Nosocomial diarrhea is a common complication of hospitalization that is most often not due to Clostridium difficile. We review the diverse causes of nosocomial diarrhea and provide an algorithm for diagnosing and managing patients when C. difficile tests are negative.
Abstract
Diarrhea is common among hospitalized patients but the causes are distinct from those of diarrhea in the community. We review existing data about the epidemiology of nosocomial diarrhea and summarize recent progress in understanding the mechanisms of diarrhea. Clinicians should recognize that most cases of nosocomial diarrhea have a noninfectious etiology, including medications, underlying illness, and enteral feeding. Apart from Clostridium difficile, the frequency of infectious causes such as norovirus and toxigenic strains of Clostridium perfringens, Klebsiella oxytoca, Staphylococcus aureus, and Bacteroides fragilis remains largely undefined and test availability is limited. Here we provide a practical approach to the evaluation and management of nosocomial diarrhea when tests for C. difficile are negative.
Nosocomial diarrhea is a common complication in hospitalized patients but its causes and significance are underappreciated. Diarrhea predisposes patients to infections, contributes to morbidity and mortality, and increases hospital length of stay and costs [1–6]. Physicians frequently focus on Clostridium difficile infection (CDI) as the primary cause of diarrhea but most cases are due to medications, enteral feeding, and underlying illness [5–15]. In fact, clinical studies indicate that 12%–32% of hospitalized patients develop diarrhea but ≤20% of cases are attributable to CDI [7, 12, 13]. Other infectious causes are uncommon, but alterations in the intestinal microbiome appear to play a role in many patients [16–19]. Here we review the infectious and noninfectious causes of nosocomial diarrhea, focusing primarily on adults in industrialized countries, and provide an algorithm for diagnosing and managing patients with nosocomial diarrhea when C. difficile tests are negative.
BACKGROUND AND PATHOPHYSIOLOGY
Definitions
Diarrhea is defined as at least 1 day with ≥3 unformed stools or a significant increase in stool frequency above baseline [18, 20, 21]. Nosocomial diarrhea is an acute episode of diarrhea in a hospitalized patient that was not present on admission and arises after ≥3 days of hospitalization [7, 22]. Clinically, this definition is useful because the likelihood of community-acquired viral, bacterial, or parasitic gastroenteritis developing after the third hospital day is low enough that testing and evaluation can be focused on causes that are more likely in hospitalized patients [22].
Clinical Spectrum of Disease
Most nosocomial diarrhea not due to CDI is mild or moderate and resolves after a few days, though there are exceptions [7]. For example, toxin-producing strains of Clostridium perfringens and Klebsiella oxytoca can cause severe symptoms or colitis [23, 24]. Norovirus infection, which is classically associated with a short vomiting illness in the community, often lasts longer in hospitalized patients and can be particularly prolonged and severe in transplant patients [4, 25]. Medication-associated diarrhea can also be severe and chemotherapy-induced diarrhea can be indistinguishable from CDI [3, 20, 26].
Incidence
Nosocomial diarrhea is common. Two studies from 1987 and 1991 followed large numbers of patients from admission to discharge, documenting diarrhea in 32% and 22% of patients, respectively [7, 12]. More recently, a point prevalence study of 485 hospitalized patients found that 12% of patients had diarrhea, including 27% of those hospitalized for ≥3 weeks [13]. Other studies focusing on high-risk groups such as hematopoietic stem cell transplant (HSCT) patients report rates of diarrhea as high as 80% [11, 27].
Impact
CDI is a recognized cause of increased morbidity, mortality, hospital length of stay, and healthcare costs [21]. The impact of diarrhea from other causes is less well characterized, but it contributes to fluid and electrolyte abnormalities and nutritional deficiency, and has been associated with an increased risk of wound and urinary tract infections [2, 6, 9]. The increased risk of bloodstream infection associated with femoral catheters has also been attributed to fecal contamination. Diarrhea may also negatively affect other patient outcomes by limiting the use of necessary treatments such as antibiotics, enteral nutrition, immunosuppressants, and antineoplastics. For example, severe chemotherapy-induced diarrhea may necessitate adjustment of the cancer treatment, which can decrease cure rates and contribute to mortality [3]. Similarly, diarrhea in solid organ transplant patients has been associated with an increased rate of acute rejection, graft loss, and decreased survival, presumably due to modification of the immunosuppressant regimen [1].
Pathophysiology
Traditional efforts to categorize diarrhea as osmotic, secretory, or inflammatory probably oversimplify the pathophysiology in hospitalized patients, who often have multiple factors simultaneously contributing to diarrhea, including underlying disease, trauma, inflammation, infection, altered diet, medications, and epithelial cell dysfunction and breakdown [28]. Recent attention has focused on the role of the intestinal microbiota, a complex community of >10 trillion (≥1013) microorganisms inhabiting the gut that plays an important role in human health and disease [17]. In the healthy state, the microbiota and host interact in a mutually beneficial manner, with the host providing a consistent nutrient source and environment and the microbiota participating in digestion, metabolism, immune homeostasis, and resistance to infection. In hospitalized patients, antibiotics and other interventions cause diarrhea by disrupting the microbiota and normal host-microbiota interaction [16–18, 29]. Thus, broad-spectrum antibiotics and antibiotics that achieve high concentrations within the intestinal lumen historically posed the greatest risk of antibiotic-associated diarrhea (AAD) and CDI because they disrupt the intestinal flora to a greater degree [20]. Also, just as host factors are important, individual differences in the microbial metagenome may play a role in predisposing patients to diarrhea, infection, or severe disease [3, 29, 30].
