score | 0.58 | 0.35 | 0.10 |
| Income | −0.43 | 0.16 | <0.01 |
| Education, years | −0.10 | 0.04 | <0.01 |
| ABP night/day ratiob | |||
| Age, years | 0.002 | 0.0006 | <0.001 |
| Male | −0.02 | 0.01 | 0.05 |
| Smoker | −0.01 | 0.01 | 0.21 |
| Alcohol use | −0.002 | 0.01 | 0.82 |
| CES-D score | 0.00003 | 0.0005 | 0.95 |
| CSSS score | 0.02 | 0.01 | 0.12 |
| Income | −0.01 | 0.005 | <0.01 |
| Education, years | −0.004 | 0.001 | <0.001 |
Abbreviations: ABP, ambulatory blood pressure; BMI, body mass index; CES-D, Center for Epidemiological Studies Depression; CSSS, CARDIA Study Social Support Scale; SES, socioeconomic status.
aOutcome variable is nondipping status.
bOutcome variable is ABP night/day ratio.
Table 4.
Multivariable predictors of ambulatory blood pressure nondipping
| Variable | ORa | 95% CIs | |
|---|---|---|---|
| High income | 0.35 | 0.17–0.70 | |
| High education | 0.52 | 0.27–0.99 | |
| Education, per year | 0.90 | 0.84–0.97 | |
| Income, per category | 0.73 | 0.53–1.00 | |
| CSSS score | 1.86 | 0.87–3.96 | |
| Regression coefficientb | SE | P value | |
| High income | −0.03 | 0.01 | 0.01 |
| High education | −0.02 | 0.009 | 0.046 |
| Income | −0.01 | 0.005 | 0.02 |
| Education | −0.004 | 0.001 | <0.01 |
| CSSS score | 0.02 | 0.01 | 0.19 |
All analyses were adjusted for age, sex, body mass index, and tobacco use. Abbreviations: CI, confidence interval; CSSS, CARDIA Study Social Support Scale; OR, odds ratio.
aOutcome variable is non-dipping status.
bOutcome variable is ambulatory blood pressure night-day ratio.
Table 5.
Multivariable predictors of ambulatory blood pressure nondipping stratified by sex
| Variable | Men | Women | ||||
|---|---|---|---|---|---|---|
| ORa | 95% CIs | ORa | 95% CIs | |||
| High income | 0.23 | 0.08–0.65 | 0.42 | 0.15–1.18 | ||
| High education | 0.70 | 0.26–1.86 | 0.41 | 0.17–0.98 | ||
| Education, per year | 0.93 | 0.82–1.05 | 0.89 | 0.80–0.98 | ||
| Income, per category | 0.56 | 0.31–1.01 | 0.74 | 0.49–1.12 | ||
| CSSS score | 3.39 | 0.88–12.98 | 1.50 | 0.55–4.11 | ||
| Black Hispanic vs. white Hispanic | 3.71 | 1.10–12.57 | 1.41 | 0.55–3.62 | ||
| Regression coefficientb | SE | P value | Regression coefficientb | SE | P value | |
| High income | −0.037 | 0.02 | 0.02 | −0.018 | 0.02 | 0.24 |
| High education | −0.01 | 0.02 | 0.53 | −0.026 | 0.01 | 0.03 |
| Income | −0.018 | 0.008 | 0.03 | −0.01 | 0.006 | 0.10 |
| Education | −0.004 | 0.002 | 0.05 | −0.004 | 0.001 | 0.008 |
| CSSS score | 0.05 | 0.02 | 0.005 | −0.002 | 0.01 | 0.91 |
All analyses were adjusted for age, body mass index, and tobacco use. Abbreviations: CI, confidence interval; CSSS, CARDIA Study Social Support Scale; OR, odds ratio.
aOutcome variable is nondipping status.
bOutcome variable is ambulatory blood pressure night/day ratio.