Next-generation sequencing technologies are now being used to more thoroughly characterize the impact of antibiotics on the microbiota, with the expectation that this will lead to an improved understanding of pathogenesis. For example, sequencing of bacterial DNA from feces of a patient who developed diarrhea during a course of oral amoxicillin-clavulanic acid showed marked reductions in commensal bacteria that are likely to be mechanistically linked to the development of diarrhea and persist beyond the course of antibiotics (Figure 1) [16]. In such cases, antibiotic removal of bacteria that normally produce butyrate, a colonic epithelial cell nutrient, and break down undigested carbohydrates results in epithelial dysfunction and an increased osmotic load within the intestinal lumen, leading to diarrhea [17, 18]. Another potential mechanism for AAD is decreased bacterial metabolism of bile acids because bile acids have a profound secretory effect on colonic epithelium [18]. Similar mechanisms by which microbiota alterations result in an increased susceptibility to infection (eg, with C. difficile) and contribute to the diarrhea associated with enteral feeding, chemotherapy, and radiotherapy are also being studied [3, 29, 30].
Figure 1.
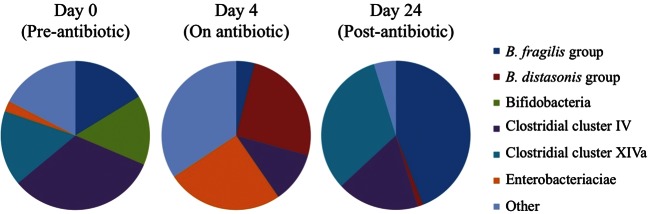
Fecal bacterial microbiota before, during, and after an episode of antibiotic-associated diarrhea. Pie charts represent the bacterial microbiota as determined by 16S ribosomal DNA amplification and sequencing of feces from a 39-year-old man who developed antibiotic-associated diarrhea within 24 hours of starting amoxicillin/clavulanic acid for sinusitis. The diarrhea persisted for the duration of the 10-day antibiotic course and resolved 4 days after antibiotic discontinuation. Adapted with permission from Young and Schmidt and ASM Press [16].
DIFFERENTIAL DIAGNOSIS
Nosocomial diarrhea differs from diarrhea originating in the community in several ways. First, unlike acute community-onset diarrhea, which is frequently infectious, relatively few cases in hospitals are attributable to infection during nonepidemic periods [5, 7, 11, 13, 31]. Second, diagnosis of infections in hospitalized patients is complicated by high rates of asymptomatic carriage (eg, C. difficile) and a lack of readily available diagnostic testing for other potential infectious causes [18, 19, 21, 25, 32–34]. Third, prompt recognition of infectious causes, especially C. difficile and norovirus, is desirable to limit transmission to other hospitalized patients [21, 25].
Infectious Causes Associated With Antibiotics
Clostridium difficile is the most common infectious cause of nosocomial diarrhea, representing 10%–20% of cases [12, 13, 19, 21, 23, 35]. CDI is typically associated with prior antibiotics but may follow other exposures that also disrupt the microbiota. (See recent guidelines and reviews for further discussion of CDI [21, 27, 32].) Other toxin-producing bacteria that have been associated with diarrhea following antibiotics are discussed next.
Klebsiella oxytoca
Pathogenic strains of Klebsiella oxytoca produce a toxin that inhibits DNA synthesis [33]. Such strains cause 50%–80% of cases of C. difficile negative, hemorrhagic colitis after antibiotics but are probably not a significant cause of nonbloody AAD [24, 36]. A prospective study of hospitalized patients with AAD identified cytotoxic K. oxytoca in 3 of 18 (16.7%) patients with bloody diarrhea but none of 89 patients with nonbloody diarrhea [36]. More recently, a laboratory study identified cytotoxic K. oxytoca in only 2.3% of 429 stool specimens submitted for C. difficile testing, confirming that K. oxytoca is relatively rare in routine stool samples [33]. Most patients are adults and present with acute onset of abdominal pain, bloody diarrhea, and leukocytosis after exposure to penicillins or other antibiotics [24]. Symptoms resolve upon antibiotic discontinuation, and therapy directed at K. oxytoca is not necessary [24]. Diagnosis is supported by recovery of pure or predominant K. oxytoca from stool or colon aspirate, but few wild-type strains produce toxins and tests for toxin-producing K. oxytoca are not available clinically [33, 36].
Clostridium perfringens
Enterotoxin-producing type A C. perfringens is an established cause of food poisoning and infrequent cause of AAD [23, 37]. The majority of data supporting a role for C. perfringens in AAD come from cross-sectional studies showing a higher prevalence and bacterial counts of C. perfringens in symptomatic patients vs controls, and from outbreaks of nosocomial diarrhea associated with C. perfringens and no other pathogens [23, 37]. Others have observed high carriage rates and similar concentrations of C. perfringens in asymptomatic patients [37]. Regardless, large studies suggest that only 1%–3% of diarrheal samples have C. perfringens as a potential cause; occasional studies report up to 8% as positive [19, 23, 35, 38]. Clinically, the median duration is 7 days, 1 in 5 patients have ≥10 stools per day, and patients respond to metronidazole [23]. Pseudomembranes have not been reported [23, 37]. Diagnostic testing is not widely available and <5% of wild-type C. perfringens strains are toxigenic, making culture impractical [35]. A research immunoassay has been developed to detect the enterotoxin (CPEnt) and polymerase chain reaction (PCR) for the cpe gene has also been used [19, 35].