Impact of race on ABP nondipping
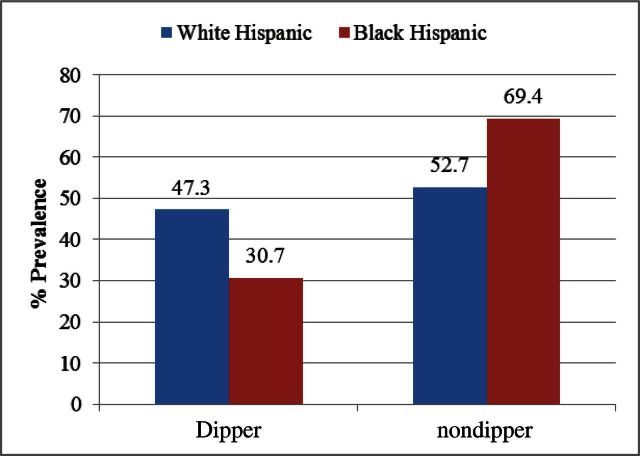
In this cohort of Hispanics, race was not associated with education, income, depressive symptoms, social support, alcohol, or smoking (Table 6). However, the prevalence of ABP nondipping varied significantly by race (69.4% among black Hispanics vs. 52.7% among white Hispanics; P = 0.048; Figure 1). There was a >2-fold odds of being a nondipper for black Hispanics vss white Hispanics after adjusting for age, sex, BMI, and tobacco use (OR, 2.83, 95% CI 1.29–6.23; P = 0.005). In sex-stratified models, race remained independently associated with nondipping status among men but not women. Educational levels were important in determining ABP nondipping among white Hispanics (71.4% vs. 35.9%; P = 0.002) but not among black Hispanics (70.6% vs. 67.9%; P = 0.82). Prevalence of ABP nondipping was high among black Hispanics regardless of educational level, whereas among white Hispanics ABP nondipping prevalence was high only among those with lower education (Figure 2a). Among participants with high income levels, black Hispanics had a higher prevalence of ABP nondipping than white Hispanics (61.1% vs. 27.6%; P = 0.02). All Hispanics with low income levels had a higher prevalence of ABP nondipping regardless of race (68.9% vs. 72.7%; P = 0.69) compared with Hispanics with high income levels (Figure 2b). For the outcome of ABP dipping status, we found a nonsignificant statistical interaction of race with education status (P = 0.054) and a statistically significant interaction of race with income (P = 0.01). In exploring SES as a potential mediator of the association of race with ABP nondipping, we did not see an association between race and education or income in this Hispanic cohort.
Table 6.
Characteristics of Hispanic subjects stratified by race
| Variable | White Hispanic (n = 74) | Black Hispanic (n = 62) | Other/no response (n = 44) | P valuea | P valueb |
|---|---|---|---|---|---|
| Age, years | 69.1 ± 9.3 | 64.4 ± 8.6 | 67.7 ± 6.7 | <0.01 | 0.34 |
| Male | 43.2% | 37.1% | 43.2% | 0.47 | 0.99 |
| Alcohol use | 66.2% | 61.3% | 61.4% | 0.55 | 0.59 |
| Smoker | 55.4% | 45.2% | 59.1% | 0.23 | 0.70 |
| Education, years | 10.0 ± 4.4 | 9.3 ± 4.3 | 8.7 ± 4.5 | 0.94 | 0.11 |
| Income category | 2.4 ± 0.8 | 2.4 ± 1.4 | 2.2 ± 0.8 | 0.99 | 0.20 |
| CESD score | 7.2 ± 8.7 | 7.55 ± 10.56 | 9.5 ± 10.7 | 0.94 | 0.21 |
| High depressive symptoms | 16.4% | 16.4% | 22.7% | 0.99 | 0.40 |
| CSSS score | 2.9 ± 0.43 | 2.8 ± 0.43 | 2.8 ± 0.47 | 0.11 | 0.18 |
| High social support | 56.7% | 43.6% | 47.7% | 0.13 | 0.34 |
aComparing black Hispanic with white Hispanic.
bComparing Other/no response with white Hispanic.
Figure 1.
Proportion of participants according to ambulatory blood pressure nondipping status by race. The prevalence of nondipping depends on race. The proportion of white Hispanics was not different among dippers vs. nondippers; however, the proportion of black Hispanics more than doubles when going from dippers to nondippers.
Figure 2.