Others
Staphylococcus aureus has been questioned as a cause of AAD but it can occur rarely (0.2%–4%), especially with methicillin-resistant strains that produce toxins [19, 39, 40]. Salmonella species are a rare cause of AAD and pseudomembranous colitis [18].
Infectious Causes not Associated With Antibiotics
Norovirus is the predominant cause of infectious gastroenteritis in the community, accounting for up to 90% of outbreaks and 5%–30% of patients presenting to clinics and hospitals with diarrhea during active seasons [41]. In hospitals, norovirus is an important cause of outbreaks but the extent of sporadic infections is unknown [25, 42]. Lopman et al conducted a 1-year study of diarrheal outbreaks in hospitals in England [25]. Using an outbreak definition of ≥2 cases from the same unit within 7 days, norovirus was detected in ≥1 specimens from 63% of outbreaks with samples collected [25]. Interestingly, the median duration of symptoms was 3 days and vomiting was absent in almost half of cases [25]. Rotavirus, astrovirus, and adenovirus can spread nosocomially in young children [43, 44]. Finally, enterotoxigenic Bacteroides fragilis is an emerging cause of diarrhea in community settings, but its role in nosocomial diarrhea is unknown and it does not appear to be associated with antibiotics [34].
Additional Infectious Causes in Immunocompromised Patients
Infectious diarrhea in immunocompromised patients is often longer and more severe, but asymptomatic carriage is also common [4, 11]. In addition to C. difficile, cytomegalovirus and gastrointestinal viruses (eg, rotavirus, adenovirus, norovirus) can cause significant morbidity in transplant patients [8, 10, 11, 31, 32]. Norovirus has been associated with prolonged symptoms and shedding lasting months in transplant patients [4]. Finally, parasites and bacteria that are typically associated with community-acquired diarrhea (eg, Giardia, Cryptosporidium, Strongyloides, Campylobacter) have been reported in transplant patients with hospital-onset diarrhea and should probably be considered when risk factors are present [8, 10, 22, 31].
Medications and Enteral Feeding
More than 700 drugs have diarrhea as a side effect and 15%–40% of patients on enteral feeding develop diarrhea [6, 20, 26, 29]. As a result, medications and enteral feeding account for the majority of cases of diarrhea in hospitalized patients, especially intensive care unit, transplant, and cancer patients [3, 5, 6, 9, 11, 27, 31]. Drug-induced diarrhea can be inflammatory or noninflammatory and caused by an effect on the intestine or the microbiota [3, 18, 20, 26]. Antibiotics are estimated to be responsible for 25% of drug-induced diarrhea but other medications also induce diarrhea commonly (Table 1) [3, 9, 20, 26]. Rates are particularly high with antineoplastic agents and immunosuppressants; iatrogenic diarrhea due to laxative overdose is also common (Table 1) [3, 10, 20]. Some medications contain sorbitol or other carbohydrates as excipients that can cause osmotic diarrhea [9, 20, 26]. Enteral feeding is a potential cause of diarrhea that may be reduced by continuous infusion and adjustment of the formula and fiber content, but diarrhea persists in 10%–15% of patients [6, 29].
Table 1.
Medications Most Commonly Associated With Diarrhea in Hospitalized Patients
| Medication | Frequency | Noninflammatory Diarrhea | Inflammatory Diarrhea |
|---|---|---|---|
| α-Glucosidase inhibitors (acarbose) | ≥20% | X | |
| Antiarrhythmics (digoxin toxicity, quinidine) | ≤10% | X | |
| Antibiotics (especially β-lactams, clindamycin, fluoroquinolones) | 5%–25% | X | X |
| Anti-inflammatory agents (olsalazine, gold agents, auranofin) | ≥20% | X | X |
| Antiretrovirals (nelfinavir, didanosine) | ≥20% | X | |
| β-Blockers (carvedilol) | ≤12% | X | |
| Cholinergic drugs (donepezil, pyridostigmine) | 10%–20% | X | |
| Colchicine | 80% | X | |
| Cytotoxic chemotherapeutic agents (irinotecan, 5-FU, capectine) | 30%–80% | X | X |
| Immunosuppressants (mycophenolate, tacrolimus, azathioprine) | 30%–60% | X | |
| Laxatives (osmotic, stimulant) | DD | X | X |
| Metformin | ≥20% | X | |
| Mg++ containing drugs (antacids, laxatives) | DD | X | |
| Octreotide | 5%–13% | X | |
| Oral electrolyte replacement solutions | ≥20% | X | |
| Poorly absorbable carbohydrates (lactulose, sorbitol excipients, probiotics) | DD | X | |
| Promotility agents (Reglan) | >10% | X | |
| Prostaglandin analogs (misoprostol) | ≥20% | X | |
| Selective serotonin reuptake inhibitors (sertraline) | ≥20% | X | |
| Ticlopidine | >10% | X | X |
| Tyrosine kinase inhibitors | 20%–60% | X | X |
Underlying Conditions
A wide array of chronic conditions such as lactose intolerance, inflammatory bowel disease, irritable bowel syndrome, and diabetic enteropathy can contribute to diarrhea in hospitals but rarely present as nosocomial diarrhea. Colonic ischemia is an important cause of acute bloody diarrhea and abdominal pain that can present in hospitalized patients, especially vascular surgery and elderly patients [45]. Other causes include substance abuse withdrawal and overflow diarrhea with fecal impaction [7, 9]. In critically ill patients, hypoalbuminemia has been associated with diarrhea but it is unclear if this is a primary cause or a marker of the severity of illness and malnutrition [6, 9]. Graft-vs-host disease is a common cause in HSCT patients [11].
Frequency and Etiologies by Patient Group
The frequency and causes of diarrhea vary significantly among hospitalized patient groups. Patients hospitalized for short periods with few exposures have relatively low rates of diarrhea (≤5%). Patients with longer lengths of stay and more intense treatments, such as intensive care, transplantation, and cancer chemotherapy, have higher rates of diarrhea, ranging from 15% to 80% (Table 2) [1, 3, 5, 6, 8, 10, 11, 14, 15, 27, 31, 46, 47]. In these groups, it can be difficult to determine the specific cause of symptoms but some etiologies are more likely than others (Table 2).
Table 2.
Relative Frequency of Clostridium difficile and Other Causes of Nosocomial Diarrhea in High-Risk Patient Subgroups
| Antibiotics | Intensive Care | Chemotherapy | SOT | HSCT | |
|---|---|---|---|---|---|
| Diarrhea (total)a | 5%–25% | ≥15%–40% | 20%–80% | 7%–27% | 43%–79% |
| Infectious (% of total)b | 10%–30% | 10%–30%c | ≤20%d | 17%–20% | 6%–19% |
| C. difficileb | 10%–25% | 10%–25%c | 10%–14% | 5%–10% | 1%–20% |
| Other toxigenic bacteriab,e | 1%–8% | 1%–8%c | Unknown | Unknown | Unknown |
| Norovirus and other virusesb | Unknown | Unknown | Unknown | Unknown | 8%f |
| Opportunistic infections (cytomegalovirus)b | N/S | N/S | N/S | ≤5% | <5% |
| Noninfectious (% of total)g | 70%–90% | 70%–90%c | ≥80%d | 80%–83% | 81%–94% |
Abbreviations: HSCT, hematopoietic stem cell transplant; N/S, not significant; SOT, solid organ transplant.
a Proportion of patients developing diarrhea in each risk group.
b Proportion of total diarrheal episodes in risk group attributable to an infectious cause or individual infectious agent.
c Data not available for intensive care population. Specified percentages are for antibiotic-associated diarrhea.
d Estimated percentage; data not available for chemotherapy patients.
e Antibiotic-associated: Clostridium perfringens, Klebsiella oxytoca, Staphylococcus aureus (does not include Bacteroides fragilis).
f Most often adenovirus, astrovirus, or rotavirus; likely includes a mix of nosocomial and community infections.
g Proportion of total diarrheal episodes with no infectious cause identified. Most common noninfectious causes by group are as follows: Antibiotics—antibiotic effect on microbiota or gut, laxatives; Intensive care—laxatives, antibiotics, sorbitol-containing medications, enteral feeding; Chemotherapy—laxatives, antineoplastic agents, antibiotics, radiotherapy; SOT—immunosuppressants, bacterial overgrowth; HSCT—chemotherapy, immunosuppressants, antibiotics, radiotherapy, laxatives, graft-vs-host disease.
EVALUATION AND MANAGEMENT
Evaluation
The first step in evaluating a patient with suspected nosocomial diarrhea is to verify the presence of diarrhea and assess the onset, duration, and severity of symptoms. The frequency, consistency, and volume of stools should be determined and any signs or symptoms of dehydration, infection, or sepsis should be noted. Severe abdominal cramping suggests an inflammatory process but is not specific for infection. Vomiting is also nonspecific but should prompt consideration of norovirus. Bloody stools occur rarely in AAD (or CDI) with the exception of K. oxytoca hemorrhagic colitis. For severity assessment, a number of factors have been examined as predictors of severe CDI but there are no validated criteria for CDI or non–C. difficile diarrhea [21]. A separate grading system is used for chemotherapy-induced diarrhea [3].