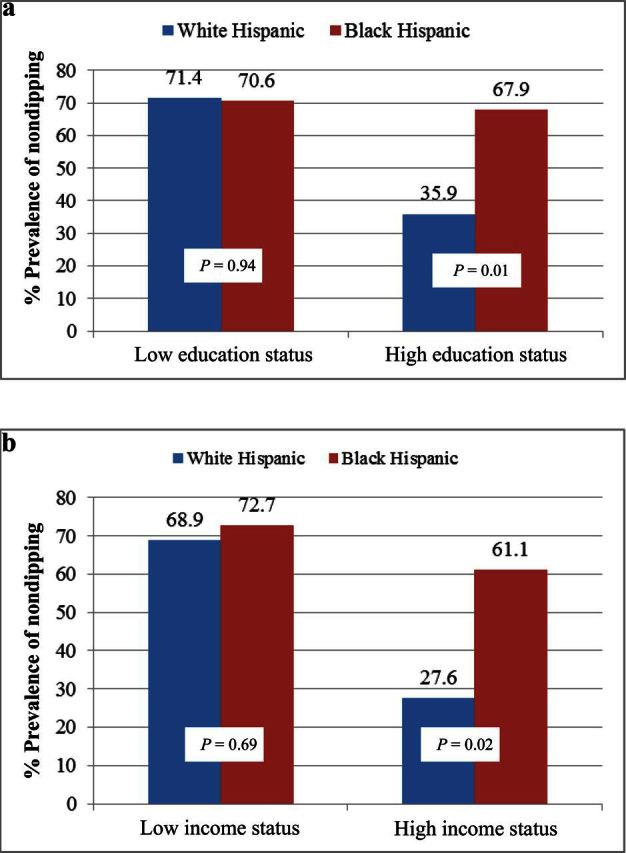
Differences in dipping status by race and education and race and income. (a) Prevalence of ambulatory blood pressure (ABP) nondipping was high among black Hispanics regardless of educational level, whereas among white Hispanics, ABP nondipping prevalence was high only among those with lower education. (b) Among participants with high income levels, being black Hispanic was associated with more prevalent ABP nondipping compared with white Hispanic. All Hispanics at low income levels regardless of race had a similar prevalence of ABP nondipping.
DISCUSSION
These data are the first to indicate that less education and less income are independently associated with more prevalent ABP nondipping in a mostly normotensive cohort of Hispanics. This study documents a 58% prevalence of ABP nondipping, which is substantial compared with studies that indicate a prevalence ranging 30%–40% among normotensive and untreated hypertensive populations.29,30 These results are the first to show that race is a significant determinant of ABP nondipping in a cohort of Hispanics. Black Hispanic are significantly more likely to be nondippers than white Hispanics. Furthermore, race in this cohort of Hispanics appears to significantly impact the relationship between SES and dipping.
There is a remarkable dearth of information about the prevalence and correlates of ABP nondipping among US Hispanics. Non-Hispanic blacks are more likely to be classified as nondippers than non-Hispanic whites.15,16 Only 1 study of Mexican-Americans2 and one small study of Caribbean Hispanics3 suggested that Hispanics, like non-Hispanic blacks, are more likely to be nondippers than non-Hispanic whites. These studies were limited by the absence of the added dimensions of Hispanic race and SES and psychosocial factors to explore their potential relationship to ABP measures in Hispanics. Although the cause of the high prevalence of ABP nondipping in this Hispanic cohort is unclear, there is evidence among non-Hispanic blacks that the ABP nondipping pattern may be related more to adverse environmental and psychosocial factors than to genetic factors.12,13,31 African blacks have greater nocturnal dipping than US non-Hispanic blacks, comparable with the dipping observed in US non-Hispanic whites.32 Because US Hispanics share similar socioeconomic and environmental disadvantages with non-Hispanic blacks, this important line of thinking needs to be further studied.
In this study, ABP nondipping was independently related to SES factors, with higher education and higher income associated with a lower prevalence of nondipping in a Hispanic cohort. The reason for the effect of low SES on ABP dipping is not completely understood. It is possible that individuals with lower SES are more likely to be exposed to more frequent and severe stressors and thereby experience more frequent sympathetic activation. This chronic or even intermittent adrenergic stimulation, even in the absence of overt hypertension, may be reflected as blunted nocturnal ABP variability representing an altered sympathetic–parasympathetic balance.8,9,33 A higher SES is associated with positive health outcomes regardless of disease,34,35 and this effect likely derives not just from an improved health behavior profile but also secondary to decreased psychological and physiological effects of stress,36 which involves lower exposure to stress compared with their low SES counterparts, as well as the availability of greater resources with which to cope with stress.