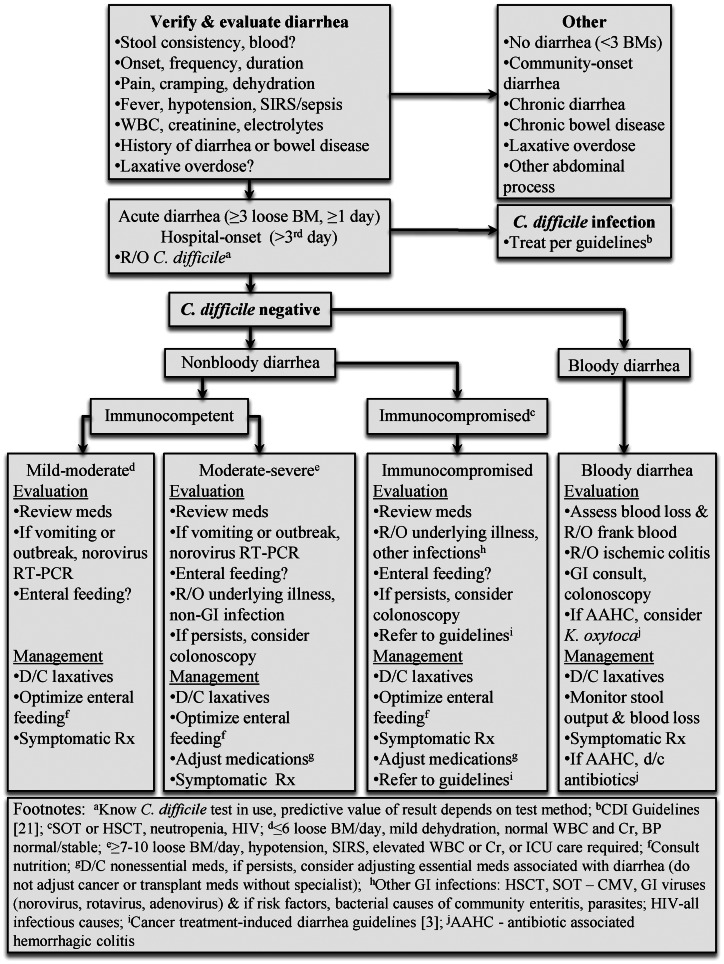
Clostridium difficile infection should be excluded in all patients with clinically significant diarrhea regardless of antibiotic exposure. It is important for physicians to know the type of test that is used for C. difficile at their local institution. Many laboratories are currently transitioning from tests that detect C. difficile toxins to tests that detect C. difficile directly, but methods vary between institutions and can have a significant impact on the predictive value of results [21]. The medical history should be reviewed for preexisting conditions that may contribute to diarrhea (eg, inflammatory bowel disease), and iatrogenic causes like laxative overdose should be excluded. If diarrhea persists and laxatives or CDI are not responsible, additional evaluation may be indicated, depending on the presence or absence of blood in the stool, the host immune status, and the severity of symptoms (Figure 2). Medications should be reviewed with a pharmacist to identify potential causes of drug-induced diarrhea (Table 1) [3, 6, 8]. If the patient is receiving enteral nutrition, the rate and site of infusion and formula should be evaluated for optimization [6, 29]. Norovirus testing by reverse transcriptase PCR should be considered in immunocompetent patients when vomiting is present, immunocompromised patients with persistent symptoms, and potential outbreaks when multiple patients or staff have similar symptoms on the same ward [4, 41, 48]. Testing for fecal white blood cells is insensitive and nonspecific and should not be performed routinely [49]. Tests for fecal lactoferrin and other inflammatory markers are potentially useful in selected cases but there are inadequate data in patients with nosocomial diarrhea to support their routine use at this time. Testing for other infectious causes has a low yield except possibly in transplant patients [22]. In these patients, active cytomegalovirus infection and other gastrointestinal viruses such as norovirus, adenovirus, and rotavirus should be excluded but most cases are due to medications or graft-vs-host disease [8, 10, 11, 31]. In human immunodeficiency virus–infected patients or transplant patients with risk factors for community-acquired bacteria or parasites or a history of diarrhea prior to admission, stool culture and tests for parasites may be considered but should not be performed routinely [22]. Testing a single sample is sufficient unless the patient is from a parasite-endemic region. Patients with significant, persistent diarrhea, and negative test results may be considered for colonoscopy. Colonic ischemia should be excluded in patients with bloody diarrhea [45]. Testing is generally not available for enterotoxin-producing strains of C. perfringens, K. oxytoca, and S. aureus. In select cases, when infection is strongly suspected, special arrangements may be made with the laboratory to look for overgrowth of these organisms in culture, but most strains do not produce toxins.
Figure 2.
Algorithm for the evaluation and management of patients with nosocomial diarrhea. Abbreviations: BM, bowel movement; BP, blood pressure; CDI, Clostridium difficile infection; CMV, cytomegalovirus; Cr, creatinine; D/C, discontinue; GI, gastrointestinal; HIV, human immunodeficiency virus; HSCT, hematopoietic stem cell transplant; ICU, intensive care unit; R/O, rule out; RT-PCR, reverse transcriptase polymerase chain reaction; SIRS, systemic inflammatory response syndrome; SOT, solid organ transplant; WBC, white blood cell.
Treatment
A staged approach is appropriate for immunocompetent patients with mild to moderate diarrhea [9, 29]. Laxatives should be discontinued and CDI should be treated when present [21]. Nonessential medications that are commonly associated with diarrhea should be discontinued and enteral nutrition, if present, should be optimized [6, 9, 29]. Supportive therapy should be administered, including oral or intravenous fluids and electrolyte repletion as necessary. Antidiarrheal agents have not been systematically evaluated in nosocomial diarrhea but may be useful in selected C. difficile–negative cases. Immunocompromised patients and patients with severe diarrhea require frequent monitoring and earlier, more aggressive intervention. For these patients, a more extensive evaluation for infectious causes may be indicated and medications should be carefully reviewed to identify drugs that may be contributing to symptoms. Guidelines are available for management of chemotherapy-induced diarrhea [3]. All patients with CDI or norovirus infection should be isolated as early as possible. Isolation may rarely be warranted with outbreaks of other infectious agents such as toxigenic C. perfringens or transmissible viruses.