Studies have found that depressive disorders are related to incident cardiovascular morbidity and mortality.37 Data show that low social support is associated with an increased likelihood of being a nondipper among non-Hispanic blacks.24 However, our cohort of Hispanics had low levels of depressive symptoms and high levels of perceived social support, and these 2 psychosocial factors did not predict ABP dipping.
Our study reports an association between race and ABP nondipping in a Hispanics cohort. Hispanic race is infrequently reported or assessed and its impact on ABP dipping and SES and psychosocial factors is not known. Hispanics share a diverse ancestry, with varying admixture of Native American, European, and West African ancestry.38,39 This is the first study to note that black Hispanics are more prone to ABP nondipping than white Hispanics. Hispanics with greater African admixture may have more similarity in prevalence of ABP nondipping with non-Hispanic blacks than previously appreciated. Geographic ancestral origins may contribute to the differential distribution of ABP nondipping among black vs. white Hispanics. The association of lower SES with ABP nondipping in this Hispanic population seems driven by the correlation seen in white Hispanics, and the high prevalence of nondipping among black Hispanics does not appear to be explained by SES or psychosocial factors. The role/association of African vs. European genetic ancestry specifically with regards to ABP, SES, or psychosocial factors remains to be explored. Furthermore, it is unclear whether race in the context of this study is reflecting a physiological variable or a social label. Perceived racism is a social environmental characteristic identified as a psychosocial stressor contributing to increased rates of hypertension among non-Hispanic blacks.40,41 Among Hispanics, perceived racism may be related to both daytime and nocturnal ABP 42 and also potentially impacted upon by race. These issues remain to be further defined.
A strength of our study is the standard and validated assessment of ABP on a Hispanic population. ABP was assessed using participant diary reports of sleep onset and wake-up times rather than arbitrary fixed-time intervals. This approach provides a more accurate assessment of ABP during sleep because waking times can vary considerably between participants. Although comprised of only 180 participants, the current study is still the largest study of diurnal ABP assessment in a Hispanic population. This is important because there is less published information about ABP dipping and other cardiovascular risk factors in this population. Another strength is the simultaneous assessment of several SES and psychosocial factors.
Several limitations must be noted. First, our study includes mostly Caribbean Hispanics, who represent only one subfraction of all Hispanics.43 Thus our findings may not be generalizable to all Hispanics. Second, our assessment of race and ethnicity was through self-designation, which carries limitations.44,45 Hispanics are an admixed population, and the US concept of race being only white or black may be confusing.46 There is discordance between understandings of race among Hispanics and the predominant US conceptualizations of this construct. Among Hispanics, the question of race is frequently confused with the question of ethnicity. Some Hispanics feel that being Hispanic is its own race and thus refuse to categorize along the US system; there is also a perception that for Hispanics to identify as black or white in the United States, he/she is attaching or aligning themselves with the US white or black community. We therefore spent considerable time with each participant to explain what was meant when we asked them to self-identify race. We did not address dietary factors or sleep quality; however the impact of these factors on ABP dipping is not clear.9, 47–49 Lastly, a potential limitation is the exclusion of Hispanics who were not able to racially self-identify for a portion of the analysis. The prevalence of nondipping in this “Other/No Response” group was exactly 50%. In additional regression models that included “Other/No Response” as a separate category, the odds of being a nondipper for black Hispanics (OR, 2.8; 95% CI, 1.3–6.2) compared with white Hispanics remained similar to what was seen in the original analysis. The “Other/No Response” group did not predict ABP dipping in this model.
In conclusion, our study contributes to the growing body of research on Hispanic cardiovascular health and extends the understanding of SES and race differences in ABP dipping. In a predominantly normotensive Hispanic cohort, we documented a substantial prevalence of ABP nondipping, particularly among black Hispanics and showed that lower SES is a predictor of dipping status. In this cohort of Hispanics, race potentially impacts the relation of SES with nocturnal ABP dipping. With regards to ABP, black and white Hispanics may have commonalities with their non-Hispanic counterparts that have previously been underappreciated. This implies that conclusions made about the health status of Hispanics should incorporate the assessment of race in this population.
DISCLOSURES
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
The authors thank the staff and the participants of the NOMAS for their valuable contributions. In particular, the authors acknowledge Janet T. De Rosa, Research Manager for the NOMAS, whose insight and support was invaluable in the execution of this ancillary study. This research was supported in part by an NIH/NINDS R01 NS 29993 (to Dr Sacco), an NHLBI P01 HL047540 (to Dr Schwartz), the Robert Wood Johnson Harold Amos Medical Faculty Development Program (to Dr Rodriguez), and an NHLBI K23 HL079343 (to Dr Rodriguez).
REFERENCES
- 1. Hansen TW, Kikuya M, Thijs L, Bjorklund-Bodegard K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens 2007; 25:1554–1564 [DOI] [PubMed] [Google Scholar]
- 2. Hyman DJ, Ogbonnaya K, Taylor AA, Ho K, Pavlik VN. Ethnic differences in nocturnal blood pressure decline in treated hypertensives. Am J Hypertens 2000; 13:884–891 [DOI] [PubMed] [Google Scholar]
- 3. Phillips RA, Sheinart KF, Godbold JH, Mahboob R, Tuhrim S. The association of blunted nocturnal blood pressure dip and stroke in a multiethnic population. Am J Hypertens 2000; 13:1250–1255 [DOI] [PubMed] [Google Scholar]
- 4. Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 1993; 88:1973–1998 [DOI] [PubMed] [Google Scholar]
- 5. Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med 1993; 329:103–109 [DOI] [PubMed] [Google Scholar]
- 6. Everson SA, Lynch JW, Kaplan GA, Lakka TA, Sivenius J, Salonen JT. Stress-induced blood pressure reactivity and incident stroke in middle-aged men. Stroke 2001; 32:1263–1270 [DOI] [PubMed] [Google Scholar]
- 7. Janicki-Deverts D, Cohen S, Adler NE, Schwartz JE, Matthews KA, Seeman TE. Socioeconomic status is related to urinary catecholamines in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Psychosom Medic 2007; 69:514–520 [DOI] [PubMed] [Google Scholar]
- 8. Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL. Nighttime blood pressure dipping: the role of the sympathetic nervous system. Am J Hypertens 2002; 15:111–118 [DOI] [PubMed] [Google Scholar]
- 9. Sherwood A, Routledge FS, Wohlgemuth WK, Hinderliter AL, Kuhn CM, Blumenthal JA. Blood pressure dipping: ethnicity, sleep quality, and sympathetic nervous system activity. Am J Hypertens 2011; 24:982–988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hickson DA, Diez Roux AV, Wyatt SB, Gebreab SY, Ogedegbe G, Sarpong DF, Taylor HA, Wofford MR. Socioeconomic position is positively associated with blood pressure dipping among African-American adults: the Jackson Heart Study. Am J Hypertens 2011; 24:1015–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. deNavas-Walt C BD, Mills RJ. US Census Bureau, current population reports, income, poverty and health insurance coverage in the United States, 2003. US Government Printing Office: Washington, DC, 2004:60–226 [Google Scholar]
- 12. Ituarte PH, Kamarck TW, Thompson HS, Bacanu S. Psychosocial mediators of racial differences in nighttime blood pressure dipping among normotensive adults. Health Psychol 1999; 18:393–402 [DOI] [PubMed] [Google Scholar]
- 13. Kario K, Schwartz JE, Davidson KW, Pickering TG. Gender differences in associations of diurnal blood pressure variation, awake physical activity, and sleep quality with negative affect: the work site blood pressure study. Hypertension 2001; 38:997–1002 [DOI] [PubMed] [Google Scholar]
- 14. Spruill TM, Gerin W, Ogedegbe G, Burg M, Schwartz JE, Pickering TG. Socioeconomic and psychosocial factors mediate race differences in nocturnal blood pressure dipping. Am J Hypertens 2009; 22:637–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gretler DD, Fumo MT, Nelson KS, Murphy MB. Ethnic differences in circadian hemodynamic profile. Am J Hypertens 1994; 7:7–14 [DOI] [PubMed] [Google Scholar]