Probiotics have been shown to be effective in preventing pediatric AAD and treating childhood infectious gastroenteritis, but their safety and efficacy in hospitalized adults are unproven [6, 29, 50]. In particular, caution should be used with probiotics in patients with compromised immunity or intestinal mucosa [21, 50, 51]. In these patients, there is an increased risk of gut translocation of probiotic organisms, and rare cases of bacteremia, fungemia, and mortality due to probiotic strains have been reported [51]. This is an active area of research that will continue to evolve.
SUMMARY AND FUTURE DIRECTIONS
Nosocomial diarrhea is a common and underappreciated complication of hospitalization that is generally not caused by C. difficile. Most cases are noninfectious but surprisingly little is known about the other causes of nosocomial diarrhea, especially in intensive care unit, transplant, and cancer patients. Medications cause the majority of diarrhea via side effects, toxicity, and disruption of the intestinal microbiome, which in the future may be ameliorated by changes in management, prebiotics, or probiotics.
There is a significant need for systematic prospective studies to define the epidemiology and impact of diarrhea in hospitalized patients and high-risk subgroups. In particular, the incidence of norovirus and other potential infectious causes needs to be clarified with studies that include comprehensive microbiologic testing and large numbers of patients. More data are also needed regarding changes in the microbiome introduced by hospitalization and common treatments and the role of the microbiome in diarrhea pathogenesis and complications. The Infectious Diseases Society of America and Society for Healthcare Epidemiology of America recently updated their guidelines for CDI [21] but guidelines do not exist for most other causes of nosocomial diarrhea, and there is a major need for standardization of criteria for diagnosis, severity assessment, and management.
Notes
Acknowledgments. We thank Cinda Christensen, PharmD, for her review of the table of medications associated with diarrhea.
Financial support. This work was supported by the National Institutes of Health and the National Center for Research Resources (grant number UL1 RR024146).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Bunnapradist S, Neri L, Wong W, et al. Incidence and risk factors for diarrhea following kidney transplantation and association with graft loss and mortality. Am J Kidney Dis. 2008;51:478–86. doi: 10.1053/j.ajkd.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 2.Lima NL, Guerrant RL, Kaiser DL, Germanson T, Farr BM. A retrospective cohort study of nosocomial diarrhea as a risk factor for nosocomial infection. J Infect Dis. 1990;161:948–52. doi: 10.1093/infdis/161.5.948. [DOI] [PubMed] [Google Scholar]
- 3.Stein A, Voigt W, Jordan K. Chemotherapy-induced diarrhea: pathophysiology, frequency and guideline-based management. Ther Adv Med Oncol. 2010;2:51–63. doi: 10.1177/1758834009355164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roddie C, Paul JP, Benjamin R, et al. Allogeneic hematopoietic stem cell transplantation and norovirus gastroenteritis: a previously unrecognized cause of morbidity. Clin Infect Dis. 2009;49:1061–8. doi: 10.1086/605557. [DOI] [PubMed] [Google Scholar]
- 5.Kelly TW, Patrick MR, Hillman KM. Study of diarrhea in critically ill patients. Crit Care Med. 1983;11:7–9. doi: 10.1097/00003246-198301000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Wiesen P, Van Gossum A, Preiser JC. Diarrhoea in the critically ill. Curr Opin Crit Care. 2006;12:149–54. doi: 10.1097/01.ccx.0000216583.64804.46. [DOI] [PubMed] [Google Scholar]
- 7.McFarland LV. Epidemiology of infectious and iatrogenic nosocomial diarrhea in a cohort of general medicine patients. Am J Infect Control. 1995;23:295–305. doi: 10.1016/0196-6553(95)90060-8. [DOI] [PubMed] [Google Scholar]
- 8.Maes B, Hadaya K, de Moor B, et al. Severe diarrhea in renal transplant patients: results of the DIDACT study. Am J Transplant. 2006;6:1466–72. doi: 10.1111/j.1600-6143.2006.01320.x. [DOI] [PubMed] [Google Scholar]
- 9.Ringel AF, Jameson GL, Foster ES. Diarrhea in the intensive care patient. Crit Care Clin. 1995;11:465–77. [PubMed] [Google Scholar]
- 10.Ginsburg PM, Thuluvath PJ. Diarrhea in liver transplant recipients: etiology and management. Liver Transpl. 2005;11:881–90. doi: 10.1002/lt.20500. [DOI] [PubMed] [Google Scholar]
- 11.Cox GJ, Matsui SM, Lo RS, et al. Etiology and outcome of diarrhea after marrow transplantation: a prospective study. Gastroenterology. 1994;107:1398–407. doi: 10.1016/0016-5085(94)90542-8. [DOI] [PubMed] [Google Scholar]