- 16. Mayet J, Chapman N, Li CK, Shahi M, Poulter NR, Sever PS, Foale RA, Thom SA. Ethnic differences in the hypertensive heart and 24-hour blood pressure profile. Hypertension 1998; 31:1190–1194 [DOI] [PubMed] [Google Scholar]
- 17. Rodriguez CJ, Sciacca RR, Diez-Roux AV, Boden-Albala B, Sacco RL, Homma S, DiTullio MR. Relation between socioeconomic status, race-ethnicity, and left ventricular mass: the Northern Manhattan study. Hypertension 2004; 43:775–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Russo C, Jin Z, Homma S, Rundek T, Elkind MS, Sacco RL, Di Tullio MR. Effect of diabetes and hypertension on left ventricular diastolic function in a high-risk population without evidence of heart disease. Eur J Heart Fail 2010; 12:454–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. O’Brien E, Asmar R, Beilin L, Imai Y, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens 2005; 23:697–701 [DOI] [PubMed] [Google Scholar]
- 20. Baumgart P, Kamp J. Accuracy of the SpaceLabs Medical 90217 ambulatory blood pressure monitor. Blood Press Monit 1998; 3:303–307 [PubMed] [Google Scholar]
- 21. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111:697–716 [DOI] [PubMed] [Google Scholar]
- 22. Salomaa V, Niemela M, Miettinen H, Ketonen M, Immonen-Raiha P, Koskinen S, Mahonen M, Lehto S, Vuorenmaa T, Palomaki P, Mustaniemi H, Kaarsalo E, Arstila M, Torppa J, Kuulasmaa K, Puska P, Pyorala K, Tuomilehto J. Relationship of socioeconomic status to the incidence and prehospital, 28-day, and 1-year mortality rates of acute coronary events in the FINMONICA myocardial infarction register study. Circulation 2000; 101:1913–1918 [DOI] [PubMed] [Google Scholar]
- 23. Knox SS, Adelman A, Ellison RC, Arnett DK, Siegmund K, Weidner G, Province MA. Hostility, social support, and carotid artery atherosclerosis in the National Heart, Lung, and Blood Institute Family Heart Study. Am J Cardiol 2000; 86:1086–1089 [DOI] [PubMed] [Google Scholar]
- 24. Rodriguez CJ, Burg MM, Meng J, Pickering TG, Jin Z, Sacco RL, Boden-Albala B, Homma S, Di Tullio MR. Effect of social support on nocturnal blood pressure dipping. Psychosomatic Medicine 2008; 70:7–12 [DOI] [PubMed] [Google Scholar]
- 25. Radloff LS. The CES-D scale. A self-report depression scale for research in the general population. App. Psychol Meas 1977; 1:385–401 [Google Scholar]
- 26. Gallegos-Carrillo K, Flores YN, Denova-Gutierrez E, Mendez-Hernandez P, Dosamantes-Carrasco LD, Henao-Moran S, Borges G, Halley-Castillo E, Macias N, Salmeron J. Physical activity and reduced risk of depression: results of a longitudinal study of Mexican adults. Health Psychol 2012. Sep 3, 2012:[Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27. Gallagher D, O’Regan C, Savva GM, Cronin H, Lawlor BA, Kenny RA. Depression, anxiety and cardiovascular disease: which symptoms are associated with increased risk in community dwelling older adults? J Affect Disord 2012; 142:132–138 [DOI] [PubMed] [Google Scholar]
- 28. Kanbay M, Turgut F, Uyar ME, Akcay A, Covic A. Causes and mechanisms of nondipping hypertension. Clin Exp Hypertens 2008; 30:585–597 [DOI] [PubMed] [Google Scholar]
- 29. Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, Ojima T, Shimada K. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens 2003; 16:434–438 [DOI] [PubMed] [Google Scholar]
- 30. de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, de la Cruz JJ, Sobrino J, Llisterri JL, Alonso J, Vinyoles E, Pallares V, Sarria A, Aranda P, Ruilope LM. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension 2009; 53:466–472 [DOI] [PubMed] [Google Scholar]
- 31. Stepnowsky CJ, Jr, Nelesen RA, DeJardin D, Dimsdale JE. Socioeconomic status is associated with nocturnal blood pressure dipping. Psychosom Med 2004; 66:651–655 [DOI] [PubMed] [Google Scholar]
- 32. Fumo MT, Teeger S, Lang RM, Bednarz J, Sareli P, Murphy MB. Diurnal blood pressure variation and cardiac mass in American blacks and whites and South African blacks. Am J Hypertens 1992; 5:111–116 [DOI] [PubMed] [Google Scholar]