- 12.Samore MH, DeGirolami PC, Tlucko A, Lichtenberg DA, Melvin ZA, Karchmer AW. Clostridium difficile colonization and diarrhea at a tertiary care hospital. Clin Infect Dis. 1994;18:181–7. doi: 10.1093/clinids/18.2.181. [DOI] [PubMed] [Google Scholar]
- 13.Garey KW, Graham G, Gerard L, et al. Prevalence of diarrhea at a university hospital and association with modifiable risk factors. Ann Pharmacother. 2006;40:1030–4. doi: 10.1345/aph.1H028. [DOI] [PubMed] [Google Scholar]
- 14.Aksoy DY, Tanriover MD, Uzun O, et al. Diarrhea in neutropenic patients: a prospective cohort study with emphasis on neutropenic enterocolitis. Ann Oncol. 2007;18:183–9. doi: 10.1093/annonc/mdl337. [DOI] [PubMed] [Google Scholar]
- 15.Husain A, Aptaker L, Spriggs DR, Barakat RR. Gastrointestinal toxicity and Clostridium difficile diarrhea in patients treated with paclitaxel-containing chemotherapy regimens. Gynecol Oncol. 1998;71:104–7. doi: 10.1006/gyno.1998.5158. [DOI] [PubMed] [Google Scholar]
- 16.Young VB, Schmidt TM. Antibiotic-associated diarrhea accompanied by large-scale alterations in the composition of the fecal microbiota. J Clin Microbiol. 2004;42:1203–6. doi: 10.1128/JCM.42.3.1203-1206.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young VB. The intestinal microbiota in health and disease. Curr Opin Gastroenterol. 2012;28:63–9. doi: 10.1097/MOG.0b013e32834d61e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beaugerie L, Petit JC. Microbial-gut interactions in health and disease. Antibiotic-associated diarrhoea. Best Pract Res Clin Gastroenterol. 2004;18:337–52. doi: 10.1016/j.bpg.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Asha NJ, Tompkins D, Wilcox MH. Comparative analysis of prevalence, risk factors, and molecular epidemiology of antibiotic-associated diarrhea due to Clostridium difficile, Clostridium perfringens, and Staphylococcus aureus. J Clin Microbiol. 2006;44:2785–91. doi: 10.1128/JCM.00165-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chassany O, Michaux A, Bergmann JF. Drug-induced diarrhoea. Drug Saf. 2000;22:53–72. doi: 10.2165/00002018-200022010-00005. [DOI] [PubMed] [Google Scholar]
- 21.Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA) Infect Control Hosp Epidemiol. 2010;31:431–55. doi: 10.1086/651706. [DOI] [PubMed] [Google Scholar]
- 22.Bauer TM, Lalvani A, Fehrenbach J, et al. Derivation and validation of guidelines for stool cultures for enteropathogenic bacteria other than Clostridium difficile in hospitalized adults. JAMA. 2001;285:313–9. doi: 10.1001/jama.285.3.313. [DOI] [PubMed] [Google Scholar]
- 23.Larson HE, Borriello SP. Infectious diarrhea due to Clostridium perfringens. J Infect Dis. 1988;157:390–1. doi: 10.1093/infdis/157.2.390. [DOI] [PubMed] [Google Scholar]
- 24.Hogenauer C, Langner C, Beubler E, et al. Klebsiella oxytoca as a causative organism of antibiotic-associated hemorrhagic colitis. N Engl J Med. 2006;355:2418–26. doi: 10.1056/NEJMoa054765. [DOI] [PubMed] [Google Scholar]
- 25.Lopman BA, Reacher MH, Vipond IB, Sarangi J, Brown DW. Clinical manifestation of norovirus gastroenteritis in health care settings. Clin Infect Dis. 2004;39:318–24. doi: 10.1086/421948. [DOI] [PubMed] [Google Scholar]
- 26.Abraham B, Sellin JH. Drug-induced diarrhea. Curr Gastroenterol Rep. 2007;9:365–72. doi: 10.1007/s11894-007-0044-x. [DOI] [PubMed] [Google Scholar]
- 27.Bobak D, Arfons LM, Creger RJ, Lazarus HM. Clostridium difficile-associated disease in human stem cell transplant recipients: coming epidemic or false alarm? Bone Marrow Transplant. 2008;42:705–13. doi: 10.1038/bmt.2008.317. [DOI] [PubMed] [Google Scholar]
- 28.Sellin JH. The pathophysiology of diarrhea. Clin Transplant. 2001;15(suppl 4):2–10. doi: 10.1111/j.1399-0012.2001.00002.x. [DOI] [PubMed] [Google Scholar]
- 29.Whelan K, Schneider SM. Mechanisms, prevention, and management of diarrhea in enteral nutrition. Curr Opin Gastroenterol. 2011;27:152–9. doi: 10.1097/MOG.0b013e32834353cb. [DOI] [PubMed] [Google Scholar]
- 30.Manichanh C, Varela E, Martinez C, et al. The gut microbiota predispose to the pathophysiology of acute postradiotherapy diarrhea. Am J Gastroenterol. 2008;103:1754–61. doi: 10.1111/j.1572-0241.2008.01868.x. [DOI] [PubMed] [Google Scholar]
- 31.Kamboj M, Mihu CN, Sepkowitz K, Kernan NA, Papanicolaou GA. Work-up for infectious diarrhea after allogeneic hematopoietic stem cell transplantation: single specimen testing results in cost savings without compromising diagnostic yield. Transpl Infect Dis. 2007;9:265–9. doi: 10.1111/j.1399-3062.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 32.Riddle DJ, Dubberke ER. Clostridium difficile infection in solid organ transplant recipients. Curr Opin Organ Transplant. 2008;13:592–600. doi: 10.1097/MOT.0b013e3283186b51. [DOI] [PubMed] [Google Scholar]
- 33.Smith SA, Campbell SJ, Webster D, Curley M, Leddin D, Forward KR. A study of the prevalence of cytotoxic and non-cytotoxic Klebsiella oxytoca fecal colonization in two patient populations. Can J Infect Dis Med Microbiol. 2009;20:e169–72. doi: 10.1155/2009/913895. Accessed 1 February 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sears CL. Enterotoxigenic Bacteroides fragilis: a rogue among symbiotes. Clin Microbiol Rev. 2009;22:349–69. doi: 10.1128/CMR.00053-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heimesaat MM, Granzow K, Leidinger H, Liesenfeld O. Prevalence of Clostridium difficile toxins A and B and Clostridium perfringens enterotoxin A in stool samples of patients with antibiotic-associated diarrhea. Infection. 2005;33:340–4. doi: 10.1007/s15010-005-5067-3. [DOI] [PubMed] [Google Scholar]
- 36.Zollner-Schwetz I, Hogenauer C, Joainig M, et al. Role of Klebsiella oxytoca in antibiotic-associated diarrhea. Clin Infect Dis. 2008;47:e74–8. doi: 10.1086/592074. [DOI] [PubMed] [Google Scholar]
- 37.Modi N, Wilcox MH. Evidence for antibiotic induced Clostridium perfringens diarrhoea. J Clin Pathol. 2001;54:748–51. doi: 10.1136/jcp.54.10.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asha NJ, Wilcox MH. Laboratory diagnosis of Clostridium perfringens antibiotic-associated diarrhoea. J Med Microbiol. 2002;51:891–4. doi: 10.1099/0022-1317-51-10-891. [DOI] [PubMed] [Google Scholar]
- 39.Boyce JM, Havill NL. Nosocomial antibiotic-associated diarrhea associated with enterotoxin-producing strains of methicillin-resistant Staphylococcus aureus. Am J Gastroenterol. 2005;100:1828–34. doi: 10.1111/j.1572-0241.2005.41510.x. [DOI] [PubMed] [Google Scholar]
- 40.Flemming K, Ackermann G. Prevalence of enterotoxin producing Staphylococcus aureus in stools of patients with nosocomial diarrhea. Infection. 2007;35:356–8. doi: 10.1007/s15010-007-6268-8. [DOI] [PubMed] [Google Scholar]
- 41.Glass RI, Parashar UD, Estes MK. Norovirus gastroenteritis. N Engl J Med. 2009;361:1776–85. doi: 10.1056/NEJMra0804575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koo HL, Ajami NJ, Jiang ZD, Atmar RL, DuPont HL. Norovirus infection as a cause of sporadic healthcare-associated diarrhoea. J Hosp Infect. 2009;72:185–7. doi: 10.1016/j.jhin.2009.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Festini F, Cocchi P, Mambretti D, et al. Nosocomial rotavirus gastroenteritis in pediatric patients: a multi-center prospective cohort study. BMC Infect Dis. 2010;10:235. doi: 10.1186/1471-2334-10-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ford-Jones EL, Mindorff CM, Gold R, Petric M. The incidence of viral-associated diarrhea after admission to a pediatric hospital. Am J Epidemiol. 1990;131:711–8. doi: 10.1093/oxfordjournals.aje.a115555. [DOI] [PubMed] [Google Scholar]
- 45.Feuerstadt P, Brandt LJ. Colon ischemia: recent insights and advances. Curr Gastroenterol Rep. 2010;12:383–90. doi: 10.1007/s11894-010-0127-y. [DOI] [PubMed] [Google Scholar]
- 46.Ekberg H, Tedesco-Silva H, Demirbas A, et al. Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med. 2007;357:2562–75. doi: 10.1056/NEJMoa067411. [DOI] [PubMed] [Google Scholar]
- 47.Boudjema K, Camus C, Saliba F, et al. Reduced-dose tacrolimus with mycophenolate mofetil vs. standard-dose tacrolimus in liver transplantation: a randomized study. Am J Transplant. 2011;11:965–76. doi: 10.1111/j.1600-6143.2011.03486.x. [DOI] [PubMed] [Google Scholar]
- 48.Lopman BA, Reacher MH, Vipond IB, et al. Epidemiology and cost of nosocomial gastroenteritis, Avon, England, 2002–2003. Emerg Infect Dis. 2004;10:1827–34. doi: 10.3201/eid1010.030941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Savola KL, Baron EJ, Tompkins LS, Passaro DJ. Fecal leukocyte stain has diagnostic value for outpatients but not inpatients. J Clin Microbiol. 2001;39:266–9. doi: 10.1128/JCM.39.1.266-269.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morrow LE, Gogineni V, Malesker MA. Synbiotics and probiotics in the critically ill after the PROPATRIA trial. Curr Opin Clin Nutr Metab Care. 2012;15:147–50. doi: 10.1097/MCO.0b013e32834fcea8. [DOI] [PubMed] [Google Scholar]
- 51.Liong MT. Safety of probiotics: translocation and infection. Nutr Rev. 2008;66:192–202. doi: 10.1111/j.1753-4887.2008.00024.x. [DOI] [PubMed] [Google Scholar]