- 33. Imai Y, Abe K, Sasaki S, Minami N, Nihei M, Munakata M, Murakami O, Matsue K, Sekino H, Miura Y. Altered circadian blood pressure rhythm in patients with Cushing’s syndrome. Hypertension 1988; 12:11–19 [DOI] [PubMed] [Google Scholar]
- 34. Du XL, Lin CC, Johnson NJ, Altekruse S. Effects of individual-level socioeconomic factors on racial disparities in cancer treatment and survival: findings from the National Longitudinal Mortality Study, 1979–2003. Cancer 2011; 117:3242–3251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Major JM, Doubeni CA, Freedman ND, Park Y, Lian M, Hollenbeck AR, Schatzkin A, Graubard BI, Sinha R. Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PLoS One 2010; 5:e15538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mujahid MS, Diez Roux AV, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (the Multi-Ethnic Study of Atherosclerosis). Am J Hypertens 2011; 24:187–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Haynes SG, Levine S, Scotch N, Feinleib M, Kannel WB. The relationship of psychosocial factors to coronary heart disease in the Framingham study. I. Methods and risk factors. Am J Epidemiol 1978; 107:362–383 [DOI] [PubMed] [Google Scholar]
- 38. Bonilla C, Shriver MD, Parra EJ, Jones A, Fernandez JR. Ancestral proportions and their association with skin pigmentation and bone mineral density in Puerto Rican women from New York city. Hum Genet 2004; 115:57–68 [DOI] [PubMed] [Google Scholar]
- 39. Bonilla C, Parra EJ, Pfaff CL, Dios S, Marshall JA, Hamman RF, Ferrell RE, Hoggart CL, McKeigue PM, Shriver MD. Admixture in the Hispanics of the San Luis Valley, Colorado, and its implications for complex trait gene mapping. Ann Hum Genet 2004; 68:139–153 [DOI] [PubMed] [Google Scholar]
- 40. Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. Am J Public Health 1996; 86:1370–1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sims M, Diez-Roux AV, Dudley A, Gebreab S, Wyatt SB, Bruce MA, James SA, Robinson JC, Williams DR, Taylor HA. Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. Am J Public Health 2012; 102(Suppl 2):S258–S265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brondolo E, Libby DJ, Denton EG, Thompson S, Beatty DL, Schwartz J, Sweeney M, Tobin JN, Cassells A, Pickering TG, Gerin W. Racism and ambulatory blood pressure in a community sample. Psychosom Med 2008; 70:49–56 [DOI] [PubMed] [Google Scholar]
- 43. Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: the National Health Interview Survey 2000–2005. J Gen Intern Med 2010; 25:847–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kaufman JS, Cooper RS. Commentary: considerations for use of racial/ethnic classification in etiologic research. Am J Epidemiol 2001; 154:291–298 [DOI] [PubMed] [Google Scholar]
- 45. Jones CP. Invited commentary: “race,” racism, and the practice of epidemiology. Am J Epidemiol 2001; 154:299–304; discussion 305–306 [DOI] [PubMed] [Google Scholar]
- 46. Allen VC, Lachance C, Rios-Ellis B, Kaphingst KA. Issues in the assessment of “race” among Latinos: implications for research and policy. Hisp J Behav Sci 2011; 33:411–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jehn ML, Brotman DJ, Appel LJ. Racial differences in diurnal blood pressure and heart rate patterns: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Arch Intern Med 2008; 168:996–1002 [DOI] [PubMed] [Google Scholar]
- 48. Hughes JW, Kobayashi I, Deichert NT. Ethnic differences in sleep quality accompany ethnic differences in night-time blood pressure dipping. Am J Hypertens 2007; 20:1104–1110 [DOI] [PubMed] [Google Scholar]
- 49. Prather AA, Blumenthal JA, Hinderliter AL, Sherwood A. Ethnic differences in the effects of the DASH diet on nocturnal blood pressure dipping in individuals with high blood pressure. Am J Hypertens 2011; 24:1338–1344 [DOI] [PMC free article] [PubMed] [Google Scholar]